Abstract
Background & objectives
Spontaneous intracranial hypotension (SIH) is an underdiagnosed and debilitating condition caused by a spinal cerebrospinal fluid (CSF) leak. Although SIH can lead to substantial morbidity and disability, little data exists about patients’ perspectives. Without hearing directly from patients, our understanding of the full experience of having SIH is limited, as is our ability to identify and use appropriate patient-reported outcome measures (PROMs) within clinical care and research. The purpose of this study was to conduct qualitative interviews with confirmed SIH patients to fully describe their experiences and identify relevant concepts to measure.
Methods
Patients were recruited from an SIH specialty clinic at a large, U.S.-based healthcare center. Patients undergoing an initial consultation who were ≥ 18 years old, English-speaking, met the International Classification of Headache Disorders-3 criteria for SIH, and had a brain MRI with contrast that was positive for SIH were eligible to participate. During semi-structured qualitative interviews with a trained facilitator, participants were asked to describe their current SIH symptoms, how their experiences with SIH had changed over time, and the aspects of SIH that they found most bothersome. Analysts reviewed the data, created text summaries, and wrote analytic reports.
Results
Fifteen participants completed interviews. Common symptoms reported by patients included headache, tinnitus, ear fullness/pressure/pain, and neck or interscapular pain. Patients reported that their symptoms worsened over the course of their day and with activity. The most bothersome aspect of SIH was disruption to daily activities and limits to physical activities/exercise, which were severe. With regard to symptoms, the most bothersome and impactful included physical pain and discomfort (including headache), as well as fatigue.
Conclusions
Patients reported a diverse set of symptoms that were attributed to SIH, with devastating impacts on functioning and high levels of disability. Researchers considering use of PROMs for SIH should consider inclusion of both symptom scales and aspects of functioning, and future work should focus on evaluating the validity of existing measures for this patient population using rigorous qualitative and quantitative methods in diverse samples. Additionally, these data can be used to assist clinicians in understanding the impacts of SIH on patients.
Similar content being viewed by others

Background
Spontaneous intracranial hypotension (SIH) is an underdiagnosed condition caused by a spinal cerebrospinal fluid (CSF) leak that leads to substantial morbidity and disability [1,2,3]. Patients with SIH classically suffer from orthostatic headaches (i.e. headaches that are worse when upright and relieved with recumbency) as well as various cranial nerve related symptoms including diplopia, tinnitus, disequilibrium, and cognitive dysfunction [4]. There has been marked increase in the number of recognized cases of SIH in the past decade and it is now considered an important treatable cause of secondary headaches [5]. The efficacy of various treatments for SIH (i.e. epidural blood patching, surgery, venous embolization) are poorly established due to a paucity of prospective studies and the absence of any randomized controlled clinical trials [6]. The field is now pivoting toward these critical studies in order to establish consensus recommendations and to define a clear treatment algorithm. In order for these studies to be meaningful, patient reported outcome measures (PROMs) that adequately capture the spectrum of SIH patient symptoms and disability must be identified or developed.
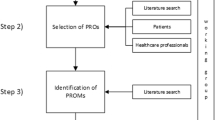
To be appropriate for use in clinical care and research contexts, PROMs for SIH should be anchored concretely in the patients’ experiences, capture the concepts that are most salient to patients, and supported by rigorous validity evidence [7,8,9] The first step in this process is to elicit these concepts from patients using rigorous qualitative methods [7]. To our knowledge, there are no PROMs with validity support for use in SIH, and to date, no PROMs have been developed specifically for SIH. A literature review on the efficacy of treatments for SIH reveals that the vast majority of studies report patient reported outcomes (PROs) subjectively without using formal PROMs, report symptoms based on the clinician’s impression, or do not describe outcome assessment methods at all [10]. The few studies that do include established PROMs use a visual analogue scale (VAS), which assesses only pain and is therefore woefully inadequate for capturing the range of symptoms and the spectrum of disability in SIH. Other currently available headache PROs may not capture the spectrum of what SIH patients experience given the considerable variability in presentation ranging from headache, visual disturbance, auditory changes, memory loss, etc [1]. To our knowledge, there are no prior studies that attempt to understand SIH by directly asking patients about their experience. This is important because a physician derived and reported understanding of SIH may differ from the lived experience of patients, and we are not able to measure what matters to patients without this understanding.
The purpose of this study was to conduct concept elicitation interviews with SIH patients to understand the key concepts that are relevant for understanding the symptoms and experiences of patients with SIH [7]. We plan to use the information from these qualitative interviews to develop or identify appropriate measures for adults with SIH that are grounded in the patient experience.
Methods
This is a prospective, qualitative concept elicitation study, using a narrative research approach [7]. The aims of concept elicitation are to understand the experience of the patient, identify common and uncommon symptoms that patients associate with SIH, and to document the terminologies used by patients when describing their experiences.
Participants & setting
Patients who were 18 years of age or older, English-speaking, met the International Classification of Headache Disorders-3 (ICHD-3) criteria for SIH, had a brain magnetic resonance imaging (MRI) with contrast that was positive for SIH (e.g. pachymeningeal enhancement, brain sagging, venous distension sign), and had not been previously treated at our institution were eligible to participate [11]. As part of standard clinical care, patients were contacted over the phone by the Neuroradiology Nurse Practitioner (NP) in order to gather clinical history, review imaging, and to determine suitability for a visit to Duke. A board certified Neuroradiologist with at least 6 years of experience specializing in the diagnosis and treatment of SIH reviewed all patient data and imaging to confirm the diagnosis. Once eligibility was assessed, the patient was contacted by a member of the qualitative study team to consent and schedule the interview. The Duke Institutional Review Board deemed this study exempt from human subjects research.
Data collection
Three qualitative interviewers, with an average of 5 years of qualitative interview experience, conducted one-on-one interviews with participants via a semi-structured interview guide (Supplementary Material 2), with interviewers given freedom to ask follow up probes of their own design, and at their own discretion. Participants were asked to describe their current SIH symptoms, how their experiences with SIH have changed (e.g. worse vs. better), and the aspects of SIH that they found most bothersome. Based on clinical knowledge of SIH, a list of potential symptoms was also included in the interview guide as possible probes [4]. If participants did not spontaneously discuss a symptom on the list, the interviewers would probe on the specific symptom. Finally, participants were asked about what first prompted them to seek treatment, what they did to manage their SIH symptoms, and their goals for upcoming treatment. All interviews were conducted over Zoom and audio recorded with participant permission. Interview recordings were transcribed via a third-party transcription service, and then quality checked by one of the analysts upon return. Participants were given a $25 gift card as remuneration.
Data Analysis
In addition to the audio files and interview transcripts, interviewers took detailed notes during the interview. In their notes, they reported on any challenges the participant had with speech (e.g. difficulty forming words, slurring of speech, stuttering), difficulty finding words, perceived attitudes about the questions asked, and interview duration. The interviewer conducting the interview then used all of these data (i.e. audio files, transcripts, interview notes) to complete individual interview text summaries shortly following completion of the interview using a standardized debriefing form [12, 13]. Text summaries were used to evaluate the data at the individual participant level, and included descriptions of the symptoms mentioned, dominant themes and other findings. Interviewers met bi-weekly during data collection to discuss the findings from the interviews, including symptom experiences of the participants and emerging ideas.
Once data collection was finished and all the individual interview text summaries were complete, two analysts, who were also interviewers, worked together to review the data across all participants. Analysts worked together to organize data by subtopic, based on the interview guide. From there, analysts divided sections of data, read through the data, and generated notes on these data as themes emerged. For the symptom list, analysts reviewed participant descriptions of their symptoms throughout the course of the interview and then grouped those experiences in a symptom list. Then the two analysts worked together to write analytic reports summarizing the emerging themes. Throughout the analysis process, the two analysts met frequently to discuss findings and provide feedback on each other’s writing. Final analytic reports were reviewed and approved by the study team. Based on these qualitative interviews of the SIH patient experience as well as the symptom list, target concepts were identified and recommendations for potential useful PROMs were generated in tabular format.
Results
Interviews occurred between August 2021 and January 2022. Of the 17 patients contacted, 15 agreed to participate and two patients did not return our attempts to contact them.
Demographics. The 15 individuals included 6 men and 9 women with diagnosed SIH who were on average 51 years old (std = 10 years). Most participants were white and all had at least a high school degree or equivalent (Table 1). Two reported that they were on disability leave from work, with 4 reporting full time employment, 4 reporting part-time employment, and 4 being retired. Five participants had no previous treatment for their SIH, with 9 participants reporting prior epidural blood patches, with the average number of patches being 2 (range: 1–5). About half of the participants (7/15) had a previous history of headaches prior to developing SIH.
Symptoms. Headache pain was reported by all participants when asked to describe their experience with SIH (Table 2). The majority of patients described their headache as including pain and pressure at the back of their head. Words like “pulling”, “pushing”, and “squeezing” were used to describe the pain and pressure, and “sharp” or “shooting” to indicate severe pain. One participant (ID: sc10) compared it directly to their experiences with typical headaches, “I would say it’s more a pressure. And I experience it – initially it was kind of all over and more like a typical headache. But after time and I started to curb my activity, it just becomes more of a pressure thing.”
Unprompted by the interviewer, the next most frequently listed symptoms were head pressure (which was discussed separately from head pain by patients) and ear pressure. Blurry vision, difficulty remembering things, word finding difficulty, sensitivity to light and sound were all symptoms that multiple participants endorsed, but almost no participants endorsed those symptoms until the interviewer listed them as an option (Table 2). Other less common symptoms included impaired speech (e.g., difficulty forming words, stutter), runny nose or liquid drainage (rhinorea), vomiting, loss of mobility, low back pain, difficulty swallowing (dysphagia), eyeball pain (ophthalmalgia), and sensitivity to smell (hyperosmia).
Factors affecting symptom rating and attributes. Several participants stated that their symptoms got worse as the day went on. To try and manage the pain and other symptoms, most participants would lie down or be still as often as they could. Participants used phrases like, if they “catch it early” it is easier to manage, but if they “push it” (e.g., don’t lay down, sit down, etc.) the symptoms (especially head pain and pressure) become unmanageable.
Another factor that affected perceived severity was the presence of an accompanying symptom. For example, dizziness with headache, or nausea with headache led the participant to classify the headache symptom as severe or intense, but days with only headache pain were classified as moderate. For example, one participant (ID: sc06) said, “If I had the spinning, then I would say it was severe but I haven’t had the spinning actually in a couple weeks; and that’s when it’s bad. But I’m also at a point where there’s things I don’t do and especially won’t do in the afternoon because of the possibility of the dizziness.”
Most Bothersome Aspects of SIH. When discussing the most bothersome aspect of living with SIH, participants talked about the disruption to daily activities caused by the painful and uncomfortable symptoms they experienced, including headache, fatigue, and nausea (Table 3). For example, people mentioned being frustrated that they could not run to the store on a whim or physically pick up their children. Similarly, other participants identified the most bothersome aspect of SIH as limits on their ability to be physically active and to exercise. Participants described having to “dial things back” or limit their activities in order to prevent pain episodes. Most participants described needing to lie down or sit down several times a day in order to manage the head pain and alleviate the head pressure. Moreover, two participants mentioned the social impact of not being able to do certain activities because those activities could cause them pain. Three participants said that their SIH limited their ability to interact with their children, restricting their physical movement so they could not hold their children or impacting their ability to participate in school activities (e.g. see quote from participant #sc04 in Table 3).
Expectations for treatment. Most patients stated they hoped treatment could improve the headache severity and pain intensity. Many have the expectation that the pain and accompanying symptoms will completely go away with treatment. A few participants stated they were unsure if all symptoms would go away, but they were hopeful that treatment could at least help with the headache severity, and they stated they could live with mild headaches if there was no choice.
“I get migraines, and people ask me, “Well, try your migraine medication.” It doesn’t work because during this time, I have had migraines, and I’ve taken my medication, and that alleviates my migraine, but it does not alleviate the pain and the pressure in the back of my head.” - sc02
“Yeah. Well, I hope I can help someone else. And yeah I’m just excited because I was thinking probably even 50 years ago, I bet there wasn’t even treatment for something like this. So, I feel really fortunate that they have a way to hopefully treat this and control it.“ – sc10
Experience with diagnosis. Nine participants reported that they received treatment for another condition before they were diagnosed with SIH. These included: sinus infections, migraines, allergies, sarcoidosis, TMJ, stress, and psychological issues, as well as side effects of pre-existing conditions such as back problems or pregnancy. Participants described waiting for months or even years between the initial onset of their symptoms and their diagnosis or treatment. Of the 13 participants who reported a timeframe, 4 reported that they were treated within about 3 months of initial symptoms, 5 reported they were treated within 6 months to a year of the initial onset of symptoms, and 4 reported it took over a year from the onset of symptoms to their SIH diagnosis, with one participant reporting that they were still waiting (over a year) for treatment as of their interview date. The longest time to diagnosis of those we spoke to was over 2 years. Nearly all participants (11/15) reported that their initial symptom was a headache or migraine. Two participants were diagnosed with SIH as a result of a scan for another condition. One participant was trained as a medical professional and was therefore able to advocate for a diagnosis after recognizing the symptoms, despite their doctor’s opinion that the symptoms were stress-related. Another reported that their headaches started after a car accident, and they were able to easily access care and receive a diagnosis quickly because they were friends with a neurologist. One participant described having to beg to be seen by their spouse’s neurologist out of desperation for answers. Once participants were diagnosed, they described the comfort that their SIH diagnoses brought; with one (ID: sc07) saying: “It was a relief to know it was not all literally in my head, that they had findings, that there is something going on, and they can see it, that it’s not just stress.” While another reported being “thrilled” to finally have a diagnosis.
Potentially useful PROMs
A number of measurable concepts were identified as meaningful to patients diagnosed with SIH. For each concept, existing measures with published validity evidence were identified as potentially useful for patients with SIH (Table 4).
Discussion
This article represents, to our knowledge, the first description of patient experiences using qualitative methods to elicit meaningful concepts directly from patients with ICHD-3 confirmed SIH. As expected, headache was the primary symptom in SIH with all patients reporting the presence of a headache without prompting. SIH patients also described multiple additional concerning symptoms. Tinnitus and ear fullness were the next most common after headache, followed by neck and interscapular pain, nausea, fatigue, cognitive dysfunction, disequilibrium, hyperacusis, photophobia and diplopia, as well as many others. It is important to note that eliciting these symptoms required prompting in many cases, and that some patients conceptualized ‘worse’ days as those when they had additional symptoms alongside their headache (e.g. dizziness, nausea).
The list of symptoms associated with SIH that patients provided in the qualitative interviews align with and expand on those previously reported in the literature. In a systematic review and meta-analysis, D’Antona et al. found that headache was the most common symptom in SIH patients (present in 97% of patients) [4]. The reported non-headache SIH symptoms also align with this work, although our study was more exhaustive and included additional symptoms not previously captured such as interscapular pain, word finding difficulty, photophobia, hearing loss, impaired speech, rhinorrhea, ophthalmalgia, and hyperosmia. Movement disorders (e.g. ataxia, bradykinesia) were not reported by our patient cohort, but are rarely reported in the SIH literature, and are typically represented in the form of single case reports [14,15,16]. It also is important to note that patients utilized lay terms when describing their symptoms (see examples in Table 2); any symptom PROM that is developed should utilize terminology that patients can understand.
Universally, SIH patients reported considerable disability and a substantial impact on their daily function. In a cross-sectional online survey of SIH patients, Cheema et al. [17] also found substantial reductions in quality of life in SIH patients using the EQ-5D-5 L measure [18] and that the headaches due to SIH resulted in a very severe impact on functioning based on the Headache Impact Test (HIT-6) [19]. The qualitative results in our study are consistent with these findings. This prior report also found that greater than 25% of SIH patients had lost their job secondary to the resultant disability, which is greater than the rate found in our cohort (n = 2) [17]. This discrepancy may be due to the smaller sample size in the present study and the fact that 26.7% (n = 4) were already retired. In addition to functioning, patients in our cohort described impacts on social/role functioning as well as impacts on daily activities that were often considerable.
This study formally and qualitatively documents the patient experience of SIH, but also generates two important conclusions that can to help guide future measurement strategies. First, patients should be prompted to capture the extent and breadth of variably present symptoms in SIH. In the absence of prompting, it is likely that some symptoms that are concerning to patients and that may be helpful in differentiating SIH from other causes of headache will remain uncaptured. Second, patient disability was considerable and impacts on function were high. As a result, any patient-centered measurement strategy for SIH should capture not only symptom severity but also the downstream effects on quality of life such as disruptions in social, emotional, and physical functioning.
Based on the results from our qualitative interviews, we have identified a number of concepts that are measurable and meaningful to patients (Table 4). While identifying what is important to patients is vital for any measurement strategy, decisions about which specific PROMs to utilize for SIH will ultimately be dependent on the proposed context of use [20]. Currently, the field would benefit from measures that track patient status over time within a clinical setting, as well as highly accurate and sensitive measures to evaluate treatment benefit. An additional use of measures would be to differentiate between SIH and other diagnoses. Thus, our recommendations (Table 4) include existing measures that may be useful for these purposes, with a focus on measures following a rigorous process for development (e.g. PROMIS®) and/or those listed within common data elements (e.g. National Institutes of Health Heal Initiative) [21]. In addition to the list provided, we suggest that clinicians and researchers also consider screening for depression and anxiety in these patients [21]. Please note, further cognitive debriefing and psychometric evaluation are needed to support the choice of specific measures; this work is currently underway.
Establishing a diagnosis of SIH can be challenging given the protean symptom profile which can overlap with that expected for other diagnoses. For example, the classic presenting symptom in SIH, an orthostatic headache, is not always present in SIH patients and can be seen in the setting of other diagnoses such as cervicogenic headache and postural orthostatic tachycardia syndrome [22, 23]. As a result, greater than 90% of SIH patients are initially misdiagnosed, delaying curative intervention and compounding disability through prolonged disease courses and unnecessary treatments [24]. Qualitatively documenting the spectrum of symptom presentation in SIH will allow for future research focused on specific symptoms that may allow for the differentiation between these often confused clinical diagnoses.
Although the demographics of the included population in this study generally align with those reported in the prior SIH literature, [4] our sample was relatively affluent. Given that the patient cohort was derived from those presenting to a major SIH treatment center, this likely reflects the requirement for considerable travel for treatment in most cases, including across state lines. Ideally, future studies would further expand upon our work to include a broader and more diverse subset of the SIH population. Another potential limitation of this study is the stringent inclusion criteria that required not only a confirmed ICHD-3 SIH diagnosis but also a brain MRI that was positive for SIH findings. It is well known that some patients with ICHD-3 confirmed SIH have a normal brain MRI [22]. There may be yet unknown differences in the SIH patient experience and symptom profile between those with a positive brain MRI and those where it is negative. Finally, given the prevalence of memory dysfunction in the SIH population, the inability of patients to recall some of their experiences could introduce bias when trying to capture the full spectrum of disease, a potentially pervasive problem that is not limited solely to this study.
Conclusion
SIH is a debilitating condition that is increasingly recognized as a treatable cause of secondary headaches. However, the conduct of important studies and the development of treatment guidelines have been hampered by the lack of validated PROMs for SIH, without which it is difficult to determine the comparative efficacy of different treatments. This study represents the first critical step in establishing such PROMs by reporting the SIH patient experience using qualitative concept elicitation interviews. Future work should build upon this effort to develop new measures or to determine the appropriateness of existing measures which should capture both the severity of patient symptoms as well as the impact of SIH on patient function and the extent of their resultant disability.
Data Availability
Not applicable.
Abbreviations
- SIH:
-
Spontaneous intracranial hypotension
- CSF:
-
Cerebrospinal fluid
- PROM:
-
Patient-reported outcome measure
- VAS:
-
Visual analogue scale
- MRI:
-
Magnetic resonance imaging
- NP:
-
Nurse practitioner
- HIT-6:
-
Headache impact test
- ICHD-3:
-
International classification of headache disorders-3 criteria
References
Amrhein TJ, Kranz PG (2019) Spontaneous intracranial hypotension: imaging in diagnosis and treatment. Radiol Clin North Am 57:439–451 2019/02/03. https://doi.org/10.1016/j.rcl.2018.10.004
Schievink WI, Maya MM, Moser FG et al (2018) Coma: a serious complication of spontaneous intracranial hypotension. Neurology 90:e1638–e1645. 2018/04/15
Jesse CM, Häni L, Fung C et al (2022) The impact of spontaneous intracranial hypotension on social life and health-related quality of life. J Neurol 269:5466–5473. https://doi.org/10.1007/s00415-022-11207-7
D’Antona L, Jaime Merchan MA, Vassiliou A et al (2021) Clinical presentation, Investigation Findings, and treatment outcomes of spontaneous intracranial hypotension syndrome: a systematic review and Meta-analysis. JAMA Neurol 78:329–337. 2021/01/05
Schievink WI, Maya MM, Moser F et al (2007) Frequency of spontaneous intracranial hypotension in the emergency department. J Headache Pain 8:325–328. https://doi.org/10.1007/s10194-007-0421-8
Kranz PG, Malinzak MD, Amrhein TJ et al (2017) Update on the diagnosis and treatment of spontaneous intracranial hypotension. Curr Pain Headache Rep 21:37. https://doi.org/10.1007/s11916-017-0639-3
Patrick DL, Burke LB, Gwaltney CJ et al (2011) Content validity–establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO good research practices task force report: part 1–eliciting concepts for a new PRO instrument. Value Health 14:967–977. 2011/12/14
Patrick DL, Burke LB, Gwaltney CJ et al (2011) Content validity–establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 2–assessing respondent understanding. Value Health 14:978–988. 2011/12/14
Patient-Focused FDAFDA (2018) Drug Development Guidance Series for Enhancing the Incorporation of the Patient’s Voice in Medical Product Development and Regulatory Decision Making.
Amrhein TJ, Kranz PG, Cantrell S et al (2022) Efficacy of epidural blood patching or surgery in spontaneous intracranial hypotension: an evidence map protocol. Syst Rev 11:116. 2022/06/07
International Headache Society. The International Classification of Headache Disorders 3rd edition, https://www.ichd-3.org/7-headache-attributed-to-non-vascular-intracranial-disorder/7-2-headache-attributed-to-low-cerebrospinal-fluid-pressure/7-2-3-headache-attributed-to-spontaneous-intracranial-hypotension/ (accessed 15 March 2021)
Willis GB (2015) Analysis of the cognitive interview in questionnaire design. Oxford University Press
Miller K, Chepp V, Willson S et al (2014) Cognitive interviewing methodology. John Wiley & Sons
Iyer RS, Wattamwar P, Thomas B (2017) Reversible Holmes’ tremor due to spontaneous intracranial hypotension. BMJ Case Reports ; 2017: bcr-2017-220348. DOI: https://doi.org/10.1136/bcr-2017-220348
Mokri B, Ahlskog JE, Luetmer PH (2006) Chorea as a manifestation of spontaneous CSF leak. Neurology 67:1490–1491. https://doi.org/10.1212/01.wnl.0000240059.96502.bf
Salazar R (2016) Spontaneous intracranial hypotension Associated with Kinetic Tremor and Ataxia. Tremor Other Hyperkinet Mov (N Y) 6:366 2016/06/29. https://doi.org/10.7916/d8hq3zn5
Cheema S, Joy C, Pople J et al (2022) Patient experience of diagnosis and management of spontaneous intracranial hypotension: a cross-sectional online survey. BMJ Open 12:e057438. https://doi.org/10.1136/bmjopen-2021-057438
EuroQol–a new facility for the measurement of health-related quality of life (1990) Health Policy 16:199–208 1990/11/05. https://doi.org/10.1016/0168-8510(90)90421-9
Kosinski M, Bayliss MS, Bjorner JB et al (2003) A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res 12:963–974 2003/12/04
US Food and Drug Administration (2020), June 18 FDA patient-focused drug development guidance series for enhancing the incorporation of the patient’s voice in medical product development and regulatory decision making, https://www.fda.gov/drugs/development-approval-process-drugs/fda-patient-focused-drug-development-guidance-series-enhancing-incorporation-patients-voice-medical
National Institutes of Health HEAL Initiative. Common Data Elements (CDEs), Program (2022) https://heal.nih.gov/data/common-data-elements accessed February 2, 2023)
Kranz PG, Gray L, Amrhein TJ (2018) Spontaneous intracranial hypotension: 10 myths and misperceptions. Headache: The Journal of Head and Face Pain 58:948–959. https://doi.org/10.1111/head.13328
D’Amico D, Usai S, Chiapparini L et al (2020) Headache in spontaneous intracranial hypotension: an overview with indications for differential diagnosis in the clinical practice. Neurol Sci 41:423–427. 2020/10/10
Schievink WI (2003) Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol 60:1713–1718. https://doi.org/10.1001/archneur.60.12.1713
Acknowledgements
Not applicable.
Funding
Financial support for this project was provided by Putnam Seed Fund: Duke University Medical Center Department of Radiology and the Tate Family Charitable Gift. Funders were not involved in the design of the study, the collection, analysis, or interpretation of the data, nor writing the manuscript.
Author information
Authors and Affiliations
Contributions
TJA, MM, KE, MDM, PGK, CKZ: Conception and study design.
TJA, MM, KE, MDM, LG, PGK, EHW, CKZ: Acquisition, analysis, interpretation of data.
TJA, MM, KE, MDM, LG, PGK, EHW, CKZ: Drafting and revising the manuscript.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Duke Institutional Review Board deemed this study exempt from human subjects research.
Consent for publication
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Disclaimer
The views expressed in this submitted article are those of the authors and do not represent an official position by the funder or institution.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amrhein, T.J., McFatrich, M., Ehle, K. et al. Patient experience of spontaneous intracranial hypotension (SIH): qualitative interviews for concept elicitation. J Patient Rep Outcomes 7, 82 (2023). https://doi.org/10.1186/s41687-023-00625-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41687-023-00625-4