Abstract
Repulsive guidance molecule (RGM) is a glycosylphosphatidylinositol (GPI)-anchored glycoprotein that has diverse functions in the developing and pathological central nervous system (CNS). The binding of RGM to its receptor neogenin regulates axon guidance, neuronal differentiation, and survival during the development of the CNS. In the pathological state, RGM expression is induced after spinal cord injury, and the inhibition of RGM promotes axon growth and functional recovery. Furthermore, RGM expression is also observed in immune cells, and RGM regulates inflammation and neurodegeneration in autoimmune encephalomyelitis. RGMa induces T cell activation in experimental autoimmune encephalomyelitis (EAE), which is the animal model of multiple sclerosis (MS). RGM is expressed in pathogenic Th17 cells and induces neurodegeneration by binding to neogenin. Angiogenesis is an additional key factor involved in the pathophysiology of EAE. Via neogenin, treatment with RGMa can suppress endothelial tube formation; this finding indicates that RGMa inhibits neovascularization. These observations suggest the feasibility of utilizing the RGMa-neogenin signaling pathway as a therapeutic target to overcome inflammation and neurodegeneration. This review focuses on the molecular mechanisms of inflammation and angiogenesis via RGM-neogenin signaling.
Similar content being viewed by others
Background
Repulsive guidance molecule (RGM) is a glycosylphosphatidylinositol (GPI)-anchored glycoprotein with an N-terminal signal peptide, an Arg-Gly-Asp site, a partial von Willebrand type D domain, and a hydrophobic domain of unknown function [1]. RGM was originally identified as an axon repellent in the chick retinotectal system [2, 3]. Neogenin, the receptor for RGM and netrins, is widely expressed in both embryonic and adult tissues and mediates various functions [4, 5]. There are three homologs of RGM in vertebrates: RGMa, RGMb (DRAGON), and RGMc (hemojuvelin). The homologies of chick RGM to mouse RGMa, RGMb, and RGMc are 78, 43, and 40%, respectively.
The binding of RGMa to neogenin regulates axon guidance, neuronal differentiation, and survival during the development of the central nervous system (CNS) [6,7,8]. Although RGMa expression levels are relatively low in the adult CNS, RGMa expression is induced following ischemic stroke in humans and spinal cord injury in rats [9, 10]. In an animal model of spinal cord injury, treatment with an RGMa-neutralizing antibody at the lesion site significantly enhances axon regeneration and motor function recovery [11]. Because the stimulation of neurons with RGMa induces RhoA and ROCK (Rho-associated coiled-coil-containing protein kinase), resulting in axon growth inhibition, the effect of this antibody may be dependent on the inhibition of this signaling pathway.
In addition to its aforementioned roles, RGMa is involved in neuroinflammatory diseases. The notion that the pathogenesis of multiple sclerosis (MS) is associated with acquired autoimmunity to the CNS has been widely accepted. In MS, immune cells infiltrate the CNS and attack myelin sheaths, leading to demyelination, axonal damage, and neurological disabilities [12, 13]. CD4+ T cells are critical effector cells in CNS inflammation [14]. Interestingly, the inhibition of RGMa via a neutralizing antibody reduces cytokine production, demyelination, and neurodegeneration and relieves neurological deficits in experimental autoimmune encephalomyelitis (EAE) [15, 16]. In addition to its role in neuroimmune interactions, RGMa inhibits angiogenesis, which is often accompanied by inflammation, as mentioned below.
Thus, these findings indicate that the RGM-neogenin signaling pathway is strongly associated with disease severity in neuroinflammatory diseases. In this review, we introduce the pivotal role of RGMa in inflammation and angiogenesis and discuss the potential therapeutic implications of targeting this signaling.
The RGMa-neogenin pathway mediates autoimmune encephalomyelitis
Although the RGM-neogenin interaction mediates diverse functions in the developing and adult CNS, we also found that RGMa was expressed in bone marrow-derived dendritic cells and that neogenin was expressed in CD4+ T cells. Based on these observations, we assessed the role of RGMa in immune systems and found that the inhibition of RGMa suppressed the T cell response and attenuated the severity of EAE [15]. RGMa treatment of CD4+ T cells induces the activation of the small GTPase Rap1 and increases the adhesion of CD4+ T cells to intracellular adhesion molecule-1 (ICAM-1). Treatment with an RGMa-neutralizing antibody attenuates the clinical severity of myelin oligodendrocyte glycoprotein (MOG)-induced EAE and diminishes relapses in proteolipid protein (PLP)-induced EAE. In humans, an RGMa-specific antibody reduces T cell proliferation and pro-inflammatory cytokine production in peripheral blood mononuclear cells (PBMCs) from individuals with MS. Thus, the RGMa-neogenin signaling pathway is involved in T cell-mediated autoimmune processes in MS (Fig. 1).
RGMa-neogenin signaling mediates autoimmune encephalomyelitis. RGMa in antigen-presenting cells (APCs) binds to neogenin, leading to the activation of CD4+ T cells in both the peripheral and the central nervous systems. Blocking RGMa with a neutralizing antibody diminishes immune responses and ameliorates the severity of EAE
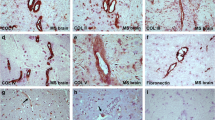
Interferon-gamma (IFN-γ)-producing Th1 cells were initially regarded as a predominant effector CD4+ T cell subset that induces the pathogenesis of MS [17]. More recently, interleukin-23 (IL-23) has been shown to be required for the induction of EAE [18] and the pathogenic activity of T helper type 17 (Th17) cells. The key role of IL-17-producing Th17 cells in the pathogenesis of EAE has been established [19]. Indeed, a deficiency of IL-17, IL-17 receptor, or IL-23 receptor diminishes clinical signs in EAE [20,21,22]. Interestingly, among T cell subsets, including Th0, Th1, Th17, and Treg cells, Th17 cells highly express RGMa. The specific function of RGMa in Th17 cells was determined to be involved in neurodegeneration in EAE [16]. In particular, in Th17 cells, RGMa binds to neogenin and induces Akt dephosphorylation and axonal degeneration (Fig. 2). An RGMa-specific neutralizing antibody diminished neuronal damage and alleviated clinical symptoms of Th17-induced EAE. Taken together, these observations suggest that RGMa could be a therapeutic target for MS. Polymorphisms of RGMa have been correlated with expression changes in IFN-γ and tumor necrosis factor (TNF) in MS patients [23]. This finding raises the intriguing possibility of an association between genetic susceptibility in MS pathogenesis and RGMa.
Angiogenesis via the RGMa-neogenin pathway
In MS, in addition to various prominent features, such as inflammation, demyelination, and axonal damage, neovascularization is found in inflammatory lesions. In EAE, an angiogenic response is observed following alterations in blood-brain barrier (BBB) permeability and the release of vascular endothelial growth factor (VEGF) [24, 25]. Both detrimental and beneficial effects have been reported in angiogenesis. Since the angiogenic response is related to excess energy consumption and the expansion of inflammation, this response’s pathological contributions to the disease progression of MS and EAE are widely accepted [26]. However, trophic factors from new vessels exert positive effects on the nervous systems. VEGF derived from new blood vessels exhibits pro-inflammatory effects during the early phase of EAE but is involved in repair processes during the late phase of EAE. VEGF mediates the proliferation, migration, and differentiation of neural progenitors and the survival and migration of oligodendrocyte precursor cells [27, 28]. Prostaglandin I2 (PGI2) produced from new blood vessels is associated with motor recovery in EAE [29]. Thus, specific molecules derived from new vascular cells can be therapeutic targets for MS.
We have shown that RGMa inhibits angiogenesis via neogenin [30]. In the presence of VEGF, RGMa suppresses endothelial tube formation by human umbilical artery endothelial cells (HUAECs), and this effect could be partially reversed by knocking down neogenin. RGMa treatment of HUAECs decreased VEGF-induced phosphorylation of focal adhesion kinase (FAK). It has been demonstrated that netrins, the other ligands of neogenin, also regulate neovascularization. The binding of netrin-4 to neogenin causes neogenin to associate with its co-receptor Unc5b and inhibits angiogenesis both in cultured HUAECs and in an animal model of laser-induced choroidal neovascularization [31]. In contrast, netrin-1 promotes tube formation in HUAECs, and knocking down netrin-1 in zebrafish inhibits vascular sprouting, suggesting that netrin-1 induces angiogenesis [32,33,34]. However, it is also reported that netrin-1 inhibits angiogenesis via the activation of Unc5b and the disruption of Unc5b induces excess vessel branching and the extension of endothelial filopodia [35, 36]. Netrin-4 binds only to neogenin, whereas netrin-1 is predicted to interact with neogenin, Unc5b, and Unc5c. Differences in binding affinity to neogenin might be responsible for these proteins’ different effects on angiogenesis.
Conclusions
Here, we reviewed the role of RGMa in inflammation and angiogenesis, particularly in MS. Since RGMa mediates both immune responses and neurodegeneration in EAE, the inhibition of RGMa could be a promising therapeutic intervention for MS. Further research will establish the feasibility of an anti-RGMa antibody for treating MS.
Abbreviations
- BBB:
-
Blood-brain barrier
- CNS:
-
Central nervous systems
- EAE:
-
Experimental autoimmune encephalomyelitis
- FAK:
-
Focal adhesion kinase
- GPI:
-
Glycosylphosphatidylinositol
- HUAECs:
-
Human umbilical artery endothelial cells
- ICAM-1:
-
Intracellular adhesion molecule-1
- IFN-γ:
-
Interferon-gamma
- IL:
-
Interleukin
- MOG:
-
Myelin oligodendrocyte glycoprotein
- MS:
-
Multiple sclerosis
- PBMCs:
-
Peripheral blood mononuclear cells
- PGI2 :
-
Prostaglandin I2
- PLP:
-
Proteolipid protein
- RGM:
-
Repulsive guidance molecule
- Th1:
-
T helper type 1
- TNF:
-
Tumor necrosis factor
- VEGF:
-
Vascular endothelial growth factor
References
Yamashita T, Mueller BK, Hata K. Neogenin and repulsive guidance molecule signaling in the central nervous system. Curr Opin Neurobiol. 2007;17:29–34.
Monnier PP, Sierra A, Macchi P, Deitinghoff L, Andersen JS, Mann M, Flad M, Hornberger MR, Stahl B, Bonhoeffer F, et al. RGM is a repulsive guidance molecule for retinal axons. Nature. 2002;419:392–5.
Stahl B, Muller B, von Boxberg Y, Cox EC, Bonhoeffer F. Biochemical characterization of a putative axonal guidance molecule of the chick visual system. Neuron. 1990;5:735–43.
De Vries M, Cooper HM. Emerging roles for neogenin and its ligands in CNS development. J Neurochem. 2008;106:1483–92.
Mueller BK, Yamashita T, Schaffar G, Mueller R. The role of repulsive guidance molecules in the embryonic and adult vertebrate central nervous system. Philos Trans R Soc Lond B Biol Sci. 2006;361:1513–29.
Matsunaga E, Tauszig-Delamasure S, Monnier PP, Mueller BK, Strittmatter SM, Mehlen P, Chedotal A. RGM and its receptor neogenin regulate neuronal survival. Nat Cell Biol. 2004;6:749–55.
Rajagopalan S, Deitinghoff L, Davis D, Conrad S, Skutella T, Chedotal A, Mueller BK, Strittmatter SM. Neogenin mediates the action of repulsive guidance molecule. Nat Cell Biol. 2004;6:756–62.
Wilson NH, Key B. Neogenin interacts with RGMa and netrin-1 to guide axons within the embryonic vertebrate forebrain. Dev Biol. 2006;296:485–98.
Schwab JM, Conrad S, Monnier PP, Julien S, Mueller BK, Schluesener HJ. Spinal cord injury-induced lesional expression of the repulsive guidance molecule (RGM). Eur J Neurosci. 2005;21:1569–76.
Schwab JM, Monnier PP, Schluesener HJ, Conrad S, Beschorner R, Chen L, Meyermann R, Mueller BK. Central nervous system injury-induced repulsive guidance molecule expression in the adult human brain. Arch Neurol. 2005;62:1561–8.
Hata K, Fujitani M, Yasuda Y, Doya H, Saito T, Yamagishi S, Mueller BK, Yamashita T. RGMa inhibition promotes axonal growth and recovery after spinal cord injury. J Cell Biol. 2006;173:47–58.
Hauser SL, Oksenberg JR. The neurobiology of multiple sclerosis: genes, inflammation, and neurodegeneration. Neuron. 2006;52:61–76.
Trapp BD, Nave KA. Multiple sclerosis: an immune or neurodegenerative disorder? Annu Rev Neurosci. 2008;31:247–69.
Goverman J. Autoimmune T cell responses in the central nervous system. Nat Rev Immunol. 2009;9:393–407.
Muramatsu R, Kubo T, Mori M, Nakamura Y, Fujita Y, Akutsu T, Okuno T, Taniguchi J, Kumanogoh A, Yoshida M, et al. RGMa modulates T cell responses and is involved in autoimmune encephalomyelitis. Nat Med. 2011;17:488–94.
Tanabe S, Yamashita T. Repulsive guidance molecule-a is involved in Th17-cell-induced neurodegeneration in autoimmune encephalomyelitis. Cell Rep. 2014;9:1459–70.
Sospedra M, Martin R. Immunology of multiple sclerosis. Annu Rev Immunol. 2005;23:683–747.
Becher B, Durell BG, Noelle RJ. Experimental autoimmune encephalitis and inflammation in the absence of interleukin-12. J Clin Invest. 2002;110:493–7.
Bettelli E, Carrier Y, Gao W, Korn T, Strom TB, Oukka M, Weiner HL, Kuchroo VK. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441:235–8.
Hu Y, Ota N, Peng I, Refino CJ, Danilenko DM, Caplazi P, Ouyang W. IL-17RC is required for IL-17A- and IL-17F-dependent signaling and the pathogenesis of experimental autoimmune encephalomyelitis. J Immunol. 2010;184:4307–16.
Komiyama Y, Nakae S, Matsuki T, Nambu A, Ishigame H, Kakuta S, Sudo K, Iwakura Y. IL-17 plays an important role in the development of experimental autoimmune encephalomyelitis. J Immunol. 2006;177:566–73.
McGeachy MJ, Chen Y, Tato CM, Laurence A, Joyce-Shaikh B, Blumenschein WM, McClanahan TK, O'Shea JJ, Cua DJ. The interleukin 23 receptor is essential for the terminal differentiation of interleukin 17-producing effector T helper cells in vivo. Nat Immunol. 2009;10:314–24.
Nohra R, Beyeen AD, Guo JP, Khademi M, Sundqvist E, Hedreul MT, Sellebjerg F, Smestad C, Oturai AB, Harbo HF, et al. RGMA and IL21R show association with experimental inflammation and multiple sclerosis. Genes Immun. 2010;11:279–93.
Girolamo F, Coppola C, Ribatti D, Trojano M. Angiogenesis in multiple sclerosis and experimental autoimmune encephalomyelitis. Acta Neuropathol Commun. 2014;2:84.
Kirk S, Frank JA, Karlik S. Angiogenesis in multiple sclerosis: is it good, bad or an epiphenomenon? J Neurol Sci. 2004;217:125–30.
Putnam TJ. The pathogenesis of multiple sclerosis: a possible vascular factor. N Engl J Med. 1933;209:786–90.
Jin K, Zhu Y, Sun Y, Mao XO, Xie L, Greenberg DA. Vascular endothelial growth factor (VEGF) stimulates neurogenesis in vitro and in vivo. Proc Natl Acad Sci U S A. 2002;99:11946–50.
Hayakawa K, Pham LD, Som AT, Lee BJ, Guo S, Lo EH, Arai K. Vascular endothelial growth factor regulates the migration of oligodendrocyte precursor cells. J Neurosci. 2011;31:10666–70.
Muramatsu R, Takahashi C, Miyake S, Fujimura H, Mochizuki H, Yamashita T. Angiogenesis induced by CNS inflammation promotes neuronal remodeling through vessel-derived prostacyclin. Nat Med. 2012;18:1658–64.
Harada K, Fujita Y, Yamashita T. Repulsive guidance molecule A suppresses angiogenesis. Biochem Biophys Res Commun. 2016;469:993–9.
Lejmi E, Leconte L, Pedron-Mazoyer S, Ropert S, Raoul W, Lavalette S, Bouras I, Feron JG, Maitre-Boube M, Assayag F, et al. Netrin-4 inhibits angiogenesis via binding to neogenin and recruitment of Unc5B. Proc Natl Acad Sci U S A. 2008;105:12491–6.
Park KW, Crouse D, Lee M, Karnik SK, Sorensen LK, Murphy KJ, Kuo CJ, Li DY. The axonal attractant netrin-1 is an angiogenic factor. Proc Natl Acad Sci U S A. 2004;101:16210–5.
Wilson BD, Ii M, Park KW, Suli A, Sorensen LK, Larrieu-Lahargue F, Urness LD, Suh W, Asai J, Kock GA, et al. Netrins promote developmental and therapeutic angiogenesis. Science. 2006;313:640–4.
Nguyen A, Cai H. Netrin-1 induces angiogenesis via a DCC-dependent ERK1/2-eNOS feed-forward mechanism. Proc Natl Acad Sci U S A. 2006;103:6530–5.
Lu X, Le Noble F, Yuan L, Jiang Q, De Lafarge B, Sugiyama D, Breant C, Claes F, De Smet F, Thomas JL, et al. The netrin receptor UNC5B mediates guidance events controlling morphogenesis of the vascular system. Nature. 2004;432:179–86.
Larrivee B, Freitas C, Trombe M, Lv X, Delafarge B, Yuan L, Bouvree K, Breant C, Del Toro R, Brechot N, et al. Activation of the UNC5B receptor by netrin-1 inhibits sprouting angiogenesis. Genes Dev. 2007;21:2433–47.
Acknowledgements
We are grateful to all the Yamashita’s lab members for the critical discussions.
Funding
This work was supported by funding to TY from the Practical Research Project for Rare/Intractable Diseases from the Japan Agency for Medical Research and Development (AMED).
Availability of data and materials
Not applicable.
Authors’ contributions
YF and TY wrote the manuscript. Both authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Yes
Ethics approval and consent to participate
Not applicable
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Fujita, Y., Yamashita, T. The roles of RGMa-neogenin signaling in inflammation and angiogenesis. Inflamm Regener 37, 6 (2017). https://doi.org/10.1186/s41232-017-0037-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41232-017-0037-6