Abstract
Background
Several studies have shown that normal weight central obesity (NWCO) is associated with cardiovascular disease (CVD) risk factors. However, studies conducted in the Japanese population have been very limited. Thus, the relationships between normal weight central obesity, classified using body mass index (BMI), the waist-to-height ratio (WHtR), and CVD risk factors in middle-aged Japanese adults were investigated.
Methods
The participants were Japanese adults aged 40–64 years who had undergone periodic health examinations in Japan during the period from April 2013 to March 2014. The participants were categorized into the following four groups: normal weight (BMI 18.5–24.9 kg/m2) and no central obesity (WHtR < 0.5) (NW); normal weight and central obesity (WHtR ≥ 0.5) (NWCO); obesity (BMI ≥ 25 kg/m2) and no central obesity (OB); and obesity and central obesity (OBCO). Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or taking medication for hypertension. Dyslipidemia was defined as LDL-C ≥ 140 mg/dl, HDL-C < 40 mg/dl, triglyceride ≥ 150 mg/dl, or taking medication for dyslipidemia. Diabetes was defined as fasting plasma glucose ≥ 126 mg/dl, random plasma glucose ≥ 200 mg/dl, HbA1c ≥ 6.5%, or receiving medical treatment for diabetes mellitus. A logistic regression model was used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) for hypertension, dyslipidemia, and diabetes.
Results
A total of 117,163 participants (82,487 men and 34,676 women) were analyzed. The prevalence of NWCO was 15.6% in men and 30.2% in women. With reference to NW, the ORs for hypertension (adjusted OR 1.22, 95% CI 1.17–1.27 in men, 1.23, 1.16–1.31 in women), dyslipidemia (1.81, 1.74–1.89 in men, 1.60, 1.52–1.69 in women), and diabetes (1.35, 1.25–1.46 in men, 1.60, 1.35–1.90 in women) were significantly higher in NWCO.
Conclusions
Normal weight with central obesity was associated with CVD risk factors, such as hypertension, dyslipidemia, and diabetes, compared with normal weight without central obesity, regardless of sex. It is important to focus on normal weight with central obesity for the prevention of CVD in Japanese middle-aged adults.
Similar content being viewed by others
Background
In the general population, obesity is consistently and strongly related to higher risks of cardiovascular disease (CVD) incidence and death [1]. By contrast, a recent study showed that abdominal obesity is associated with insulin resistance and higher risks of metabolic syndrome and CVD, whereas general obesity is not [2]. Moreover, “normal weight central obesity,” defined by considering general obesity and central obesity, has been shown to be associated with CVD risk factors and increased mortality [3]. Thus, it can be effective to consider both general obesity and central obesity for prevention of CVD.
General obesity is most commonly assessed using the body mass index (BMI) [4]. Although the BMI is strongly correlated with gold standard body fat measures, it cannot distinguish between lean and fat mass and provides no indication of body fat distribution [4]. By contrast, abdominal obesity is assessed using indicators such as waist circumference (WC), waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR) [5]. A previous systematic review demonstrated that, as indices of abdominal obesity, the WHtR was a better predictor than BMI and WC for diabetes, dyslipidemia, hypertension, and CVD in both sexes in populations of various nationalities [6]. The WHtR may be a simpler and better predictor of early health risks [7,8,9]. Thus, it is effective to use BMI and the WHtR for defining general obesity and central obesity.
Several studies reported that normal weight central obesity defined by BMI and WHR [10,11,12], body fat percentage [13, 14], and WC [15,16,17] were associated with CVD risk factors. By contrast, there were a few studies regarding the association of normal weight central obesity defined by BMI and WHtR with CVD risk factors [18,19,20]. Moreover, to the best of our knowledge, studies conducted in the Japanese population have been very limited.
Accordingly, the aim of the present study was to investigate the prevalence of normal weight central obesity classified using BMI and the WHtR and to examine the relationships between normal weight with central obesity and CVD risk factors, especially hypertension, dyslipidemia, and diabetes, in middle-aged Japanese adults. We hypothesized that, in Japanese men and women, those with normal weight and central obesity have a higher risk of CVD risk factors compared with those with normal weight and no central obesity or obesity with no central obesity.
Methods
Subjects and setting
The subjects of this study were Japanese men and women aged 40–64 years who had undergone periodic health examinations provided by the All Japan Labor Welfare Foundation (Tokyo), a health service center in Japan, during the period from April 2013 to March 2014. Written, informed consent was obtained from the subjects. The study protocol was approved by the Medical Ethics Committee of Showa University School of Medicine (Approval No. 2132) and the Ethics Committee of the All Japan Labor Welfare Foundation (Approval No. 3-1-0004).
Variables and their measurement
The following information was obtained from each subject using a self-administered questionnaire, which was recommended for specific health examination by the Japanese government (Ministry of Health, Labour and Welfare) [21]: age, sex, smoking status (current smoker, ex-smoker, non-smoker), alcohol intake (daily, sometimes, none), and physical activity equal to walking at least 60 min per day (yes, no).
Height and weight were measured in increments of 0.1 cm and 0.1 kg, respectively, by trained staff. BMI was calculated as the weight (kg) divided by the squared height (m2). WC was measured to the nearest 0.1 cm at the umbilical level in a standing position [22]. The WHtR was calculated as WC divided by height. Blood pressure in the sitting position was measured using an automated machine (HEM-907, Omron, Kyoto, Japan).
Venous blood samples were drawn from the study subjects to measure serum levels of high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides, blood glucose, and hemoglobin A1c (HbA1c). The samples were stored in a cooler at 4 °C for transportation to at an external laboratory (SRL, Tokyo, Japan) and measured within 24 h of being drawn. HDL-C and LDL-C were determined by a direct method, while the triglyceride level was measured by an enzyme method (AU5400, BECKMAN COULTER, Brea, CA, USA). The blood glucose level was obtained by the hexokinase method (AU5400, BECKMAN COULTER), while HbA1c was measured by a latex agglutination method (JCA-BM9130, JEOL, Tokyo, Japan).
Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or taking medication for hypertension [23]. Dyslipidemia was defined as LDL-C ≥ 140 mg/dl, HDL-C < 40 mg/dl, triglycerides ≥ 150 mg/dl, or taking medication for dyslipidemia [24]. Diabetes was defined as fasting plasma glucose (≥ 8 h after the last caloric intake) ≥ 126 mg/dl, random plasma glucose ≥ 200 mg/dl, HbA1c (National Glycohemoglobin Standardization Program) ≥ 6.5%, or receiving medical treatment for diabetes mellitus [25, 26].
Definition of normal weight central obesity
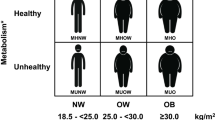
BMI was categorized into three groups: < 18.5 (underweight), 18.5–24.9 (normal weight), and ≥ 25 kg/m2 (obesity) [27]. WHtR was dichotomized as follows: < 0.5 (no central obesity) and ≥ 0.5 (central obesity) [28, 29]. Moreover, according to previous studies [19, 20], the subjects were categorized into the following four groups: normal weight and no central obesity (NW); normal weight and central obesity (NWCO); obesity and no central obesity (OB); and obesity and central obesity (OBCO). In the present study, underweight subjects (BMI < 18.5 kg/m2) were excluded from the analysis.
Statistical analysis
The Kruskal-Wallis test or chi-squared test was used to compare the characteristics among the four groups (NW, NWCO, OB, and OBCO) for each sex. In the analysis stratified by sex, a logistic regression model was used to calculate the odds ratios (ORs) and the 95% confidence intervals (CIs) for hypertension, dyslipidemia, and diabetes. In the model, age, weight, smoking status, alcohol intake, and physical activity were included to control for potential confounding factors [19].
In this study, a P value of less than 0.05 was considered significant. All data were analyzed using JMP version 13.0 (SAS Institute Japan Co., Ltd., Tokyo, Japan).
Results
Of the 310,577 subjects, 310,498 participated in this study. From among these participants, 185,430 participants with missing data and 7905 participants who were underweight (BMI < 18.5 kg/m2) were excluded. Thus, a total of 117,163 participants (82,487 men and 34,676 women) were analyzed.
The median WC was higher in men than in women, whereas the median WHtR was higher in women than in men (Table 1). The proportions of NW, NWCO, OB, and OBCO were 50.8%, 19.9%, 1.6%, and 27.7%. The proportions were 52.2%, 15.6%, 2.1%, and 30.1% in men and 47.6%, 30.2%, 0.3%, and 21.8% in women, respectively.
The characteristics of the four groups classified by BMI and WHtR (NW, NWCO, OB, and OBCO) are shown in Table 2 for men and Table 3 for women. The prevalences of hypertension, dyslipidemia, and diabetes in OBCO were 48.9%, 68.9%, and 16.2% in men and 43.8%, 57.6%, and 11.0% in women, respectively. The prevalences of hypertension, dyslipidemia, and diabetes were higher in OBCO than in NW, NWCO, and OB, regardless of sex. The prevalences in NWCO were 39.6%, 60.1%, and 9.6% in men and 31.0%, 48.4%, and 3.6% in women, respectively. The participants with NWCO had higher prevalences of hypertension, dyslipidemia, and diabetes than those with NW, regardless of sex.
Next, logistic regression analysis was conducted to calculate the crude and adjusted ORs for hypertension, dyslipidemia, and diabetes and their 95% CIs in each sex (Table 4 for men and Table 5 for women). When compared with NW, the adjusted ORs for hypertension (adjusted OR 1.58, 95% CI 1.51–1.65 in men; 1.55, 1.43–1.69 in women), dyslipidemia (1.84, 1.76–1.93 in men; 1.85, 1.70–2.01 in women), and diabetes (1.83, 1.70–1.97 in men; 3.11, 2.57–3.77 in women) were significantly increased in OBCO, regardless of sex. With reference to NW, the ORs for hypertension (1.22, 1.17–1.27 in men; 1.23, 1.16–1.31 in women), dyslipidemia (1.81, 1.74–1.89 in men; 1.60, 1.52–1.69 in women), and diabetes (1.35, 1.25–1.46 in men; 1.60, 1.35–1.90 in women) were significantly increased in NWCO.
Discussion
In our study, the prevalence of NWCO defined using a combination of BMI and WHtR was 19.9%. The prevalence was higher than the reported NWCO prevalence in Thailand (15.4%) [20], whereas it was lower than that in South Africa (29.5%) [19]. One of the reasons could be the difference in the BMI cut-off level. The cut-off level in the Thai study was BMI < 25.0 kg/m2, and thus underweight subjects were included in the normal weight group. Moreover, in the South African study, the method for measurement of WC was different from that of the present study. WC in this study was measured at the umbilical level in a standing position [20], while it was measured at the level of the narrowest point between the lower costal border and the iliac crest in the South African study [19]. Therefore, the differences in the BMI cut-off level and the method of WC measurement might have affected the prevalence of NWCO.
In the present study, the prevalence of NWCO was higher in women than in men (30.2% vs. 15.6%). One possible explanation for the result might be that, in the present study, the proportion of normal weight was higher in women than in men (77.8% vs. 67.8%), and the proportion of central obesity was higher in women than in men (52.0% vs. 45.7%). However, the result that women had a higher prevalence of NWCO than men is not consistent with previous studies [18, 22]. Future studies will be needed to elucidate the sex differences in the prevalence of NWCO.
Normal weight with central obesity was associated with CVD risks such as hypertension, dyslipidemia, and diabetes in the present study; the ORs for hypertension, dyslipidemia, and diabetes were significantly increased in NWCO, as well as in OBCO, compared with NW, regardless of sex. These results were consistent with previous studies [18, 20, 30]. The present study suggested that using a combination of measures, including a measure of general obesity and a measure of central obesity, would be more appropriate in identifying CVD risk factors. Thus, the findings of the present study suggest that those who are NWCO need to be screened like those who are OBCO. Because these individuals with NWCO are considered normal weight, namely non-overweight/obesity, they do not usually receive the appropriate health education and prompt intervention to prevent the CVD risk factors. Moreover, a previous study reported that WHtR and BMI are independently associated with CVD risk [31]. Therefore, it is important to conduct screening for NWCO using a combination of BMI and WHtR [7,8,9] and intervene actively to prevent CVD risks such as hypertension, diabetes, and dyslipidemia.
To the best of our knowledge, this is the first study to investigate the prevalence of normal weight with central obesity and to examine the relationships between normal weight with central obesity classified using BMI and WHtR and CVD risk factors (especially hypertension, dyslipidemia, and diabetes) in middle-aged adults in Japan. A strength of the present study was the large sample size (over 110,000 participants), which contributed to a decrease in random error. Moreover, height, weight, and WC of study participants were measured by trained technicians, and these anthropometric variables were used to define obesity and central obesity. By contrast, some limitations of the present study should be noted. First, potential confounding factors that were not obtained in the present study might have affected the study’s findings. For instance, the information on dietary intake [32] and socioeconomic status [16], which has been reported to be associated with CVD risk factors, was not collected. Second, the study design was cross-sectional, which makes it difficult to examine causal relationships. Thus, further studies, including prospective studies, will be needed to establish causality.
Conclusions
In conclusion, the present study showed that normal weight with central obesity was associated with CVD risk factors, such as hypertension, dyslipidemia, and diabetes, compared with normal weight without central obesity, regardless of sex. The present findings suggest that it is important to focus on normal weight with central obesity defined using a combination of BMI and WHtR to prevent CVD in Japanese middle-aged adults.
Availability of data and materials
The data used for this study are available on reasonable request and only after approval by the Ethics Committee of the All Japan Labor Welfare Foundation.
Abbreviations
- 95% CI:
-
95% confidence interval
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- HbA1c:
-
Hemoglobin A1c
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- NW:
-
Normal weight and no central obesity
- NWCO:
-
Normal weight and central obesity
- OB:
-
Obesity and no central obesity
- OBCO:
-
Obesity and central obesity
- ORs:
-
Odds ratios
- WC:
-
Waist circumference
- WHR:
-
Waist-to-hip ratio
- WHtR:
-
Waist-to-height ratio
References
Ortega FB, Lavie CJ, Blair SN. Obesity and cardiovascular disease. Circ Res. 2016. https://doi.org/10.1161/circresaha.115.306883.
Goh VHH, Hart WG. Excess fat in the abdomen but not general obesity is associated with poorer metabolic and cardiovascular health in premenopausal and postmenopausal Asian women. Maturitas. 2018. https://doi.org/10.1016/j.maturitas.2017.10.002.
Oliveros E, Somers VK, Sochor O, Goel K, Lopez-Jimenez F. The concept of normal weight obesity. Prog Cardiovasc Dis. 2014. https://doi.org/10.1016/j.pcad.2013.10.003.
Adab P, Pallan M, Whincup PH. Is BMI the best measure of obesity? BMJ. 2018. https://doi.org/10.1136/bmj.k1274.
Wiltink J, Michal M, Wild PS, Zwiener I, Blettner M, Munzel T, et al. Associations between depression and different measures of obesity (BMI, WC, WHtR, WHR). BMC Psychiatry. 2013. https://doi.org/10.1186/1471-244x-13-223.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012. https://doi.org/10.1111/j.1467-789X.2011.00952.x.
Ashwell M, Gibson S. Waist-to-height ratio as an indicator of ‘early health risk’: simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open. 2016. https://doi.org/10.1136/bmjopen-2015-010159.
Hori A, Nanri A, Sakamoto N, Kuwahara K, Nagahama S, Kato N, et al. Comparison of body mass index, waist circumference, and waist-to-height ratio for predicting the clustering of cardiometabolic risk factors by age in Japanese workers--Japan Epidemiology Collaboration on Occupational Health study. Circ J. 2014;78:1160–8.
Hsieh SD, Muto T. Metabolic syndrome in Japanese men and women with special reference to the anthropometric criteria for the assessment of obesity: proposal to use the waist-to-height ratio. Prev Med. 2006. https://doi.org/10.1016/j.ypmed.2005.08.007.
Sahakyan KR, Somers VK, Rodriguez-Escudero JP, Hodge DO, Carter RE, Sochor O, et al. Normal-weight central obesity: implications for total and cardiovascular mortality. Ann Intern Med. 2015. https://doi.org/10.7326/m14-2525.
Sharma S, Batsis JA, Coutinho T, Somers VK, Hodge DO, Carter RE, et al. Normal-weight central obesity and mortality risk in older adults with coronary artery disease. Mayo Clin Proc. 2016. https://doi.org/10.1016/j.mayocp.2015.12.007.
Coutinho T, Goel K, Correa de Sa D, Carter RE, Hodge DO, Kragelund C, et al. Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease: role of “normal weight central obesity”. J Am Coll Cardiol. 2013. https://doi.org/10.1016/j.jacc.2012.10.035.
Jia A, Xu S, Xing Y, Zhang W, Yu X, Zhao Y, et al. Prevalence and cardiometabolic risks of normal weight obesity in Chinese population: a nationwide study. Nutr Metab Cardiovasc Dis. 2018. https://doi.org/10.1016/j.numecd.2018.06.015.
Kim MK, Han K, Kwon HS, Song KH, Yim HW, Lee WC, et al. Normal weight obesity in Korean adults. Clin Endocrinol (Oxf). 2014. https://doi.org/10.1111/cen.12162.
Du T, Sun X, Yin P, Huo R, Ni C, Yu X. Increasing trends in central obesity among Chinese adults with normal body mass index, 1993-2009. BMC Public Health. 2013. https://doi.org/10.1186/1471-2458-13-327.
Zhang P, Wang R, Gao C, Jiang L, Lv X, Song Y, et al. Prevalence of central obesity among adults with normal BMI and its association with metabolic diseases in Northeast China. PLoS One. 2016. https://doi.org/10.1371/journal.pone.0160402.
Tanamas SK, Permatahati V, Ng WL, Backholer K, Wolfe R, Shaw JE, et al. Estimating the proportion of metabolic health outcomes attributable to obesity: a cross-sectional exploration of body mass index and waist circumference combinations. BMC Obes. 2015. https://doi.org/10.1186/s40608-016-0085-5.
Ashwell M, Gibson S. Waist to height ratio is a simple and effective obesity screening tool for cardiovascular risk factors: analysis of data from the British National Diet And Nutrition Survey of adults aged 19-64 years. Obes Facts. 2009. https://doi.org/10.1159/000203363.
Owolabi EO, Ter Goon D, Adeniyi OV. Central obesity and normal-weight central obesity among adults attending healthcare facilities in Buffalo City Metropolitan Municipality, South Africa: a cross-sectional study. J Health Popul Nutr. 2017. https://doi.org/10.1186/s41043-017-0133-x.
Thaikruea L, Thammasarot J. Prevalence of normal weight central obesity among Thai healthcare providers and their association with CVD risk: a cross-sectional study. Sci Rep. 2016. https://doi.org/10.1038/srep37100.
Nagahama S, Kurotani K, Pham NM, Nanri A, Kuwahara K, Dan M, et al. Self-reported eating rate and metabolic syndrome in Japanese people: cross-sectional study. BMJ Open. 2014. https://doi.org/10.1136/bmjopen-2014-005241.
Hsieh SD, Yoshinaga H, Muto T. Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes Relat Metab Disord. 2003. https://doi.org/10.1038/sj.ijo.0802259.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014. https://doi.org/10.1038/hr.2014.20.
Teramoto T, Sasaki J, Ishibashi S, Birou S, Daida H, Dohi S, et al. Executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan -2012 version. J Atheroscler Thromb. 2013;20:517–23.
Nanri A, Nakagawa T, Kuwahara K, Yamamoto S, Honda T, Okazaki H, et al. Development of risk score for predicting 3-year incidence of type 2 diabetes: Japan epidemiology collaboration on occupational health study. PLoS One. 2015. https://doi.org/10.1371/journal.pone.0142779.
Kabeya Y, Kato M, Isogawa A, Takahashi Y, Matsushita Y, Goto A, et al. Descriptive epidemiology of diabetes prevalence and HbA1c distributions based on a self-reported questionnaire and a health checkup in the JPHC diabetes study. J Epidemiol. 2014;24:460–8.
Organization WH. World Health Organization. Body mass index - BMI. 2018. http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Accessed 11.29 2018.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010. https://doi.org/10.1017/s0954422410000144.
Wakabayashi I. Necessity of both waist circumference and waist-to-height ratio for better evaluation of central obesity. Metab Syndr Relat Disord. 2013. https://doi.org/10.1089/met.2012.0131.
Lam BC, Koh GC, Chen C, Wong MT, Fallows SJ. Comparison of body mass index (BMI), body adiposity index (BAI), waist circumference (WC), waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) as predictors of cardiovascular disease risk factors in an adult population in Singapore. PLoS One. 2015. https://doi.org/10.1371/journal.pone.0122985.
Tatsumi Y, Watanabe M, Kokubo Y, Nishimura K, Higashiyama A, Okamura T, et al. Effect of age on the association between waist-to-height ratio and incidence of cardiovascular disease: the Suita study. J Epidemiol. 2013;23:351–9.
Gonzalez-Rodriguez LG, Perea Sanchez JM, Aranceta-Bartrina J, Gil A, Gonzalez-Gross M, Serra-Majem L, et al. Intake and dietary food sources of fibre in spain: differences with regard to the prevalence of excess body weight and abdominal obesity in adults of the ANIBES study. Nutrients. 2017. https://doi.org/10.3390/nu9040326.
Acknowledgements
The authors would like to thank all study participants and Dr. Nobuo Yanagisawa, Dr. Takeshi Kawaguchi, Mr. Takahiro Tamura, and Mr. Yutaka Hoshina at the All Japan Labor Welfare Foundation for supporting the study.
Funding
This study was supported in part by a grant from the Ministry of Education, Culture, Sports, Science and Technology of Japan (Basic Research (C), #17 K09130, 2017–2019).
Author information
Authors and Affiliations
Contributions
TS, HO, and TY contributed to the study design, interpretation of data, and manuscript preparation. TS conducted the statistical analysis and drafted this manuscript. SN and MK contributed to the acquisition of data. IO and YS contributed to the data interpretation. HO and TY supported drafting the manuscript. AK made substantial contributions to the conception of this study and project administration. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Medical Ethics Committee of Showa University School of Medicine (Approval No. 2132) and the Ethics Committee of the All Japan Labor Welfare Foundation (Approval No. 3-1-0004). Informed consent for the use of personal information was obtained from each participant in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Shirasawa, T., Ochiai, H., Yoshimoto, T. et al. Associations between normal weight central obesity and cardiovascular disease risk factors in Japanese middle-aged adults: a cross-sectional study. J Health Popul Nutr 38, 46 (2019). https://doi.org/10.1186/s41043-019-0201-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-019-0201-5