Abstract
Background
Anthracycline chemotherapy and thoracic radiation therapy (RT) are known causes of cardiomyopathy among cancer survivors, however, management guidelines for this population are lacking. In this study we describe our single institution management approach for cancer survivors with low left ventricular ejection fraction (LVEF) secondary to cancer treatment.
Methods
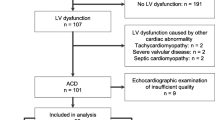
We conducted a retrospective descriptive study of childhood and young adult (CAYA) cancer survivors in the Adult Long-Term Follow-Up Clinic at Memorial Sloan Kettering Cancer Center enrolled between November 2005 and July 2019. Those included were treated with anthracycline and/or thoracic RT as a part of their cancer therapy and had recorded a LVEF of < 55% on at least one post-treatment echocardiogram. Details regarding survivor characteristics, screening, and management were abstracted. Differences in management approaches among survivors with LVEF of 50–54.9%, 40–49.9%, and < 40% were described. Qualitative management approaches were abstracted as well.
Results
Among 668 CAYA survivors in the initial cohort, 80 were identified who had received anthracycline and/or thoracic RT and had a LVEF of < 55%. Median age at cancer diagnosis was 16.1 years, median time from cancer diagnosis was 25.8 years, and 55% of survivors were female. Cardiology referrals, nuclear stress tests, multi-gated acquisition scans, angiograms, echocardiograms, treatment with angiotensin converting enzyme inhibitors or receptor blockers, beta-blockers, diuretics, aldosterone antagonists, aspirin, and insertion of pacemaker or implantable cardioverter-defibrillators differed by LVEF category. Documentation suggested uncertainty regarding management of survivors with borderline low-LVEF, with low-LVEF that improved on follow-up, and with subsequent cancers requiring additional treatment.
Conclusions
The management of CAYA cancer survivors with low-LVEF largely followed guidelines designed for the general population, however, uncertainty remains for issues specific to cancer survivors. Cardiomyopathy management guidelines that address issues specific to cancer survivors are needed.
Similar content being viewed by others
Introduction
Five-year survival rates for childhood, adolescent, and young adult (CAYA) cancer have increased from 58% in the mid-1970s to well over 80% in the past decade [1], helping to avert an estimated 38 032 cancer deaths from 1975 to 2006 [2]. It is estimated that there are nearly 400 000 survivors of childhood and adolescent cancer in the United States [3]. As more of these children live on to adulthood, cancer survivor health is an increasingly relevant aspect of healthcare. Cancer survivors have a higher risk of many chronic health conditions, including joint problems, infertility, hearing and vision loss, cognitive dysfunction, secondary cancers [4, 5], and cardiac problems – especially as a result of anthracycline chemotherapy or thoracic radiation therapy (RT) [5,6,7].
About 60% of CAYA survivors have been exposed to anthracyclines and/or thoracic RT as a part of their treatment [5]. Cardiac complications associated with these therapies are largely dependent on cumulative dose and time since treatment, with a relative hazard of up to six times that of siblings [8]. Several organizations, including the Children’s Oncology Group [9] and European Society of Cardiology (ESC) [10], provide guidelines for detecting cardiomyopathy in this population, with recommendations that include serial echocardiography [11]. However, once heart problems are detected, management guidelines for low left ventricular ejection fraction (LVEF) or cardiomyopathy specific to cancer survivors are lacking [12,13,14]. The ESC does recommend angiotensin converting enzyme inhibitors or receptor blockers (ACEI/ARB) in combination with beta-blockers in cancer survivors with symptomatic or asymptomatic cardiac dysfunction (unless contraindicated) but do not provide recommendations on other treatments [10]. A study using Delphi methodology querying physicians for their management approach of these survivors elucidated on this uncertainty, finding agreement in some areas (echocardiogram and ECG screening frequency, exercise promotion, referrals to cardiology, and use of ACEI) and disagreement in other areas (use of other cardiac testing, frequency of screening during pregnancy, and use of beta-blockers) [15].
In this retrospective descriptive study, we obtain data from the Memorial Sloan Kettering (MSK) Adult Long-Term Follow-Up Program to describe approaches for monitoring and managing low-LVEF in CAYA cancer survivors with a history of anthracycline chemotherapy and/or thoracic RT. For clarity, we categorized survivors by lowest LVEF on transthoracic echocardiogram, with a goal of elucidating how these survivors are managed and how everyday practice compares to guideline-concordant care for the general population [12, 13].
Methods
Study Population
Our study population consists of CAYA cancer survivors enrolled in the MSK Adult Long-Term Follow-Up Program enrolled between November 2005 and July 2019. The MSK Adult Long-Term Follow-Up Program delivers longitudinal risk-based health care, including management of late effects, for adults who had their first primary malignancy prior to age 40 and who are at risk for late effects or have multiorgan complications following cancer therapy [16]. Survivors must be over 18 and finished with therapy to be followed in the clinic. Screening and surveillance for late effects occurs during an annual visit. In accordance with the COG guidelines [9], an annual cardiac exam is performed including medical history and blood pressure recordings, as well as echocardiograms at intervals based on anthracycline and thoracic RT dose. From the initial cohort, survivors who received anthracycline and/or thoracic RT as part of their cancer treatment and had a lowest LVEF of < 55% on echocardiogram were identified.
Main outcomes and measures
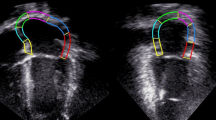
Patient characteristics, such as demographics, cancer diagnoses, comorbidities, and treatment details including anthracycline doses (converted to doxorubicin equivalents) [17] and thoracic RT doses were recorded. Detailed measures from the echocardiogram with the lowest recorded LVEF were obtained, including fractional shortening, left ventricular wall thickness, left atrial size, and valvular disease. Other heart health outcomes such as coronary artery disease, congestive heart failure, and myocardial infarction were obtained from patient charts. Additional cardiac monitoring was abstracted as well, including subsequent echocardiograms, ECGs, Holter monitors, stress tests, multi-gated acquisition (MUGA) scans, cardiac MRIs, and angiograms. Treatments provided, including medications such as ACEI/ARB, beta-blockers, diuretics, aldosterone antagonists, statins, and aspirin were obtained, as well as information on surgical procedures such as pacemaker or implantable cardioverter-defibrillator (ICD) placement, stent placement, valve replacement, and coronary artery bypass. Lastly, qualitative information on assessments and plans were also obtained to elucidate on the medical management of this unique patient population.
Results were stratified into three lowest recorded LVEF categories: < 41%, 41–49.9%, and 50–54.9%, which were informed by American Heart Association guidelines [13] representing survivors that have clearly reduced LVEF, are considered borderline, or may need additional cardiac monitoring, respectively.
Results
Overview
Among 668 survivors who received anthracycline chemotherapy and/or thoracic RT, 80 (12.0%) had a lowest recorded LVEF of < 55%. Of these 80 survivors, 70 (87.5%) were non-Hispanic White and 36 (45.0%) were male. The most common primary cancer types represented were 31 (38.8%) with Hodgkin’s lymphoma, 26 (32.5%) with sarcoma, and 12 (15.0%) with non-Hodgkin’s lymphoma. Seventy-three (91.3%) survivors received anthracycline chemotherapy and 49 (61.3%) received thoracic RT as part of their cancer treatment. Of those who received anthracycline chemotherapy, 10 (12.5%) received dexrazoxane as a cardioprotective measure. Fifty-seven (71.3%) were diagnosed before age 20, and 69 (86.3%) were living by the end of the follow-up period (Table 1). Survival status (P = 0.027), diabetes mellitus (P = 0.004), thoracic RT dose (P = 0.030), and use of dexrazoxane (P = 0.049) were significantly varied by group.
The mean lowest LVEF on echocardiogram was 44.7%. Twenty-four survivors (30%) had a lowest LVEF of < 41% and 6 (7.5%) had fractional shortening of < 20% on lowest LVEF echocardiogram. The most common valvular diseases included 24 (30.0%) with mitral regurgitation and 28 (35.0%) with tricuspid regurgitation. Twenty-three survivors (28.8%) had symptoms associated with low-LVEF, 21 (26.3%) were diagnosed with coronary artery disease, 14 (17.5%) were diagnosed with congestive heart failure, and 2 (2.5%) died of a cardiac complication by the end of the follow-up period (Table 2). Low fractional shortening (P < 0.001), left ventricular hypertrophy (P = 0.013), left atrial enlargement (P = 0.003), mitral regurgitation (P < 0.001), tricuspid regurgitation (P = 0.011), aortic regurgitation (P = 0.007), coronary artery disease (P = 0.033), and congestive heart failure (P < 0.001) were significantly varied by group.
Fifty-six survivors (70.0%) overall received a referral to a cardiologist, and 77 (96.3%) received additional cardiac testing after their lowest recorded LVEF. The most common subsequent testing included 71 (88.8%) with at least one ECG, 26 (32.5%) with at least one echocardiogram stress test, and 22 (27.5%) with at least one angiogram. Sixty-two (77.5%) survivors had echocardiogram intervals of 1 year, 12 (15.0%) with intervals of > 1 year, and 6 (7.5%) with intervals of < 1 year (Table 3). Cardiology referrals (P = 0.003), nuclear stress tests (P = 0.030), MUGA scans (P = 0.027), angiograms (P = 0.005), and shorter echocardiogram follow-up intervals (P < 0.001) were significantly varied by group. Mean LVEFs by prescribed cardiac monitoring ranged from 34.6% for nuclear stress tests to 46.6% for cardiac MRI (Fig. 1).
Fifty-one survivors (63.8%) were prescribed at least one cardiovascular medication. The most common medications represented included 37 (46.3%) who were prescribed ACEI/ARB, 30 (37.5%) who were prescribed beta-blockers, and 28 (35.0%) who were prescribed statins. Twelve (15.0%) survivors received at least one surgical intervention – with 11 (13.8%) receiving a pacemaker or ICD and 7 (8.8%) undergoing a valve replacement (Table 4). Receiving any medication (P < 0.001), specifically ACEI/ARB (P = 0.010), beta-blockers (P < 0.001), diuretics (P = 0.001), aldosterone antagonists (P = 0.015), or aspirin (P = 0.036) was significantly varied by group, as was receiving a pacemaker or ICD (P = 0.031). Mean LVEFs by prescribed cardiac medications ranged from 35.9% for aldosterone antagonists to 43.5% for statins. Mean LVEFs by surgical interventions ranged from 38.1% for pacemaker or ICDs to 46.5% for stent placement (Fig. 2).
<41% LVEF group
Survivors that fell into the < 41% LVEF group (N = 24) had a median lowest LVEF of 32.5% (IQR: 28.0–37.5) and a median time from diagnosis of 33.0 years (IQR: 23.8–42.4). This reflected a relatively longer follow-up time, a measure that was significantly varied by group (P = 0.002). These survivors were sicker overall, and were more likely to have left ventricular hypertrophy, left atrial enlargement, valvular disease, coronary artery disease, and congestive heart failure than other groups. Many of these survivors were symptomatic and were referred to and managed by a cardiologist, where follow-up intervals were as narrow as a few months. Some of these survivors were noted to see multiple cardiologists at outside institutions, often closer to their place of residence. Some received Holter monitors depending on the severity and characteristic of symptoms. Many survivors reported fatigue, chest pain, shortness of breath, and palpitations. Several survivors with advanced disease were hospitalized for cardiac symptoms. Diabetes mellitus was more prevalent in this group as well, and two died of cardiac complications during the follow-up period.
Some of the survivors in the < 41% LVEF group presented to acute care with cardiac symptoms, at times requiring admission to the cardiac intensive care unit and administration of inotropic agents. While the majority progressed gradually, the decision to treat these survivors was usually less ambiguous than it was for the two other low-LVEF groups. Treatments generally began with ACEI/ARB or beta-blockers. These survivors were more carefully consulted about the importance of exercise, diet, and electrolyte control. At least one patient struggled to keep up with care due to socioeconomic factors. All female survivors of reproductive age were advised to notify the medical team if they became pregnant. Another patient put off oral contraceptives as it complicated her blood pressure control. Further, cardiology input was solicited for survivors who developed subsequent cancers with regards to therapeutic options.
41–49.9% LVEF group
Survivors that fell into the 41–49.9% LVEF group (N = 18) had a median lowest LVEF of 46.5% (IQR: 44.3–48.0) and a median time from diagnosis of 26.3 years (IQR: 24.9–30.5). There was more heterogeneity in the presentation of disease among these survivors than among those in the lowest LVEF category. This variability may have contributed to a slightly higher utilization of additional cardiac testing, such as echocardiogram stress tests, pharmacological nuclear stress tests, MUGA scans, and angiograms.
In the setting of symptoms, treatments generally began once LVEF dropped below 50%, and was often titrated to maximum tolerable therapeutic doses. At times, however, treatment was put off if the patient was asymptomatic and further testing did not raise any concerns. Some survivors that initially presented to cardiology with symptoms and low-LVEF were later determined to be experiencing an acute episode, with a resolution of symptoms and improved LVEF thereafter. One patient in this group was diagnosed with low-LVEF at 22 weeks of pregnancy. This patient was given a Holter monitor, tested monthly with echocardiograms and for brain natriuretic peptide, given beta-blockers and diuretics as needed, and was referred to a high-risk obstetric medical group. Another patient was referred to cardiology specifically for determining whether amphetamines for attention deficient disorder was appropriate given his borderline low-LVEF. Further, several younger survivors described keeping up with their appointments and medications as stressful and getting in the way of living a normal life.
50–54.9% LVEF group
Survivors that fell into this category in our study had a median lowest LVEF of 52.5% (50.6–53.1) and a median time from diagnosis of 23.7 (15.5–31.0) years. These survivors were the least likely to be symptomatic (21.1%), most likely to have echocardiogram follow-up intervals of > 1 year (28.9%), and were the least likely to receive medications (42.1%) or surgical interventions (10.5%).
Preventative treatments such as ACEI/ARB or beta-blockers were implemented in 42.1% of these survivors. Because many of these survivors were young and did not have hypertension at baseline, doses were slowly titrated and discontinued if debilitating hypotensive symptoms presented. Like all groups, survivors were consulted on diet and exercise. Survivors not requiring immediate treatment were informed of their cardiac risk due to their cancer treatment and of the importance of long-term monitoring to detect potential issues.
Discussion
To our knowledge, this is the first study to describe management approaches for monitoring and treating low-LVEF among adult survivors of CAYA cancer with a history of anthracycline chemotherapy or thoracic RT. Qualitatively, we found that management approaches largely followed guidelines for low-LVEF in the general population. Several preventative and screening guidelines for this population are available in the literature, with a distinct lack of high-level evidence for treatments [11, 18]. As a result, clinicians often rely on guidelines from the American Heart Association and American College of Cardiology (AHA/ACC) or ESC, which are designed for the general population [12, 19]. However, considering the relative young age and high prevalence of both comorbidities and subsequent neoplasms in this population, general guidelines may not be adequate.
One notable difference we observed was the relatively low use of aldosterone antagonists including spironolactone (8.8%) – which was generally lower than other heart failure medications – despite compelling data supporting its use to decrease mortality [20]. It is possible that aldosterone antagonists’ hormonal side effects may have contributed to clinicians prescribing this class of medications less frequently than other heart failure medications in this young population. Spironolactone binds the androgen receptor and induces gynecomastia in men and amenorrhea in premenopausal women [20]. Newer aldosterone antagonists with less hormonal side effects have been introduced [20], however, some clinicians may be conditioned to avoid this class all-together in younger patients.
We observed ambiguity in the management of survivors with higher LVEFs. The 41–49.9% (borderline) LVEF group had highest rate of obtaining echocardiogram and pharmacological stress tests and MUGA scans, while the 50–54.9% LVEF group had the highest rate of receiving at least one test overall, ECGs, and cardiac MRIs – the latter of which provides similar information as echocardiograms (valve pathology, ejection fractions) but with better image quality, more accuracy, and higher cost [21]. This suggests that clinicians were searching for more evidence to inform their treatment decisions. The uncertainty among clinicians for managing these patients mirrors what has been reported for survivors with borderline LVEF in the general population, where firm evidence-based management guidelines are lacking [22]. That said, there is evidence that aldosterone antagonists [23, 24] and ARB [25] can reduce heart failure hospitalizations among those with borderline LVEF; future studies of their use in the survivorship setting are needed.
We also observed a subgroup of survivors who had low-LVEF as an acute episode around the time of treatment, with improved LVEF on subsequent echocardiograms. For asymptomatic survivors, medical records reflected uncertainty in management. Spontaneous improvement in LVEF has been reported in the general population, with the recommendation that patients be kept on the same medical regimen [26, 27]. However, recommendations for cancer survivors who may have had an acute low-LVEF episode – which is believed to manifest through a mechanism that is distinct from chronic cardiomyopathy – are sparse [28].
Lastly, we observed survivors who were under consideration for additional anthracycline and/or thoracic RT for a secondary cancer. For survivors with low-LVEF, clinicians in this study weighed the benefit that additional cancer therapy would provide with the risk that it may accelerate existing heart problems. For the general population, routine measurement of LVEF before the administration of anthracyclines is generally believed to have low utility, as low-LVEF is a relatively rare condition in otherwise healthy patients [29,30,31]. However, considering that childhood and young adult cancer survivors have a much higher risk of cardiac complications [8] with guidelines that recommend regular cardiac screenings [9], left ventricular function is extremely relevant. Still, with lack of specific recommendations, management of these survivors varies. Additional guidelines that consider a patient’s heart health and cancer burden when deciding to administer subsequent anthracyclines or thoracic RT would be useful.
Our analysis is limited as it only describes management practices at a single institution. Future research of management practices at other institutions could elucidate other problems unique to this population, ultimately providing the framework for future guidelines. Until these guidelines become available, cancer survivors with cardiomyopathy secondary to treatment should continue to be managed according to guidelines for the general population. Further, we have also found that enrollment in a specialized survivor clinic improves patient adherence to guideline-concordant care, a finding that has been shown by other institutions for screening [32]. Clinicians with experience dealing with issues unique to cancer survivors can help fill any gaps that current management guidelines may have.
Conclusion
In summary, our results suggest that the management of childhood and young adult cancer survivors with low-LVEF largely follows guidelines designed for the general population. However, uncertainty regarding treatment for survivors with borderline low-LVEF, those with acute episodes of low-LVEF, or those undergoing additional treatment for a subsequent malignancy continues to be a challenge for clinicians treating this high-risk population. Future research should consider a focus on these scenarios. We hope this single institution experience on common practice approaches can be used to inform future clinical trials and formal guidelines concerning best practices for cancer survivors with heart failure secondary to cancer treatment.
Availability of data and materials
Statistical code available upon request.
Change history
19 August 2022
A Correction to this paper has been published: https://doi.org/10.1186/s40959-022-00141-2
References
Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–85.
Smith MA, Seibel NL, Altekruse SF, et al. Outcomes for children and adolescents with cancer: challenges for the twenty-first century. J Clin Oncol. 2010;28(15):2625–34.
Phillips SM, Padgett LS, Leisenring WM, et al. Survivors of childhood cancer in the United States: prevalence and burden of morbidity. Cancer Epidemiol Biomarkers Prev. 2015;24(4):653–63.
Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–82.
Hudson MM, Ness KK, Gurney JG, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013;309(22):2371–81.
Berry GJ, Jorden M. Pathology of radiation and anthracycline cardiotoxicity. Pediatr Blood Cancer. 2005;44(7):630–7.
Sadurska E. Current Views on Anthracycline Cardiotoxicity in Childhood Cancer Survivors. Pediatr Cardiol. 2015;36(6):1112–9.
Mulrooney DA, Yeazel MW, Kawashima T, et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ. 2009;339:b4606.
Children's Oncology Group. Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. http://www.survivorshipguidelines.org/pdf/2018/COG_LTFU_Guidelines_v5.pdf. Published Version 5.0 - October 2018. Accessed.
Zamorano JL, Lancellotti P, Rodriguez Munoz D, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(36):2768–801.
Armenian SH, Hudson MM, Mulder RL, et al. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2015;16(3):e123-136.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147-239.
Trachtenberg BH, Landy DC, Franco VI, et al. Anthracycline-associated cardiotoxicity in survivors of childhood cancer. Pediatr Cardiol. 2011;32(3):342–53.
Kenney LB, Ames B, Margossian R, et al. Regional practice norms for the care of childhood cancer survivors at risk for cardiomyopathy: A Delphi study. Pediatr Blood Cancer. 2019;66(9):e27868.
Oeffinger KC, Hudson MM. Long-term complications following childhood and adolescent cancer: foundations for providing risk-based health care for survivors. CA Cancer J Clin. 2004;54(4):208–36.
Feijen EAM, Leisenring WM, Stratton KL, et al. Derivation of Anthracycline and Anthraquinone Equivalence Ratios to Doxorubicin for Late-Onset Cardiotoxicity. JAMA Oncol. 2019;5(6):864–71.
Conway A, McCarthy AL, Lawrence P, Clark RA. The prevention, detection and management of cancer treatment-induced cardiotoxicity: a meta-review. BMC Cancer. 2015;15:366.
Khakoo AY, Yeh ET. Therapy insight: Management of cardiovascular disease in patients with cancer and cardiac complications of cancer therapy. Nat Clin Pract Oncol. 2008;5(11):655–67.
Samuel JL, Delcayre C. Heart failure: aldosterone antagonists are underused by clinicians. Nat Rev Cardiol. 2010;7(3):125–7.
Gardner BI, Bingham SE, Allen MR, Blatter DD, Anderson JL. Cardiac magnetic resonance versus transthoracic echocardiography for the assessment of cardiac volumes and regional function after myocardial infarction: an intrasubject comparison using simultaneous intrasubject recordings. Cardiovasc Ultrasound. 2009;7:38.
Hsu JJ, Ziaeian B, Fonarow GC. Heart Failure With Mid-Range (Borderline) Ejection Fraction: Clinical Implications and Future Directions. JACC Heart Fail. 2017;5(11):763–71.
Solomon SD, Claggett B, Lewis EF, et al. Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure with preserved ejection fraction. Eur Heart J. 2016;37(5):455–62.
Pitt B, Pfeffer MA, Assmann SF, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.
Yusuf S, Pfeffer MA, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003;362(9386):777–81.
Gulati G, Udelson JE. Heart Failure With Improved Ejection Fraction: Is it Possible to Escape One’s Past? JACC Heart Fail. 2018;6(9):725–33.
Chavey WE. Ejection fraction is back to normal-now what? J Fam Pract. 2010;59(3):142–7.
Volkova M, Russell R 3rd. Anthracycline cardiotoxicity: prevalence, pathogenesis and treatment. Curr Cardiol Rev. 2011;7(4):214–20.
Peddi P, Master SR, Dwary AD, et al. Utility of routine pretreatment evaluation of left ventricular ejection fraction in breast cancer patients receiving anthracyclines. Breast J. 2019;25(1):62–8.
Enns DL, Mandelson MT, Aboulafia DM. Utility of Left Ventricular Ejection Fraction Measurements Before the Administration of Doxorubicin-Based Chemotherapy in Patients With Diffuse Large B-Cell Lymphoma. Mayo Clin Proc Innov Qual Outcomes. 2018;2(3):277–85.
Conrad AL, Gundrum JD, McHugh VL, Go RS. Utility of routine left ventricular ejection fraction measurement before anthracycline-based chemotherapy in patients with diffuse large B-cell lymphoma. J Oncol Pract. 2012;8(6):336–40.
Casagrande SS, McEwen LN, Herman WH. Changes in Health Insurance Coverage Under the Affordable Care Act: A National Sample of US Adults With Diabetes, 2009 and 2016. Diabetes Care. 2018;41(5):956–62.
Funding
This research was supported by the National Cancer Institute of the National Institute of Health; R25CA020449 and P30CA008748.
Author information
Authors and Affiliations
Contributions
Concept and design: All authors. Acquisition, analysis, or interpretation of data: Delavar, Boutros. Drafting of the manuscript: Delavar. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Delavar. Administrative, technical, or material support: All authors. Supervision: Tonorezos. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by Memorial Sloan Kettering Cancer Center committee on human research.
Consent for publication
Written informed consent for publication was obtained from all individual participants included in the study.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: author Wendy L. Schaffer's last name was written incorrectly.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Delavar, A., Boutros, C., Barnea, D. et al. Approaches for monitoring and treating cardiomyopathy among cancer survivors following anthracycline or thoracic radiation treatment. Cardio-Oncology 8, 11 (2022). https://doi.org/10.1186/s40959-022-00138-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40959-022-00138-x