Abstract
Objective
To assess the association between objective bladder function parameters in relation to urinary symptoms, and to analyze the sensitivity and specificity of subjective urinary symptom-assessment in predicting objective bladder dysfunction in a multiple sclerosis (MS) population.
Methods
Consecutive MS patients with Expanded Disability Status Score (EDSS) ≤7.0 were included in this prospective study. In a single visit, patients were evaluated for the presence of urinary symptoms, then assessed for the following urological parameters: maximum urinary flow rate (Qmax), postvoid residual urine volume (PVR), and detrusor sphincter dyssinergia (DSD).
Results
One hundred nine subjects were included with a mean disease duration of 12.5 ± 8.7 years, 90.8% had a relapsing-remitting course; the mean EDSS score was 2.6 ± 1.7. Overall, 53.5% complained of at least one urinary symptom, and the most reported one was urgency (40.7%), followed by frequency (15.7%) and incomplete emptying (12.0%). Abnormal values were found for Qmax in 34.9%, for PVR in 40.4% of participants; DSD was diagnosed in 33.9% of the cases. Only Qmax was found negatively associated with the EDSS score (p = 0.007), but no other association was observed. The presence of urinary symptoms was poor predictor of bladder dysfunction, urgency among the others showed relatively higher predicting value.
Conclusions
Subjective urinary symptoms assessment failed in predicting bladder function. Our results confirmed the value of objective urological assessment in patients with MS, irrespective of the presence of urinary symptoms.
Similar content being viewed by others
Introduction
Urinary disturbances may be a presenting sign in up to 14% of newly diagnosed Multiple Sclerosis (MS) patients [1], and is a major problem for over 50% of patients at some point throughout their disease course [2]. Urinary symptoms in MS can be grouped into three general syndromes: a) detrusor hyperreflexia - decreased storage capacity; b) incomplete emptying - hypotonic detrusor muscles; c) detrusor sphincter dyssynergia (DSD) - lack of detrusor/sphincter coordination.
Under-recognition of bladder dysfunction may have implications on quality of care given that effective therapies are available in preventing urinary complications and in improving patient’s quality of life [3, 4]. Few and heterogeneous studies have investigated the relationship between subjective urinary complaints and objective urological parameters in MS patients, reaching different conclusions [3, 5,6,7,8,9]. Is a routinary evaluation of urinary symptoms sufficient to exclude the presence of bladder dysfunction in patients with MS? To address this question, we designed a prospective study with the following objectives: 1) To assess the association between objective bladder function parameters in relation to urinary complaints; 2) to analyze the sensitivity and specificity of subjective urinary symptom-assessment in predicting objective bladder dysfunction in patients with MS.
Methods
Subjects
During a period of 1 year we have been prospectively recruiting consecutive patients with MS [10] from our MS Centre, San Camillo-Forlanini Hospital of Rome, Italy. Patients with the following features were excluded: 1) Expanded Disability Status Score (EDSS) score >7.0; 2) primary progressive course; 3) any conditions adversely affecting bladder function, other than MS; 4) presence of non-sterile urine culture; 5) any symptomatic treatments for bladder dysfunction; 6) current participation in other clinical trials.
During a single scheduled visit, through a face-to-face unstructured interview, patients were asked about the presence of urinary symptoms, as part of the bowel/bladder Functional System (FS) score, including urgency, frequency, hesitancy, urge incontinence and incomplete emptying. The symptoms were considered as present or absent, irrespective of severity or duration of the symptoms. The patient’s clinical status has been assessed by EDSS.
Assessment of bladder function
On the same day, all the patients were evaluated by an experienced urologist (G.B.) for the following urological parameters: maximum urinary flow rate (Qmax), postvoid residual urine volume (PVR), and detrusor sphincter dyssinergia (DSD). Qmax measurement was obtained by a computerized uroflowmeter (normal values >15 ml/s). PVR was indirectly measured by ultrasound scan (normal values <60 ml). DSD, as a loss of coordinated action of the detrusor and external sphincter muscles, was diagnosed on the basis of a combined assessment of urinary flow recordings and external urethral sphincter Electromyography (EMG) with surface electrodes [11, 12].
Statistical analysis
Only subjects with fully completed data were considered evaluable for the statistical analysis. All values are presented as mean ± SD or median (interquantile range) for continuous variables and as a number of subjects (percentage) for categorical variables. Comparisons were performed by means of analysis of variance for mean values and of Chi-square test. In order to identify the variables associated with bladder dysfunction, a logistic regression analysis was performed, considering the presence of abnormal urological parameters (Qmax, PVR, DSD) as outcome of the dependent variable and regressors were the presence of urinary symptoms and clinical parameters. Sensitivity and specificity of urinary symptoms for bladder dysfunction detection were calculated on a per-patient basis.
Results
Of the 141 patients screened, 109 (77.3%) met the study criteria and completed the protocol assessments (Table 1). Sample mean age was 44.6 ± 10.1 years, 80 (73.4%) subjects were females, the mean disease duration was 12.5 ± 8.7 years, 99 (90.8%) had a relapsing-remitting (RR) course, 10 (9.2%) had a secondary-progressive (SP) course; mean EDSS score was equal to 2.6 ± 1.7. Most of the patients were under immunomodulatory agents (N = 69 patients, 63.3%), a minority under immunosuppressive agents (n = 6, 5.5%), and a third were untreated (n = 34 patients, 31.2%).
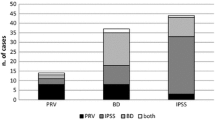
Fifty-eight patients (53.5%) complained of at least one urinary symptom, of these 65.5% one symptom, 24.1% two symptoms, while 10.4% complained of at least three symptoms. The frequency of specific urinary symptoms was as follows: urgency (40.7%), frequency (15.7%), incomplete emptying (12.0%), hesitancy (8.3%), urge incontinence (3.7%). No significant differences were observed between females and males patients in the frequency of urinary symptoms. Overall the mean Qmax value was 19.8 ± 9.7 ml/s, it was abnormal in 34.9% of subjects. The mean PVR was 66.9 ± 82.1 ml abnormal in 40.4% of participants. No significant differences were found for Qmax and PVR between females and males patients. Then, DSD was diagnosed in 37 subjects (33.9%), 32 (40.2%) females and 4 males patients (14.8%; p = 0.016).
By linear regression analysis, as expected both age (p <0.001) and disease duration (p <0.001) were positively associated with EDSS score. Whereas, when considering the urological parameters, only Qmax was found negatively associated with EDSS score (p = 0.007), and no other association was observed. Furthermore, the presence of urinary symptoms was poor predictor of objective bladder dysfunction, as assessed by the diagnostic procedures employed in our study. Overall urgency is what showed higher, albeit small, values of both sensitivity and specificity in predicting Qmax values (57.89; 69.01), PVR (50.0; 66.15) and DSD (36.99; 52.78). The other symptoms generally showed high specificity but with very low sensitivity (Table 2).
Discussion
We conducted a prospective study in a large MS population, not undergoing symptomatic treatment for urinary disturbances (to obtain unbiased evaluations and a more homogeneous sample possible), evaluating urinary symptoms and objective bladder dysfunction parameters. Our results indicated that a routine urinary symptoms assessment has a poor predictive value of objective bladder dysfunction in patients with MS. In our population over half of patients experienced at least one urinary symptom, and only about one third of patients showed at least one abnormal urological parameter. Urgency, more of the other symptoms, showed to be modestly sensitive and specific in predicting the presence of abnormal urological parameters, whereas the other symptoms showed no significant predictive value. This agrees with the findings of a large MS population study, where subjective assessments by bladder FS score and Guy’s Neurological Disability Scale bladder function score were not predictive of a clinically relevant postmicturition volume [13]. Similarly, in a prospective study of symptomatic MS patients, no significant correlation was found between clinical features and urodynamic patterns [5]. Instead, Betts et al. showed that MS patients with irritative bladder symptoms and lower limb pyramidal involvement were highly likely to have detrusor hyperreflexia, such as to make unnecessary to run the urodynamic study to choose the anticholinergic therapy [7]; similarly Araki et al. found that urinary irritative symptoms reflect the disease severity [9]. Betts et al. reported a linear progression of residual urine volume with bladder FS score, and suggested to perform the post-void urine volume measurement only in patients with significant disability [7].
In our population, possible explanations for the lack of predictive value of urinary assessments in detecting bladder dysfunction are several. First, the modality of data collection of urinary symptoms may be questionable. Although our choice to adopt an unstructured interview for the collection of major urinary symptoms was intended to reproduce clinical routine practice, the use of validated questionnaires would have allowed a more homogenous and reliable assessment [14]. Second, the selection of the objective urological parameters adopted in our study may be questionable as compared to more reliable and invasive diagnostic procedures, such as simultaneous recording of intravesical pressure and needle sphincter electromyography [12]. Third, the co-existence of common impairments such as changes in cognition, fatigue, and constipation may impair the patient’s awareness of the symptom itself. Furthermore, physical disability may impair the patient’s urinary control, without having a direct effect on bladder function.
So far international management guidelines for urinary disturbances have been developed [15, 16], but are not specific for the MS population. The International Scientific Committee of the 5th International Consultation on Incontinence on 2012 has formulated general recommendations for the diagnosis of neurogenic lower urinary tract dysfunction (NLUTD): a) patients with neurologic disease known to be associated with NLUTD should be evaluated for the presence of lower urinary tract symptoms; b) urodynamic tests should selectively be employed to supplement clinical assessment in determining management in NLUTD; c) sphincter EMG can be valuable in the diagnosis of patients with neurologic bladder dysfunction and can be considered as a diagnostic method in patients with NLUTD and neurologic urinary incontinence [15]. Several European national panels have published their own MS management consensus [17,18,19,20], although, they are mainly based on studies with low levels of evidence. While all groups advocate urological evaluation of symptomatic patients, the recommended approaches for asymptomatic patients are partially divergent and do not reach consensus [17,18,19,20].
Conclusions
In our MS population a routine subjective urinary symptoms assessment poorly correlated with objective bladder dysfunctions. Urgency resulted as the most predictive symptom, albeit modestly. Our data, in line with previous studies [5, 13], suggest that in patients with MS objective bladder evaluation, irrespective of subjective urinary symptoms, may contribute to a more complete and reliable assessment of patient’s disability. Given the feasibility of these non-invasive urological evaluations, we recommend making that objective assessment of bladder function become standard considerations in the evaluation of patients with MS, regardless of the presence of subjective urinary symptoms.
References
Fowler JF. Neurology of bladder, bowel, and sexual dysfunction. Butterworth-Heinemann Medical: Woburn, MA; 1999.
Miller H, Simpson CA, Yeates WK. Bladder dysfunction in multiple sclerosis. Br Med J. 1965;1(5445):1265–9.
DasGupta R, Fowler CJ. Bladder, bowel and sexual dysfunction in multiple sclerosis: management strategies. Drugs. 2003;63(2):153–66.
Kalsi V, Fowler CJ. Therapy insight: bladder dysfunction associated with multiple sclerosis. Nat Clin Pract Urol. 2005;2(10):492–501.
Gallien P, Robineau S, Nicolas B, Le Bot MP, Brissot R, Verin M. Vesicourethral dysfunction and urodynamic findings in multiple sclerosis: a study of 149 cases. Arch Phys Med Rehabil. 1998;79(3):255–7.
Kirchhof K, Fowler CJ. The value of the kurtzke functional systems scales in predicting incomplete bladder emptying. Spinal Cord. 2000;38(7):409–13.
Betts CD, D’Mellow MT, Fowler CJ. Urinary symptoms and the neurological features of bladder dysfunction in multiple sclerosis. J Neurol Neurosurg Psychiatry. 1993;56(3):245–50.
Litwiller SE, Frohman EM, Zimmern PE. Multiple sclerosis and the urologist. Urol. 1999;161(3):743–57.
Araki I, Matsui M, Ozawa K, et al. Relationship between urinary symptoms and disease-related parameters in multiple sclerosis. J Neurol. 2002;249(8):1010–5.
McDonald WI, Compston A, Edan G, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50(1):121–7.
Amarenco G, de Sèze M, Ruffion A, et al. Clinical and urodynamic evaluations of urinary disorders in multiple sclerosis. Ann Phys Rehabil Med. 2014;57(5):277–87.
Stoffel JT. Detrusor sphincter dyssynergia: a review of physiology, diagnosis, and treatment strategies. Transl Androl Urol. 2016;5(1):127–35.
Kragt JJ, Hoogervorst EL, Uitdehaag BM, Polman CH. Relation between objective and subjective measures of bladder dysfunction in multiple sclerosis. Neurology. 2004;63(9):1716–8.
Aharony SM, Lam O, Corcos J. Evaluation of lower urinary tract symptoms in multiple sclerosis patients: review of the literature and current guidelines. Can Urol Assoc J. 2017;11(1–2):61–4.
Abrams PCL, Khoury S, Wein A. Incontinence. 5th ed. Amhem: European association of urology; 2013.
Groen J, Pannek J, Castro Diaz D, et al. Summary of European Association of Urology (EAU) guidelines on neuro-urology. Eur Urol. 2016;69(2):324–33.
Ghezzi A, Carone R, Del Popolo G, et al. Recommendations for the management of urinary disorders in multiple sclerosis: a consensus of the Italian Multiple Sclerosis Study Group. Neurol Sci. 2011;32(6):1223–31.
De Ridder D, Van Der Aa F, Debruyne J, et al. Consensus guidelines on the neurologist’s role in the management of neurogenic lower urinary tract dysfunction in multiple sclerosis. Clin Neurol Neurosurg. 2013;115(10):2033–40.
Amarenco G, Chartier-Kastler E, Denys P, et al. First-line urological evaluation in multiple sclerosis: validation of a specific decision-making algorithm. Mult Scler. 2013;19(14):1931–7.
de Sèze M, Ruffion A, Denys P, et al. The neurogenic bladder in multiple sclerosis: review of the literature and proposal of management guidelines. Mult Scler. 2007;13(7):915–28.
Acknowledgements
We would like to thank the nursing staff for their kind assistance in helping conduct the study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets collected and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
SH, GB, SG, CG conception and design of the work. SH, OP data collection. SH, OP, GB data analysis and interpretation. SH drafting the article. All the authors critical revision of the article. All the authors final approval of the version to be published.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable
Ethics approval and consent to participate
The study underwent on approval of local Ethical Committee and all patients have given written informed consent to participate, as well as processing personal data authorization.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Haggiag, S., Bolla, G., Picconi, O. et al. Discrepancies between urinary symptoms assessment and objective bladder dysfunctions in multiple sclerosis. Mult Scler Demyelinating Disord 2, 11 (2017). https://doi.org/10.1186/s40893-017-0029-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40893-017-0029-z