Abstract
Background
Colorectal carcinomas (CRCs) arise from premalignant precursors in an adenoma-carcinoma sequence, in which adenoma with high-grade dysplasia (HGD) and early-stage carcinoma are defined as advanced neoplasia. A limited number of studies have evaluated the long-term outcomes of endoscopic submucosal dissection (ESD) for advanced colorectal neoplasia. This study aimed to assess the efficacy and safety of ESD for advanced colorectal neoplasia as well as the long-term outcomes, including local recurrence and metastasis.
Methods
We analyzed data collected from 610 consecutive patients with 616 advanced colorectal neoplasia lesions treated with ESD between January 2007 and December 2013. Clinical, endoscopic, and histological data were collected over a median follow-up period of 58 months to determine tumor stage and type, resection status, complications, tumor recurrence, and distant metastasis.
Results
The overall rates of en bloc resection, histological complete resection, and major complications were 94.3%, 89.4%, and 2.3%, respectively. Hybrid ESD was an independent factor of piecemeal resection. Tumor location in the colon was associated with increased risk of ESD-related complications. During the follow-up period, all patients remained free of metastasis. However, local recurrence occurred in 4 patients (0.8%); piecemeal resection was a risk factor.
Conclusions
ESD is effective and safe for resection of advanced colorectal neoplasia, with a high en bloc resection rate and favorable long-term outcomes. ESD is indicated for the treatment of HGD and early-stage CRC to obtain curative resection and reduce local recurrence rate.
Similar content being viewed by others
Background
Colorectal carcinoma (CRC) is currently a common cancer and is the third leading cause of cancer-related death worldwide [1, 2]. Most CRCs arise from premalignant precursors along a long-term adenoma-carcinoma sequence [3]. In this sequence, adenoma with high-grade dysplasia (HGD) and early-stage carcinoma are defined as advanced neoplasia [4, 5]. Identification and removal of such early-stage tumors have been associated with the prevention of CRC-related death [6]. Recently, endoscopic submucosal dissection (ESD) has been increasingly used for colorectal epithelial lesions [7]. Compared with conventional endoscopic resection, ESD enables en bloc resection with a high rate, which contributes to accurate histological evaluation [8, 9]. The number of studies on outcomes of ESD for superficial colorectal tumors is increasing [7, 10, 11]. However, data on the long-term outcomes of ESD for advanced colorectal neoplasia are still lacking. Hence, this study was performed to assess the efficacy, safety, and long-term outcomes of ESD for advanced colorectal neoplasia.
Patients and methods
Patient selection
ESD was initially indicated for lesions requiring endoscopic en bloc resection, for which the snare technique is difficult to implement, including laterally spreading tumors (LSTs), superficial invasive submucosal carcinoma, large depressed tumors, and large elevated lesions that are likely early-stage cancers [10, 12]. Consecutive patients with advanced colorectal neoplasia treated with ESD at our center between January 2007 and December 2013 were selected. Exclusion criteria included findings of a deep submucosal invasive carcinoma, as determined by endoscopic examination, and the presence of other invasive carcinomas and circumferential tumors that required surgical resection because of the increased technical difficulty and the anticipated risk of stenosis.
The clinicopathologic information of selected patients was collected to analyze the long-term outcomes after ESD. The study was performed in accordance with the Declaration of Helsinki (5th version). All patients were informed of the risks and benefits of ESD, and each patient provided written informed consent for the procedure. This study protocol was approved by the institutional review board of Zhongshan Hospital, Fudan University (No. 2009135).
Endoscopic submucosal dissection
ESD was performed with the patient under general intravenous anesthesia, and indices of the patient’s cardiorespiratory functions (heart rate, blood pressure, and oxygen saturation) were continually monitored. Endoscopic equipment and accessories were introduced as described in previous reports [13, 14]. The procedure began by marking dots on the normal mucosa approximately 5 mm away from the tumor (Fig. 1). After the submucosal injection of 5 mL of solution (including 5% indigo carmine and 1% epinephrine) using a 23-gauge disposable needle, a mucosal incision was created along the marker dots using a needle knife. Next, under direct vision, we continued to use a hook knife to dissect the submucosal connective tissue beneath the tumor; the muscularis propria layer along the edge of the lesions could also be peeled if necessary. During the dissection, the solution was injected repeatedly if necessary. After resection was completed, all visible vessels of the artificial ulcer bed were thoroughly coagulated with argon plasma coagulation to prevent postoperative bleeding. Hybrid ESD was defined as the combined use of conventional endoscopic resection and the ESD technique, with a special ESD knife, and resection was completed by snaring [7, 12, 15]. Hybrid ESD was performed when standard ESD was infeasible.
Endoscopic submucosal dissection (ESD) of a high-grade rectal dysplasia. a Endoscopic view of the lesion; b marker dots on the normal mucosa; c mucosal incision along the marker dots; d the artificial ulcer bed after ESD; e tissue specimens fixed to a wooden plate using thin needles; f endoscopic view of the scar during follow-up period
After ESD, surgery was recommended when tumors were suspicious with risk factors of lymph node metastasis such as deep submucosal invasion, lymphovascular infiltration, poor differentiation, and tumor budding.
Histopathological examination
Resected specimens were stretched, pinned, fixed in formalin solution and assessed microscopically. The World Health Organization classification for tumors of the digestive system was used for histopathological evaluation [16]. An en bloc resection was defined as an excision of the tumor in one piece without fragmentation. Histological complete resection was defined as en bloc resection with negative horizontal and vertical margins. The definition of R0 resection was a histological complete resection and no risk of lymph node metastasis according to histological examination of the resected specimen following the Japanese Society for Cancer of the Colon and Rectum (JSCCR) guideline criteria [17].
Complication observation
Bleeding and perforation are major ESD-related complications. Minor bleeding was treated with immediate coagulation and was not viewed as a complication. Delayed bleeding was defined as hematochezia or melena requiring an endoscopic hemostatic procedure from 0 to 14 days after ESD completion.
Follow-up
All patients were followed up either at our institution or in partnership with their referring centers. Follow-up colonoscopy was performed at 6 and 12 months after colorectal ESD. Then, patients were suggested to be followed according to the surveillance guidelines [18, 19]. The last follow-up was performed in December 2016.
Data collection and statistical analysis
Clinicopathological and endoscopic data, including age, sex, tumor characteristics, histology, resection status, complications, local recurrence, and metastasis, were collected from the database of colorectal ESDs of our center and analyzed. Statistical analysis among groups was performed using Pearson’s Chi square test, a continuity correction Chi square test, or Fisher’s exact test as appropriate. Risks for piecemeal resection, complications, and local recurrence were assessed by univariate and/or multivariate logistic regression analyses as appropriate. SPSS Statistics 18 software (IBM, Chicago, IL, USA) was used for statistical analysis. P < 0.05 was considered to be statistically significant.
Results
Characteristics of patients
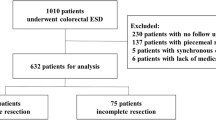
Between January 2007 and December 2013, 610 patients (354 men and 256 women) with 616 advanced colorectal neoplasia lesions were identified and analyzed in this study (Fig. 2). Six patients had 2 lesions. The median age of the patients was 64 (range, 23–89) years; 370 (60.7%) patients were older than 60 years.
Pathologic results
The average tumor size was 2.9 ± 1.3 cm (median, 2.5 cm; range, 1.0–9.0 cm). As shown in Table 1, polypoid tumor was the most common macroscopic type, and HGD was the most common histological type. Only 12 (1.9%) lesions presented with invasive lymphovascular infiltration.
A total of 57 patients had deep submucosal invasion and/or invasive lymphovascular infiltration: 56 accepted additional radical surgery, and 1 with rectal lesion rejected additional radical surgery and underwent additional local radiotherapy. Two patients with T1b carcinomas (submucosal invasion ≥ 1000 μm in depth) had a histological complete resection. Although additional surgery was recommended to the 2 abovementioned patients, it was rejected because of the high surgical risk associated with comorbidities and old age, and instead each accepted an intensive follow-up.
Feasibility of endoscopic submucosal dissection
En bloc resection was achieved in 581 (94.3%) of the 616 lesions, and histological complete resection was achieved in 551 (89.4%) lesions. Outcomes related to ESD are shown in Table 2. Univariate analysis showed that tumor location and resection method were significantly associated with the ESD piecemeal resection rate. Multivariate analysis indicated that piecemeal resection rate was independently higher in tumors treated by hybrid ESD than in tumors treated by standard ESD (Table 3).
Complications
Ten (1.6%) patients who underwent endoscopic hemostatic procedures had postoperative bleeding, and 4 (0.7%) patients had a perforation during the ESD procedure (Table 2). All cases of recognized intraoperative perforation or postoperative bleeding were successfully managed by endoscopic closure or coagulation. Perforations were also managed with subsequent conservative treatment, including fasting and intravenous antibiotics for a few days. There were no treatment-related deaths. In both the univariate and multivariate analyses, tumor location in the colon was an independent contributor to ESD-related complications (Table 4).
Follow-up results
Excluding the 57 patients who underwent additional surgery or radiotherapy, 533 patients were evaluated for the outcomes of ESD. Thirty-nine patients were lost to follow-up; among them, 27 had HGD, 9 had carcinomas in situ, and 3 had T1a carcinomas (submucosal invasion < 1000 μm in depth). The other 514 patients with 520 lesions had a median follow-up period of 58 months (range, 36–117 months). Local recurrence was detected in 4 (0.8%) patients, all of whom showed HGD (Table 2). Piecemeal resection was a significant contributor to local recurrence (Table 5). No patients developed metastasis to either the lymph nodes or distant organs during the follow-up period.
Discussion
In the present study, ESD achieved en bloc resection and histological complete resection rates of 94.3% and 89.4% for patients with advanced colorectal neoplasia, and the rate of major complications was only 2.3%. Hybrid ESD was an independent factor of piecemeal resection. Tumor location in the colon was associated with increased risk of ESD-related complications.
ESD offered a high en bloc and complete resection rate for early-stage CRC and HGD in the colorectum, even for lesions that were larger than 4.0 cm in diameter or located deeper in the submucosal layer [8, 9]. Additionally, the complete resection rate of ESD was relatively higher than that of endoscopic mucosal resection (EMR) [8]. On the other hand, EMR is unlikely to offer a high complete resection rate for large colorectal epithelial lesions or for post-EMR tumor recurrences. A piecemeal EMR resection results in increased post-EMR recurrences and uncertainty in histological assessment of the complete resection [20]. However, ESD of colorectal tumors is technically difficult. Therefore, hybrid ESD (a combined EMR and ESD technique) has been proposed to facilitate the ESD procedure and could be an option in certain situations [21, 22]. The multivariate analysis conducted in the present study indicated that the piecemeal resection rate was independently higher for tumors treated with hybrid ESD than for tumors treated with standard ESD. The risk of recurrence after piecemeal removal is relatively high, suggesting that standard ESD is preferred for patients with potential malignance [3].
Previous work indicated that ESD was the first-line treatment for tumors larger than 2.0 cm [23]. In the present study, ESD was indicated for lesions requiring endoscopic en bloc resection for which it was difficult to use the snare technique. ESD was the preferred treatment for advanced colorectal neoplasia and tumors with higher malignant potential, such as non-granular LST (LST-NG) [24], irrespective of tumor size. Notably, tumor location in the colon contributed to piecemeal resection in the present study. Hayashi et al. [25] indicated that poor endoscopic operability was an independent predictor of histological incomplete resection and perforation. Hori et al. [26] studied predictive factors for technical difficulty in ESD of the colorectum and indicated that colon flexure location was an independent risk factor for piecemeal resection. Isomoto et al. [27] reported that a tumor located in the right-side colon was an independent risk factor for histological incomplete resection. Although multivariate analysis indicated that tumor location was not an independent risk factor of piecemeal resection in the present study, ESD for colon tumors requires more experience and attention due to the unique anatomical characteristics of the colon and its flexures.
Repici et al. [28] suggested that colorectal anatomic characteristics were the main contributors to the risk of ESD-related complications. We noted that colon tumor location was an independent risk factor for complications. Hori et al. [26] also indicated that tumor location at the colon flexure was an independent risk factor for ESD-related complications and that ESD for colon tumors requires more technical skills and, especially for tumors located at flexures. However, the importance of tumor location was influenced by the endoscopist’s experience.
Our results indicate an adequate safety profile for colorectal ESD. Major complications occurred in 14 (2.3%) patients: 10 had postoperative bleeding, and 4 had a perforation. Postoperative bleeding could be managed with endoscopy without emergency surgery, and patients then often recovered under conservative observation. In the present study, all cases of recognized perforation were successfully managed immediately by endoscopic closure using endoclips.
In the present large consecutive study with a median follow-up period of more than 4 years, neither ESD-related nor disease-specific death was observed. The overall local recurrence rate was low and occurred in patients with piecemeal resection of tumors. As discussed above, hybrid ESD is a significant and independent contributor to piecemeal resection, which is the most important risk factor for local recurrence after endoscopic resection for colorectal neoplasia [7]. Consistently, in the present study, we found that the local recurrence rate of patients treated with hybrid ESD was higher than that of patients treated with standard ESD, but without significant difference, probably because the proportion of patients who underwent hybrid ESD was low. Thus, standard ESD is indicated for treating carcinomatous lesions because it features en bloc resection, which may decrease the risk of local recurrence.
The potential malignance of a lesion should be considered before choosing the endoscopic resection method. A regular endoscopic examination during follow-up is important, particularly for patients with piecemeal resection. Follow-up colonoscopy was recommended at 3–6 months after piecemeal resection, and it has been reported that most local recurrent lesions were detected within 12 months after the initial endoscopic resection [28, 29]. When local recurrence occurs, additional ESD was acceptable [30, 31].
For patients with invasive tumors, such as T1 carcinomas with deep submucosal invasion, surgical treatment is safer than ESD. It was reported that long-term outcomes were favorable if patients with non-R0 resection undergo appropriate additional surgical resection [10]. According to the 2014 JSCCR Guidelines for the Treatment of Colorectal Cancer [17], patients with T1 CRC should be considered for additional colectomy with lymph node dissection. However, the probability of lymph node metastasis is extremely low if no other risk factors exist [10, 32, 33]. In the present study, 2 patients with T1 CRC had a histological complete resection. Although additional surgery was recommended, it was rejected by these 2 patients because of high surgical risk, and instead each patient accepted an intensive follow-up. No recurrence or lymph node metastasis occurred during the follow-up period.
The limitations of the present study included its retrospective design and single-center analysis, although we evaluated many consecutive case series. Thus, a prospective and multi-center study is warranted.
Conclusions
ESD is effective and safe for the resection of advanced colorectal neoplasia, with a high en bloc resection rate and favorable long-term outcomes. ESD is indicated for the treatment of early-stage CRC and HGD to obtain curative resection and prevent local recurrence.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29.
Chen W, Zheng R, Zeng H, et al. The incidence and mortality of major cancers in China, 2012. Chin J Cancer. 2016;35(1):73.
Repici A, Hassan C, De Paula Pessoa D, et al. Efficacy and safety of endoscopic submucosal dissection for colorectal neoplasia: a systematic review. Endoscopy. 2012;44:137–50.
Imperiale TF, Yu M, Monahan PO, et al. Risk of advanced neoplasia using the National Cancer Institute’s colorectal cancer risk assessment tool. J Natl Cancer Inst. 2016;109(1). https://doi.org/10.1093/jnci/djw181.
Sawhney MS, Dickstein J, LeClair J, et al. Adenomas with high-grade dysplasia and early adenocarcinoma are more likely to be sessile in the proximal colon. Colorectal Dis. 2015;17:682–8.
Atkin WS, Edwards R, Kralj-Hans I, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375:1624–33.
Oka S, Tanaka S, Saito Y, et al. Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am J Gastroenterol. 2015;110:697–707.
Saito Y, Fukuzawa M, Matsuda T, et al. Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors determined by curative resection. Surg Endosc. 2010;24:343–52.
Saito Y, Uraoka T, Yamaguchi Y, et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc. 2010;72:1217–25.
Shigita K, Oka S, Tanaka S, et al. Long-term outcomes after endoscopic submucosal dissection for superficial colorectal tumors. Gastrointest Endosc. 2017;85:546–53.
Yamada M, Saito Y, Takamaru H, et al. Long-term clinical outcomes of endoscopic submucosal dissection for colorectal neoplasms in 423 cases: a retrospective study. Endoscopy. 2017;49(3):233–42.
Tanaka S, Kashida H, Saito Y, et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015;27(4):417–34.
Chen T, Yao LQ, Xu MD, et al. Efficacy and safety of endoscopic submucosal dissection for colorectal carcinoids. Clin Gastroenterol Hepatol. 2016;14:575–81.
Saito Y, Otake Y, Sakamoto T, et al. Indications for and technical aspects of colorectal endoscopic submucosal dissection. Gut Liver. 2013;7:263–9.
Terasaki M, Tanaka S, Oka S, et al. Clinical outcomes of endoscopic submucosal dissection and endoscopic mucosal resection for laterally spreading tumors larger than 20 mm. J Gastroenterol Hepatol. 2012;27:734–40.
Bosman FT, Carneiro F, Hruban RH, et al. WHO classification of tumours of the digestive system. Lyon: IARC; 2010.
Watanabe T, Itabashi M, Shimada Y, et al. Japanese society for cancer of the colon and rectum (JSCCR) guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol. 2015;20:207–39.
Rex DK, Kahi CJ, Levin B, et al. Guidelines for colonoscopy surveillance after cancer resection: a consensus update by the American Cancer Society and the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2006;130:1865–71.
Bartel MJ, Brahmbhatt BS, Wallace MB. Management of colorectal T1 carcinoma treated by endoscopic resection from the Western perspective. Dig Endosc. 2016;28(3):330–41.
Cao Y, Liao C, Tan A, et al. Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy. 2009;41:751–7.
Pimntel-Nunes P, Dinis-Ribeiro M, Ponchon T, et al. Endoscopic submucosal dissection: European society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy. 2015;47(9):829–54.
Toyonaga T, Man-I M, Morita Y, et al. Endoscopic submucosal dissection (ESD) versus simplified/hybrid ESD. Gastrointest Endosc Clin. 2014;24(2):191–9.
Nishiyama H, Isomoto H, Yamaguchi N, et al. Endoscopic submucosal dissection for laterally spreading tumours of the colorectum in 200 consecutive cases. Surg Endosc. 2010;24:2881–7.
Fujishiro M, Yahagi N, Kakushima N, et al. Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol. 2007;5:678–83.
Hayashi N, Tanaka S, Nishiyama S, et al. Predictors of incomplete resection and perforation associated with endoscopic submucosal dissection for colorectal tumors. Gastrointest Endosc. 2014;79(3):427–35.
Hori K, Uraoka T, Harada K, et al. Predictive factors for technically difficult endoscopic submucosal dissection in the colorectum. Endoscopy. 2014;46:862–70.
Isomoto H, Nishiyama H, Yamaguchi N, et al. Clinicopathological factors associated with clinical outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy. 2009;41:679–83.
Repici A, Pellicano R, Strangio G, et al. Endoscopic mucosal resection for early colorectal neoplasia: pathologic basis, procedures, and outcomes. Dis Colon Rectum. 2009;52:1502–15.
Winawer SJ, Zauber AG, Fletcher RH, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology. 2006;130:1872–85.
Niimi K, Fujishiro M, Kodashima S, et al. Long-term outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy. 2010;42:723–9.
Hurlstone DP, Shorthouse AJ, Brown SR, et al. Salvage endoscopic submucosal dissection for residual or local recurrent intraepithelial neoplasia in the colorectum: a prospective analysis. Colorect Dis. 2008;10:891–7.
Nakadoi K, Tanaka S, Kanao H, et al. Management of T1 colorectal carcinoma with special reference to criteria for curative endoscopic resection. J Gastroenterol Hepatol. 2012;27:1057–62.
Yoshii S, Nojima M, Nosho K, et al. Factors associated with risk for colorectal cancer recurrence after endoscopic resection of t1 tumors. Clin Gastroenterol Hepatol. 2014;12:292–302.
Authors’ contributions
Study conception and design: P-HZ, TC. Acquisition of data: W-ZQ, Y-QZ, TC. Analysis and interpretation of data: P-HZ, M-DX, TC, L-QY, Y-SZ, L-LC, Y-YH. Drafting of manuscript: TC. Critical revision: P-HZ, M-DX, TC, W-ZQ, J-WH, MO. Final approval of the version: P-HZ, TC. All authors read and approved the final manuscript.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (No. 81502523), and grant from Shanghai Committee of Science and Technology (Nos. 17140901100, 16DZ2280900, and 14411950505).
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data and material are available.
Consent for publication
We all consent for publication.
Ethics approval and consent to participate
This study protocol was approved by the institutional review board of Zhongshan Hospital, Fudan University (No. 2009135).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chen, T., Qin, WZ., Yao, LQ. et al. Long-term outcomes of endoscopic submucosal dissection for high-grade dysplasia and early-stage carcinoma in the colorectum. Cancer Commun 38, 3 (2018). https://doi.org/10.1186/s40880-018-0273-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40880-018-0273-4