Abstract
Background
The programmed cell death 1 (PD-1) inhibitor pembrolizumab is a promising agent for treatment of several different malignancies, but as with all immunotherapy there is a potential risk of immune-related adverse events. Adrenocorticotropic hormone (ACTH) deficiency and hypophysitis have been reported in patients treated with a different PD-1 inhibitor, nivolumab. However, clinical characteristics of these side effects associated with pembrolizumab have yet to be described in detail.
Case presentation
An 85-year-old Japanese woman was diagnosed with advanced squamous cell lung cancer. The patient was treated with 200 mg pembrolizumab every three weeks as first-line therapy. Routine examination including thyroid function, complete blood count, serum cortisol and sodium levels before each pembrolizumab infusion had shown no significant changes up to the eighth cycle. However, 8 days after the eighth cycle of single-agent pembrolizumab, she presented with rapidly worsening general fatigue and appetite loss over two days. Laboratory data revealed a low serum cortisol level (0.92 μg/dL) with inappropriately low ACTH (8.3 pg/mL), hyponatremia (122 mmol/L) and hypoglycemia (68 mg/dL). Standard-dose short ACTH testing showed an unsatisfactory cortisol response, indicating adrenal insufficiency. Pituitary magnetic resonance imaging showed diffuse substantial gadolinium enhancement, T2 hyperintensity, loss of pituitary bright spot, but no pituitary enlargement. Serum cortisol and ACTH levels were low throughout the day, and urinary free cortisol excretion fell below the lower normal limit. There was no ACTH and cortisol response in the corticotropin-releasing hormone test, despite significant responses of other anterior pituitary hormones to their corresponding challenge tests. Thus, isolated ACTH deficiency was diagnosed, and hypophysitis was suspected as the etiology. After administration of 15 mg/day hydrocortisone, the patient’s debilitation, hyponatremia, and hypoglycemia swiftly disappeared.
Conclusion
This is a case of isolated ACTH deficiency possibly due to hypophysitis in a patient with advanced lung cancer, in whom recent routine examinations had shown unremarkable results. We therefore conclude that isolated ACTH deficiency can suddenly arise during pembrolizumab monotherapy, albeit probably only rarely. Caution should be exercised to make sure that adrenal insufficiency is recognized immediately in order to achieve swift recovery by steroid replacement.
Similar content being viewed by others
Background
Programmed cell death 1 (PD-1), programmed cell death 1 ligand 1 (PD-L1) and cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) are targets for checkpoint inhibition in cancer immunotherapy [1]. Since the anti-CTLA-4 IgG1 monoclonal antibody ipilimumab was first approved for the treatment of malignant melanoma in 2011, several other immune checkpoint inhibitors have gained approval, namely the PD-1 inhibitors pembrolizumab and nivolumab in 2014, and the PD-L1 inhibitors atezolizumab in 2016, and avelumab and durvalumab in 2017. Despite their clinical efficacy, ICI use carries potential risks for a broad spectrum of unfavorable immune-mediated tissue damage, termed immune-related adverse events (irAEs). The increasing use of ICIs is resulting in accumulating numbers of cases of endocrine irAEs such as thyroid dysfunction, hypophysitis, type 1 diabetes mellitus, and primary or secondary adrenal insufficiency [2, 3]. However, clinical characteristics of secondary adrenal insufficiency and hypophysitis specifically associated with pembrolizumab treatment remain unknown because of the rarity of this adverse event. Here, we present a case of isolated adrenocorticotropic hormone (ACTH) deficiency possibly due to hypophysitis during single-agent pembrolizumab therapy for advanced squamous cell lung cancer.
Case presentation
An 85-year-old Japanese woman with squamous cell lung carcinoma presented with rapidly worsening general fatigue and appetite loss over two days, eight days after the eighth cycle of pembrolizumab monotherapy. Stage IV squamous cell lung cancer (T3N2M1a) had been diagnosed seven months prior to this. Pembrolizumab had been administered as first-line therapy because biopsy indicated that the PD-L1 tumor proportion score was 100% and no epidermal growth factor receptor mutations, anaplastic lymphoma kinase rearrangements and c-ros oncogene 1 rearrangements were present. The patient had received eight cycles of 200 mg pembrolizumab every three weeks, resulting in stable disease. Routine examination with thyroid hormones and the hypothalamic-pituitary-adrenal axis before each pembrolizumab infusion had shown no significant changes up to the eighth cycle (Table 1). There was no history of concomitant steroid use during immunotherapy, and the patient denied any recent steroid use.
On physical examination, body mass index was 20.6 kg/m2 (height 153 cm, weight 47 kg), body temperature was 37.0 °C, blood pressure was 112/60 mmHg with a regular pulse of 96 beats/min. The patient was debilitated, but there were no remarkable findings for the head, neck, chest, abdomen or extremities. No visual deficit was apparent according to the confrontation method.
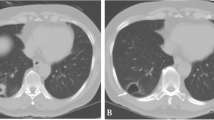
Laboratory examination on arrival (1300 h) revealed a low serum cortisol level with an inappropriately low ACTH level, hyponatremia with a raised antidiuretic hormone (ADH) level, and hypoglycemia, but no eosinophilia (Table 1). Urine osmolarity was inappropriately high at 630 mOsm/kg despite low plasma osmolarity of 247 mOsm/kg, indicating inappropriate ADH secretion. There was a poor response to standard-dose short ACTH testing (Fig. 1). Pituitary magnetic resonance imaging revealed higher intensity on T2-weighted imaging, homogeneous gadolinium distribution in the pituitary and the stalk on enhanced imaging, and the lack of a posterior pituitary bright signal on T1-weighted imaging (Fig. 2). However, pituitary enlargement was not apparent. Serum anti-pituitary cell antibody-1 (BML, Inc., Tokyo, Japan) was negative. Urinary free cortisol excretion was 9.8 μg/day (range, 11.2–80.3 μg/day). There were no cortisol responses and poor ACTH (basal at 6.4 to peak at 11.2 pg/mL) secretion responses on corticotropin-releasing hormone testing, and the values for other anterior pituitary hormones on challenge tests were all unremarkable (Fig. 3). The insulin tolerance test was avoided in consideration of the patient’s advanced age. The adrenal glands were unremarkable on computed tomography. Thus, the patient was diagnosed as having isolated ACTH deficiency. Hydrocortisone administered at 15 mg/day, split over three times daily (7.5–5-2.5 mg), swiftly improved the patient’s general condition, corrected the inappropriately high ADH level, and normalized serum sodium concentration. While urine volume increased to about 3000 mL/day after hydrocortisone supplementation, the hypertonic saline test showed a substantial ADH response. Polyuria spontaneously improved with time.
Pituitary challenge tests. Horizontal axis: time course. Vertical axis: hormone levels. a Corticotropin-releasing hormone test. b Thyrotropin-releasing hormone test. c Gonadotropin-releasing hormone test. d Growth hormone-releasing peptide 2 test. ACTH, adrenocorticotropic hormone; FSH, follicle stimulating hormone; GH, growth hormone; LH, luteinizing hormone; PRL, prolactin; TSH, thyroid stimulating hormone
The patient was discharged, and levels of ACTH and cortisol after the morning hydrocortisone, and thyroid function, were followed monthly in outpatient care. While cortisol levels ranged from 8.12 to 18.3 μg/dL, ACTH levels were not detectable on any occasion during the observation period (5 months after admission). Thus, ACTH deficiency obviously persisted, while thyroid function remained normal, and white blood cell count, eosinophil count, serum electrolytes and glucose were all unremarkable.
Discussion and conclusions
Lung cancer is a leading cause of cancer-related mortality, with the majority of cases being non-small cell lung carcinoma (NSCLC). Immune checkpoint inhibition targeting PD-1 enhances peripheral T-cell immunity, resulting in an antitumor effect, and has shown substantial potential for the treatment of several malignancies including NSCLC [4]. Recently, the anti-PD-1 IgG4 monoclonal antibody pembrolizumab has been recommended as first-line monotherapy for advanced NSCLC with high PD-L1 expression, but lacking targetable driver gene mutations, because of its superiority over conventional platinum-based chemotherapy for both progression-free and overall survival [5, 6]. While ICIs are promising agents for cancer treatment, their use carries a potential risk of irAEs including endocrinopathies (i.e. hypophysitis, hypopituitarism, autoimmune diabetes and thyroiditis). Ten et al. recently reviewed cases of hypophysitis and anterior pituitary insufficiency [7]. Patient median age was 61 years, most were male, median onset from the initiation of immune checkpoint inhibitor use was 12 weeks, and most cases were associated with the use of the CTLA-4 inhibitor ipilimumab [7].
The present case was diagnosed as having ACTH deficiency based on low basal cortisol level, inadequate cortisol secretion responses on a rapid ACTH test and a CRH test, and an insufficient ACTH secretion response on a CRH, although data on insulin tolerance were lacking [8]. Additionally, the low dehydroepiandrosterone sulfate level of 5 ng/mL (reference range for females aged 71 years and above, 7–177 ng/mL) was also compatible with this diagnosis, because patients with ACTH deficiency were reported to have significantly lower dehydroepiandrosterone sulfate than those without [9]. Recently, several cases of isolated ACTH deficiency associated with the use of the PD-1 inhibitor nivolumab have been reported [3]. However, cases associated with pembrolizumab have rarely been described. To the best of our knowledge, at the time of writing there were only two reports of ACTH deficiency associated with pembrolizumab use (Table 2) [10, 11]. These findings suggest a difference in incidence rates of this adverse event even among these drugs in the same class. There are differences between our present case and these previous two reports in the treatment regimen and the onset of pituitary disorders. Whether pembrolizumab or cancer chemotherapy were involved in disease etiology were unclear in the previous reports, but this present case certainly suggests that isolated ACTH deficiency can occur during single-agent pembrolizumab treatment. This present case also suggests the possible occurrence of pituitary damage at early onset, although previous reports showed ACTH deficiency occurred after stopping pembrolizumab.
The mechanism responsible for the development of ACTH deficiency associated with pembrolizumab remains to be fully elucidated, but hypophysitis is a possible etiology in the present case. Lymphocytic hypophysitis, the most common form of primary hypophysitis, typically gives rise to anterior pituitary dysfunction and marked pituitary enlargement resulting in mass effects [12]. The incidence of such mass effects, resulting in headache or visual impairment, was reported to be as high as 56–83% [12]. In addition to pituitary enlargement, homogeneous strong gadolinium uptake, loss of bright signal intensity in the posterior pituitary lobe and thickened pituitary stalk are signs of lymphocytic hypophysitis on magnetic resonance imaging [13]. In contrast, pituitary enlargement was reported as mild, and thus mass effects such as headache and visual defects are rare in patients with ICI-associated hypophysitis. A case of hypophysitis associated with CTLA-4 blockade was first described in 2003, after which a substantial number of subsequent cases of ipilimumab-induced hypophysitis have been reported due to the increased use of this agent in clinical practice, and a higher incidence of hypophysitis relative to other ICIs [14, 15]. Although the etiology has not been fully elucidated, previous studies suggest that ipilimumab can bind CTLA-4 antigen expressed in the pituitary to evoke lymphocytic infiltration resulting in pituitary toxicity [16, 17]. In patients with ipilimumab-induced hypophysitis, pituitary enlargement and thickened stalk are generally mild or sometimes not present at all [12, 15, 18]. Correspondingly, a recent review reported that none of 57 ipilimumab-induced hypophysitis cases suffered visual impairment [15]. Despite the lower frequency of cases relative to ipilimumab-induced hypophysitis, several instances of hypophysitis associated with the use of the PD-1 inhibitor nivolumab have been reported. These showed a more trivial pituitary enlargement than typical for lymphocytic hypophysitis [3, 19]. Thus, pituitary enlargement on imaging might have too low a sensitivity for diagnosis in such a setting. Diffuse substantial gadolinium enhancement, T2 hyperintensity, and loss of pituitary bright spot on magnetic resonance imaging in this present case might be associated with pituitary inflammation, although pituitary enlargement was not apparent.
Hypophysitis is a well-known endocrine irAE, but its incidence varies depending on the ICI agent employed. A recent systematic review and meta-analysis reported that hypophysitis was rarely observed in patients treated by PD-1 or PD-L1 blockade, despite its more frequent occurrence in patients on combination therapy of CTLA-4 together with PD-1 inhibitors and with CTLA-4 inhibitors alone [2, 20]. Early recognition of hypophysitis and subsequent ACTH deficiency is crucial because it is potentially life-threatening but remediable by steroid replacement therapy. A retrospective cohort study indicated that eosinophilia is an early indicator of ACTH deficiency during PD-1 inhibitor treatment [21]. However, these findings were not applicable to the present case, because the complete blood count did not show any change even at the last cycle of pembrolizumab (Table 1). Because of its rarity, a case of hypophysitis associated with pembrolizumab treatment has yet to be described in the literature. Thus, further cases need to be accumulated to fully comprehend disease characteristics and clinical course.
Conclusively, isolated ACTH deficiency can suddenly occur during pembrolizumab monotherapy in the absence of any warning findings at routine examination. Caution should be exercised for early recognition of adrenal insufficiency so that swift recovery can be achieved by steroid replacement.
Availability of data and materials
The data used in this current report are available from the corresponding author on reasonable request.
Abbreviations
- ACTH:
-
Adrenocorticotropic hormone
- ADH:
-
Antidiuretic hormone
- CTLA-4:
-
Cytotoxic T-lymphocyte-associated antigen 4
- ICI:
-
Immune checkpoint inhibitor
- irAE:
-
Immune-related adverse event
- NSCLC:
-
Non-small cell lung carcinoma
- PD-1:
-
Programmed cell death 1
- PD-L1:
-
Programmed cell death 1 ligand 1
References
Sharma P, Wagner K, Wolchok JD, Allison JP. Novel cancer immunotherapy agents with survival benefit: recent successes and next steps. Nat Rev Cancer. 2011;11(11):805–12.
Barroso-Sousa R, Barry WT, Garrido-Castro AC, Hodi FS, Min L, Krop IE, Tolaney SM. Incidence of endocrine dysfunction following the use of different immune checkpoint inhibitor regimens: a systematic review and meta-analysis. JAMA Oncol. 2018;4(2):173–82.
Ohara N, Ohashi K, Fujisaki T, Oda C, Ikeda Y, Yoneoka Y, Hashimoto T, Hasegawa G, Suzuki K, Takada T. Isolated Adrenocorticotropin deficiency due to Nivolumab-induced Hypophysitis in a patient with advanced lung adenocarcinoma: a case report and literature review. Intern Med. 2018;57(4):527–35.
Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–54.
Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, Gottfried M, Peled N, Tafreshi A, Cuffe S, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung Cancer. N Engl J Med. 2016;375(19):1823–33.
Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, Gottfried M, Peled N, Tafreshi A, Cuffe S, et al. Updated analysis of KEYNOTE-024: Pembrolizumab versus platinum-based chemotherapy for advanced non-small- cell lung Cancer with PD-L1 tumor proportion score of 50% or greater. J Clin Oncol. 2019;37(7):537–46.
Tan MH, Iyengar R, Mizokami-Stout K, Yentz S, MacEachern MP, Shen LY, Redman B, Gianchandani R. Spectrum of immune checkpoint inhibitors-induced endocrinopathies in cancer patients: a scoping review of case reports. Clin Diabetes Endocrinol. 2019;5:1.
Yanase T, Tajima T, Katabami T, Iwasaki Y, Tanahashi Y, Sugawara A, Hasegawa T, Mune T, Oki Y, Nakagawa Y, et al. Diagnosis and treatment of adrenal insufficiency including adrenal crisis: a Japan Endocrine Society clinical practice guideline [opinion]. Endocr J. 2016;63(9):765–84.
Sayyed Kassem L, El Sibai K, Chaiban J, Abdelmannan D, Arafah BM. Measurements of serum DHEA and DHEA sulphate levels improve the accuracy of the low-dose cosyntropin test in the diagnosis of central adrenal insufficiency. J Clin Endocrinol Metab. 2012;97(10):3655–62.
Boudjemaa A, Rousseau-Bussac G, Monnet I. Late-onset adrenal insufficiency more than 1 year after stopping Pembrolizumab. J Thorac Oncol. 2018;13(3):e39–40.
Oristrell G, Baneras J, Ros J, Munoz E. Cardiac tamponade and adrenal insufficiency due to pembrolizumab: a case report. Eur Heart J Case Rep. 2018;2(2):yty038.
Gubbi S, Hannah-Shmouni F, Stratakis CA, Koch CA. Primary hypophysitis and other autoimmune disorders of the sellar and suprasellar regions. Rev Endocr Metab Disord. 2018;19(4):335–47.
Gutenberg A, Larsen J, Lupi I, Rohde V, Caturegli P. A radiologic score to distinguish autoimmune hypophysitis from nonsecreting pituitary adenoma preoperatively. AJNR Am J Neuroradiol. 2009;30(9):1766–72.
Phan GQ, Yang JC, Sherry RM, Hwu P, Topalian SL, Schwartzentruber DJ, Restifo NP, Haworth LR, Seipp CA, Freezer LJ, et al. Cancer regression and autoimmunity induced by cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma. Proc Natl Acad Sci U S A. 2003;100(14):8372–7.
Faje A. Immunotherapy and hypophysitis: clinical presentation, treatment, and biologic insights. Pituitary. 2016;19(1):82–92.
Iwama S, De Remigis A, Callahan MK, Slovin SF, Wolchok JD, Caturegli P. Pituitary expression of CTLA-4 mediates hypophysitis secondary to administration of CTLA-4 blocking antibody. Sci Transl Med. 2014;6(230):230ra45.
Caturegli P, Di Dalmazi G, Lombardi M, Grosso F, Larman HB, Larman T, Taverna G, Cosottini M, Lupi I. Hypophysitis secondary to cytotoxic T-lymphocyte-associated protein 4 blockade: insights into pathogenesis from an autopsy series. Am J Pathol. 2016;186(12):3225–35.
Min L, Hodi FS, Giobbie-Hurder A, Ott PA, Luke JJ, Donahue H, Davis M, Carroll RS, Kaiser UB. Systemic high-dose corticosteroid treatment does not improve the outcome of ipilimumab-related hypophysitis: a retrospective cohort study. Clin Cancer Res. 2015;21(4):749–55.
Okano Y, Satoh T, Horiguchi K, Toyoda M, Osaki A, Matsumoto S, Tomaru T, Nakajima Y, Ishii S, Ozawa A, et al. Nivolumab-induced hypophysitis in a patient with advanced malignant melanoma. Endocr J. 2016;63(10):905–12.
Baxi S, Yang A, Gennarelli RL, Khan N, Wang Z, Boyce L, Korenstein D. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: systematic review and meta-analysis. BMJ. 2018;360:k793.
Ariyasu R, Horiike A, Yoshizawa T, Dotsu Y, Koyama J, Saiki M, Sonoda T, Nishikawa S, Kitazono S, Yanagitani N, et al. Adrenal insufficiency related to anti-programmed Death-1 therapy. Anticancer Res. 2017;37(8):4229–32.
Acknowledgements
Not applicable.
Funding
The authors did not receive any specific funding for this work.
Author information
Authors and Affiliations
Contributions
ST, MK, TN, MT and KM participated in the endocrinological treatment and data collection. ST, MK, TN, KM and IT participated in the oncological treatment and data collection. All authors contributed to data interpretation. ST wrote the manuscript with the assistance of all other authors. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tanaka, S., Kushimoto, M., Nishizawa, T. et al. Isolated ACTH deficiency during single-agent pembrolizumab for squamous cell lung carcinoma: a case report. Clin Diabetes Endocrinol 6, 1 (2020). https://doi.org/10.1186/s40842-019-0092-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40842-019-0092-9