Abstract
Introduction
Deaths from second-hand smoke (SHS) exposure are increasing, but there is not sufficient evidence to recommend a particular SHS intervention or intervention development approach. Despite the available guidance on intervention reporting, and on the role and nature of pilot and feasibility studies, partial reporting of SHS interventions is common. The decision-making whilst developing such interventions is often under-reported. This paper describes the processes and decisions employed during transitioning from the aim of adapting an existing mosque-based intervention focused on public health messages, to the development of the content of novel community-based Smoke-Free Home (SFH) intervention. The intervention aims to promote smoke-free homes to reduce non-smokers’ exposure to SHS in the home via faith-based messages.
Methods
The development of the SFH intervention had four sequential phases: in-depth interviews with adults in households in Dhaka, identification of an intervention programme theory and content with Islamic scholars from the Bangladesh Islamic Foundation (BIF), user testing of candidate intervention content with adults, and iterative intervention development workshops with Imams and khatibs who trained at the BIF.
Results
It was judged inappropriately to take an intervention adaptation approach. Following the identification of an intervention programme theory and collaborating with stakeholders in an iterative and collaborative process to identify barriers, six potentially modifiable constructs were identified. These were targeted with a series of behaviour change techniques operationalised as Quranic verses with associated health messages to be used as the basis for Khutbahs. Following iterative user testing, acceptable intervention content was generated.
Conclusion
The potential of this community-based intervention to reduce SHS exposure at home and improve lung health among non-smokers in Bangladesh is the result of an iterative and collaborative process. It is the result of the integration of behaviour change evidence and theory and community stakeholder contributions to the production of the intervention content. This novel combination of intervention development frameworks demonstrates a flexible approach that could provide insights for intervention development in related contexts.
Similar content being viewed by others
Introduction
Historically, behaviour change intervention content is under-reported [1], impacting replicability, subsequent development, and scalability. A recent review of second-hand smoke (SHS) intervention studies [2] indicated that partial reporting of SHS interventions is common. It was recommended that intervention reporting guidelines are adhered to and that comprehensive reporting of behaviour change techniques (BCTs) and the provision of a logic model linking BCTs to the intervention theory of change is mandated. The need to be pragmatic in resource-limited contexts is common in intervention development [3]. The decisions taken in these contexts and elsewhere may enlighten those seeking to understand what leads to successful intervention development. A range of theoretical models and intervention development approaches to protect children from SHS [4] have been proposed, but recent reviews of smoke-free homes (SFH) [5, 6] and of SHS interventions for children [7] have not provided the basis for specific recommendations. Hoddinott [8] suggests that a greater understanding of the effectiveness of interventions will result from transparent reporting of how stakeholder groups are involved in decision-making during the development of complex interventions. This paper describes the process of developing the content of a novel mosque-based smoke-free home (SFH) intervention in Bangladesh that has subsequently been trialled [9].
Key messages regarding feasibility
1) Previous work had identified concerns around the feasibility of developing smoke-free homes messages that could be delivered in mosques.
2) Our approach demonstrates it is feasible to develop explicitly faith-based messages for use in mosques by working iteratively with stakeholder groups from religious communities.
3) The reported intervention development utilised a 4-phase process for working with stakeholders from religious communities to develop faith-based intervention content.
Background
SHS is the combination of emissions of smoke emitted between a puff of lit tobacco and the smoke that is exhaled by smokers [10]. Children’s risks from asthma [11], acquiring lower respiratory tract infections [12, 13], and tuberculosis [14, 15] are all increased by exposure to SHS. Children living in smoking households are also at high risk of becoming adult smokers later [16]. Childhood exposure to SHS is strongly associated with the prevalence of adult smoking [17].
Whilst between 1990 and 2006, the estimated number of deaths attributed to SHS fell, it has subsequently increased, driven by increases in SHS exposure in South Asia, East Asia, and the Pacific [18]. The WHO estimates that 1.2 million deaths per year are attributable to non-smokers being exposed to SHS [19]. This research focuses on a setting-based approach [20], focussing on engendering a health-supporting environment [21] to protect non-smoking adults and children from the harms of SHS in their homes. There have been calls for research into the efficacy of health interventions that are delivered by Imams or in mosques [22, 23]. The work builds on the findings of a pilot trial conducted in England which concluded that an SFH intervention was acceptable to Muslim communities and feasible to deliver in mosques [24]. In the present work, the intervention development explicitly aimed to result in faith-based material directly targeted at smokers via faith leaders based in mosques (Imams and khatibs) for the planned trial [25] (MRC RGMR/P008941/1).
Methods
Development approach
The starting point of the intervention development approach was material arising from the UK-based MCLASS trial [26], for which a package of SFH materials was developed that drew upon consensus around the religious prohibition of the use of tobacco products among Muslims [27, 28], and evidence that a complex intervention that included a mosque-based component had promising effects on SFH prevalence [29]. The MCLASS intervention took a settings-based approach, seeking to support health-promoting environments. The intervention was tailored to the cultural values of the target population: South-Asian men ill-served by smoking cessation services that do not address cultural sensitivities [30,31,32]. Relatively few faith setting-based interventions have been developed for mosques [33].
A recent UK Medical Research Council (MRC)-funded project has produced a taxonomy of intervention development approaches for complex interventions [34]. This specified eight categories: partnership, target population-centred, evidence and theory-based, implementation-based, efficiency-based, stepped or phased-based intervention specific, and combination. Our development work does not fit neatly into this taxonomy, in that we had previously undertaken SHS intervention development in the UK [26]. We initially expected to undertake an intervention adaptation approach using the Programme Theory of Adapted Health Interventions [35] making use of the UK-based MCLASS trial materials [26]. However, subsequent process evaluation of the existing intervention [24] raised issues around the acceptability of religious teachers taking on a health promotion role, and it was reported that some participants were unhappy that the mosque was being used as a context for delivering health promotion messages:
When you come to the mosque, you want to pray, you know? And [its’] a place of worship really. And you don’t want to come here and do other things you know? You want to escape from these things you see. (FGD-Men) (p.300)
We subsequently looked to ayah (Quranic verse) for messages that supported SFH so that the messages were drawn from the Quran and would not be jarring for worshippers or out of place in mosques. Given the limited expertise of we in the Quranic scripture, it was felt important to undertake an intervention development process that examined the wider context of smoking and SFH, and following content development, put this before stakeholder groups in Bangladesh for iteration, including those with a scholarly understanding of Quranic scripture.
We elected to undertake a development process that consisted of four phases:
-
1)
Interviews exploring barriers and facilitators of SFH with adults from locations near the planned recruitment sites.
-
2)
Identification of an intervention programme theory and content with Islamic scholars from the Bangladesh Islamic Foundation (BIF) with expertise in Quranic scripture to identify candidate content
-
3)
User testing of candidate intervention content with adults.
-
4)
Iterative intervention development workshops with Imams and khatibs.
Phase 1—Interviews exploring barriers and facilitators of SFH
Face-to-face interviews were conducted from May to July 2017 in the Mirpur and Gulshan regions of Dhaka city with six men and two women (see Table 1).
Drawing upon prior work [36,37,38] and a relevant systematic review and thematic synthesis [39], a semi-structured interview schedule that explored smoking behaviours, and barriers and facilitators to an SFH intervention delivered within mosques by Imams was developed. Given the aforementioned process evaluation [24] had identified issues around the acceptability and feasibility of the use of mosques to disseminate SHS messages, we took this opportunity to elicit opinions on this. Interviews lasted between 23 and 48 min. They were audio-recorded and fully transcribed then translated from Bangla to English. The interview data were then analysed using deductive content analysis [40]. First a categorisation matrix was developed based on the interview schedule, piloted with one transcript, and set up in Excel. The data were coded to the matrix, and then, each category, e.g., smoking behaviours, was written up.
Phase 2—Identification of programme theory and content
The basis for the programme theory to guide the development of the content targeting SFH was planned to be selected following the face-to-face interviews. The aim was to identify evidence-based modifiable constructs present within the interview findings and map these to BCTs [41] that seemed likely to result in changes in those constructs based on study team expertise. These BCTs were then operationalised as intervention content with the support of Quranic verses (ayahs) and linked health messages. To seed the programme content design process, we sought advice from a Muslim colleague with knowledge of social cognitive constructs and the BCT taxonomy [41] as to relevant ayahs that supported health messages that could operate as the basis for BCTs. These were fed into the Arabic Quranic Search Tool, which is a semantic search tool for the Quran based on a Quranic ontology [42] to identify a long list of ayahs which matched related concepts. To select from these ayahs and messages, we collaborated with Islamic Scholars from the Bangladesh Islamic Foundation, a government organisation under the Ministry of Religious Affairs in Bangladesh whose role is to spread the values and ideals of Islam among people. The long list of ayahs was screened for those that mapped on to social cognitive constructs within our intervention programme theory. As such, these were ayahs that would support health messages that function as BCTs or prompts to perform BCTs that would potentially result in changes to the intervention programme theory constructs. Subsequently, these ayahs were then expanded upon into statements that could form the suggested basis for a Khutbah (sermon)—the time before Arabic Khutbah during Friday Jumu’ah prayers. The health messages connected ayahs to personal implications for individuals’ faith and tobacco use.
Phase 3—User testing of candidate intervention content
To test the understanding and acceptability of the selected ayahs and health messages, we employed a user testing methodology [43] using face-to-face interviews. This occurred between September and November 2017 in the Mirpur region of Dhaka. All 12 ayahs and associated health messages were tested with a small sample of men and women (n=6, see Table 2) within the communities where we planned to trial the intervention.
For each pair of ayah and health messages, the researcher read out the ayah and asked the participant what this meant to them. The health message was subsequently read to them, and questions probing their understanding were asked, including how the message linked to the ayah. Feedback on the clarity of wording and suggestions for improvement were also sought. Interviews lasted between 40 and 70 min. Data analysis was as described in phase 1.
Phase 4—Iterative intervention development workshops with Imams and khatibs
The iterative workshops were undertaken in two sessions (labelled A and B) with Imams/khatibs from 12 mosques (see Table 3). Imams are those who lead everyday prayers in the mosques. Khatib or khateebs are those who deliver Khutbah and lead the Friday prayers. All of the Imams/khatibs were attendees of the Imam Training Academy, Bangladeshi Islamic Foundation, part of the Ministry of Religious Affairs.
We employed the same user-testing methodology applied in Phase 3 [43]. Experience of, and views on, delivering health and behaviour change messages within their religious teaching were also discussed. The two workshops lasted 180 min each. Data analysis was as described in Phase 1.
Results
Phase 1—Interviews exploring barriers and facilitators of SFH
Smoking behaviours
There was typically one smoker in each participant’s home, often the interview participants themselves. The number of times they smoked in the home ranged from one to eight times a day, usually in the morning and at night, during the day the men were out at work. Some said that they try to smoke on the balcony or in an empty room, which was difficult for the three families who live together in one room. Only one smoker claimed to never smoke in the home.
I felt that the smoke will be harmful for my family members and I stopped smoking inside home. (P01: Male, 35 years, Smoker, highly educated)
Barriers and drivers to achieving an SFH
Whilst all interview participants knew of the risks of smoking to the smoker, knowledge of the dangers of SHS varied and was better among the more educated, although they still underestimated the extent of potential harm.
I know that it harms equally others who are around someone who is smoking. That is why I have quit smoking at home totally now. (P01: Male, 35 years, Smoker, highly educated)
The consensus was there were no disadvantages of having an SFH. Participants identified multiple benefits, mentioning particularly the positive impact on the health of family members, especially children. Indeed, this was seen to be the key motivator. Other benefits were seen to be eliminating the smell and improving air quality in the home, reducing the risk of an accidental fire and sons not copying their father’s smoking behaviour.
Everyone loves their children. People would be ready to do anything for the betterment of their children. If they stop smoking at home then the air of that house would not be polluted. Wives and children of smokers will be able to inhale clean air and they will remain healthy. There would not be any bad smell of cigarette smoke in clothing. The overall environment of home will remain very good. (P07: Male, 36 years, Smoker, moderately educated)
The key challenge to achieving an SFH was smokers ignoring requests to smoke outside the home. Several men acknowledged this, whilst one woman spoke of how it would be difficult for women to ask men to smoke outside, suggesting they may not listen or worse, react angrily. She hoped the men would be motivated themselves.
She tells me not to smoke inside home, she has told me. Then, sometimes, I stop smoking inside home, then maybe after a few days, I start smoking in the home again, you know. (P07: Male, 38 years, Smoker, not educated)
Motivating and convincing the smokers would be a challenge, I think. As in our society men are often dominating, it is not likely that all of them will listen, some of them may get angry hearing such things. In some families there might be conflict. If the smokers are motivated enough by themselves, it would be better. (P08: Female, 45 years, Non-smoker, highly educated)
Acceptability and feasibility of a mosque-based SHS intervention
All the interview participants thought it was a good idea to educate people about SHS through mosques because of the credibility and influence of the Imam as a religious leader, and the mix of people who would hear the messages. Most had not heard health messages in the mosque before.
Those who have faith in religion go to the mosque, that's why normally they should abide by the rules and regulations of the religion. As the Imam is a religious leader, people listen to him and discuss problems with him, if he talks about smoking, some people will definitely listen to those messages. (P01: Male, 35 years, Smoker, highly educated)
People who go to the mosque regularly and on time are mostly guardians from families, the young generation like us are less in number. So, by them (these guardians) these kinds of messages can spread to others. Another thing would be best if we can make women in our homes more aware and they will definitely be able to make sure that nobody smokes at home. (P06: Male, 34 years, Smoker, moderately educated)
The consensus was that the content of the messages would need to be tailored to the audience. Women and children would need knowledge about SHS to persuade family members not to smoke inside and to protect themselves from smoke, whereas the men would benefit from learning about SHS in the context of Islamic scripture.
Women also need awareness. They will then tell the smoker family members not to smoke inside home. If children get to know the harms of SHS they would then try to protect themselves from second-hand smoking. (P07: Male, 38 years, Smoker, not educated)
The messages should vary. In the mosque the Imam can tell people about these (messages) with hadiths and Quran teachings. But for women there can be other things. For children the message should be in such form that they can communicate with their parents. (P02: Male, 40 years, Smoker, limited ability to read)
In terms of feasibility, the time before Arabic Khutbah (when the largest proportion of a mosque’s congregation attends) was seen as the sensible time to deliver the messages as most men attend then, thus maximising the size of the audience.
We, poor people, rich people, everybody goes to Jum’ah prayer. It's like the Eid day. Old people, younger people, small children gather together. So, it would be good delivering these messages during Jum’ah prayer. Everybody will listen and give importance. (P05: Female, 42 years, Smoker, not educated)
Other ideas for message delivery were Quran classes (for children), Madrasa classes, and other congregations like Milad mahfil (a custom practised by many Muslims as an expression of reverence for Prophet Muhammad (PBUH)) and Waz mahfil (Islamic sermon in the communities) although these were acknowledged to reach fewer people and occur less frequently.
Phase 2—Identification of programme theory and content
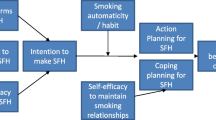
Based on the evidence of the previous utility of the model for understanding and intervening on smoking behaviour [44, 45], we selected the Theory of Planned Behaviour, extended with action planning and coping planning as the starting basis for the programme theory to guide the development of the intervention content (see Fig. 1) targeting SHS. The constructs we sought to operationalise drawn from this model were Attitude, Social Norms, Intention formation, Self-efficacy, Action Planning, and Coping planning. Using the interview findings and the selected constructs from the programme theory, a Muslim colleague with knowledge of social cognitive constructs and the BCT taxonomy [41] supplied a list of ayahs that could support messages to promote change in these potentially modifiable constructs that were identified as being present within the interview. The programme theory constructs findings were then mapped to BCTs [41] that seemed likely to result in changes in those constructs based on study team expertise and subsequently result in change in air quality (AQ) and smoke-free home (SFH) status. The list of ayahs, the constructs targeted, the health messages, and the BCTs the health messages were mapped to is contained in Table 4.
Phase 3—User testing of candidate intervention content results
All participants understood the general meaning of the ayahs and the health messages as well as the links between the two. Small edits to the precise wording of some of the public health messages were made, to improve comprehension; for example, for the message linked to Ayah Sura At-Takaathur (see Table 4, ayah 4), the concept of “worldly pleasure” was unclear to some leading to a suggestion to reword this. No major changes were deemed necessary at this stage.
Phase 4—Iterative intervention development workshops with Imams and khatibs Imams’ experience and views of delivering health promotion messages
There was a view among the Imams that they talk about health-related issues in the mosques only when directly relevant to religion, for example, addiction to smoking or alcohol or eating good foods; or when prompted by a current public health issue such as an outbreak of disease where they may advise on disease prevention strategies.
Addiction and smoking are sometimes discussed in mosques because it is destroying our children and adults, taking them away from Allah. There are young people who are always behaving badly to their parents. They are acting unaware of the consequences both in this world and the hereafter. (B07: Imam, khatib and Principal)
Allah has even told us to eat pleasant foods... Drugs, smoking, these are already Haram by Allah's law and moreover there are unpalatable, stinky food, which is why these are harmful for health. (A06: Imam)
A few days ago, city corporation people came to us and told us to talk on Chikungunya in Jumu’ah prayers. So, we did this. (B03: Imam and khatib)
The exception was during Ramadan when there is more emphasis on changing people’s “bad” behaviours and helping them to focus more on praying to Allah.
They were generally motivated to deliver health messages in mosques and familiar with including messages during Khutbah in Jumu’ah prayer about behaviours that harm people both physically and spiritually. Educating men about the risks of smoking and SHS was seen as a good idea, particularly as people rarely learn about SHS, so the intervention was considered to represent an opportunity, with the input of international researchers seen as an asset. Additionally, this perceived scientific foundation of the intervention was seen as important as Imams did not consider themselves experts on public health, rather their expertise was in spiritual matters.
Actually, you have to pray to Allah from Dunya (this world). After death, there is no chance for earning good deeds. So, for earning good deeds, the first condition is Haya (life). Abstaining from addiction what Allah prohibited and what the prophet (PBUH) did and encouraged us to do, if we follow those, the Hayat will increase. (A01: Imam)
If we can tell them about some medical facts on smoking along with religious messages on it, they will be more aware of it. (B04: Imam)
We have both indirect and direct smoking here which is very bad. People do not hear much about second-hand smoking from anyone I guess. (B02: Iman and Teacher)
So, if we get a booklet or guideline including information on medical science, and if the messages are included by studying Quran and Hadith, then these will be more acceptable. People will understand that not only Imams know about Quran and Hadiths but also are knowledgeable of other fields. (A02: Iman and khatib)
They were also happy to deliver messages about planning, attempting, and failing to change behaviours, observing that people are used to this, and Islam teaches them how to face such situations, with Imams seen as a trusted source of support.
I think this is a great opportunity for Imams and common people because thousands of people can be reached with these messages and thus, Imams can make more people aware. (A05: Imam and khatib)
Jumu’ah prayers on Fridays was seen as the most appropriate time to deliver the messages, as this is when there are large numbers of people in the mosque, and they have time to elaborate on the meaning. There was a view among some that it would be important to deliver a message one week, discuss it the next week, and then return to it several weeks later as a reminder.
Feedback on ayahs and health messages
Imams were keen to undertake a careful check of the selected ayahs and proposed links with health messages. Some wanted more time outside of the workshop to do this work, whilst others advised that alims (Islamic scholars) should review the final list of ayahs and associated health messages.
There was agreement that the same ayahs and linked public health messages were appropriate for all mosques. The Imams’ suggestions for the 12 ayahs (listed in Table 4) are summarised below. The consensus across both workshops was that ayahs 3, 5, 7, 9, and 12 were appropriate and that ayah 4 was not suitably linked to the public message, although no one had an idea for a replacement. For the others, suggestions for alternatives were offered. These were usually to avoid misinterpretation or strengthen the take-home message. For two ayahs, changes were proposed to correct the meaning in the context of Islamic scripture.
Ayahs 1 and 10 were considered by some Imams to be open to misinterpretation. For Ayah 1, there was some concern that people might think that smoking is beneficial. Ayah 10 was seen as confusing about the type of knowledge being referred to; it should be understood to be knowledge of religion not knowledge of the harms of SFH. For ayahs 6 and 12, some Imams wanted to strengthen the message about the forgiveness of Allah. Alternatives for ayah 8 were offered to further encourage people to change their smoking and second-hand smoke behaviours by emphasising the importance of following the life and guidance of the prophet.
The two ayahs that were questioned in terms of religious accuracy were 2 and 11. For ayah 2, precision was needed that it is the Imam (not the scientist) who has authority to advise on what harms and heals to be consistent with the laws of Sariah. For ayah 11, the selected ayah was referring to divorce hence inappropriate.
As a result of the workshops, half the Ayahs were replaced with different Ayahs that better conveyed the messages or were more closely related to the public health messages targeted to be delivered. Ayahs 1, 6, 8, 10, 11, and 12 were changed. Ayahs 1, 8, 10, 11, and 12 were replaced with Ayahs suggested by the scholars of the Islamic Foundation, Bangladesh, and Ayah 6 was replaced with another Ayah chosen by ARK researchers (see Table columns 6 & 7).
Format of the intervention content
The final version of the intervention was formatted as a booklet for Imams that contained the Arabic ayah, a translation into Bangla, and the related health message (see Fig. 2 for examples translated into English).
The intervention booklet finally contained 12 ayah and related health messages in total (see Table 1 columns 6 & 7). Training on delivery of the intervention was provided over a half-day and was supported by a training manual. Training materials are available at [https://www.york.ac.uk/healthsciences/research/public-health/projects/mclass11/#tab-3]. Imams or khatibs in the mosques that were randomised to deliver the SFH intervention received copies of the intervention booklet to distribute to their congregation members after Friday Jumu’ah prayers or in study circles. Intervention delivery started immediately after training and continued for 12 weeks. Full details of the trial procedures have been previously published [9].
Discussion
The intervention development process reported here primarily took an evidence and theory-based approach [34], based on the MRC Framework [46, 47], in common with multiple approaches to intervention development [48]. Additionally, we took a partnership approach and engaged with stakeholder groups to both generate ideas about components and features of the intervention [49] and make decisions about the content, format, and delivery of the intervention [48]. As such, this was a combination approach to intervention development [34].
Summary of this approach
In accordance with MRC guidance [46], considerable resources were invested to develop an intervention with a conceivable intervention effect on SFHs. This process benefitted from intervention development that had previously been undertaken as part of the UK MCLASS trial [1, 24, 26], as well as intervention development work that preceded this [29]. The four phases undertaken were resource-consuming. However, each phase either directly or indirectly supported the creation or adaption of intervention content, with interviews exploring barriers and facilitators of SFH with adults, subsequent identification of an intervention programme theory and population of initial content with Quranic scripture, user testing of candidate intervention content with adults that resulted in minor changes to aid understanding, and iterative intervention development workshops with Imams and khatibs that resulted in major changes to the content to better reflect Islamic scholarship. The paucity of evidence as to effective SFH interventions [5, 6], and the previously highlighted concerns about intervention content [24], provided the impetus to appropriately support engagement with stakeholders to understand the religious and socio-cultural sensitivities of promoting SFH in a mosque setting [30, 50]. This approach reflects calls to conceptualise stakeholder involvement as an ongoing, iterative process [51, 52], and represents the efforts to develop shared terminology, successful prioritisation of early and consistent engagement, and recognition of stakeholders’ contributions [53].
Limitations
This intervention has subsequently been trialled [9] and found not to be effective in reducing household SHS exposure compared with usual services. However, further process evaluation and analysis of secondary outcomes [25] is planned that will explore effects on hypothesised intervention casual pathways and intervention fidelity [54].
We benefited from generous support from colleagues with deep knowledge of ayahs, social cognition models, and/or the behaviour change technique taxonomy [41]. Additionally, access to the Quranic Search Tool [42] provided a starting point for engagement with faith leaders that would have been difficult to replicate without significant external support. The ease with which these resources can be replicated is not obvious but speak to the necessity to properly resource intervention development and/or adaptation activities in culturally sensitive settings [53].
This work predates a landmark series of studies [55,56,57] that triangulated evidence for links between social cognitive constructs and BCTs [41]. Whilst prior to the availability of the Theory and Technique Tool that resulted from these studies, it was typical as part of an intervention development process to make use of study team expertise to map social cognitive constructs identified through qualitative or quantitative inquiry to BCTs, and this is a less robust method than the evidence synthesis and expert consensus approach that provided the data that is now available to support the mapping of such links. As such, the BCT mapping upon which we based our selection of ayahs may be less than optimal.
Conclusion
This religious community-based intervention to reduce SHS exposure at home and improve lung health among non-smokers in Bangladesh is the result of an iterative and collaborative 4-stage process. It makes use of behaviour change theory to support faith-community contributions to the production of culturally sensitive intervention content suitable for a mosque-based setting. Whilst further process evaluation is necessary to understand its failure to affect SHS [9], this novel combination of intervention development framework components demonstrates a flexible approach that could provide insights for intervention development in related culturally sensitive contexts that could support health behaviour change.
Availability of data and materials
De-identified participant data will be made available from the point of and up to 5 years after the acceptance for publication. These data can be requested from the Principal Investigator (Prof Kamran Siddiqi; kamran.siddiqi@york.ac.uk) and will be shared after the provision of a methodologically sound proposal, and only under a data-sharing agreement that provides for commitment to using the data only for research purposes and not to identify any individual participant, securing the data using appropriate computer technology, and destroying or returning the data after analyses are completed. The proposals will be assessed and approved by members of the Programme Management Group. The intervention manual and indoor-air-quality feedback leaflet are available on the study webpage: https://www.york.ac.uk/healthsciences/research/public-health/projects/mclass11/#tab-3.
References
Ainsworth H, Shah S, Ahmed F, Amos A, Cameron I, Fairhurst C, et al. Muslim communities learning about second-hand smoke (MCLASS): study protocol for a pilot cluster randomised controlled trial. Trials. 2013;14:295.
Dherani M, Zehra SN, Jackson C, Satyanaryana V, Huque R, Chandra P, et al. Behaviour change interventions to reduce second-hand smoke exposure at home in pregnant women–a systematic review and intervention appraisal. BMC Pregnancy Childbirth. 2017;17(1):1–10.
Turner KM, Rousseau N, Croot L, Duncan E, Yardley L, O’Cathain A, et al. Understanding successful development of complex health and healthcare interventions and its drivers from the perspective of developers and wider stakeholders: an international qualitative interview study. BMJ Open. 2019;9(5):e028756.
Gehrman CA, Hovell MF. Protecting children from environmental tobacco smoke (ETS) exposure: a critical review. Nicotine Tob Res. 2003;5(3):289–301.
Baxter S, Blank L, Everson-Hock ES, Burrows J, Messina J, GuillaUme L, et al. The effectiveness of interventions to establish smoke-free homes in pregnancy and in the neonatal period: a systematic review. Health Educ Res. 2011;26(2):265–82.
Behbod B, Sharma M, Baxi R, Roseby R, Webster P. Family and carer smoking control programmes for reducing children's exposure to environmental tobacco smoke. Cochrane Database Syst Rev. 2018;1(1):CD001746. https://doi.org/10.1002/14651858.CD001746.pub4.
Rosen LJ, Myers V, Hovell M, Zucker D, Noach MB. Meta-analysis of parental protection of children from tobacco smoke exposure. Pediatrics. 2014;133(4):698–714.
Hoddinott P. A new era for intervention development studies. In: BioMed Central; 2015.
Mdege ND, Fairhurst C, Wang H-I, Ferdous T, Marshall A-M, Hewitt C, et al. Efficacy and cost-effectiveness of a community-based smoke-free-home intervention with or without indoor-air-quality feedback in Bangladesh (MCLASS II): a three-arm, cluster-randomised, controlled trial. Lancet Global Health. 2021;9(5):e639–50.
Satcher D. Health effects of exposure to environmental tobacco smoke: the report of the california environmental protection agency: DIANE Publishing; 2000.
Burr ML, Anderson H, Austin J, Harkins L, Kaur B, Strachan D, et al. Respiratory symptoms and home environment in children: a national survey. Thorax. 1999;54(1):27–32.
Ashley MJ, Ferrence R. Reducing children’s exposure to environmental tobacco smoke in homes: issues and strategies. Tobacco Control. 1998;7(1):61–5.
Jones LL, Hassanien A, Cook DG, Britton J, Leonardi-Bee J. Parental smoking and the risk of middle ear disease in children: a systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2012;166(1):18–27.
Leung CC, Lam TH, Ho KS, Yew WW, Tam CM, Chan WM, et al. Passive smoking and tuberculosis. Arch Int Med. 2010;170(3):287–92.
Lin H-H, Ezzati M, Murray M. Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. Plos Med. 2007;4(1):e20.
Amos A, Hastings G, Angus K, Bostock Y, Fidler J. A review of young people and smoking in England: Public Health Research: Consortium York, UK; 2009.
Mbulo L, Palipudi KM, Andes L, Morton J, Bashir R, Fouad H, et al. Secondhand smoke exposure at home among one billion children in 21 countries: findings from the Global Adult Tobacco Survey (GATS). Tob Control. 2016;25(e2):e95–e100.
Yousuf H, Hofstra M, Tijssen J, Leenen B, Lindemans JW, van Rossum A, et al. Estimated worldwide mortality attributed to secondhand tobacco smoke exposure, 1990-2016. JAMA Netw Open. 2020;3(3):e201177.
Tobacco. 2021. https://www.who.int/news-room/fact-sheets/detail/tobacco.
Tones K, Green J. Health promotion: planning and strategies: Sage; 2004.
Neufeld J, Kettner J. The settings approach in public health: thinking about schools in infectious disease prevention and control. In: National collaborative center of infectious diseases: University of Manitoba …; 2014.
Grace C, Begum R, Subhani S, Kopelman P, Greenhalgh T. Prevention of type 2 diabetes in British Bangladeshis: qualitative study of community, religious, and professional perspectives. BMJ. 2008;337.
Mustafa Y, Baker D, Puligari P, Melody T, Yeung J, Gao-Smith F. The role of imams and mosques in health promotion in Western societies—a systematic review protocol. Syst Rev. 2017;6(1):1–5.
King R, Warsi S, Amos A, Shah S, Mir G, Sheikh A, et al. Involving mosques in health promotion programmes: a qualitative exploration of the MCLASS intervention on smoking in the home. Health Educ Res. 2017;32(4):293–305.
Mdege N, Fairhurst C, Ferdous T, Hewitt C, Huque R, Jackson C, et al. Muslim Communities Learning About Second-hand Smoke in Bangladesh (MCLASS II): study protocol for a cluster randomised controlled trial of a community-based smoke-free homes intervention, with or without Indoor Air Quality feedback. Trials. 2019;20(1):11.
Shah S, Ainsworth H, Fairhurst C, Tilbrook H, Sheikh A, Amos A, et al. Muslim communities learning about second-hand smoke: a pilot cluster randomised controlled trial and cost-effectiveness analysis. NPJ Prim Care Respir Med. 2015;25(1):1–7.
Ghouri N, Atcha M, Sheikh A. Influence of Islam on smoking among Muslims. BMJ. 2006;332(7536):291–4.
Haq M, Sufi A, Haque A, Hassan S, Rehman H, Abaza F, et al. Eliminate second-hand smoking from islamic campuses in North America. J IMA. 2010;42(3):97.
Siddiqi K, Sarmad R, Usmani R, Kanwal A, Thomson H, Cameron I. Smoke-free homes: an intervention to reduce second-hand smoke exposure in households. Int J Tuberc Lung Dis. 2010;14(10):1336–41.
Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10–21.
Bush J, White M, Kai J, Rankin J, Bhopal R. Understanding influences on smoking in Bangladeshi and Pakistani adults: community based, qualitative study. BMJ. 2003;326(7396):962.
Highet G, Ritchie D, Platt S, Amos A, Hargreaves K, Martin C, et al. The re-shaping of the life-world: male British Bangladeshi smokers and the English smoke-free legislation. Ethn Health. 2011;16(6):519–33.
Liu JJ, Wabnitz C, Davidson E, Bhopal RS, White M, Johnson MR, et al. Smoking cessation interventions for ethnic minority groups—a systematic review of adapted interventions. Prev Med. 2013;57(6):765–75.
O’Cathain A, Croot L, Sworn K, Duncan E, Rousseau N, Turner K, et al. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud. 2019;5(1):1–27.
Liu J, Davidson E, Bhopal R, White M, Johnson M, Netto G, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technol Assess (Winchester, England). 2012;16(44):1.
Jackson C, Huque R, Satyanarayana V, Nasreen S, Kaur M, Barua D, et al. “He Doesn’t Listen to My Words at All, So I Don’t Tell Him Anything”—a qualitative investigation on exposure to second hand smoke among pregnant women, their husbands and family members from rural Bangladesh and urban India. Int J Environ Res Public Health. 2016;13(11):1098.
Sharma T, Khapre M. Exposure of second hand smoke in women and children: a narrative review. J Fam Med Prim Care. 2021;10(5):1804.
Robin RC, Noosorn N, Alif SM. Secondhand smoking among children in rural households: a community based cross-sectional study in Bangladesh. Osong Public Health Res Perspect. 2020;11(4):201.
Passey ME, Longman JM, Robinson J, Wiggers J, Jones LL. Smoke-free homes: what are the barriers, motivators and enablers? A qualitative systematic review and thematic synthesis. BMJ Open. 2016;6(3):e010260.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Alqahtani M, Atwell E. Arabic Quranic search tool based on ontology: Springer; 2016. p. 478–85.
Theo Raynor D, Blackwell K, Middleton W. What do writers need to know about user testing? Medical Writing. 2015;24(4):215–8.
Joveini H, Dehdari T, Hashemian M, Maheri M, Shahrabadi R, Rohban A, et al. Effects of an educational intervention on male students’ intention to quit water pipe smoking: an application of the theory of planned behavior (TPB) and health action process approach (HAPA). J Educ Community Health. 2020;7(2):73–80.
McMillan B, Higgins AR, Conner M. Using an extended theory of planned behaviour to understand smoking amongst schoolchildren. Addict Res Theory. 2005;13(3):293–306.
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337.
Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321(7262):694–6.
O'Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9(8):e029954.
Locock L, Robert G, Boaz A, Vougioukalou S, Shuldham C, Fielden J, et al. Testing accelerated experience-based co-design: a qualitative study of using a national archive of patient experience narrative interviews to promote rapid patient-centred service improvement. Health Serv Delivery Res. 2014;2(4).
Davidson EM, Liu JJ, Bhopal R, White M, Johnson MR, Netto G, et al. Behavior change interventions to improve the health of racial and ethnic minority populations: a tool kit of adaptation approaches. Milbank Q. 2013;91(4):811–51.
Boaz A, Hanney S, Borst R, O'Shea A, Kok M. How to engage stakeholders in research: design principles to support improvement. Health Res Policy Syst. 2018;16(1):60.
Deverka PA, Lavallee DC, Desai PJ, Esmail LC, Ramsey SD, Veenstra DL, et al. Stakeholder participation in comparative effectiveness research: defining a framework for effective engagement. J Comp Eff Res. 2012;1(2):181–94.
Heckert A, Forsythe LP, Carman KL, Frank L, Hemphill R, Elstad EA, et al. Researchers, patients, and other stakeholders’ perspectives on challenges to and strategies for engagement. Res Involv Engagem. 2020;6:60.
Ahmed S, Khan JA. Disseminating public health messages about second-hand smoking through mosque congregations in Bangladesh. Lancet Global Health. 2021;9(5):e567–8.
Carey RN, Connell LE, Johnston M, Rothman AJ, De Bruin M, Kelly MP, et al. Behavior change techniques and their mechanisms of action: a synthesis of links described in published intervention literature. Ann Behav Med. 2019;53(8):693–707.
Connell LE, Carey RN, De Bruin M, Rothman AJ, Johnston M, Kelly MP, et al. Links between behavior change techniques and mechanisms of action: an expert consensus study. Ann Behav Med. 2019;53(8):708–20.
Johnston M, Carey RN, Connell Bohlen L, Johnston DW, Rothman A, de Bruin M, et al. Linking behavior change techniques and mechanisms of action: triangulation of findings from literature synthesis and expert consensus. PsyArXiv. 2018;10.
Acknowledgements
This trial was funded by the Medical Research Council UK under the Global Alliance for Chronic Diseases research programme (MR/P008941/1). Our thanks to Dr Hetaf Alammar for generously reviewing the intervention programme theory and providing the initial list of related ayahs. Thanks to Dr. Mohammed Alqathani and Professor Eric Atwell for generating a further list of related ayahs using the Arabic Quranic search tool (Alqathani & Atwell, 2016). Thanks to Kazi Nurul Islam, Secretary, Islamic Foundation for his facilitation in approving the intervention materials. We are grateful to the Islamic Foundation, Bangladesh; participating scholars, imams, and khatibs; and all participants who have contributed.
Funding
Medical Research Council UK under the Global Alliance for Chronic Diseases research programme. Grant number MR/P008941/1.
Author information
Authors and Affiliations
Consortia
Contributions
IK drafted the manuscript, conceived the intervention development approach, and contributed to the design, conduct, and interpretation of the findings. ZAA contributed to the design, conduct, interpretation of findings, and writing of the manuscript. CJ contributed to the intervention development approach, design, conduct, interpretation of the findings, and writing of the manuscript. RH contributed to the design and conduct, and interpretation of the findings. NM contributed to the design, conduct, interpretation of the findings, and writing of the manuscript. KS conceived the intervention idea and contributed to the design, conduct, interpretation of the results, and writing of the manuscript. All authors participated in manuscript revisions and read and approved the final manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kellar, I., Al Azdi, Z., Jackson, C. et al. Muslim Communities Learning About Second-hand Smoke in Bangladesh (MCLASS II): a combined evidence and theory-based plus partnership intervention development approach. Pilot Feasibility Stud 8, 136 (2022). https://doi.org/10.1186/s40814-022-01100-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-022-01100-5