Abstract
Background
The trunk is the foundation for transfer and dissipation of forces throughout the lower extremity kinetic chain. Individuals with knee disorders may employ trunk biomechanical adaptations to accommodate forces at the knee or compensate for muscle weakness. This systematic review aimed to synthesize the literature comparing trunk biomechanics between individuals with knee disorders and injury-free controls.
Methods
Five databases were searched from inception to January 2022. Observational studies comparing trunk kinematics or kinetics during weight-bearing tasks (e.g., stair negotiation, walking, running, landings) between individuals with knee disorders and controls were included. Meta-analyses for each knee disorder were performed. Outcome-level certainty was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE), and evidence gap maps were created.
Results
A total of 81 studies investigating trunk biomechanics across six different knee disorders were included (i.e., knee osteoarthritis [OA], total knee arthroplasty [TKA], patellofemoral pain [PFP], patellar tendinopathy [PT], anterior cruciate ligament deficiency [ACLD], and anterior cruciate ligament reconstruction [ACLR]). Individuals with knee OA presented greater trunk flexion during squatting (SMD 0.88, 95% CI 0.58–1.18) and stepping tasks (SMD 0.56, 95% CI 0.13–.99); ipsilateral and contralateral trunk lean during walking (SMD 1.36; 95% CI 0.60–2.11) and sit-to-stand (SMD 1.49; 95% CI 0.90–2.08), respectively. Greater trunk flexion during landing tasks in individuals with PFP (SMD 0.56; 95% CI 0.01–1.12) or ACLR (SMD 0.48; 95% CI 0.21–.75) and greater ipsilateral trunk lean during single-leg squat in individuals with PFP (SMD 1.01; 95% CI 0.33–1.70) were also identified. No alterations in trunk kinematics of individuals with TKA were identified. Evidence gap maps outlined the lack of investigations for individuals with PT or ACLD, as well as for trunk kinetics across knee disorders.
Conclusion
Individuals with knee OA, PFP, or ACLR present with altered trunk kinematics in the sagittal and frontal planes. The findings of this review support the assessment of trunk biomechanics in these individuals in order to identify possible targets for rehabilitation and avoidance strategies.
Trial registration: PROSPERO registration number: CRD42019129257.
Similar content being viewed by others
Key Points
-
(1)
Individuals with knee osteoarthritis, patellofemoral pain, or anterior cruciate ligament reconstruction present with altered trunk kinematics in the sagittal and frontal planes, while no trunk alterations were identified in individuals with total knee arthroplasty.
-
(2)
There is a noticeable lack of investigation of trunk kinematics and kinetics in individuals with patellar tendinopathy and anterior cruciate ligament deficiency.
-
(3)
Assessing trunk kinematics in clinical practice may help to identify possible targets for rehabilitation and avoidance strategies in individuals with osteoarthritis, patellofemoral pain, or anterior cruciate ligament reconstruction.
Introduction
Knee disorders are very common [1,2,3,4] and are linked to prolonged recovery periods and higher reinjury rates [5,6,7,8]. Pain is reported to continue for 5–8 years after physical therapies for patellofemoral pain (PFP) in 1 of every 2 patients [5], while nearly 1 in 4 young athletic patients who sustain an anterior cruciate ligament (ACL) injury and return to high-risk sport will sustain another ACL injury at some point in their career [6]. To improve secondary and tertiary prevention efforts, a greater understanding of the effects of knee disorders on trunk biomechanics is required given its influence on knee loading.
The trunk accounts for 38% of whole-body center of mass position [9] and is the foundation for transfer and dissipation of forces throughout the lower extremity kinetic chain during weight-bearing tasks [10,11,12]. For example, landing from a jump with the trunk flexed was reported to result in 28% less quadriceps activation when compared to landing with the trunk more erect [13]. Conversely, hip extensor weakness is commonly reported in individuals with knee disorders [14,15,16], which would be expected to be compensated with a more erect trunk posture during dynamic activities [10]. Such trunk motion would increase the demand on the quadriceps and could have implications for several injuries at the knee, including patellar tendinopathy, PFP, and ACL strain (resulting from quadriceps-induced anterior shear forces acting on the tibiofemoral joint) [10]. In the frontal plane, increases in ipsilateral trunk lean (i.e., toward the stance limb) can reduce medial knee load in a dose–response manner [17]. Although this compensatory motion may be beneficial for individuals with medial knee osteoarthritis (OA) [17], ipsilateral trunk lean could create a valgus moment at the knee [10], which may be associated with ACL injury [18] and PFP [19]. A reduction of knee valgus has also been reported to be associated with decreased knee pain levels [20].
Previous systematic reviews have not synthesized the literature to identify trunk biomechanics in individuals with knee disorders. Such a review would inform researchers and clinicians on the utility of assessing trunk biomechanics in different types of knee disorders to identify possible targets for intervention. Therefore, the aims of this systematic review were to: (1) determine whether trunk biomechanics are altered in individuals with knee disorders compared to controls; (2) determine the level of the evidence certainty available; and (3) identify evidence gaps in the literature.
Methods
This systematic review has been conducted and reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) [21] and Prisma in Exercise, Rehabilitation, Sport medicine and SporTs science (PERSiST) guidelines [22]. The review protocol was pre-registered in PROSPERO (registration number: CRD42019129257).
Data Sources and Search Strategy
A comprehensive literature search in Medline via OVID, Embase via OVID, CINAHL via EBSCOhost, SPORTDiscus via EBSCOhost, and Web of Science was performed from database inception to January 2022. The search strategy performed in Medline is presented in Additional file 1A. The electronic search was complemented by hand-searching the references of the retrieved studies and citation tracking of the original studies in Google Scholar.
Selection Criteria
Observational cross-sectional and case–control studies comparing trunk biomechanics (kinematics or kinetics) during weight-bearing tasks (e.g., stair negotiation, walking, running, landings) between injury-free individuals (controls) and those with knee disorders were included. Knee disorders included were: knee OA, PFP, ACL deficiency [ACLD], and patellar tendinopathy [PT], total knee arthroplasty [TKA], and ACL reconstruction [ACLR]. As the prevalence of co-existing tibiofemoral and patellofemoral OA (40%) is higher than isolated tibiofemoral (4%) or patellofemoral (24%) OA [23], no compartment-specific OA was determined in the included studies (i.e., knee OA). Studies were excluded if they did not report a comparator group composed by controls, or investigated laboratory-induced tasks (e.g., balance provocations, sudden force release or external perturbation, laboratory-induced trips). Randomized controlled trials, cluster clinical trials, controlled (non-randomized) clinical trials, cadaveric studies, review papers, editorials, abstracts, and letters were not included. There was no restriction on participant sex or age, or year of publication. Language was limited to English, Portuguese or Spanish.
Review Process
A single investigator (MCW) exported all studies identified by the electronic search to Covidence (Collins St, Melbourne, AU) where duplicates were removed. Titles, abstracts, and full-text screening were performed independently for eligibility by two reviewers (MCW and RVB). Any disagreements were resolved by consensus and the input of a third reviewer (MHMD).
Methodological Quality Assessment
Methodological quality assessment was performed using a modified 14-item Downs and Black checklist [24, 25]. The modified Downs and Black checklist was used instead of the modified Newcastle–Ottawa scale as registered in PROSPERO because the former has been used in similar systematic reviews [26,27,28] and had good interrater reliability [29]. The domains considered not applicable to assess observational cross-sectional studies were removed resulting in a modified version of 14 domains [24, 30]. Studies were considered as ‘high quality’ (HQ) when scoring 11 or higher, ‘moderate quality’ (MQ) when scoring from 6 to 10 and ‘low quality’ (LQ) when scoring 5 or lower [28]. Assessments were performed independently by two reviewers (MCW and MHMD), and disagreements were resolved by consensus and the input of a third reviewer (RVB).
Data Extraction
Study characteristics including publication details (e.g., author, year, study design), population characteristics (e.g., knee injury/surgery, number of participants, age, sex, body mass index), procedures (e.g., task, instrumentation), and outcomes were extracted and entered into Excel by one reviewer (MCW). All extracted data were double-checked by a second reviewer (MHMD). If necessary, authors were contacted via e-mail for further information to facilitate accurate data extraction. When possible, data reported as graphs were digitized and extracted using WebPlotDigitizer 4.0 (Ankit Rohatgi, San Francisco, CA).
Data Analysis
Extracted data on trunk biomechanics were grouped according to population, measurement method (e.g., kinematics, kinetics), planes of motion (i.e., sagittal, frontal, or transverse planes), outcome (e.g., peak or range of motion [RoM], angle at initial contact [IC], or take-off), and task. Similar tasks were separated into categories: walking, running, stepping tasks (e.g., stair ascent, stair descent, step-down task), squatting tasks (e.g., single-leg squat, sit-to-stand), landing and jumping tasks. Outcomes were separately analyzed considering the task phase (e.g., IC, weight acceptance [peak/RoM], or take-off) or whether they were relative to another parameter (e.g., peak vertical ground reaction force) as they may represent different joint mechanics [31,32,33,34]. When a study reported outcomes that measured peak angle and RoM (which are similar underlying parameters), they were pooled together. When a study used a waveform analysis (e.g., statistical parametric mapping), qualitative synthesis was performed as data were unable to be pooled. Where two or more studies were available, data were pooled in a meta-analysis using a random effects model (Review Manager Version 5.3.). Standardized mean differences (SMD) and 95% confidence intervals (CIs) were calculated for all variables analyzed in the knee disorders versus control groups by dividing the difference between groups by the pooled SD. SMD were interpreted according to Cohen’s criteria: large effect defined as ≥ 0.8, moderate as > 0.5 and < 0.8, small effect as ≤ 0.5 and ≥ 0.2, and < 0.2 as no effect [35]. Statistical heterogeneity was quantified by the I2 statistic where I2 < 50% was considered not important, 50–75% as moderate, and > 75% as high heterogeneity [36]. Sensitivity analyses were performed by removing studies when there was high heterogeneity or where we used a digitizing software to extract data from graphs.
Level of Certainty
Following the Cochrane recommendation [37], outcome-level certainty was assessed for all meta-analyses using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE). A modified version proposed for observational studies was used as per recent publications [38,39,40]. The criteria adopted in this review comprise 4 domains: (1) risk of bias (i.e., more than 25% of participants from studies with a high risk of bias; studies scoring as low quality in the Downs and Black checklist were rated as high risk of bias), (2) inconsistency (i.e., substantial heterogeneity across the studies [− 1 for I2 > 50%; − 2 for I2 > 75%]), (3) imprecision (i.e., total sample size < 100 participants per group, large confidence intervals or confidence intervals that do not overlap), and (4) indirectness (i.e., study population and outcome measures do not align with the purpose of the review) (Table 1). Publication bias (i.e., visual inspection of funnel plot’s asymmetry or Egger’s test P < 0.10) was assessed when at least 10 studies were pooled [37, 38]. We downgraded one level for each domain not met from ‘high’ to ‘very low.’ Inconsistency was the only domain that could be double downgraded. We upgraded one level if more than 50% of pooled studies had a large effect (i.e., Cohen’s criteria ≥ 0.8). Levels of certainty were defined as follows:
-
1.
High: Further research is very unlikely to change confidence in the estimate of the effect;
-
2.
Moderate: Further research is likely to have an important impact on confidence in the estimate of the effect and may change the estimate;
-
3.
Low: Further research is very likely to have an important impact on confidence in the estimate of the effect and is likely to change the estimate;
-
4.
Very low: There is very little confidence in the effect estimate.
Evidence Gap Map
An evidence gap map was created to provide an overview of the evidence available investigating trunk biomechanics in individuals with knee disorders. The evidence gap map allows the identification of outcomes with sufficient or insufficient evidence due to the number of similar studies [41]. For the presentation of the evidence, all data were grouped according to measurement method, planes of motion, outcome, and task categories as previously mentioned. To assess levels of evidence synthetized in the evidence gap map, an updated version of van Tulder’s criteria was used as listed below [42]:
-
1.
Strong evidence: provided by pooled results derived from three or more studies, including a minimum of two high-quality studies, which were statistically homogeneous (P > 0.05); may be associated with a statistically significant or non-significant pooled result.
-
2.
Moderate evidence: provided by statistically significant pooled results derived from multiple studies that were statistically heterogeneous (P < 0.05), including at least one high-quality study; or from multiple low-quality studies, which were statistically homogeneous (P > 0.05).
-
3.
Limited evidence: provided by results from one high-quality study or multiple low-quality studies that are statistically heterogeneous (P < 0.05).
-
4.
Very limited evidence: provided by results from one low-quality study.
-
5.
Conflicting evidence: provided by inconsistent findings among multiple trials and derived from multiple studies regardless of quality that are statistically heterogeneous.
Results
Search Results and Studies’ Characteristics
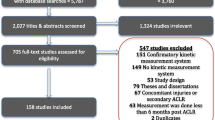
The electronic database search yielded 14,463 studies initially (Fig. 1). Following the removal of duplicates, 10,676 studies were screened by title and abstracts for inclusion. Of these, 158 full-text studies were screened for inclusion and 83 studies did not meet eligibility criteria. Reasons for exclusion are presented in Additional file 1B. Six additional studies were also included based on hand-searching. Eighty-one studies were then included in this review.
From the 81 included studies, 26 studies investigated individuals with OA [43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68], 7 investigated individuals with TKA [69,70,71,72,73,74,75], 19 investigated individuals with PFP [76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94], 2 investigated individuals with PT [95, 96], 5 investigated individuals with ACLD [97,98,99,100,101], 19 investigated individuals with ACLR [34, 102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119], and 3 investigated more than 1 knee disorder (e.g., ACLD and ACLR, knee OA and TKA) [120,121,122].
Fifty-eight studies investigated three-dimensional trunk kinematics in the sagittal plane (knee OA [n = 16], TKA [n = 7], PFP [n = 13], PT [n = 2], ACLD [n = 3], ACLR [n = 17]), 54 in the frontal plane (knee OA [n = 21], TKA [n = 2], PFP [n = 15], ACLD [n = 3], ACLR [n = 13]), and 16 in the transverse plane (knee OA [n = 7], PFP [n = 4], ACLD [n = 1], ACLR [n = 4]). One study investigated trunk acceleration using triaxial accelerometers in individuals with ACLR [102], 1 study investigated trunk kinematics in the frontal plane using 3D accelerometers [64], and 1 study investigated trunk kinematics in the sagittal plane using a bi-axial accelerometer and a gyroscope in individuals with TKA [72]. One study investigated two-dimensional trunk sagittal plane displacement in individuals with PFP [82], and 2 studies investigated two-dimensional trunk sagittal and frontal planes displacement in individuals with ACLD [97, 99].
Participant Characteristics
Studies included 894 individuals with knee OA [43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68, 121], 160 individuals with TKA [69,70,71,72,73,74,75, 121], 28 individuals with PT [95, 96], 442 individuals with PFP [76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94], 203 individuals with ACLD [97,98,99,100,101, 120, 122], 702 individuals with ACLR [34, 102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120, 122], and 1875 controls. The detailed characteristics of participants included in each study, their measurement methods, and outcomes are presented in Additional file 1C.
Methodological Quality
Agreement between raters for the Downs and Black checklist was 88% with scores ranging from 4 to 12. Of the 81 studies, 22 were high quality, 56 were moderate quality, and 3 were low quality (Additional file 1D).
Data Findings
From the 81 included studies, 45 were included in meta-analyses. Thirty-six studies were not included due to heterogeneity in tasks or outcomes or missing data. A qualitative synthesis of the unpooled studies along with the reporting quality was performed. For the knee disorders where meta-analysis was possible (i.e., knee OA, TKA, PFP, and ACLR), the qualitative synthesis is presented in Additional file 1E. For those where meta-analysis was not possible (i.e., PT and ACLD), the qualitative synthesis is presented below. The SMD and 95% CI of the unpooled studies are presented in Additional file 1F.
Knee OA versus Controls
Trunk Kinematics in the Sagittal Plane
Moderate-certainty evidence from 4 studies (233 participants) [60, 65, 66, 121] showed no differences between groups for trunk flexion during walking (SMD = 0.40, 95% CI = − 0.05 to 0.84; Z = 1.76, P = 0.08 [Fig. 2A]). High-certainty evidence with large effect from 4 studies (402 participants) [54, 56, 59, 67] showed greater trunk flexion in individuals with knee OA compared to controls during sit-to-stand (SMD = 0.088, 95% CI = 0.58–1.18; Z = 5.80, P = 0.001 [Fig. 2B]). Moderate-certainty evidence with moderate effect from 2 studies (95 participants) [43, 57] showed greater trunk flexion in individuals with knee OA compared to controls during stair ascent and descent (SMD = 0.56, 95% CI = 0.13–.99; Z = 2.55, P = 0.001 [Fig. 2C]).
Meta-analyses of trunk kinematics in individuals with knee OA compared to controls. Trunk kinematics in the sagittal plane during walking (A), sit-to-stand (B), and stepping tasks (C). Trunk kinematics in the frontal plane during walking (D) and sit-to-stand (E). Trunk kinematics in the transverse plane during walking (F). (1) varus OA group, (2) valgus OA group, (3) mild OA group, (4) moderate OA group, (5) C-TST OA group, (6) IC-STS OA, (7) SI-STS OA group, (8) less severe OA group, (9) more severe OA group, (10) group with unilateral pain and radiographic knee OA, (11) group with unilateral pain and bilateral radiographic knee OA, (12) group with bilateral pain and radiographic knee OA, (13) mild OA group, (14) moderate OA group, (15) severe OA group, (16) group with unilateral OA pain, (17) group with bilateral OA pain. HQ high quality, MQ moderate quality, OA osteoarthritis, KL Kellgren–Lawrence grade. † Groups divided considering different magnitudes of compensation strategies while performing the task
Trunk Kinematics in the Frontal Plane
Moderate-certainty evidence with large effect from 8 studies (643 participants) [45,46,47, 50, 58, 60, 65, 66] showed greater ipsilateral trunk lean during walking (SMD = 1.36; 95% CI = 0.60–2.11; Z = 3.53, P = 0.004 [Fig. 2D]). The high heterogeneity (I2 = 94%) was mainly influenced by the results of Creaby et al. [46], which was confirmed following visual inspection. A sensitivity analysis was then performed with the removal of Creaby et al. [46]. Results changed to moderate-certainty evidence with moderate effect of greater ipsilateral trunk lean in individuals with knee OA compared to controls, and the heterogeneity was reduced (SMD = 0.51; 95% CI = 0.20–0.82; Z = 3.25, P = 0.001 [I2 = 59%]) (Additional file 1G). High-certainty evidence with large effect from 2 studies (227 participants) [56, 59] showed greater contralateral trunk lean in individuals with knee OA compared to controls during sit-to-stand (SMD = 1.49; 95% CI = 0.90–2.08; Z = 4.99, P = 0.001 [Fig. 2E]).
Trunk Kinematics in the Transverse Plane
Moderate-certainty evidence from 3 studies (208 participants) [60, 65, 66] showed no differences between groups for ipsilateral trunk rotation during walking (SMD = 0.00; 95% CI = − 0.28 to 0.28; Z = 0.01, P = 1.00 [Fig. 2F]).
TKA versus Controls
Trunk Kinematics in the Sagittal Plane
Moderate-certainty evidence from 3 studies (95 participants) [73, 74, 121] showed no differences between groups for trunk flexion during walking (SMD = 0.09; 95% CI = − 0.31 to 0.50; Z = 0.45, P = 0.66 [Fig. 3A]), whereas moderate-certainty evidence from 3 studies (116 participants) [69, 73, 74] also showed no differences between groups during stair ascent and descent (SMD = − 0.15; 95% CI = − 0.55 to 0.25; Z = 0.75, P = 0.46 [Fig. 3B]).
Meta-analyses of trunk kinematics in individuals with TKA compared to controls. Trunk kinematics in the sagittal plane during walking (A) and stepping tasks (B). Trunk kinematics in the frontal plane during walking (C) and stepping tasks (D). Trunk kinematics in the transverse plane during walking (E) and stepping tasks (F). TKA Total knee arthroplasty, MQ moderate quality
Trunk Kinematics in the Frontal Plane
Moderate-certainty evidence from 2 studies (70 participants) [73, 74] showed no differences between groups for ipsilateral trunk lean during walking (SMD = − 0.10; 95% CI = − 0.57 to 0.37; Z = 0.40, P = 0.69 [Fig. 3C]) and stair ascent and descent (SMD = − 0.20; 95% CI = − 0.67 to 0.27; Z = 0.82, P = 0.41 [Fig. 3D]). Moderate-certainty evidence from 2 studies (70 participants) [73, 74] showed no differences between groups for contralateral trunk lean during walking (SMD = 0.06; 95% CI = − 0.41 to 0.53; Z = 0.26, P = 0.80 [Fig. 3C]) and stair ascent and descent (SMD = − 0.07; 95% CI = − 0.54 to 0.40; Z = 0.30, P = 0.76 [Fig. 3D]).
Trunk Kinematics in the Transverse Plane
Moderate-certainty evidence with moderate effect from 2 studies (70 participants) [73, 74] showed greater ipsilateral trunk rotation (SMD = 0.52; 95% CI = 0.04 to 0.99; Z = 2.11, P = 0.03 [Fig. 3E]) in individuals with TKA compared to controls during walking, whereas moderate-certainty evidence from 2 studies (70 participants) [73, 74] showed no differences between groups for ipsilateral trunk rotation during stair ascent and descent (SMD = 0.00; 95% CI = − 0.47 to 0.47; Z = 0.02, P = 0.99 [Fig. 3F]).
PFP versus Controls
Trunk Kinematics in the Sagittal Plane
Moderate-certainty evidence from 3 (126 participants) [77, 79, 90] and 2 studies (143 participants) [88, 89] showed no differences between groups for trunk flexion during running (SMD = 0.32; 95% CI = − 0.15 to 0.79; Z = 1.33, P = 0.18 [Fig. 4A]) and stair ascent and descent (SMD = 0.01; 95% CI = − 0.32 to 0.34; Z = 0.05, P = 0.96 [Fig. 4B]), respectively. Moderate-certainty evidence with moderate effect from 2 studies (70 participants) [80, 91] showed greater trunk flexion during landing tasks (SMD = 0.56; 95% CI = 0.01–1.12; Z = 1.98, P = 0.05 [Fig. 4C]).
Meta-analyses of trunk kinematics and strength in individuals with PFP compared to controls. Trunk kinematics in the sagittal plane during running (A), stepping (B), and landing tasks (C). Trunk kinematics in the frontal plane during running (D), squatting (E), stepping (F), and landing tasks (G). Trunk kinematics in the transverse plane during landing tasks (H). (1) PFP and control groups with knee crepitus, PFP and control groups without knee crepitus, (3) PFP group with elevated fear avoidance beliefs, (4) PFP group with low fear avoidance beliefs. PFP patellofemoral pain, HQ high quality, MQ moderate quality, SLH single-leg hop for distance, SLS single-leg squat, FSD forward step-down. ‡Data supplied by author
Trunk Kinematics in the Frontal Plane
Moderate-certainty evidence from 4 studies (158 participants) [77, 79, 85, 90] showed no differences between groups for ipsilateral trunk lean during running (SMD = 0.20; 95% CI = − 0.12 to 0.52; Z = 1.20, P = 0.23 [Fig. 4D]). Moderate-certainty evidence with large effect from 3 studies (174 participants) [81, 84, 92] showed greater ipsilateral trunk lean in individuals with PFP compared to controls during single-leg squat (SMD = 1.01; 95%CI = 0.33–1.70; Z = 2.91, P = 0.004 [Fig. 4E]). Moderate-certainty evidence from 2 studies (120 participants) [83, 88] showed no differences between groups for ipsilateral trunk lean during stepping tasks (SMD = 0.39; 95% CI = − 0.13 to 0.91; Z = 1.46, P = 0.014 [Fig. 4F]). Moderate-certainty evidence from 2 studies (108 participants) [86, 88] showed no differences between groups for contralateral trunk lean during stair descent (SMD = 0.09; 95% CI = − 0.29 to 0.47; Z = 0.46, P = 0.64 [Fig. 4F]). Very low-certainty evidence from 2 studies (70 participants) [80, 91] showed no differences between groups for ipsilateral trunk lean during landing tasks (SMD = 1.12; 95% CI = − 1.22 to 3.47; Z = 0.94, P = 0.35 [Fig. 4G]).
Trunk Kinematics in the Transverse Plane
Very low-certainty evidence from 2 studies (70 participants) [80, 91] showed no differences between group for ipsilateral trunk rotation during landing tasks (SMD = − 0.63; 95% CI = − 1.86 to 0.61; Z = 0.99, P = 0.32 [Fig. 4H]).
PT versus Controls
Trunk Kinematics in the Sagittal Plane
One moderate-quality study [96] reported no differences between groups for trunk flexion during three different variations of squatting tasks. One high-quality study [95] reported no differences between groups for trunk flexion during a drop vertical landing.
ACLD versus Controls
Trunk Kinematics in the Sagittal Plane
One moderate-quality study [100] reported no differences between groups for trunk flexion during walking. One moderate-quality study [100] reported greater trunk flexion in individuals with ACLD during stair ascent and descent. One moderate-quality study [122] reported greater trunk flexion in individuals with ACLD during landing from a single-leg hop for distance, while no differences between groups were reported during jumping and landing from a single-leg vertical hop [122]. Two moderate quality studies [97, 99] reported lower two-dimensional trunk flexion displacement in individuals with ACLD during landing and cutting tasks [97] and single-leg landing [99].
Trunk Kinematics in the Frontal Plane
One moderate-quality study [100] reported lower contralateral trunk lean in individuals with ACLD during walking, while another moderate-quality study [120] reported no differences between groups during walking and running. One moderate-quality study [101] reported greater ipsilateral trunk lean in individuals with ACLD during single-leg squat, while another moderate-quality study [120] reported no differences between groups. One moderate-quality study [100] reported greater contralateral trunk lean in individuals with ACLD during stair ascent and descent. One moderate-quality study [120] reported lower contralateral trunk lean in individuals with ACLD during landing of single-leg hop for distance. One moderate-quality study [97] reported greater two-dimensional lateral trunk displacement (side not specified) in individuals with ACLD during landing and cutting tasks.
Trunk Kinematics in the Transverse Plane
One moderate-quality study [100] reported greater ipsilateral trunk rotation during walking and lower contralateral trunk rotation during stair ascent and descent.
ACLR versus Controls
Trunk Kinematics in the Sagittal Plane
Moderate-certainty evidence with moderate effect from 3 studies (229 participants) [34, 106, 114] showed greater trunk flexion at IC in individuals with ACLR compared to controls during landing tasks (SMD = 0.69; 95% CI = 0.38–1.01; Z = 4.34, P = 0.001 [Fig. 5A]). Moderate-certainty evidence with small effect from 13 studies (933 participants) [34, 104, 106, 108,109,110, 112,113,114, 117,118,119, 122] showed greater peak/RoM trunk flexion in individuals with ACLR compared to controls during landing tasks (SMD = 0.48; 95% CI = 0.21–0.75; Z = 3.48, P = 0.005 [Fig. 5A]). Very low-certainty evidence from 4 studies (312 participants) [109, 110, 118, 122] showed no differences between groups for trunk flexion during jumping tasks (SMD = − 0.76; 95% CI = − 1.62 to 0.10; Z = 1.74, P = 0.08 [Fig. 5B]).
Meta-analyses of trunk kinematics in individuals with ACLR compared to controls. Trunk kinematics in the sagittal plane during landing (A) and jumping (B) tasks. Trunk kinematics in the frontal plane during landing tasks (C). (1) ACLR group with high fear of reinjury, (2) ACLR group with low fear of reinjury. ACLR anterior cruciate ligament reconstruction, HQ high quality, LQ low quality, MQ moderate quality, BDJ bilateral drop jump, DVJ drop vertical jump, SLDJ single-leg drop jump, SLH single-leg hop for distance, SLVJ single-leg vertical jump, VCJ single-leg vertical countermovement jump
Trunk Kinematics in the Frontal Plane
Low-certainty evidence from 2 studies (180 participants) [34, 106] showed no differences between groups for ipsilateral trunk lean at IC during landing tasks (SMD = − 0.01; 95% CI = − 0.48 to 0.46; Z = .05, P = .96 [Fig. 5C]). Moderate-certainty evidence from 6 studies (568 participants) [34, 104, 106, 113, 116, 119] showed no differences between groups for ipsilateral trunk lean (peak/RoM) during landing tasks (SMD = 0.23; 95% CI = − 0.05 to 0.51; Z = 1.58, P = 0.11 [Fig. 5C]).
Evidence Gap Map
Evidence gap maps for discrete variables of trunk kinematics and kinetics as well as waveform analyses of trunk biomechanics are presented in Additional files 1H and 1I, respectively. Overall, PT is the knee disorder with the least amount of studies (2 [95, 96]), which have only investigated trunk kinematics in the sagittal plane. Similarly, trunk kinematics in individuals with ACLD was investigated in only 7 studies [97,98,99,100,101, 120, 122], which were heterogeneous for tasks and outcomes and could not be pooled. Inconclusive evidence is outlined for trunk kinematics in the transverse plane, with studies not clearly specifying which side the trunk is rotating toward. There was also insufficient evidence for trunk kinetics, with investigations limited to ACLR. Furthermore, waveform analyses of trunk kinematics or kinetics have not been performed in individuals with ACLD, PT, or TKA.
Discussion
This review identified 81 studies investigating trunk biomechanics across 6 different knee disorders (i.e., knee OA, PFP, PT, ACLD, TKA and ACLR). In individuals with knee OA, greater trunk flexion and contralateral trunk lean during sit-to-stand, greater trunk flexion during stepping tasks, and greater ipsilateral trunk lean during walking were identified. On the other hand, no alterations were identified in trunk sagittal or frontal planes in individuals with TKA. Individuals with PFP demonstrated greater trunk flexion during landing tasks and greater ipsilateral trunk lean during single-leg squat. Individuals with ACLR also demonstrated greater trunk flexion during landing tasks. These findings show that changes in trunk biomechanics in the sagittal and frontal planes are present in the most common knee disorders. This systematic review also highlights areas with the need for more research, with noticeable lack of investigations in individuals with PT or ACLD.
Trunk Biomechanics for Participants with Knee OA
Individuals with knee OA demonstrated greater trunk flexion during sit-to-stand [54, 56, 59] and stair negotiation [43, 57]. Sit-to-stand and stair negotiation require high knee extensor moments and generate great knee loading [59, 123,124,125]. Since the increase in trunk flexion can reduce knee loading [126], these findings possibly represent a compensatory strategy to reduce knee loading and avoid or control knee pain [53, 68]. However, the persistent use of this strategy may lead to chronic disuse of knee extensors and subsequent muscle weakness [127]. Decreased knee extensor strength is associated with increased risk of worsening of knee pain and lower physical function [128].
Individuals with knee OA presented greater ipsilateral trunk lean during walking [45,46,47, 50, 58, 60, 65]. This is likely a mechanism to reduce high knee varus moments and medial knee loading, which are associated with the progression of knee OA severity [129] and pain [130]. Although increasing ipsilateral trunk lean reduces knee varus moments in a dose–response manner [17], with greater angulations being associated with worse radiographic knee OA [50], its effect on pain is inconclusive [17] and subsequent hip abductor weakness may be an unintended consequence [10].
Individuals with knee OA demonstrated greater contralateral trunk lean during sit-to-stand (moderate-certainty evidence with large effect) [56, 59]. While this strategy is likely employed to reduce knee loads on the affected knee [56, 59], it may overload the unaffected or less affected knee, leading also to unintended consequences [50, 131].
Trunk Biomechanics for Participants with TKA
No alterations were identified in trunk sagittal and frontal planes during walking and stepping tasks in individuals with TKA [73, 74, 121]. It has been suggested that the absence of differences between individuals with TKA and controls may be due to positive effects of surgical and conservative managements on knee pain, limiting the need for trunk compensations [73, 74, 121]. In fact, a recent systematic review [132] has identified that excessive trunk amplitudes during walking, as seen pre-operatively, decreased after TKA. However, care should be taken when interpreting our findings due to the limited number of studies included in this review. In addition, more studies are warranted investigating sit-to-stand as it is the task that most consistently elicits trunk compensations [132] and it was not investigated in individuals with TKA.
Trunk Biomechanics for Participants with PFP
Individuals with PFP presented greater trunk flexion during landing tasks [80, 91], whereas no differences were found during running and stepping tasks [77, 79, 88,89,90]. Landing tasks impose higher patellofemoral joint loading compared to walking, stepping, and squatting tasks [133] and may reflect the upper limits of lower‐limb joint loading experienced [134]. Since PFP commonly affects young physically active individuals [2], it may be that only a higher knee loading task such as landing would elicit a compensatory trunk flexion. In tasks with lower knee loading, other compensatory strategies may be used such as the modification of step length in running [135] and cadence in stair negotiation [136].
Individuals with PFP presented greater ipsilateral trunk lean during single-leg squat [81, 84, 92]. Greater ipsilateral trunk lean during single-leg squat has been reported as a strategy to compensate for hip abductor weakness in individuals with PFP [10]. Although ipsilateral trunk lean can reduce the demand on the hip abductors [10], such an adaptation might increase knee valgus moments [10, 97, 137], and patellofemoral joint loading [137]. Future studies are required to understand long-term consequences of compensatory ipsilateral trunk lean in individuals with PFP.
Trunk Biomechanics for Participants with ACLD
The qualitative synthesis suggests that individuals with ACLD may alter trunk motion during stepping and landing tasks, although there is no consistency over the direction of these changes. Two studies reported a more extended trunk posture in individuals with ACLD compared to controls during landing tasks [97, 99], while 2 other studies reported greater trunk flexion during landing and stepping tasks [98, 100]. A more extended trunk posture represents a stiffened movement that may be indicative of fear of reinjury [31]. Conversely, increased trunk flexion is indicative of quadriceps weakness and/or avoidance [138]. These findings indicate that there seems to be more than just one compensatory trunk strategy and individuals with ACLD may respond differently given their fear of reinjury or reliance on quadriceps function. However, further studies are warranted due to the low number of studies included in this review.
There is also conflicting evidence for trunk kinematics in the frontal plane. Greater ipsilateral trunk lean was reported in individuals with ACLD during single-leg landing and squat [97, 101], while greater contralateral trunk lean was reported during stair negotiation [100], suggesting that changes in trunk kinematics in the frontal plane may be task dependent. Alternate stepping may allow greater trunk displacement in the frontal plane and a contralateral trunk lean [139, 140], while only an ipsilateral trunk lean may be possible during single-leg landing and squat. Further research is needed as we were unable to pool data due to the low number of studies.
Trunk Biomechanics for Participants with ACLR
Moderate-certainty evidence demonstrated greater trunk flexion in individuals with ACLR during landing tasks [104, 106, 108,109,110, 112,113,114, 122], likely to reduce quadriceps demand and knee pain. A subgroup of athletes at the time of return-to-sport after ACLR with low-quadriceps symmetry between limbs (i.e., < 85% of isometric strength) presented greater trunk flexion during landing compared to controls [141]. In the same study, quadriceps strength symmetry was found to be a unique and significant predictor of landing symmetry in peak trunk flexion [141]. A recent study [138] has also reported that reductions in peak trunk flexion are correlated to improved pain scores and increased knee extensor moments between baseline and follow-up (2 and 8 years post-ACLR). Therefore, the identification of such a strategy may indicate the need to enhance quadriceps strength and function, especially at the time of return-to-sport [141]. Greater quadriceps neuromuscular function would provide better knee energy attenuation and reduce the level of pain [138] and risk of secondary injury [142, 143].
Clinical Implications
The findings of this systematic review support the assessment of trunk biomechanics in individuals with OA, PFP, or ACLR to identify possible targets for rehabilitation, especially for those with chronic pain. Reliable, valid, and time- and cost-effective field-based assessments of biomechanics can be performed through two-dimensional motion capture [144,145,146,147,148,149] and wearable inertial measurement units (IMU) [150, 151]. To target altered trunk kinematics in the sagittal and frontal planes, clinicians can consider interventions like progressive resistance training [152], virtual reality training [153], and motor feedback control using IMUs, visual or verbal feedback [154,155,156]. The assessment of trunk biomechanics may also provide an objective marker of quadriceps avoidance strategies [138], hip muscle weakness [10, 138], and disease prognosis [50, 138].
The compensatory strategies identified in this systematic review may be useful as a temporary strategy when pain is exacerbated (acute phases) to alleviate symptoms. They could be part of self-management programs [157, 158], although their effectiveness needs further testing. Also, long-term use of these strategies may lead to chronic disuse of the knee extensors or hip abductors.
Limitations and Future Directions
Although the findings of this systematic review highlight that individuals with knee OA, PFP, and ACLR seem to present with altered trunk biomechanics, the cross-sectional nature of the included studies precludes us from establishing cause and effect, as well as long-term consequences. Prospective cohort studies or randomized controlled trials are needed to determine the causal relationship and long-term consequences of altered trunk biomechanics in individuals with knee OA, PFP, and ACLR.
Some meta-analyses of this systematic review included a small number of studies, which may limit a more precise estimation of the effect. Some meta-analyses that included few studies had low values of heterogeneity. Caution is needed when interpreting these values as they may considerably change upon the inclusion of new studies. Further studies may improve the precision of the estimated effect and provide a more accurate interpretation of heterogeneity.
The findings of this systematic review outline the lack of studies in individuals with PT and ACLD, as well as insufficient evidence for trunk kinematics in the transverse plane and trunk kinetics across knee disorders. Further research is warranted to fill these gaps and strengthen future recommendations.
Conclusion
Individuals with knee OA, PFP, or ACLR present with altered trunk kinematics in the sagittal and frontal planes. No trunk biomechanical alterations were identified in individuals with TKA, whereas a noticeable lack of investigation in individuals with PT or ACLD precludes any conclusion. Our findings support the assessment of trunk biomechanics in individuals with OA, PFP, or ACLR to identify possible targets for rehabilitation and avoidance strategies.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and in Additional file 1: Appendices A, B, C, D, E, F, G, H, and I.
References
Montalvo AM, Schneider DK, Webster KE, Yut L, Galloway MT, Heidt RS, et al. Anterior cruciate ligament injury risk in sport: a systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train. 2019;54:472–82.
Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, et al. Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis. PLoS ONE. 2018;13:e0190892.
Lian ØB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33:561–7.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393:1745–59.
Lankhorst NE, van Middelkoop M, Crossley KM, Bierma-Zeinstra SMA, Oei EHG, Vicenzino B, et al. Factors that predict a poor outcome 5–8 years after the diagnosis of patellofemoral pain: a multicentre observational analysis. Br J Sports Med. 2015;50:881–6.
Wiggins AJ, Grandhi M, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1861–76.
Kettunen JA, Kvist M, Alanen E, Kujala UM. Long-term prognosis for jumper’s knee in male athletes: a prospective follow-up study. Am J Sports Med. 2002;30:689–92.
De Rooij M, Van Der Leeden M, Heymans MW, Holla JFM, Häkkinen A, Lems WF, et al. Prognosis of pain and physical functioning in patients with knee osteoarthritis: a systematic review and meta-analysis. Arthritis Care Res. 2016;68:481–92.
Sasaki S, Nagano Y, Kaneko S, Imamura S, Koabayshi T, Fukubayashi T. The relationships between the center of mass position and the trunk, hip, and knee kinematics in the sagittal plane: a pilot study on field-based video analysis for female soccer players. J Hum Kinet. 2015;45:71–80.
Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40:42–51.
Balotari Botta AF, Waiteman MC, Perez VO, Gomes Garcia CL, Bazett-Jones DM, de Azevedo FM, et al. Trunk muscle endurance in individuals with and without patellofemoral pain: Sex differences and correlations with performance tests. Phys Ther Sport. 2021;52:248–55.
Borghuis J, Hof AL, Lemmink APM. The importance of sensory-motor control in providing core stability. Sport Med. 2008;38:893–916.
Blackburn JT, Padua DA. Sagittal-plane trunk position, landing forces, and quadriceps electromyographic activity. J Athl Train. 2009;44:174–9.
Rathleff MS, Rathleff CR, Crossley KM, Barton CJ. Is hip strength a risk factor for patellofemoral pain? A systematic review and meta-analysis. Br J Sports Med. 2014;48:1088.
Scattone Silva R, Nakagawa TH, Ferreira ALG, Garcia LC, Santos JEM, Serrão FV. Lower limb strength and flexibility in athletes with and without patellar tendinopathy. Phys Ther Sport. 2016;20:19–25.
Hinman RS, Hunt MA, Creaby MW, Wrigley TV, McManus FJ, Bennell KL. Hip muscle weakness in individuals with medial knee osteoarthritis. Arthritis Care Res. 2010;62:1190–3.
Simic M, Hunt MA, Bennell KL, Hinman RS, Wrigley TV. Trunk lean gait modification and knee joint load in people with medial knee osteoarthritis: the effect of varying trunk lean angles. Arthritis Care Res. 2012;64:1545–53.
Hewett TE, Myer GD, Ford KR, Heidt RS, Colosimo AJ, McLean SG, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492–501.
Myer GD, Ford KR, Di Stasi SL, Foss KDB, Micheli LJ, Hewett TE. High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: is PFP itself a predictor for subsequent ACL injury? Br J Sports Med. 2015;49:118–22.
Graci V, Salsich GB. Trunk and lower extremity segment kinematics and their relationship to pain following movement instruction during a single-leg squat in females with dynamic knee valgus and patellofemoral pain. J Sci Med Sport. 2015;18:343–7.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Ardern CL, Büttner F, Andrade R, Weir A, Ashe MC, Holden S, et al. Implementing the 27 PRISMA 2020 Statement items for systematic reviews in the sport and exercise medicine, musculoskeletal rehabilitation and sports science fields: the PERSiST (implementing Prisma in Exercise, Rehabilitation, Sport medicine and SporTs sc. Br J Sports Med. 2021;56:175–95.
Duncan RC, Hay EM, Saklatvala J, Croft PR. Prevalence of radiographic osteoarthritis: it all depends on your point of view. Rheumatology. 2006;45:757–60.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Commun Health. 1998;52:377–84.
Mousavi SH, Hijmans JM, Rajabi R, Diercks R, Zwerver J, van der Worp H. Kinematic risk factors for lower limb tendinopathy in distance runners: a systematic review and meta-analysis. Gait Posture. 2019;69:13–24.
De Bleecker C, Vermeulen S, De Blaiser C, Willems T, De Ridder R, Roosen P. Relationship between jump-landing kinematics and lower extremity overuse injuries in physically active populations: a systematic review and meta-analysis. Sport Med. 2020;50:1515–32.
Iijima H, Shimoura K, Ono T, Aoyama T, Takahashi M. Proximal gait adaptations in individuals with knee osteoarthritis: a systematic review and meta-analysis. J Biomech. 2019;87:127–41.
Neal BS, Barton CJ, Gallie R, O’Halloran P, Morrissey D. Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: a systematic review and meta-analysis. Gait Posture. 2016;45:69–82.
Barton CJ, Levinger P, Menz HB, Webster KE. Kinematic gait characteristics associated with patellofemoral pain syndrome: a systematic review. Gait Posture. 2009;30:405–16.
Coburn SL, Barton CJ, Filbay SR, Hart HF, Rathleff MS, Crossley KM. Quality of life in individuals with patellofemoral pain: a systematic review including meta-analysis. Phys Ther Sport. 2018;33:96–108.
Trigsted SM, Cook DB, Pickett KA, Cadmus-Bertram L, Dunn WR, Bell DR. Greater fear of reinjury is related to stiffened jump-landing biomechanics and muscle activation in women after ACL reconstruction. Knee Surgery, Sport Traumatol Arthrosc. 2018;26:3682–9.
Brown SR, Brughelli M, Hume PA. Knee mechanics during planned and unplanned sidestepping: a systematic review and meta-analysis. Sport Med. 2014;44:1573–88.
Hajizadeh M, Oskouei AH, Ghalichi F, Sole G. Knee kinematics and joint moments during stair negotiation in participants with anterior cruciate ligament deficiency and reconstruction: a systematic review and meta-analysis. PM R. 2016;8:563–79.
Markström JL, Grinberg A, Hager CK. Fear of reinjury following anterior cruciate ligament reconstruction is manifested in muscle activation patterns of single-leg side-hop landings. Phys Ther. 2021;21:pzab218.
Cohen J. Statistical power analysis for the behavioral sciences. New York: Routledge; 1988.
Higgins JP, Thompson SG, Deeks JJ, Altman DJ. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane; 2021. www.training.cochrane.org/handbook
Oliveira CB, Maher CG, Franco MR, Kamper SJ, Williams CM, Silva FG, et al. Co-occurrence of chronic musculoskeletal pain and cardiovascular diseases: a systematic review with meta-analysis. Pain Med. 2020;21:1106–21.
Miller JR, Van Hooren B, Bishop C, Buckley JD, Willy RW, Fuller JT. A systematic review and meta-analysis of crossover studies comparing physiological, perceptual and performance measures between treadmill and overground running. Sport Med. 2019;49:763–82.
Van Hooren B, Fuller JT, Buckley JD, Miller JR, Sewell K, Rao G, et al. Is motorized treadmill running biomechanically comparable to overground running? A systematic review and meta-analysis of cross-over studies. Sport Med. 2020;50:785–813.
Tayfur A, Haque A, Salles JI, Malliaras P, Screen H, Morrissey D. Are landing patterns in jumping athletes associated with patellar tendinopathy? A systematic review with evidence gap map and meta-analysis. Sport Med. 2022;52:123–37.
van Tulder MV, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976). 2003;28:1290–9.
Asay JL, Mündermann A, Andriacchi TP. Adaptive patterns of movement during stair climbing in patients with knee osteoarthritis. J Orthop Res. 2009;27:325–9.
Azma K, Mahdavi E, Hosseini A, Naseh I, Gholestanpour A. The effect of lateral trunk motion on the severity of knee osteoarthritis. Biomed Pharmacol J. 2015;8:139–45.
Bechard DJ, Birmingham TB, Zecevic AA, Jones IC, Giffin RJ, Jenkyn TR. Toe-out, lateral trunk lean, and pelvic obliquity during prolonged walking in patients with medial compartment knee osteoarthritis and healthy controls. Arthritis Care Res (Hoboken). 2012;64:525–32.
Creaby MW, Bennell KL, Hunt MA. Gait differs between unilateral and bilateral knee osteoarthritis. Arch Phys Med Rehabil. 2012;93:822–7.
Whatling GM, Biggs PR, Elson DW, Metcalfe A, Wilson C, Holt C. High tibial osteotomy results in improved frontal plane knee moments, gait patterns and patient-reported outcomes. Knee Surg Sport Traumatol Arthrosc. 2020;28:2872–82.
Hálfdanardóttir F, Ramsey DK, Briem K. Timing of frontal plane trunk lean, not magnitude, mediates frontal plane knee joint loading in patients with moderate medial knee osteoarthritis. Adv Orthop. 2018;2018(20):4526872.
Kean CO, Bennell KL, Wrigley TV, Hinman RS. Modified walking shoes for knee osteoarthritis: mechanisms for reductions in the knee adduction moment. J Biomech. 2013;46:2060–6.
Hunt MA, Wrigley TV, Hinman RS, Bennell KL. Individuals with severe knee osteoarthritis (OA) exhibit altered proximal walking mechanics compared with individuals with less severe OA and those without knee pain. Arthritis Care Res. 2010;62:1426–32.
Linley HS, Sled EA, Culham EG, Deluzio KJ. A biomechanical analysis of trunk and pelvis motion during gait in subjects with knee osteoarthritis compared to control subjects. Clin Biomech. 2010;25:1003–10.
Magalhães CMB, Resende RA, Kirkwood RN. Increased hip internal abduction moment and reduced speed are the gait strategies used by women with knee osteoarthritis. J Electromyogr Kinesiol. 2013;23:1243–9.
Meireles S, Reeves ND, Jones RK, Smith CR, Thelen DG, Jonkers I. Patients with medial knee osteoarthritis reduce medial knee contact forces by altering trunk kinematics, progression speed, and stepping strategy during stair ascent and descent: a pilot study. J Appl Biomech. 2019;35:280–9.
Petrella M, da Silva-Serrão PRM, Selistre LFA, Lessi GC, Gonçalves GH, Mattiello SM. Individual joint contributions to the total support moment during the sit-to-stand task differentiate mild and moderate knee osteoarthritis. Clin Biomech. 2019;70:52–8.
Preece SJ, Algarni AS, Jones RK. Trunk flexion during walking in people with knee osteoarthritis. Gait Posture. 2019;72:202–5.
Sagawa Y, Bonnefoy-Mazure A, Armand S, Lubbeke A, Hoffmeyer P, Suva D, et al. Variable compensation during the sit-to-stand task among individuals with severe knee osteoarthritis. Ann Phys Rehabil Med. 2017;60:312–8.
Sparkes V, Whatling GM, Biggs P, Khatib N, Al-Amri M, Williams D, et al. Comparison of gait, functional activities, and patient-reported outcome measures in patients with knee osteoarthritis and healthy adults using 3D motion analysis and activity monitoring: an exploratory case-control analysis. Orthop Res Rev. 2019;11:129–40.
Tanaka K, Miyashita K, Urabe Y, Ijiri T, Takemoto Y, Ishii Y, et al. Characteristics of trunk lean motion during walking in patients with symptomatic knee osteoarthritis. Knee. 2008;15:134–8.
Turcot K, Armand S, Fritschy D, Hoffmeyer P, Suvà D. Sit-to-stand alterations in advanced knee osteoarthritis. Gait Posture. 2012;36:68–72.
Turcot K, Armand S, Lübbeke A, Fritschy D, Hoffmeyer P, Suvà D. Does knee alignment influence gait in patients with severe knee osteoarthritis? Clin Biomech. 2013;28:34–9.
Turcot K, Sagawa Y, Hoffmeyer P, Suvà D, Armand S. Multi-joint postural behavior in patients with knee osteoarthritis. Knee. 2015;22:517–21.
Van Der Straaten R, Wesseling M, Jonkers I, Vanwanseele B, Bruijnes AKBD, Malcorps J, et al. Functional movement assessment by means of inertial sensor technology to discriminate between movement behaviour of healthy controls and persons with knee osteoarthritis. J Neuroeng Rehabil. 2020;17:65.
van der Straaten R, Wesseling M, Jonkers I, Vanwanseele B, Bruijnes AKBD, Malcorps J, et al. Discriminant validity of 3D joint kinematics and centre of mass displacement measured by inertial sensor technology during the unipodal stance task. PLoS ONE. 2020;15:e0232513.
Staab W, Hottowitz R, Sohns C, Sohns JM, Gilbert F, Menke J, et al. Accelerometer and gyroscope based gait analysis using spectral analysis of patients with osteoarthritis of the knee. J Phys Ther Sci. 2014;26:997–1002.
Hart HF, Collins NJ, Ackland DC, Cowan SM, Crossley KM. Gait characteristics of people with lateral knee osteoarthritis after ACL reconstruction. Med Sci Sports Exerc. 2015;47:2406–15.
Boekesteijn RJ, Smolders JMH, Busch VJJF, Geurts ACH, Smulders K. Independent and sensitive gait parameters for objective evaluation in knee and hip osteoarthritis using wearable sensors. BMC Musculoskelet Disord. 2021;22:242.
Fu S, Duan T, Hou M, Yang F, Chai Y, Chen Y, et al. Postural balance in individuals with knee osteoarthritis during stand-to-sit task. Front Hum Neurosci. 2021;15:760960.
Preece SJ, Alghamdi W. Increased trunk flexion may underlie elevated knee flexor activity in people with knee osteoarthritis. Knee. 2021;33:216–25.
Bjerke J, Öhberg F, Nilsson KG, Stensdotter AK. Compensatory strategies for muscle weakness during stair ascent in subjects with total knee arthroplasty. J Arthroplasty. 2014;29:1499–502.
Pozzi F, Marmon AR, Snyder-Mackler L, Zeni J. Lower leg compensatory strategies during performance of a step up and over task in patient six-months after total knee arthroplasty. Gait Posture. 2016;49:41–6.
Saari T, Tranberg R, Zügner R, Uvehammer J, Kärrholm J. The effect of tibial insert design on rising from a chair; motion analysis after total knee replacement. Clin Biomech. 2004;19:951–6.
Boonstra MC, De Waal Malefijt MC, Verdonschot N. How to quantify knee function after total knee arthroplasty? Knee. 2008;15:390–5.
Fenner V, Behrend H, Kuster MS. Whole body gait function during stair ascending and level walking in patients following total knee arthroplasty. Int J Phys Med Rehabil. 2014;2:1–9.
Fenner VU, Behrend H, Kuster MS. Joint mechanics after total knee arthroplasty while descending stairs. J Arthroplasty. 2017;32:575–80.
Li K, Ackland DC, McClelland JA, Webster KE, Feller JA, de Steiger R, et al. Trunk muscle action compensates for reduced quadriceps force during walking after during walking after total knee arthroplasty. Gait Posture. 2013;38:79–85.
Alvim FC, de Souza Muniz AM, Lucareli PRG, Menegaldo LL. Kinematics and muscle forces in women with patellofemoral pain during the propulsion phase of the single leg triple hop test. Gait Posture. 2019;73:108–15.
Bazett-Jones DM, Cobb SC, Huddleston WE, O’Connor KM, Armstrong BSR, Earl-Boehm JE. Effect of patellofemoral pain on strength and mechanics after an exhaustive run. Med Sci Sports Exerc. 2013;45:1331–9.
Bley AS, Correa JCF, Dos RAC, Rabelo NDDA, Marchetti PH, Lucareli PRG. Propulsion phase of the single leg triple hop test in women with patellofemoral pain syndrome: a biomechanical study. PLoS ONE. 2014;9:e97606.
Bramah C, Preece SJ, Gill N, Herrington L. Is there a pathological gait associated with common soft tissue running injuries? Am J Sports Med. 2018;46:3023–31.
dos Reis AC, Correa JCF, Bley AS, dos Anjos-Rabelo ND, Fukuda TY, Lucareli PRG. Kinematic and kinetic analysis of the single-leg triple hop test in women with and without patellofemoral pain. J Orthop Sport Phys Ther. 2015;45:799–807.
Glaviano NR, Baellow A, Saliba S. Elevated fear avoidance affects lower extremity strength and squatting kinematics in women with patellofemoral pain. Athl Train Sport Heal Care. 2019;11:192–200.
Hebert LJ, Gravel D, Arsenault AB, Tremblay G. Patellofemoral pain syndrome: the possible role of an inadequate neuromuscular mechanism. Clin Biomech. 1994;9:93–7.
Nakagawa TH, Moriya ÉTU, MacIel CD, Serrão FV. Frontal plane biomechanics in males and females with and without patellofemoral pain. Med Sci Sports Exerc. 2012;44:1747–55.
Nakagawa TH, Moriya ÉTU, Maciel CD, Serrão FV. Trunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndrome. J Orthop Sport Phys Ther. 2012;42:491–501.
Noehren B, Pohl MB, Sanchez Z, Cunningham T, Lattermann C. Proximal and distal kinematics in female runners with patellofemoral pain. Clin Biomech. 2012;27:366–71.
de Almeida Novello A, Garbelotti S, dos Anjos Rabelo ND, Ferraz AN, Bley AS, Correa JCF, et al. Descending stairs: good or bad task to discriminate women with patellofemoral pain? Gait Posture. 2018;65:26–32.
Nunes GS, Wolf DF, dos Santos DA, de Noronha M, Serrão FV. Acute effects of hip mobilization with movement technique on pain and biomechanics in females with patellofemoral pain: a randomized, placebo-controlled trial. J Sport Rehabil. 2020;29:707–15.
Schwane BG, Goerger BM, Goto S, Blackburn T, Aguilar AJ, Padua DA. Trunk and lower extremity kinematics during stair descent in women with or without patellofemoral pain. J Athl Train. 2015;50:704–12.
Waiteman MC, de Oliveira SD, Azevedo FM, Pazzinatto MF, Briani RV, Bazett-Jones DM. Women with patellofemoral pain and knee crepitus have reduced knee flexion angle during stair ascent. Phys Ther Sport. 2021;48:60–6.
Haghighat F, Ebrahimi S, Rezaie M, Shafiee E, Shokouhyan SM, Motealleh A, et al. Trunk, pelvis, and knee kinematics during running in females with and without patellofemoral pain. Gait Posture. 2021;89:80–5.
Baellow A, Glaviano NR, Hertel J, Saliba SA. Lower extremity biomechanics during a drop vertical jump and muscle strength in women with patellofemoral pain. J Athl Train. 2020;55:615–22.
Nakagawa TH, Maciel CD, Serrão FV. Trunk biomechanics and its association with hip and knee kinematics in patients with and without patellofemoral pain. Man Ther. 2015;20:189–93.
Claudon B, Poussel M, Billon-Grumillier C, Beyaert C, Paysant J. Knee kinetic pattern during gait and anterior knee pain before and after rehabilitation in patients with patellofemoral pain syndrome. Gait Posture. 2012;36:139–43.
Ho K-Y, Barrett T, Clark Z, DuVall C, Fox T, Howden C, et al. Comparisons of trunk and knee mechanics during various speeds of treadmill running between runners with and without patellofemoral pain: a preliminary study. J Phys Ther Sci. 2021;33:737–41.
Scattone Silva R, Purdam CR, Fearon AM, Spratford WA, Kenneally-Dabrowski C, Preston P, et al. Effects of altering trunk position during landings on patellar tendon force and pain. Med Sci Sports Exerc. 2017;49:2517–27.
Barker-Davies RM, Roberts A, Watson J, Baker P, Bennett AN, Fong DTP, et al. Kinematic and kinetic differences between military patients with patellar tendinopathy and asymptomatic controls during single leg squats. Clin Biomech. 2019;62:127–35.
Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43:417–22.
Oberländer KD, Brüggemann GP, Höher J, Karamanidis K. Reduced knee joint moment in ACL deficient patients at a cost of dynamic stability during landing. J Biomech. 2012;45:1387–92.
Sipprell W, Boden BP, Sheehan FT. Dynamic sagittal-plane trunk control during anterior cruciate ligament injury. Am J Sports Med. 2012;40:1068–74.
Shi D, Li N, Wang Y, Jiang S, Lin J, Zhu W. Gait modification strategies in trunk over right stance phase in patients with right anterior cruciate ligament deficiency. Gait Posture. 2016;46:63–8.
Fukuda W, Kawamura K, Yokoyama S, Kataoka Y, Ikeno Y, Chikaishi N, et al. A cross-sectional study to assess variability in knee frontal plane movement during single leg squat in patients with anterior cruciate ligament injury. J Bodyw Mov Ther. 2021;28:144–9.
Armitano CN, Morrison S, Russell DM. Upper body accelerations during walking are altered in adults with ACL reconstruction. Gait Posture. 2017;58:401–8.
Bell DR, Kulow SM, Stiffler MR, Smith MD. Squatting mechanics in people with and without anterior cruciate ligament reconstruction: the influence of graft type. Am J Sports Med. 2014;42:2979–87.
Lessi GC, Serrao FV. Effects of fatigue on lower limb, pelvis and trunk kinematics and lower limb muscle activity during single-leg landing after anterior cruciate ligament reconstruction. Knee Surg Sport Traumatol Arthrosc. 2017;25:2550–8.
Slater LV, Blemker SS, Hertel J, Saliba SA, Weltman AL, Hart JM. Sex affects gait adaptations after exercise in individuals with anterior cruciate ligament reconstruction. Clin Biomech. 2020;71:189–95.
Markström JL, Grip H, Schelin L, Häger CK. Individuals with an anterior cruciate ligament–reconstructed knee display atypical whole body movement strategies but normal knee robustness during side-hop landings: a finite helical axis analysis. Am J Sports Med. 2020;48:1117–26.
Noehren B, Abraham A, Curry M, Johnson D, Ireland ML. Evaluation of proximal joint kinematics and muscle strength following ACL reconstruction surgery in female athletes. J Orthop Res. 2014;23:1305–10.
Scarneo-Miller SE, Sorge JE, Beltz EM, Martinez JC, Root HJ, Burland JP, et al. The relationship between single-limb squat and jump-cut kinematics. Sport Biomech. 2019;11:1–12.
Setuain I, Gonzalez M, Alfaro J, Gorostiaga E, Izquierdo M. Acceleration and orientation jumping performance differences among elite professional male handball players with or without previous ACL reconstruction: an inertial sensor unit-based study. PM R. 2015;7:1243–53.
Setuain I, Millor N, Gonzále-Izal M, Gorostiaga E, Gómez M, Alfaro-Adrián J, et al. Biomechanical jumping differences among elite female handball players with and without previous anterior cruciate ligament reconstruction: a novel inertial sensor unit study. Sport Biomech. 2015;14:323–39.
Smeets A, Vanrenterghem J, Staes F, Vandenneucker H, Claes S, Verschueren S. Are anterior cruciate ligament-reconstructed athletes more vulnerable to fatigue than uninjured athletes? Med Sci Sports Exerc. 2020;52:345–53.
Sritharan P, Perraton LG, Munoz MA, Pivonka P, Bryant AL. Muscular coordination of single-leg hop landing in uninjured and anterior cruciate ligament-reconstructed individuals. J Appl Biomech. 2020;36:235–43.
Trigsted SM, Post EG, Bell DR. Landing mechanics during single hop for distance in females following anterior cruciate ligament reconstruction compared to healthy controls. Knee Surg Sport Traumatol Arthrosc. 2017;25:1395–402.
Kotsifaki A, Whiteley R, Van Rossom S, Korakakis V, Bahr R, Sideris V, et al. Single leg hop for distance symmetry masks lower limb biomechanics: time to discuss hop distance as decision criterion for return to sport after ACL reconstruction? Br J Sports Med. 2021;56:249–56.
Boggess G, Morgan K, Johnson D, Ireland ML, Reinbolt JA, Noehren B. Neuromuscular compensatory strategies at the trunk and lower limb are not resolved following an ACL reconstruction. Gait Posture. 2018;60:81–7.
Fryer C, Ithurburn MP, McNally MP, Thomas S, Paterno MV, Schmitt LC. The relationship between frontal plane trunk control during landing and lower extremity muscle strength in young athletes after anterior cruciate ligament reconstruction. Clin Biomech. 2019;62:58–65.
Kotsifaki A, Van Rossom S, Whiteley R, Korakakis V, Bahr R, Sideris V, et al. Symmetry in triple hop distance hides asymmetries in knee function after ACL reconstruction in athletes at return to sports. Am J Sports Med. 2021;50:441–50.
Kotsifaki A, Van Rossom S, Whiteley R, Korakakis V, Bahr R, Sideris V, et al. Single leg vertical jump performance identifies knee function deficits at return to sport after ACL reconstruction in male athletes. Br J Sports Med. 2022;56:490–8.
Fukuda W, Kawamura K, Yokoyama S, Kataoka Y, Ikeno Y, Chikaishi N, et al. Joint movement variability during landing in patients with anterior cruciate ligament reconstruction. J Sports Med Phys Fitness. 2021;61:1629–35.
Davies JL, Button K, Sparkes V, van Deursen RW. Frontal plane movement of the pelvis and thorax during dynamic activities in individuals with and without anterior cruciate ligament injury. Knee. 2018;25:997–1008.
Kuwahara W, Nakanishi K, Kurumadani H, Shimada N, Asaeda M, Deie M, et al. Total knee arthroplasty for patients with medial knee osteoarthritis improves trunk movement during gait. J Back Musculoskelet Rehabil. 2020;33:727–34.
Markström JL, Tengman E, Häger CK. ACL-reconstructed and ACL-deficient individuals show differentiated trunk, hip, and knee kinematics during vertical hops more than 20 years post-injury. Knee Surg Sport Traumatol Arthrosc. 2018;26:358–67.
Su F, Lai K, Hong W. Rising from chair after total knee arthroplasty. Clin Biomech. 1998;13:176–81.
Liikavainio T, Isolehto J, Helminen HJ, Perttunen J, Lepola V, Kiviranta I, et al. Loading and gait symmetry during level and stair walking in asymptomatic subjects with knee osteoarthritis: importance of quadriceps femoris in reducing impact force during heel strike? Knee. 2007;14:231–8.
Kutzner I, Heinlein B, Graichen F, Bender A, Rohlmann A, Halder A, et al. Loading of the knee joint during activities of daily living measured in vivo in five subjects. J Biomech. 2010;43:2164–73.
Straub RK, Barrack AJ, Cannon J, Powers CM. Trunk inclination during squatting is a better predictor of the knee-extensor moment than shank inclination. J Sport Rehabil. 2021;30:899–904.
Dehail P, Bestaven E, Muller F, Mallet A, Robert B, Bourdel-Marchasson I, et al. Kinematic and electromyographic analysis of rising from a chair during a “Sit-to-Walk” task in elderly subjects: role of strength. Clin Biomech. 2007;22:1096–103.
Glass NA, Torner JC, Frey Law LA, Wang K, Yang T, Nevitt MC, et al. The relationship between quadriceps muscle weakness and worsening of knee pain in the MOST cohort: a 5-year longitudinal study. Osteoarthr Cartil. 2013;21:1154–9.
Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–22.
Hall M, Bennell KL, Wrigley TV, Metcalf BR, Campbell PK, Kasza J, et al. The knee adduction moment and knee osteoarthritis symptoms: relationships according to radiographic disease severity. Osteoarthr Cartil. 2017;25:34–41.
Eddo OO, Lindsey BW, Caswell SV, Prebble M, Cortes N. Unintended changes in contralateral limb as a result of acute gait modification. J Appl Biomech. 2019;4:1–7.
Van Criekinge T, de Grave PW, Luyckx T, Claeys K. Trunk control, motion and alignment after total knee arthroplasty: a systematic review and meta-analysis. Gait Posture. 2022;94:173–88.
Van Rossom S, Smith CR, Thelen DG, Vanwanseele B, Van Assche D, Jonkers I. Knee joint loading in healthy adults during functional exercises: implications for rehabilitation guidelines. J Orthop Sports Phys Ther. 2018;48:162–73.
Sritharan P, Schache AG, Culvenor AG, Perraton LG, Bryant AL, Morris HG, et al. Patellofemoral and tibiofemoral joint loading during a single-leg forward hop following ACL reconstruction. J Orthop Res. 2022;40:159–69.
Willson JD, Sharpee R, Meardon SA, Kernozek TW. Effects of step length on patellofemoral joint stress in female runners with and without patellofemoral pain. Clin Biomech. 2014;29:243–7.
Brechter JH, Powers CM. Patellofemoral joint stress during stair ascent and descent in persons with and without patellofemoral pain. Gait Posture. 2002;16:115–23.
Waiteman MC, Briani RV, Ferraz Pazzinatto M, Ferreira AS, Ferrari D, De Oliveira SD, et al. Relationship between knee abduction moment with patellofemoral joint reaction force, stress and self-reported pain during stair descent in women with patellofemoral pain. Clin Biomech. 2018;59:110–6.
Fischer AG, Erhart-Hledik JC, Chu CR, Asay JL, Andriacchi TP. Changes in stair ascent biomechanics two to eight years after ACL reconstruction are associated with patient-reported outcomes. Gait Posture. 2019;69:91–5.
Reid SM, Lynn SK, Musselman RP, Costigan PA. Knee biomechanics of alternate stair ambulation patterns. Med Sci Sports Exerc. 2007;39:2005–11.
King SL, Underdown T, Reeves ND, Baltzopoulos V, Maganaris CN. Alternate stair descent strategies for reducing joint moment demands in older individuals. J Biomech. 2018;78:126–33.
Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am J Sports Med. 2015;43:2727–37.
Ward SH, Blackburn JT, Padua DA, Stanley LE, Harkey MS, Luc-Harkey BA, et al. Quadriceps neuromuscular function and jump-landing sagittal-plane knee biomechanics after anterior cruciate ligament reconstruction. J Athl Train. 2018;53:135–43.
Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968–78.
Lopes TJA, Ferrari D, Ioannidis J, Simic M, De Azevedo FM, Pappas E. Reliability and validity of frontal plane kinematics of the trunk and lower extremity measured with 2-dimensional cameras during athletic tasks: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2018;48:812–22.
Kingston B, Murray A, Norte GE, Glaviano NR. Validity and reliability of 2-dimensional trunk, hip, and knee frontal plane kinematics during single-leg squat, drop jump, and single-leg hop in females with patellofemoral pain. Phys Ther Sport. 2020;45:181–7.
Straub RK, Powers CM. Utility of 2D video analysis for asessing frontal plane trunk and pelvis motion during stepping, landing, and change in direction tasks: a validity study. Int J Sports Phys Ther. 2022;17:139–47.
Schurr SA, Marshall AN, Resch JE, Saliba SA. Two-dimensional video analysis is comparable to 3D motion capture in lower extremity movement assessment. Int J Sports Phys Ther. 2017;12:163–72.
Willson JD, Davis IS. Utility of the frontal plane projection angle in females with patellofemoral pain. J Orthop Sport Phys Ther. 2008;38:606–15.
Doozan M, Bazett-Jones DM, Glaviano NR. Novice versus expert intertester reliability of two-dimensional squatting kinematics in females with and without patellofemoral pain. Int J Athl Ther Train. 2021;26:154–60.
Dahl KD, Dunford KM, Wilson SA, Turnbull TL, Tashman S. Wearable sensor validation of sports-related movements for the lower extremity and trunk. Med Eng Phys. 2020;84:144–50.
Chia L, Andersen JT, McKay MJ, Sullivan J, Megalaa T, Pappas E. Evaluating the validity and reliability of inertial measurement units for determining knee and trunk kinematics during athletic landing and cutting movements. J Electromyogr Kinesiol. 2021;60:102589.
Granacher U, Gollhofer A, Hortobágyi T, Kressig RW, Muehlbauer T. The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: a systematic review. Sport Med. 2013;43:627–41.
Juras G, Brachman A, Michalska J, Kamieniarz A, Pawłowski M, Hadamus A, et al. Standards of virtual reality application in balance training programs in clinical practice: a systematic review. Games Health J. 2019;8:101–11.
dos Santos AF, Nakagawa TH, Lessi GC, Luz BC, Matsuo HTM, Nakashima GY, et al. Effects of three gait retraining techniques in runners with patellofemoral pain. Phys Ther Sport. 2019;36:92–100.
Teng H-L, Dilauro A, Weeks C, Odell C, Kincaid H, VanDine B, et al. Short-term effects of a trunk modification program on patellofemoral joint stress in asymptomatic runners. Phys Ther Sport. 2020;44:107–13.
Shull PB, Jirattigalachote W, Hunt MA, Cutkosky MR, Delp SL. Quantified self and human movement: a review on the clinical impact of wearable sensing and feedback for gait analysis and intervention. Gait Posture. 2014;40:11–9.
Smith BE, Hendrick P, Bateman M, Moffatt F, Rathleff MS, Selfe J, et al. A loaded self-managed exercise programme for patellofemoral pain: a mixed methods feasibility study. BMC Musculoskelet Disord. 2019;20:129.
Brand E, Nyland J, Henzman C, Mcginnis M. Arthritis self-efficacy scale scores in knee osteoarthritis: a systematic review and meta-analysis comparing arthritis self-management education with or without exercise. J Orthop Sports Phys Ther. 2013;43:895–910.
Acknowledgements
Authors thank São Paulo Research Foundation (FAPESP) for a scholarship (number: 2020/12257-0). The financial sponsors played no role in the design, execution, analysis and interpretation of data, or writing of the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MCW, LC, MHMD, DBJ, EP, FA, and RVB contributed to the conception and design of the review and completion of the search strategy. MCW wrote the first draft of the manuscript and performed the data analysis and the evidence gap map. MCW and MHMD conducted the screening, data extraction, and methodological quality assessment. MCW and RVB conducted the level of certainty and evidence assessments. MCW, LC, MHMD, DBJ, EP, FA, and RVB edited, revised, and approved the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Marina Waiteman, Lionel Chia, Matheus Ducatti, David Bazett‑Jones, Evangelos Pappas, Fábio de Azevedo and Ronaldo Briani declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary material including: search strategy (A), reasons for exclusion of studies excluded after full-text screening (B), summary of included studies (C), methodological quality assessment of included studies (D), qualitative and quantitative syntheses of unpooled data (E and F), sensitivity analysis (G), and evidence gap maps (H and I).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Waiteman, M.C., Chia, L., Ducatti, M.H.M. et al. Trunk Biomechanics in Individuals with Knee Disorders: A Systematic Review with Evidence Gap Map and Meta-analysis. Sports Med - Open 8, 145 (2022). https://doi.org/10.1186/s40798-022-00536-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40798-022-00536-6