Abstract
Background
Lipomatous tumors are the most common type of soft-tissue tumors. Benign lipomatous tumors are lipomas and lipoblastoma. We herein report a case of benign mesenteric lipomatous tumor and the largest collection of known benign mesenteric lipomatous tumors in children in the literature.
Case presentation
A 3-year-old girl presented with repeated dull abdominal pain and left abdominal mass swelling. On a physical examination, the child had a soft, moderately distended left abdomen that was not tender when palpated. Computed tomography and magnetic resonance imaging demonstrated a large fatty mass within the mesentery, measuring approximately 8 × 6 cm. The mass extended from the right upper quadrant to the lower pole of the kidneys. Laparotomy with resection of the mesenteric tumor was performed under general anesthesia. A well-capsuled tumor was a soft, yellow mass and found loosely attached to the mesenterium of the ileum. A histopathological examination demonstrated the lobular proliferation of mature adipocytes. Atypical lipoblasts were not seen. These features are compatible with benign lipomatous tumor, such as lipoma or lipoblastoma with maturation.
Conclusion
In conclusion, benign mesenteric lipomatous tumors tend to be large in size over 10 cm in longitudinal length. However, resection is well tolerated in the vast majority of cases with benign post-operative courses.
Similar content being viewed by others
Introduction
Lipomatous tumors are the most common type of soft-tissue tumors. Benign lipomatous tumors are “lipomas” and “lipoblastoma”. Lipoma is a rare benign lesion of mature adipose tissue. It is a well-defined, noninvasive, and encapsulated mass that can be discovered in asymptomatic patients or may cause variable nonspecific symptoms, depending on its size and location [1, 2]. Lipoblastoma is a rare benign soft-tissue tumor that occurs most commonly in infants and children [3, 4]. The vast majority are detected in children under 3 years old, with over 80% of cases occurring before 3 years old and 40% before 1 year old [3,4,5,6,7]. These tumors occur commonly in the extremities, trunk, head, and neck. However, benign mesenteric lipomatous tumors are rare. The long-term prognosis for lipoblastoma is usually excellent [5]. Metastases have never been reported, but the recurrence rates have been reported to range from 9 to 22%, which is attributed to incomplete initial excision of the tumor [6, 7]. Mesenteric lipomatous tumors are slow-growing, mobile, soft masses that do not infiltrate the surrounding organs. Gastrointestinal tract lipomas mostly present as an insidious-growing, soft, mobile mass without penetration into the surroundings.
We herein report a case of benign mesenteric lipomatous tumor and the largest collection of known benign mesenteric lipomatous tumors in children in the literature.
Case report
A 3-year-old girl presented with repeated dull abdominal pain and left abdominal mass swelling. There were no evident congenital abnormalities at birth nor any familial history of disease. On a physical examination, the child had a soft, moderately distended left abdomen that was not tender when palpated. The hemoglobin, alphafetoprotein, and beta-hCG levels were normal.
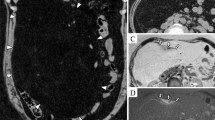
Abdominal ultrasound showed a heterogeneous soft-tissue mass measuring φ8 cm. Computed tomography demonstrated a large fatty mass within the mesentery, measuring approximately 8 × 6 cm. The mass extended from the right upper quadrant to the lower pole of the kidneys (Fig. 1). Magnetic resonance imaging (MRI) revealed a well-encapsulated soft-tissue mass lesion in the mesenteric region. The mass had a clearly defined margin and a reticular pattern with an interposing fat component showing a reduced signal on fat suppression inversion recovery imaging (Fig. 2a, b). Based on these findings, the mass was suspected of being a benign soft-tissue tumor, most likely lipoma or lipoblastoma.
Magnetic resonance imaging coronal section image obtained a well-encapsulated soft-tissue mass lesion with high intensity in the mesenteric region, a T1-weighted image obtained the mass lesion with high intensity signal. b Fat suppression inversion recovery imaging obtained an interposing fat component showing a reduced signal
Laparotomy with resection of the mesenteric tumor was performed under general anesthesia. A well-capsuled tumor was a soft, yellow mass and found loosely attached to the mesenterium of the ileum. The tumor was located 6 cm from the ileocecal valve. The tumor was not separated from small intestine. Tumor was resected with small intestine which was 5 cm and end-to-end anastomosis of the small intestine was performed without injury to adjacent structures (Fig. 3). The tumor was well circumscribed with a thin, fibrous capsule and a yellow, lobulated fatty parenchyma separated by thin fibrous septa with punctate vessels.
A histopathological examination demonstrated the lobular proliferation of mature adipocytes. Atypical lipoblasts were not seen (Fig. 4a). Immunohistochemically, there were adipocytic cells positive for p16 and cyclin-dependent kinase 4 (CDK4) but negative for murine double minutes (MDM2) (Fig. 4b–d). The feature is compatible with benign lipomatous tumor, such as lipoma or lipoblastoma with maturation.
Follow-up at 2 years revealed no evidence of recurrence.
Discussion
Mesenteric lipomatous tumors are slow-growing, mobile, soft masses that do not infiltrate the surrounding organs. Ultrasound can detect abdominal lipomatous tumors as homogenous echogenic masses; however, they may present a confusing picture, from a homogenous to a heterogeneous echo pattern [1]. According to the computed tomography findings, other fat attenuation processes associated with the mesentery are considered as differential diagnoses, including liposarcoma, lymphangiomas, and cavitating mesenteric lymph node syndrome [8]. MRI has the highest sensitivity for the pathology of the tumor among imaging modalities, as the increased vascularity in lipoblastomas compared to lipomas showed a low intensity on T1-weighted images [6]. MRI is, therefore, the current recommended modality for follow-up, particularly in cases of incomplete resection or prior recurrence. Resection and a pathological examination are ultimately needed to make a definitive diagnosis.
According to the pathological findings, the maturation pattern of lipoblastoma tends to be characterized by a high proportion of mature adipocytes at the center of the lobule with lipoblasts on the periphery. Some reports suggest that lipoblastoma may spontaneously mature or regress [4]. Coffin et al. reported the maturation of an incompletely excised lipoblastoma into a mature lipoma [5]. Similar to the present case, although atypical lipoblasts were not detected, it was difficult to distinguish between lipoblastoma with maturation and lipoma give the patient’s age.
The recent use of cytogenetics has proven useful for making the diagnosis, as translations involving the long arm of chromosome 8, particularly 8q11-13, with or without pleomorphic adenoma gene 1 (PLAG1) oncogene rearrangements, have been found to be associated with lipoblastomas [7,8,9]. This rearrangement targets the PLAG1 gene and has been reported in 82% of lipoblastomas but only 3% of conventional lipomas and never in myxoid liposarcoma [9]. In the present case, we could not examine if there was PLAG1 oncogene rearrangements or not. As atypical lipoblasts were not seen, there was, therefore, no need to distinguish lipoma from lipoblastoma with maturation.
The immunohistochemical trio of CDK4, MDM2, and p16 is a useful ancillary diagnostic tool that provides strong support for distinguishing differentiated liposarcoma from other adipocytic neoplasms [10]. A previous study found that MDM2 is highly sensitive for atypical lipomatous tumor, and without taking this marker into account, there has been a tendency to misclassify atypical lipomatous tumors as lipomas in the past [11].
A literature search was performed using the electronic database “PubMed” for all patient reports in the English literature with benign mesenteric lipomatous tumors using the search term “mesenteric lipoma”, “mesenteric lipoblastoma”, and “benign mesenteric lipomatous tumor”. Relevant data were extracted from all primary reported patients. Patients included in multiple reports were used only once for the analysis. All patients under 15 years old were combined to create this report. The clinical features of the current case were consistent with those previously reported, including her age, gender, onset, size and location of tumor, preoperative diagnosis, pathological diagnosis, operation, and complications.
All patient data from 1956 to 2020 were combined to create this report [4, 12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45]. There have been 44 cases of mesenteric lipoma and lipoblastoma in children, as shown in Table 1. These patients were 18 males and 18 females excluded cases which were not reported about gender. Twenty cases were lipoma, and 24 cases were lipoblastoma. The age at the presentation ranged from 5 months to 11 years old. Especially in the cases with lipoblastoma, the age at the presentation in 17 cases (70.9%) was under 3 years old. The tumors ranged in longitudinal length from 8 to 31 cm. Almost all tumors were over 10 cm in longitudinal length excluded not reported cases. Lipomas were located on the mesentery of the small intestine (50.0%) or omentum (10.0%). On the other hand, lipoblastomas were located on the mesentery of the small intestine (33.3%), omentum (12.5%), jejunum (4.16%), colon (8.3%), and in the peritoneal cavity (4.16%). The other reports did not describe the retroperitoneal side in detail. About the onset of cases with lipoma, 13 cases (65.0%) had abdominal pain. On the other hand, 8 cases (33.3%) with lipoblastoma had abdominal pain. Because over 50% of the cases with lipoblastoma were under 3 years old, they could not complain of abdominal pain. In 26 cases, the operative procedures were reported. In 15 cases, tumor resection without anastomosis was performed, while 11 cases received tumor resection with end-to end anastomosis. There were no cases of incomplete resection excluding 8 cases where the details were not reported. In 9 cases, the tumors weighed over 1 kg. Six cases presented with volvulus and bowel obstruction. There were no cases of recurrence and post-operative complications.
Conclusion
In conclusion, benign mesenteric lipomatous tumors tend to be large in size over 10 cm in longitudinal length. However, resection is well tolerated in the vast majority of cases with benign post-operative courses.
Availability of data and materials
All data generated during this study are included in this published article.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- CDK4:
-
Cyclin-dependent kinase 4
- MDM2:
-
Murine double minutes
- PLAG1:
-
Pleomorphic adenoma gene 1
References
Cha JM, Lee JI, Joo KR, Choe JW, Jung SW, Shin HP, et al. Giant mesenteric lipoma as an unusual cause of abdominal pain: a case report and a review of the literature. J Korean Med Sci. 2009;24:333–6.
Chaudhary V, Narula MK, Anand R, Gupta I, Kaur G, Kalra K. Giant omental lipoma in a child. Iran J Radiol. 2011;8:167–9.
McVay MR, Keller JE, Wagner CW, Jackson RJ, Smith SD. Surgical management of lipoblastoma. J Pediatr Surg. 2006;41:1067–71.
Cudnik R, Efron PA, Chen MK, Reith JD, Beierle EA. Mesenteric lipoblastoma: a rare location in children. J Pediatr Surg. 2008;43:e5-7.
Coffin CM. Lipoblastoma: an embryonal tumor of soft tissue related to organogenesis. Semin Diagn Pathol. 1994;11:98–103.
Dilley AV, Patel DL, Hicks MJ, et al. Lipoblastoma: pathophysiology and surgical management. J Pediatr Surg. 2001;36:229–31.
Kok KY, Telisinghe PU. Lipoblastoma: clinical features, treatment, and outcome. World J Surg. 2010;34:1517–22.
Hicks J, Dilley A, Patel D, Barrish J, Zhu SH, Brandt M. Lipoblastoma and lipoblastomatosis in infancy and childhood: histopathologic, ultrastructural, and cytogenetic features. Ultrastruct Pathol. 2001;25:321–33.
Bartuma H, Domanski HA, Von Steyern FV, Kullendorff CM, Mandahl N, Mertens F. Cytogenetic and molecular cytogenetic findings in lipoblastoma. Cancer Genet Cytogenet. 2008;183:60–3.
Thway K, Flora R, Shah C, Olmos D, Fisher C. Diagnostic utility of p16, CDK4, and MDM2 as an immunohistochemical panel in distinguishing well-differentiated and dedifferentiated liposarcomas from other adipocytic tumors. Am J Surg Pathol. 2012;36:462–9.
Brisson M, Kashima T, Delaney D, Tirabosco R, Clarke A, Cro S, et al. MRI characteristics of lipoma and atypical lipomatous tumor/well-differentiated liposarcoma: retrospective comparison with histology and MDM2 gene amplification. Skelet Radiol. 2013;42:635–47.
Prince TC, Shaffner LD. Mesenteric lipoma in children. Ann Surg. 1956;144:913–4.
Ogilvy WL, Owen HF. Mesenteric lipoma in children. Can J Surg. 1960;3:344–6.
Stransky E, Sevilla-Cabrera R. On a huge intraabdominal mesocolic lipoma in infancy. Ann Paediatr. 1962;198:24–34.
Friedman AC, Hartman DS, Sherman J, Lautin EM, Goldman M. Computed tomography of abdominal fatty masses. Radiology. 1981;139:415–29.
Fisher MF, Fletcher BD, Dahms BB, Haller JO, Friedman AP. Abdominal lipoblastomatosis: radiographic, echographic, and computed tomographic findings. Radiology. 1981;138:593–6.
Stringel G, Shandling B, Mancer K, Ein SH. Lipoblastoma in infants and children. J Pediatr Surg. 1982;17:277–80.
Jimenez JF. Lipoblastoma in infancy and childhood. J Surg Oncol. 1986;32(4):238–44.
Denath FM. Intraperitoneal lipoblastoma. Semin Roentgenol. 1988;23:241–2.
Gupta DK, Rohatgi M, Rao PS. Mesenteric lipoma. Indian Pediatr. 1988;25:1007–9.
Prando A, Wallace S, Marins JL, Pereira RM, de Oliveira ER, Alvarenga M. Sonographic features of benign intraperitoneal lipomatous tumors in children—report of 4 cases. Pediatr Radiol. 1990;20:571–4.
Schulman H, Barki Y, Hertzanu Y. Case report: mesenteric lipoblastoma. Clin Radiol. 1992;46:57–8.
Beebe MM, Smith MD. Omental lipoblastoma. J Pediatr Surg. 1993;28:1626–7.
Tröbs RB, Meier T, Nenning H, Mühlig K, Biesold M, Brock D. Benign mesenteric lipoblastoma. Pediatr Surg Int. 1996;11:425–6.
Posey Y, Valdivia E, Persons DL, Ally S, Smith DL, Pantazis CG, et al. Lipoblastoma presenting as a mesenteric mass in an infant. J Pediatr Hematol Oncol. 1998;20:580–2.
Kaniklides C, Frykberg T, Lundkvist K. Paediatric mesenteric lipoma, an unusual cause of repeated abdominal pain. A case report. Acta Radiol. 1998;39:695–7.
Ilhan H, Tokar B, Işiksoy S, Koku N, Pasaoglu O. Giant mesenteric lipoma. J Pediatr Surg. 1999;34:639–40.
Mo YH, Peng SS, Li YW, Shun CT. Mesenteric lipoblastoma: case report. Pediatr Radiol. 2003;33:37–40.
Al-Salem AH, Al-Nazer M. Mesenteric lipoblastoma in a 2-year-old child. Pediatr Surg Int. 2003;19:115–7.
Wolko JD, Rosenfeld DL, Lazar MJ, Underberg-Davis SJ. Torsion of a giant mesenteric lipoma. Pediatr Radiol. 2003;33:34–6.
Ozel SK, Apak S, Ozercan IH, Kazez A. Giant mesenteric lipoma as a rare cause of ileus in a child: report of a case. Surg Today. 2004;34:470–2.
Cherian A, Singh SJ, Broderick N, Zaitoun AM, Kapila L. Small bowel volvulus due to giant mesenteric lipoma. Pediatr Surg Int. 2004;20:869–71.
Jung SM, Chang PY, Luo CC, Huang CS, Lai JY, Hsueh C. Lipoblastoma/lipoblastomatosis: a clinicopathologic study of 16 cases in Taiwan. Pediatr Surg Int. 2005;21:809–12.
Yu DC, Javid PJ, Chikwava KR, Kozakewich HP, Debiec-Rychter M, Lillehei CW, et al. Mesenteric lipoblastoma presenting as a segmental volvulus. J Pediatr Surg. 2009;44:e25–8.
Jia HM, Zhang KR. Mesenteric lipoblastoma in a 4-year-old. Pediatr Radiol. 2009;39:1126.
Tang XB, Zhang T, Bai YZ, Wang WL. Giant mesenteric lipoblastoma in a 4-year-old child. J Pediatr Surg. 2009;44:859–61.
Srinivasan KG, Gaikwad A, Ritesh K, Ushanandini KP. Giant omental and mesenteric lipoma in an infant. Afr J Paediatr Surg. 2009;6:68–9.
Gentimi F, Tzovaras AA, Antoniou D, Moschovi M, Papandreou E. A giant mesenteric lipoblastoma in an 18-month old infant: a case report and review of the literature. Afr J Paediatr Surg. 2011;8:320–3.
Turk E, Edirne Y, Karaca F, Memetoglu ME, Unal E, Ermumcu O. A rare cause of childhood ileus: giant mesenteric lipoma and a review of the literature. Eurasian J Med. 2013;45:222–5.
Capasso R, Rossi E, Castelli L, Basilicata A, Zeccolini R, Zeccolini M, et al. Mesenteric lipoblastoma and cervical lipoblastomatosis: ultrasound, elastosonography, and computed tomography findings in two children. Case Rep Radiol. 2014;2014:478252.
Laguna BA, Iyer RS, Rudzinski ER, Roybal JL, Stanescu AL. Torsion of a giant mesocolic lipoma in a child with Bannayan-Riley-Ruvalcaba syndrome. Pediatr Radiol. 2015;45:449–52.
Hamidi H, Rasouly N, Khpalwak H, Malikzai MO, Faizi AR, Hoshang MM, et al. Childhood giant omental and mesenteric lipoma. Radiol Case Rep. 2016;11:41–4.
Alireza R, Mohammad SS, Mehrzad M, Houman A. Midgut volvulus caused by mesenteric lipoma. Iran J Pediatr. 2013;23:121–3.
Yang C, Wang S, Zhang J, Kong XR, Zhao Z, Li CC. An unusual cause of paediatric abdominal pain: Mesenteric masses accompanied with volvulus. Turk J Gastroenterol. 2016;27:325–9.
Nagano Y, Uchida K, Inoue M, Ide S, Shimura T, Hashimoto K, et al. Mesenteric lipoblastoma presenting as a small intestinal volvulus in an infant: a case report and literature review. Asian J Surg. 2017;40:70–3.
Acknowledgements
The authors would like to thank Brian Quinn for his critical reading of the manuscript.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
NH and AT drafted the manuscript. NH and SS carried out the acquisition of data. MY participated in the critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Ethics Committee of Kurume University School of Medicine.
Consent for publication
Informed consent was obtained from the patient for the publication of this case report, including their medical data and images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hashizume, N., Aiko, T., Fukahori, S. et al. Benign mesenteric lipomatous tumor in a child: a case report and literature review. surg case rep 6, 243 (2020). https://doi.org/10.1186/s40792-020-01020-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-020-01020-7