Abstract
A 63-year-old man, who had undergone total gastrectomy and Roux-en-Y reconstruction for gastric cancer 10 years previously, was admitted to our hospital with complaints of abdominal pain, palpable abdominal tumor, and hematemesis. On admission, the abdominal tenderness was improving and no abdominal tumor was palpable. Mild inflammatory changes and anemia were noted on blood examination. Abdominal computed tomography revealed a tumor with a layered structure in the left abdomen. The patient was diagnosed with intestinal obstruction secondary to intussusception, and surgery was performed. Retrograde intussusception was found at the site of the Y anastomosis. We conducted manual reduction using the Hutchinson procedure. The intestinal color after the reduction was good, and no intestinal resection was required. Postoperative recovery was uneventful, and the patient was discharged 12 days after surgery. Reports of jejunal intussusception after total gastrectomy with Roux-en-Y reconstruction are relatively rare. Here, we report a case of jejunal intussusception after total gastrectomy with Roux-en-Y reconstruction.
Similar content being viewed by others
Background
Intussusception occurs when a portion of intestine invaginates into an adjacent section of intestine. Common physical exam findings in adults with intussusception include intermittent abdominal pain, vomiting, gastrointestinal bleeding, and/or the presence of a palpable mass. Possible sequelae of intussusception include small bowel obstruction and ischemia. Jejunal intussusception is a rare complication after gastrectomy and extremely rare after total gastrectomy. In this case study, we report a case of retrograde intussusception at Roux-en-Y anastomosis occurring 10 years after total gastrectomy. We also review other cases of intussusception after total gastrectomy that are reported in the literature.
Case presentation
A 63-year-old man, who had undergone total gastrectomy and Roux-en-Y reconstruction for early gastric cancer 10 years previously, was transferred to our institution from a local hospital with complaints of intermittent abdominal pain, palpable abdominal tumor, and hematemesis. On arrival, he was hemodynamically stable, the abdominal tenderness was improving, and the abdominal tumor was not felt on physical examination. Mild inflammatory reaction and anemia were noted on blood examination. All other laboratory values were unremarkable and there was no evidence of acidosis.
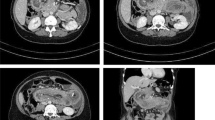
Abdominal computed tomography (CT) revealed a tumor with a layered structure in the left abdomen (Fig. 1). Endoscopy revealed a bulky, rounded, congested mass that occupied the lumen beyond the esophagojejunal anastomosis (Fig. 2) and showed a small amount of oozing from the mucosal surface caused by disruption to the blood flow resulting from intussusception. These findings led to the diagnosis of intestinal obstruction caused by jejunal intussusception. Although we observed retrograde jejunal intussusception, endoscopic reduction was not attempted and surgical repair was performed by laparotomy.
Surgery revealed retrograde jejunal intussusception in the elevated jejunum through the Y anastomosis (Fig. 3a). We reduced the intussusception using the Hutchinson procedure. The involved bowel was dilated, edematous, and congested, but there was no evidence of ischemia (Fig. 3b), and therefore, we performed only manual reduction and adhesiotomy without intestinal resection. The patient’s postoperative recovery was free of complications, and he was discharged 12 days postoperatively. He has been alive without symptoms of bowel obstruction for 2 years after operation.
a, b Intraoperatively, a retrograde intussusception at the Y-anastomosis was observed (a). Manual reduction was performed using the Hutchinson procedure (b). The color of intussuscepted intestine after the reduction was good, and intestinal resection was unnecessary (black arrow: jejunal pouch, white arrowhead: Y-anastomosis, surrounded by the dotted line and white arrow: intussuscepted intestine)
Discussion
Jejunal intussusception after gastrectomy was first reported by Bozzi [1] and is recognized as an uncommon complication, occurring in only 0.07–2.1% of patients who undergo gastrectomy [2]. Intussusception is attributed to both mechanical factors (excessive length of afferent loop, lifting afferent loop to the stomach wall, excessively large anastomosis hole, ptosis of the gastrojejunal anastomosis, postoperative adhesions, and stenosis causing reverse peristalsis) and functional factors (spasm of the intestine, peristaltic abnormality, surgical stimulation, inflammation, autonomic nervous system abnormality, enteral nutrition, drug infusion, and decrease in gastric wall tension) [2, 3]. At the site of the Roux-en-Y anastomosis in this case, adhesions were mild and no strictures or mass were observed that would cause reverse peristalsis. However, mechanical factors cannot be entirely ruled out in this patient; we suspect that some kind of peristaltic abnormality may have occurred. Tu and Kelly reported reverse peristalsis caused by an apparent ectopic pacemaker in a Roux-en-Y anastomosis of small intestinal resection [4]. This clinical condition may also cause retrograde intussusception after total gastrectomy and Roux-en-Y reconstruction.
Jejunal intussusception after total gastrectomy is rare. A review of the literature revealed 18 cases of intussusception occurring after total gastrectomy with Roux-en-Y reconstruction, including the current case (Table 1) [3, 5–18]. The majority of patients experiencing this complication were 60–70 years old. Only four cases of antegrade intussusception were observed; the other cases were retrograde intussusception. Furthermore, only six cases developed in the early postoperative period; other cases developed 1–22 years after surgery.
In 12 of the 18 reported cases, enterectomy was not performed. Kita et al. reported recurrence of intussusception within 1 year of manual reduction of intussusception. Recurrence may be more likely when only manual reduction is used, and therefore, resection and re-anastomosis should be considered [18]. We think that we may prevent retrograde intussusception by making Y leg side-to-side anastomosis in the case of gastrectomy. This is because it thinks that it may do intussusception by the peristalsis that was handed down to intestinal tract by making end-to-side anastomosis.
Conclusions
We report a case of retrograde intussusception at Roux-en-Y anastomosis 10 years after total gastrectomy.
Abbreviations
- CT:
-
Computed tomography
References
Bozzi E. So di una rara complicannza consecutive a gastroenterostomia alla V. Hacker Boll Acad Med Genova. 1914;122:3–4.
Narita H, Funabashi K, Yoshitomi H, Yamamori N, Iguchi T, Hori K, et al. Post operative intussusception—report of a case, and a comparison between adult and pediatric intussusceptions after laparotomy (in Japanese). Rinsyo Gaka (Clinical Surg). 1991;52:2125–31.
Davey WW. Retrograde intussusception following Roux-loop anastomosis in total gastrectomy. Br J Surg. 1954;42:102–3.
Tu BN, Kelly KA. Motility disorders after Roux-en-Y gastrojejunostomy. Obes Surg. 1994;4:219–26.
Kato M, Nakamura S, Hashimoto I. A case of intussusception of the jejunal afferent loop after a total gastrectomy (in Japanese). Geka Chiryo. 1965;12:495–7.
Freeman FJ, Bernatz PE, Brown Jr PW. Retrograde intussusception after total gastrectomy. Report of a case. Arch Surg. 1966;93:586–8.
Hanyu N, Suzuki H, Miho O, Nagao F. A case of jejunal intussusception after total gastrectomy (in Japanese). Nihon Syokakigeka Gakkai Zasshi (Jpn J Gastroentel Surg). 1984;17(4):791–3.
Hashimoto N, Fukano M, Sue K, Koyanagi N, Minagawa S. Adult retrograde intussusception after total gastrectomy (in Japanese). Geka. 1993;55(7):828–30.
Narushima Y, Kobayashi N, Kuroda F. A case of retrograde intussusception of jejunum after total gastrectomy (in Japanese). Nihon Fukubu Kyukyuigakukaishi. 1994;14(2):363–5.
Goto Y, Yodonawa S, Hirano M, Fujiwara A, Ogawa I. Retrograde jejunal intussusception after total gastrectomy (in Japanese with an English abstract). Nihon Rinsyo Gaka Gakkai Zasshi (J Jpn Surg Assoc). 2000;61(6):1474–7.
Ozdogan M, Hamaloglu E, Ozdemir A, Ozenc A. Antegrade jejunojejunal intussusception after Roux-en-Y esophagojejunostomy as an unusual cause of postoperative intestinal obstruction: report of a case. Surg Today. 2001;31:355–7.
Akiyama Y, Aoki K, Nakaya T, Fujiwara H. A case of retrograde jejunal intussusception of Roux-en-Y anastomotic site after total gastrectomy (in Japanese). Geka. 2005;67(5):587–9.
Matsumoto T, Kawamoto K, Sano K, Ogasahara K. Retrograde intussusception of the jejunal afferent loop developed 12 years after total gastrectomy (in Japanese). Kurashiki Cyuou Byoin Nenpo. 2005;67:107–10.
Sato S, Shinoda M, Kawaguchi S, Abe M, Kunori T, Shinya F. Case report of 21 year postgastrectomy retrograde intussusception of the jejunum occurring distal to a Roux-en-Y anastomosis (in Japanese). Nihon Fukubu Kyukyuigakukaishi. 2006;26(3):465–7.
Ueno T, Takahashi M, Kanno A, Naito H. A case of chronic intussusception leading to repeat aspiration pneumonia and second intussusception (in Japanese with an English abstract). Nihon Rinsyo Gaka Gakkai Zasshi (J Jpn Surg Assoc). 2010;71(11):2864–7.
Matsuda S, Kanai T, Nakamura A, Kuroshima N, Ueshima T, Fukushima H, et al. A case of intussusception of jejunum after total gastrectomy that occurred for an early postoperative period (in Japanese). Hamamatsu iryo senta gakujutsushi. 2012;6(1):20–3.
Lee SY, Lee JC, Yang DH. Early postoperative retrograde jejunojejunal intussusception after total gastrectomy with Roux-en-Y esophagojejunostomy: a case report. J Gastric Cancer. 2013;13(4):263–5.
Kita K, Yabuki H, Inaba S, Ohara K, Syounaka T, Watanabe K. A case report of a relapsed retrograde intussusception at a Roux-en-Y anastomosis after total gastrectomy requiring two surgery (in Japanese with an English abstract). Nihon Rinsyo Gaka Gakkai Zasshi (J Jpn Surg Assoc). 2013;74(2):391–5.
Acknowledgements
We thank the entire staff of JCHO Saga Central Hospital for treating and caring for this patient.
Funding
No funding was received for this study.
Authors’ contributions
YK, RM, TM, and KK performed the operation. YK wrote the manuscript. KK, KO, YA, and HT helped to write the manuscript and supervised the study. YK, RM, TM, SS, TS, HU, and KK provided daily medical treatment for the patient. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Informed consent was obtained from the patient for publication of this case report and any accompanying images.
Ethics approval and consent to participate
We excluded all identifying information and obtained informed consent to participate. Because this is a case report, the approval of the ethical review board of our hospital is unnecessary.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kitasato, Y., Midorikawa, R., Uchino, Y. et al. A case of retrograde intussusception at Roux-en-Y anastomosis 10 years after total gastrectomy: review of the literature. surg case rep 2, 123 (2016). https://doi.org/10.1186/s40792-016-0250-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-016-0250-6