Abstract
Background
Couples are considered infertile if they do not conceive over a 12-month period of unprotected intercourse. Studies have shown that female causes accounted for between 25 to 37 percent of infertility worldwide (with larger proportions in sub-Saharan Africa and Southeast Asia) and male causes accounted for between 8 to 22 percent. Both male and female causes accounted for between 21 to 38 percent. Although the majority of ART children are normal, there are concerns about the increased risk for adverse pregnancy outcomes. More than 30 % of ART pregnancies are twins or higher-order multiple gestations (triplets or greater) and more than one half of all ART neonates are the products of multifetal gestations, with an attendant increase in prematurity complications. The aim of this study was to evaiuate the outcome of pregnancies conceived by In-vitro fertilisation compared to those conceived naturally in two hospitals in Douala, Cameroon.
Methods
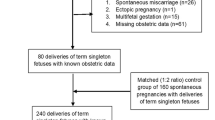
This was a prospective study carried out from October 1, 2011 to September 30, 2012. Participants were recruited from two hospitals: the Douala General Hospital (DGH) and the Clinique de l’ Aéroport (CDA), also in Douala. A total of 102 women were recruited for study: 51 who conceived by IVF (cases) and 51 who conceived naturally (controls). Of the 102 women, 52.9 % were between 31 – 39 years of age, while 21.6 % were above 40.
Results
Participants who conceived through IVF-ET were 4.1 times more likely to undergo cesarean delivery than those who conceived naturally [OR 4.10, 95 % CI 1.78–9.42]. Similarly, a higher percentage of patients in the IVF group than those in the control group have never given birth (33.3 % vs 2.0 %) (P < 0.0001). The percentage of multiple pregnancies was 7.5 times higher in the IVF group than in the control group (14.7 % vs.1.96 %) (P = 0.000).
The leading indication for cesarean delivery was advanced maternal age (27.3 %) followed by IVF or precious pregnancy (18.2 %).
Conclusions
Cesarean delivery was more frequent amongst the IVF group than in the control group. The leading indications for cesarean delivery were advanced maternal age and IVF or precious pregnancy.
The long-term neonatal outcomes of IVF babies beyond 5-min Apgar scores should be studied in Cameroon and follow-up beyond 1 year encouraged.
Similar content being viewed by others
Background
Since the introduction of In-Vitro Fertilization (IVF) in 1978 [1], an estimated 3 million babies have been born worldwide through this procedure [2]. The first baby born after IVF was Louise Brown, by cesarean section, on July 25, 1978 at Oldham hospital in the United Kingdom (UK) [1]. The birth of Louise Brown opened a new era in the management of the infertile couple. Today, there are many developments in terms of pharmaceutical substances, management protocols and laboratory techniques that have completely changed the approach to the management of infertility. The resultant effect is an increase in the number of children born to mothers through assisted reproductive technology (ART) [3].
An estimated 2–3 % of children born in some Scandinavian countries, especially Denmark, are conceived through ART [4]. With the introduction of IVF, there has been a higher rate of cesarean delivery among IVF cases than among women who conceived naturally (41.9 versus 15.5) [5]. This trend can be explained, on the one hand, by the excessive cautiousness of the obstetricians, and on the other by stress on the part of the couples caused by such things as birth trauma or fear of losing the baby. ART pregnancies are more at risk of induction of labour and elective cesarean section than those in the control group [6, 7]. A similar trend in cesarean sections has been reported in Europe and the United States. This rate has remained high over the years, in keeping with the marked increase in the number of IVF centers worldwide [3].
In Cameroon, the practice of ART was introduced in 1998 [8]. Since then an unpublished number of babies have been born to IVF mothers. The aim of this study was to evaluate the outcome of pregnancies conceived by IVF compared to those conceived naturally.
Materials and Methods
The study population included 51 consecutive IVF pregnancies obtained between October 1, 2011 and September 30, 2012 at the Clinique de l’ Aeroport (CDA) in Douala Cameroon, and from other centers out of Cameroon. All the patients were accepted for IVF because this was the only way they could obtain a pregnancy. The indication for IVF was tubal obstruction in all the cases. In Cameroon, IVF does not enjoy medical insurance coverage and so is not available to all socio-economic classes. The analysis included only pregnancies leading to a live birth (>28 weeks gestation or >1000 g birth weight).
Throughout the period of study, the same team of specialists worked in the IVF unit of CDA and treatment protocols remained the same. Controlled Ovarian Hyperstimulation (COH) in all patients was done with human menopausal gonadotropin (hMG) after desensitization with triptorelin (GnRH-a) initiated in the luteal phase (day 21) of the cycle. Human chorionic gonadotropin (hCG) was administered when the leading follicle reached 17–18 mm in diameter as measured by transvaginal sonography and serum E2 levels >500 pg/mL. Standard IVF was used in all cycles. We usually transferred 3 fresh embryos and did not perform micromanipulation in any of the cycles. Our luteal phase support was with progesterone pessaries 200 mg, thrice daily, from the day of embryo transfer to the day of the pregnancy test.
The antenatal care of the patients was performed at CDA and the Douala General Hospital (DGH), and all the patients gave birth in these two centers. Complete data regarding the course and outcome of these pregnancies were available in CDA and the DGH.
The control group consisted of 51 spontaneous gestations that were delivered at the DGH and CDA and were therefore treated by the same obstetric department as the cases. The control for each index pregnancy was the consecutive delivery at CDA and DGH matched for maternal age and with similar expected date of delivery (calculated from the first day of the last normal menstrual period).
The exclusion criteria were women with previous IVF or spontaneous pregnancies who delivered by cesarean section and/or delivered before 28 completed weeks of gestation.
Data collection
The records of the participants were reviewed and the data recorded on standardized survey questionnaires. These data were obtained from the IVF unit files, antenatal care records, and maternal and neonatal delivery and hospitalization records. Data on patients who did IVF in centers out of Cameroon were obtained from the patients.
The data focused essentially on medical and obstetric history, investigations, cause of infertility, pregnancy course and antenatal complications if any, course and mode of delivery, complications during labour and the puerperum, status of the infant at birth, and admissions into the neonatal intensive care unit. In the study group, gestational age was calculated as if the first day of the last menstrual period had been 14 days before the day of oocyte retrieval. Gestational age of the controls was confirmed by routine ultrasound scanning. The variables obtained were then controlled for both groups.
Statistical analysis
Epi-info 6.04 and R software were used for statistical analysis. The chi-squared test was used to compare rates of cesarean and vaginal delivery according to the following characteristics: technique of conception, age range of patients, number of children alive, parity, duration of infertility, IVF center and number of trials, gestational age at delivery, delivery institution. A logistic regression analysis was used to compute Odds ratios (OR’s). Statistical significance was set at P <0.05.
Ethical approval
Ethical clearance was obtained from the Institutional Review Board (IRB) of the Faculty of Health Sciences, University of Buea, Cameroon. Permission was granted by the Directors of the Douala General Hospital and the Clinique de l’Aeroport. Informed consent was obtained from participants.
Results
Maternal socio-demographic characteristics
The socio-demographic characteristics of 51 consecutive pregnancies obtained at the Clinique de l’Aeroport and IVF centers out of Cameroon were matched with those of 51 control spontaneous pregnancies for maternal age, education, marital status, religion and profession. The maternal characteristics of both groups are presented on Table 1. The age of the pregnant women ranged between 31–39. The characteristics studied were similar in both groups.
Obstetric and neonatal characteristics
Women in the IVF group had lesser lifetime pregnancies (p = 000) and delivered less than 2 children (p = 0.035). Consequently, they had less than 2 children alive (p = 0.019) (Table 2). The rate of multiple pregnancies was higher in the IVF group (p = 0000) and all the patients underwent antenatal care visits (Table 3).
Delivery characteristics
Fewer women in the IVF group gave birth vaginally. This was attributed to the significantly higher cesarean delivery rate (58.8 %) in the IVF group compared to 27.5 % (P = 0.002) of the control group. Compared to the trend in spontaneous pregnancies, increase in preterm cesarean deliveries in the IVF group was insignificant. The birth weights and 5-min Apgar scores were similar in both groups (Table 4). The various indications for cesarean delivery are presented on Table 5. The leading factors of the increase in cesarean deliveries among IVF patients were advanced maternal age and IVF or precious baby. We did not induce labour or effect instrumental deliveries. Women with less than 2 children were more likely to have a cesarean delivery in the IVF group than in the controls (P = 0.009). Similarly, those with higher parities had significantly less cesarean deliveries in the IVF group than in the spontaneous pregnancy group (P = 0.005) (Table 6). There was a significantly higher cesarean section rate among women who did IVF out of Cameroon compared to those who went through the procedure in Cameroon (P = 0.006). The duration of infertility (P = 0.073) and the number of IVF trials (P = 0.059) did not influence the cesarean delivery rates to any significant degree (Table 7). In multiple regression analysis, women with IVF were at greater risk of cesarean section than spontaneous pregnancies (OR 4.096, 95 % CI 1.78–9.42) Table 8.
Discussion
Women who conceive after IVF are usually older than those who conceive naturally; they are also often more primiparous, and have a poorer obstetric history [3]. These characteristics are all predictive of increased obstetric risk and adverse outcomes. A comparison with a control group is therefore mandatory if the prediction is to be confirmed or dismissed. In the present study, the obstetric outcomes of 51 IVF pregnancies were compared with those of 51 women who conceived naturally. All subjects were delivered in two hospitals: CDA and DGH, Cameroon. The socio-demographic characteristics were similar in the study and control groups.
Vaginal deliveries were significantly lower in the IVF group, and cesarean sections significantly higher. The global cesarean section rate in this study was 43.14 %: IVF 29.41 %, control group 13.73 %. This rate is similar to those reported previously [5, 6, 9, 10]. Women who conceived by IVF were 4 times more likely to have a cesarean delivery than those who conceived normally. Considering the comparatively low rates of antenatal complications in the control group, it seems reasonable to assume that the high rate of cesarean sections amongst IVF patients was at least in part a reflection of the equally high anxiety surrounding the management of these pregnancies. This assumption is supported by the fact that, amongst the indications for cesarean section, IVF or precious pregnancy was the next most frequent, immediately after advanced maternal age.
We used only maternal age and delivery dates to match the IVF group with that of spontaneous pregnancies; unlike Reubinof et al. who matched cases and controls with such other socio-demographic data as maternal age, parity, ethnic group, residence and delivery date [5].
Most of the IVF cases were women with advanced maternal ages; a fact which in itself could – and did – increase their obstetrical risk factors [11, 12]: the leading indication for cesarean section was advanced maternal age. Obesity and advanced maternal ages were seen to increase the risk of diabetes and cesarean delivery respectively. Among multiparas, this increase in obesity resulted either from excessive post-partum weight retention or then from weight gain between pregnancies. Obesity causes adverse pregnancy outcomes such as pre-eclampsia, gestational hypertension, gestational diabetes and cesarean delivery [13]. Several studies have confirmed that pregnancy is a trigger for excessive weight retention in many women. The Stockholm Pregnancy and Women’s Nutrition (SPAWN) Study carried out in Sweden [14, 15], followed up parous women 15 years after pregnancy and reported several factors that led to excessive weight gain, among which were a higher pre-pregnancy body mass index (BMI), higher gestational weight gain, more retained weight at 1 year post-partum, and a greater weight gain between 1-year and 15-year follow-up. The study also reported greater weight retention among parous women who had not breastfed and who had stopped smoking during pregnancy.
In terms of age distribution among study patients, 52 % were between 31 and 39, while 21.6 % were 40 and above. This corroborates the findings of Al-Turki who reported an average age of 37.38 ± 4.1 years [16] Many, 54.9 % of women in the study group had no children alive, as compared to 39.2 % in the control group. The chances of having multi-fetal pregnancies were 7.5 times higher in cases than in controls. Some studies have linked infertility and IVF treatment with multi-fetal gestations [7, 17], but others have reported only 12.7 % multi-fetal pregnancy rates [18].
There were more preterm deliveries in the IVF group than in the controls. Filicori et al. [19] and other studies attributed the high rates of preterm deliveries in IVF cases to the increased rates of multiple pregnancies after infertility treatments [20, 21]. On the contrary, Yang et al. [22] did not find any differences amongst the two groups.
IVF-assisted conception has been found to lead to negative outcomes such as preterm, low birth weight and perinatal/infant mortality [23]. Several studies have also reported adverse outcomes among women with delayed conception resulting from untreated infertility.
There is strong evidence that advanced maternal age contributes significantly to congenital malformations and later on in the offspring’s adolescence and adulthood, to an increased risk of cancer, neurologic disorders and cardiac diseases [24, 25]. Older paternal age has been associated with an increase in spontaneous abortions, preterm birth and congenital anomalies, with the highest risks when both partners are older [26–28]. Older maternal age requires more aggressive therapies to achieve a pregnancy including transferring more embryos.
Most patients in the IVF group in this study were married, had undergone tertiary level of education and were workers therefore could afford for IVF treatment though not significant. It is worth noting that the funding and regulatory framework for the provision of ART treatment varies considerably around the world and tends to be in line with the level of public and private responsibilities for purchasing healthcare. Public financing of ART ranges from virtually no subsidization in the USA and most developing countries including Cameroon to funding of a limited number of cycles based on female age in most European countries; to unrestricted reimbursement with co-payments in Australia [29]. The International Federation of Fertility Societies (IFFS) survey showed that roughly 50 % of countries had no reimbursement through national health services or private insurers in 2004 [30]; however, there was a higher proportion of countries with some level of subsidization than in the previous survey undertaken in 2002 [2, 29]. Those women who underwent IVF in a foreign country other than Cameroon were more likely to undergo a cesarean section thereby increasing the cost of obstetric care.
Among singleton pregnancies, assisted reproductive technology is associated with increased risks of preterm birth and low birth weight infants, which could explain the difference in Apgar scores reported in other studies [7, 31]. The birth weights and 5 min Apgar scores in our study were comparable between the cases and controls. IVF patients must be counselled about this risk before initiation of treatment.
The other variables studied did not influence much the cesarean delivery rate in our study: duration of infertility, the center where the IVF was performed, the number of IVF trials, the gestational age of pregnancy, and the hospital where the patient gave birth.
In our study we usually transferred 3 fresh embryos but recent studies have shown that the cumulative live birth rate (LBR) is as good as or better with single embryo transfer (SET) over 2 cycles than with two embryos transferred (DET) in 1 cycle, while greatly reducing the probability of a multiple birth [32–34]. There is need for our team to conform to current norms regarding number of embryos to be transferred.
Recent studies have also shown that women who conceived with infertility treatment were 2.95 times (95 % CI: 1.47–5.92) more likely to have planned cesarean deliveries. The increased risk for planned cesarean deliveries among singleton women who conceived with infertility treatment cannot be explained by older maternal age or higher number of morbidities during pregnancy. Counseling for women who conceive with infertility treatments may be needed to decrease unnecessary cesarean deliveries [35]. Furthermore, women with multifetal pregnancies are encouranged to try vaginal delivery [36, 37] or undergo multifetal pregnancy reduction (MFPR) [38–40].
Study limitations
The limitation to this study was the inability of matching the two groups based on gestational age, parity and the type of pregnancy (singleton or multiple). We did not also study the difference in socioeconomic status between study participants who underwent IVF abroad compared to those who did it in Cameroon and the effect of weight gain or obesity on the participants. Our study population was small compared to similar studies with about 500 patients for study and longer study periods such as those of Adler-Levy et al. in Israel [11] and Shevell et al. in a multicenter study in the United States of America (USA) [12].
Furthermore, there was no communication between the two centres where the pregnant IVF women were followed-up or gave birth. Protocols amongst the two centres may have been different accounting for increased rate of cesarean births in one centre than another. Some IVF women started their pregnancy follow-up in other health facilities and only came to the two study centres to give birth. We may have also lost some IVF cases who did not return to any of the two study centres for ANC or pregnancy follow-up especially those who did the IVF out of Cameroon. We did not study separately the outcome of singleton and multifetal pregnancies to quantify the individual effect on cesarean section increase.
Conclusions
The cesarean delivery rate was significantly higher in the cases than controls and there is a four times odds of having a cesarean delivery among those who conceived by IVF than controls. Patients who had delivered at least two times and those with over two children alive were less likely to have a cesarean delivery compared to those who had never delivered.
The leading indication for cesarean delivery was advanced maternal age in primigravida followed by IVF or precious pregnancy because of anxiety, over cautiousness and fear of birth trauma.
Further studies would examine the long-term neonatal outcomes beyond 5 min Apgar scores among IVF babies compared with matched controls and longer period of study beyond one year would be necessary.
References
Steptoe PC, Edwards RG. Birth after the reimplantation of a human embryo. Lancet Lond Engl. 1978;2:366.
Chambers GM, Sullivan EA, Ishihara O, Chapman MG, Adamson GD. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009;91:2281–94.
Mansour R, Ishihara O, Adamson GD, Dyer S, de Mouzon J, Nygren KG, et al. International committee for monitoring assisted reproductive technologies world report: assisted reproductive technology 2006. Hum Reprod. 2014;29:1536–51.
Nyboe Andersen A, Erb K. Register data on assisted reproductive technology (ART) in Europe including a detailed description of ART in Denmark. Int J Androl. 2006;29:12–6.
Reubinoff BE, Samueloff A, Ben-Haim M, Friedler S, Schenker JG, Lewin A. Is the obstetric outcome of in vitro fertilized singleton gestations different from natural ones? A controlled study. Fertil Steril. 1997;67:1077–83.
Olivennes F, Kadhel P, Rufat P, Fanchin R, Fernandez H, Frydman R. Perinatal outcome of twin pregnancies obtained after in vitro fertilization: comparison with twin pregnancies obtained spontaneously or after ovarian stimulation. Fertil Steril. 1996;66:105–9.
Allen VM, Wilson RD, Cheung A, Genetics Committee of the Society of Obstetricians and Gynaecologists of Canada (SOGC), Reproductive Endocrinology Infertility Committee of the Society of Obstetricians and Gynaecologists of Canada (SOGC). Pregnancy outcomes after assisted reproductive technology. J Obstet Gynaecol Can JOGC J Obstétrique Gynécologie Can JOGC. 2006;28:220–50.
Article de presse: Cameroun-La Clinique du bonheur. Revue Continental 2004.
Kozinszky Z, Zádori J, Orvos H, Katona M, Pál A, Kovács L. Obstetric and neonatal risk of pregnancies after assisted reproductive technology: a matched control study. Acta Obstet Gynecol Scand. 2003;82:850–6.
Helmerhorst FM. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004;328:261.
Adler-Levy Y, Lunenfeld E, Levy A. Obstetric outcome of twin pregnancies conceived by in vitro fertilization and ovulation induction compared with those conceived spontaneously. Eur J Obstet Gynecol Reprod Biol. 2007;133:173–8.
Shevell T, Malone FD, Vidaver J, Porter TF, Luthy DA, Comstock CH, et al. Assisted reproductive technology and pregnancy outcome. Obstet Gynecol. 2005;106(5 Pt 1):1039–45.
Villamor E, Cnattingius S. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population-based study. Lancet. 2006;368:1164–70.
Linne Y, Dye L, Barkeling B, Rössner S. Weight development over time in parous women—the SPAWN study—15 years follow-up. Int J Obes. 2003;27:1516–22.
Linné Y, Rössner S. Interrelationships between weight development and weight retention in subsequent pregnancies: the SPAWN study. Acta Obstet Gynecol Scand. 2003;82:318–25.
Al-Turki HA. Obstetric management after infertility treatment. Ann Afr Med. 2010;9:77–80.
Fedder J, Loft A, Parner ET, Rasmussen S, Pinborg A. Neonatal outcome and congenital malformations in children born after ICSI with testicular or epididymal sperm: a controlled national cohort study. Hum Reprod Oxf Engl. 2013;28:230–40.
Boah G. Treatment of infertility in Cameroon: a five year retrospective study (January 2003 - December 2007). Thesis for the award of the Obstetrics and Gynaecology Diploma, FMBS, University of Yaoundé 1; 2008.
Filicori M, Cognigni GE, Gamberini E, Troilo E, Parmegiani L, Bernardi S. Impact of medically assisted fertility on preterm birth. BJOG Int J Obstet Gynaecol. 2005;112 Suppl 1:113–7.
Society of Obstetricians annd Gynaecologists of Canada, Okun N, Sierra S. Pregnancy outcomes after assisted human reproduction. J Obstet Gynaecol Can JOGC J Obstétrique Gynécologie Can JOGC. 2014;36:64–83.
Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Barfield WD, et al. Assisted reproductive technology surveillance--United States, 2011. Morb Mortal Wkly Rep Surveill Summ Wash DC 2002. 2014;63:1–28.
Yang H, Choi YS, Nam KH, Kwon JY, Park YW, Kim YH. Obstetric and perinatal outcomes of dichorionic twin pregnancies according to methods of conception: spontaneous versus in-vitro fertilization. Twin Res Hum Genet Off J Int Soc Twin Stud. 2011;14:98–103.
Ombelet W, Martens G, Sutter PD, Gerris J, Bosmans E, Ruyssinck G, et al. Perinatal outcome of 12 021 singleton and 3108 twin births after non-IVF-assisted reproduction: a cohort study. Hum Reprod. 2006;21:1025–32.
Basso O, Baird DD. Infertility and preterm delivery, birthweight, and Caesarean section: a study within the Danish National Birth Cohort. Hum Reprod. 2003;18:2478–84.
Basso O, Weinberg CR, Baird DD, Wilcox AJ, Olsen J. Subfecundity as a correlate of preeclampsia: a study within the Danish National Birth Cohort. Am J Epidemiol. 2003;157:195–202.
Dain L, Auslander R, Dirnfeld M. The effect of paternal age on assisted reproduction outcome. Fertil Steril. 2011;95:1–8.
Abbas HA, Rafei RE, Charafeddine L, Yunis K. Effects of advanced paternal Age on reproduction and outcomes in offspring. NeoReviews. 2015;16:e69–83.
Luna M, Finkler E, Barritt J, Bar-Chama N, Sandler B, Copperman AB, et al. Paternal age and assisted reproductive technology outcome in ovum recipients. Fertil Steril. 2009;92:1772–5.
Connolly MP, Hoorens S, Chambers GM. The costs and consequences of assisted reproductive technology: an economic perspective. Hum Reprod Update. 2010;16:603–13.
Sullivan EA, Zegers-Hochschild F, Mansour R, Ishihara O, de Mouzon J, Nygren KG, et al. International Committee for Monitoring Assisted Reproductive Technologies (ICMART) world report: assisted reproductive technology 2004. Hum Reprod. 2013;28(5):1375-90.
Isaksson R, Gissler M, Tiitinen A. Obstetric outcome among women with unexplained infertility after IVF: a matched case–control study. Hum Reprod Oxf Engl. 2002;17:1755–61.
Luke B, Brown MB, Wantman E, Stern JE, Baker VL, Widra E, et al. Application of a validated prediction model for in vitro fertilization: comparison of live birth rates and multiple birth rates with 1 embryo transferred over 2 cycles vs 2 embryos in 1 cycle. Am J Obstet Gynecol. 2015;212:676.e1–7.
Fechner AJ, Brown KR, Onwubalili N, Jindal SK, Weiss G, Goldsmith LT, et al. Effect of single embryo transfer on the risk of preterm birth associated with in vitro fertilization. J Assist Reprod Genet. 2014;32:221–4.
Sunde A. Significant reduction of twins with single embryo transfer in IVF. Reprod Biomed Online. 2007;15 Suppl 3:28–34.
Chien L-Y, Lee Y-H, Lin Y-H, Tai C-J. Women who conceived with infertility treatment were more likely to receive planned cesarean deliveries in Taiwan. Hum Fertil. 2015;18(2):141–8.
Fox NS, Gupta S, Melka S, Silverstein M, Bender S, Saltzman DH, et al. Risk factors for cesarean delivery in twin pregnancies attempting vaginal delivery. Am J Obstet Gynecol. 2015;212:106–e1.
Tang HT, Liu AL, Chan SY, Lau CH, Yung WK, Lau WL, et al. Twin pregnancy outcomes after increasing rate of vaginal twin delivery: retrospective cohort study in a Hong Kong regional obstetric unit. J Matern Fetal Neonatal Med. 2015;28:1–7.
Haas J, Mohr Sasson A, Barzilay E, Mazaki Tovi S, Orvieto R, Weisz B, et al. Perinatal outcome after fetal reduction from twin to singleton: to reduce or not to reduce? Fertil Steril. 2015;103:428–32.
van de Mheen L, Everwijn SM, Knapen MF, Haak MC, Engels MA, Manten GT, et al. Pregnancy outcome after fetal reduction in women with a dichorionic twin pregnancy. Hum Reprod. 2015;30:1807–12.
Li R, Chen X, Yang S, Yang R, Ma C, Liu P, et al. Retain singleton or twins? multifetal pregnancy reduction strategies in triplet pregnancies with monochorionic twins. Eur J Obstet Gynecol Reprod Biol. 2013;167:146–8.
Acknowledgements
We would thank Dr. Crista Johnson Abaku of the University of Arizona, USA and Dr Elizabeth Ayuk Ako of the University of Maroua, Cameroon for the valuable suggestions they gave in the editing of this work. Special thanks to the nurses and staff of the Douala General Hospital and Clinique de l’ Aeroport Douala for the support they gave us.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
I declare that I have no competing interest.
Authors’ contributions
TOE, GS and CO conceptualized the study. CO and AS conducted the data collection. TOE and CO conducted the data analysis. TOE wrote the manuscript. JLB, EBP supervised and proof read the manuscript. All the co-authors gave advice on presentation of the results and editing of the text, and approved the final manuscript.
Authors Information
Thomas Obinchemti Egbe, MD: Senior lecturer and Consultant Obstetrician and Gynecologist, Douala General Hospital and Faculty of Health Sciences, University of Buea, Cameroon.
Guy Sandjon, MD: Consultant Obstetrician and Gynecologist, Clinique de l’Aeroport, Douala-Cameroon.
Clovis Ourtchingh, MD: Consultant Obstetrician and Gynecologist, Maroua Regional Hospital, Cameroon.
André Simo, MD: Consultant Obstetrician Gynecologist, Clinique de l’ Aeroport Douala-Cameroon.
Eugene Belley-Priso, MD: Associate Professor and Consultant Obstetrician and Gynecologist, Douala General Hospital and Faculty of Medicine and Biomedical Sciences, University of Yaounde-Cameroon.
Jean Louis Benifla, MD: Professor of Obstetrics and Gynecology, Service de Gynécologie-Obstétrique, Hôpitaux Universitaire Saint-Louis Lariboisière Fernand-Widal, 2 rue Ambroise Pare 75475 Paris Cedex 10.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Egbe, T.O., Sandjon, G., Ourtchingh, C. et al. In-vitro fertilization and spontaneous pregnancies: matching outcomes in Douala, Cameroon. Fertil Res and Pract 2, 1 (2016). https://doi.org/10.1186/s40738-015-0013-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40738-015-0013-2