Abstract
Background
Embarrassment can be a considerable problem for patients with essential tremor (ET) and is a major motivator for treatment. Depression is also a common feature of ET; as many as 35 % of patients report moderate to severe depressive symptoms. Our goal was to assess the associations between these motor and psychosocial factors (tremor, depression, embarrassment) in ET, with a particular interest in more fully assessing the possible association between depression and embarrassment.
Methods
Ninety one ET cases (age 70.4 ± 12.8 years) enrolled in a prospective, clinical-epidemiological study. Depressive symptoms were assessed with the Center for Epidemiological Studies Depression Scale (CESD-10, 0–30 [maximum]), embarrassment, with the Essential Tremor Embarrassment Assessment (ETEA, 0–70 [maximum]), and action tremor, with a detailed in-person neurological examination.
Results
Higher CESD-10 score was significantly associated with higher ETEA score (p = 0.005), but not with increasing tremor severity (p = 0.94). In stratified analyses, cases with no or minimal depressive symptoms had the lowest ETEA scores, cases with moderate depressive symptoms had intermediate ETEA scores, and cases with severe depressive symptoms had the highest ETEA scores (p = 0.01). Furthermore, at each level of tremor severity, cases with more depressive symptoms had more embarrassment.
Conclusions
Depressive symptoms seem to be more than a secondary response to the tremor in ET; they seem to amplify the level of embarrassment and, in addition to their own importance, seem to be a driver of other important clinical outcomes. Earlier treatment of depressive symptoms in ET patients could lessen the burden of secondary embarrassment.
Similar content being viewed by others
Background
According to some estimates, 60 % of essential tremor (ET) patients report embarrassment surrounding their tremor [1]. Embarrassment, classified as a “self-conscious” emotion along with shame and guilt, and in contrast to “basic” emotions such as anger and joy [2], often arises when someone violates a social rule or expectation [3]. Embarrassment is associated with autonomic reactivity including increased heart rate, blood pressure, and sweating and behavioral reactions including gaze avoidance, regret signaling, and avoidance of others [3]. Embarrassment about tremor is a considerable problem for patients with ET [1, 4–7]. It is one of the two main motivators for ET patients to initiate medical therapy [1, 4–6] and it is a particularly strong predictor of receptivity to deep brain stimulation (DBS) surgery among patients with ET [8]. Moreover, feelings of embarrassment can lead to avoidance of social situations and social isolation [9]. Indeed, handling embarrassment and the social effects of tremor has been highlighted by ET patients as one of the top issues not being addressed in their care [10].
Depressive symptoms and depression have been associated with ET in numerous case–control studies [11–17]; according to some estimates, as many as 35 % of patients report moderate to severe depressive symptoms [17]. Similar to embarrassment, depression in ET is often viewed as a secondary response to the disabling condition [11, 14]. Overall; however, depression has not been well studied in ET [11], and there is emerging evidence that depression may be a primary feature of the disease, preceding motor symptoms [18]. This suggests that depression itself could drive other clinical outcomes in ET, such as embarrassment, rather than representing a passive response to the motor symptoms.
Although tremor, embarrassment, and depression may all occur in ET, and likely impact one another, the associations among them have not been the subject of previous analyses. The goal of these analyses was to assess the associations between these motor and psychosocial factors (ie, tremor, embarrassment, and depression) in individuals with ET, with a particular interest in more fully assessing the possible association between depression and embarrassment.
Methods
Participants and evaluation
As described previously, ET cases were enrolled in a clinical-epidemiological study of the epidemiology of movement disorders at Columbia University Medical Center (CUMC) [19, 20]. The large majority of cases were derived from two sources: (1) a computerized billing database of ET patients at the Neurological Institute of New York, CUMC, and (2) advertisements to members of the International Essential Tremor Foundation. One-hundred-forty-one cases were enrolled (2009–2014). During that time period, a formal assessment of embarrassment was added. Ninety-one cases were enrolled after the embarrassment assessment was added. Cases had all received a diagnosis of ET from their treating neurologist and were confined to a geographical area within 2 h driving distance of CUMC. Prior to enrollment, one of the authors (E.D.L.) reviewed the office records of identified patients; those with diagnoses of or physical signs consistent with other movement disorders were excluded.
The CUMC Internal Review Board approved of all study procedures. Written informed consent was obtained upon enrollment. Analysis of data was also approved by the Internal Review Board at Yale School of Medicine.
During the in-person evaluation, the trained research worker administered a series of structured clinical questionnaires (demographics, clinical features, medications, family history). The research worker also administered the Center for Epidemiological Studies Depression Scale (CESD-10) (0–30 [higher scores indicate greater depressive symptoms]) [21]. The CESD is a self-report measure of 10 questions about the frequency of experiencing (0 to 3 for each item) different depressive symptoms. It is a reliable and valid instrument [22]. In addition, the Essential Tremor Embarrassment Assessment (ETEA), an assessment of tremor-related embarrassment (range = 0–70 [maximal embarrassment]) [15] was administered to ET patients [4]. The ETEA, which is a valid and reliable instrument [4], comprises 14 questions that assess overall embarrassment and its effects on the patient’s desire for tremor medication, as well as embarrassment in a variety of situations (eg, eating in public, speaking in front of a group, social situations). Each item is rated from 0 to 5, with higher scores indicating greater embarrassment [4].
All cases underwent a standardized videotaped tremor examination, which included tests of postural and kinetic tremors and assessments for the presence of other involuntary movements. The aim was to use the videotape to carefully validate ET diagnoses using rigorous research-grade diagnostic criteria [23]. Thus, each videotape was reviewed by a senior neurologist specializing in movement disorders (E.D.L.) who confirmed the ET diagnoses using Washington Heights-Inwood Genetic Study of ET (WHIGET) diagnostic criteria (moderate or greater amplitude kinetic tremor [tremor rating ≥2] during three or more tests or a head tremor, in the absence of Parkinson’s disease, dystonia or another cause) [23]. The neurologist also rated postural and kinetic tremor (range = 0–3) during 12 videotaped tests and computed a total tremor score (range = 0–36).
Statistical analyses
Data were analyzed in SPSS (Version 22.0). Chi-square tests were used to assess associations within categorical data. Total tremor score, ETEA score and CESD-10 score were all normally distributed (Kolmogorov-Smirnov Test p values = 0.67, 0.70, 0.35, respectively); hence, parametric tests (eg, Pearson’s r) were used when assessing these variables.
Several CESD-10 cut-offs have been recommended for depression, including a score ≥10 [21], and a more conservative score ≥20 [24]. To incorporate both sets of recommendations, as in a prior set of analyses [25], we divided cases into three groups based on their CESD-10 score: 0–9 (no or minimal depressive symptoms), 10–19 (moderate depressive symptoms), ≥20 (severe depressive symptoms). Scores > 20 have high sensitivity and specificity for the diagnosis of Major Depressive Disorder as defined in the DSM [26–28]. To derive strictly mathematical cut-points, CESD-10 scores were also stratified into quartiles (≤3, 4–7, 8–12, ≥13).
Linear regression models were used to assess the associations between variables.
Results
The 91 ET cases had a mean age of 70.4 ± 12.8 years and a mean tremor duration of 36.9 ± 18.7 years. The mean CESD-10 score was 9.5 ± 6.2 (range = 0–26) (Table 1), with 47 (51.6 %) having no or minimal depressive symptoms, 37 (40.7 %) having moderate depressive symptoms and 7 (7.7 %) having severe depressive symptoms. Six (6.6 %) cases had CESD-10 scores > 20, of whom one (1.1 %) was also taking an antidepressant medication. The mean ETEA score was 24.2 ± 16.9 (range = 0–61).
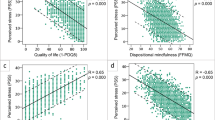
Higher total tremor score was associated with higher ETEA score (Pearson’s r = 0.27, p = 0.016 and see Fig. 1); however, higher total tremor score was not associated with higher CESD-10 score (Pearson’s r = 0.008, p = 0.94).
ETEA score by total tremor score in each CESD-10 quartile. At each level of tremor severity (ie, at each total tremor score), higher level of depressive symptoms was associated with more embarrassment; thus, cases in the lowest CESD-10 quartile (ie, fewest depressive symptoms) had the lowest levels of embarrassment and cases in the highest CESD-10 quartile (ie, most depressive symptoms) had the highest levels of embarrassment
Higher CESD-10 score was associated with higher ETEA score (Pearson’s r = 0.29, p = 0.005, Fig. 2). Furthermore, cases with no or minimal depressive symptoms had the lowest ETEA scores, cases with moderate depressive symptoms had intermediate ETEA scores, and cases with severe depressive symptoms had the highest ETEA scores (p = 0.01, Table 2). Similarly, there was a significant association between CESD-10 score quartile and ETEA score (p = 0.001, Table 2).
At each level of tremor severity (ie, at each total tremor score), higher level of depressive symptoms was associated with more embarrassment; thus, cases in the lowest CESD-10 quartile (ie, fewest depressive symptoms) had the lowest levels of embarrassment and cases in the highest CESD-10 quartile (ie, most depressive symptoms) had the highest levels of embarrassment (Fig. 1).
Cases with severe depressive symptoms (CESD-10 score ≥20) had higher ETEA scores than those with fewer depressive symptoms, despite the fact that they had similar levels of tremor severity (Table 3). Indeed, mean level of embarrassment was 50 % higher in cases with severe depressive symptoms than those with no or minimal depressive symptoms (31.4 vs. 19.9, Table 3) despite nearly identical total tremor scores (19.0 vs. 19.6, Table 3). This was associated with greater medication usage; 7 of 7 (100 %) cases with severe depressive symptoms had taken medication for tremor vs. 28/47 (59.6 %) of those with no or minimal depressive symptoms (chi-square test = 4.37, p = 0.037, Table 3).
In a subgroup analysis of 58 patients with family history of ET or tremor, higher CESD-10 score was associated with higher ETEA score (Pearson’s r = 0.30, p = 0.02). Furthermore, cases with no or minimal depressive symptoms had the lowest ETEA scores (n = 28, 21.9 ± 17.6), cases with moderate depressive symptoms had intermediate ETEA scores (n = 25, 28.6 ± 16.4), and cases with severe depressive symptoms had the highest ETEA scores (n = 5, 36.8 ± 18.2) (linear regression analysis, p = 0.04).
Discussion
Tremor, depression, and embarrassment may co-occur in many ET patients, making this an important constellation of motor and psychosocial factors. Hence, it is surprising that the associations between these factors have not been delineated previously. In the current study, higher depressive symptom scores were associated with significantly greater levels of embarrassment (p = 0.005). Indeed, cases with no or minimal depressive symptoms had the lowest embarrassment scores, cases with moderate depressive symptoms had intermediate embarrassment scores, and cases with severe depressive symptoms had the highest embarrassment scores (p = 0.01). Cases with severe depressive symptoms (CESD-10 score ≥20) had higher ETEA scores than those with fewer depressive symptoms, despite the fact that they had similar levels of tremor severity. Indeed, level of embarrassment was 50 % higher in cases with severe depressive symptoms than those with minimal depressive symptoms despite nearly identical total tremor scores.
As noted above, at each level of tremor severity, cases who had more depressive symptoms had more embarrassment. While it is conceivable that greater embarrassment could lead to more depression, it is more plausible that the converse is the case, that is, that depressive symptoms are amplifying the level of embarrassment. The CESD-10 scale measures the full range of depressive symptoms including somatic symptoms such as poor appetite, decreased energy, psychomotor retardation, and insomnia. Embarrassment is unlikely to be the direct cause of any of these depressive symptoms. Depression often acts as an amplifier of related symptoms in psychiatric disorders. Depression is associated with an increase in the distress and disability associated with chronic pain [29]. Self-conscious emotions including shame, guilt, and embarrassment increase, often dramatically, during an episode of major depressive disorder [30].
More broadly, these data also suggest that depressive symptoms are a driver of other important clinical outcomes in ET rather than merely a passive, secondary response to tremor. Depressive symptoms and/or depression have been reported as more prevalent in ET cases than controls in numerous studies [11–17]. Indeed, in the current study, more than half of the cases had moderate or severe depressive symptoms. Despite its high prevalence, the causes, effects and natural history of depression in ET have not been studied in any detail [11], although in a prior set of analyses, we showed that depressive symptoms were a strong predictor of tremor-related quality of life in ET [25]. Furthermore, its relationship to the motor features of ET may be complex. Emerging evidence suggests that depression may even be a primary feature of ET, preceding the motor features [18]. This finding has precedent in other movement disorders, including Huntington’s disease and Parkinson’s disease [31, 32]. Studies that examine the clinical correlates of depression and its relationships with other disease features in ET are therefore of importance.
One clinical implication of the current findings is that they increase the importance of treating depressive symptoms in patients with ET as, in addition to reducing depressive symptoms, it may reduce embarrassment as well. Embarrassment is a considerable problem for ET patients [1, 4–6]. It is one of the two main motivators for initiating medical therapy [1, 4–6] and can further lead to avoidance of social situations and social isolation [9]. Indeed, handling the embarrassing social effects of tremor has been highlighted by patients as one of the top issues not being addressed in their current care [10]. While the effect of depression treatment has not been specifically studied in ET patients, the effect size for the treatment of depressive symptoms with antidepressant medication in patients with Parkinson’s disease is moderate [33]. The findings of the current study also suggest that the treatment of depression with psychotherapy in patients with ET should assess and target embarrassment as well as the more usual depressive symptoms. In ET patients with depression and prominent embarrassment, referral to a psychotherapist who utilizes a symptom-based therapy method such as Cognitive-Behavioral Therapy (CBT) or Problem-Solving Therapy (PST) could be preferable to insight-oriented psychodynamic therapy.
Our cases had a mean CESD-10 score of 9.5 ± 6.2. A feature of this clinical-epidemiological study, but not of these analyes, was the enrollment of control subjects of similar age (n = 177, 74.9 ± 9.5 years). The mean CESD-10 score of these controls was only 6.7 ± 4.6, a value that was lower than that of our cases (t test = 3.84, p <0.001), indicating a higher burden of depressive symptoms among our cases, as has been reported in ET in the past [11–17].
This study should be interpreted within the context of certain limitations. First, the study was cross-sectional, so that we are not able to directly address issues of causality. Second, the sample size was modest and this may have limited our ability to detect associations. However, the study was able to detect significant main effects between several of the key variables. Third, depressive symptoms were assessed with a brief, validated screening instrument; it is possible that more in-depth psychiatric assessments could have uncovered additional associations of interest. For example, the relationship between symptoms of anxiety, including social anxiety, and embarrassment and the relationship between ET and other self-conscious emotions. In particular, anxiety is also a common feature of patients with ET [9, 17] and it could impact upon levels of embarrassment. Future studies could further assess such relationships. Fourth, we did not collect data on past history of depression in our cases; such information could have supplemented the data we collected on current depressive symptoms.
The study also had several strengths. First, to our knowledge, it is the only study to have assessed this particular gap in knowledge and these particular associations. Second, this was not a retrospective study or chart review; the study cohort was enrolled prospectively, with a standardized assessment.
Conclusions
In summary, we found that cases with severe depressive symptoms had higher embarrassment scores than those with fewer depressive symptoms, despite the fact that they had similar levels of tremor severity. Furthermore, greater tremor severity was not associated with more depressive symptoms. One interpretation of these data is that depressive symptoms are more than a secondary response to the tremor in ET; in addition to being clinically important in themselves, they also seem to drive other important outcomes such as embarrassment. Earlier treatment of depressive symptoms in ET patients might be a strategy to lessen the burden of secondary embarrassment.
Abbreviations
(CES-D), Center for Epidemiological Studies Depression Scale; (CBT), Center for Epidemiological Studies Depression Scale; (CUMC), Columbia University Medical Center; (DBS),Deep brain stimulation; (ET), Essential tremor; (ETEA), Essential Tremor Embarrassment Assessment; (PST), Essential Tremor Embarrassment Assessment; (WHIGET), Washington Heights-Inwood Genetic Study of ET
References
Louis ED, Rios E. Embarrassment in essential tremor: prevalence, clinical correlates and therapeutic implications. Parkinsonism Relat Disord. 2009;15:535–8.
Lewis M, Haviland-Jones JM, editors. Handbook of Emotions. New York: The Guilford Press; 2000. p. 623–36.
Keltner D, Buswell BN. Embarrassment: its distinct form and appeasement functions. Psychol Bull. 1997;122:250–70.
Traub RE, Gerbin M, Mullaney MM, Louis ED. Development of an essential tremor embarrassment assessment. Parkinsonism Relat Disord. 2010;16:661–5.
Holding SJ, Lew AR. Relations between psychological avoidance, symptom severity and embarrassment in essential tremor. Chronic Illn. 2015;11:69–71.
Louis ED. Clinical practice. Essential tremor. N Engl J Med. 2001;345:887–91.
Koller W, Biary N, Cone S. Disability in essential tremor: effect of treatment. Neurology. 1986;36:1001–4.
Louis ED, Gillman A. Factors associated with receptivity to deep brain stimulation surgery among essential tremor cases. Parkinsonism Relat Disord. 2011;17:482–5.
Schneier FR, Barnes LF, Albert SM, Louis ED. Characteristics of social phobia among persons with essential tremor. J Clin Psychiatry. 2001;62(5):367–72.
Louis ED, Rohl B, Rice C. Defining the treatment gap: what essential tremor patients want that they are not getting. Tremor Other Hyperkinet Mov (N Y). 2015;5:331. doi:10.7916/D87080M9. eCollection 2015.
Louis ED. Non-motor symptoms in essential tremor: A review of the current data and state of the field. Parkinsonism Relat Disord. 2016;22 Suppl 1:S115–8.
Dogu O, Louis ED, Sevim S, Kaleagasi H, Aral M. Clinical characteristics of essential tremor in Mersin, Turkey--a population-based door-to-door study. J Neurol. 2005;252:570–4.
Li ZW, Xie MJ, Tian DS, Li JJ, Zhang JP, Jiao L, et al. Characteristics of depressive symptoms in essential tremor. J Clin Neurosci. 2011;18:52–6.
Chandran V, Pal PK, Reddy JY, Thennarasu K, Yadav R, Shivashankar N. Non-motor features in essential tremor. Acta Neurol Scand. 2012;125:332–7.
Fabbrini G, Berardelli I, Falla M, Moretti G, Pasquini M, Altieri M, et al. Psychiatric disorders in patients with essential tremor. Parkinsonism Relat Disord. 2012;18:971–3.
Lee SM, Kim M, Lee HM, Kwon KY, Koh SB. Nonmotor symptoms in essential tremor: Comparison with Parkinson’s disease and normal control. J Neurol Sci. 2015;349:168–73.
Sengul Y, Sengul HS, Yucekaya SK, Yucel S, Bakim B, Pazarci NK, et al. Cognitive functions, fatigue, depression, anxiety, and sleep disturbances: assessment of nonmotor features in young patients with essential tremor. Acta Neurol Belg. 2014;115:281–7.
Louis ED, Benito-Leon J, Bermejo-Pareja F. Self-reported depression and anti-depressant medication use in essential tremor: cross-sectional and prospective analyses in a population-based study. Eur J Neurol. 2007;14:1138–46.
Louis ED, Rao AK. Functional aspects of gait in essential tremor: a comparison with age-matched parkinson’s disease cases, dystonia cases, and controls. Tremor Other Hyperkinet Mov (N Y). 2015;27:5. doi:10.7916/D8B27T7J. eCollection 2015.
Louis ED, Factor-Litvak P, Michalec M, Jiang W, Zheng W. Blood harmane (1-methyl-9H-pyrido[3,4-b]indole) concentration in dystonia cases vs. controls. Neurotoxicology. 2014;44:110–3.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84.
Bjorgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20:429–36.
Louis ED, Ottman R, Ford B, Pullman S, Martinez M, Fahn S, et al. The Washington Heights-Inwood Genetic Study of Essential Tremor: methodologic issues in essential-tremor research. Neuroepidemiology. 1997;16:124–33.
Kirsch-Darrow L, Fernandez HH, Marsiske M, Okun MS, Bowers D. Dissociating apathy and depression in Parkinson disease. Neurology. 2006;67:33–8.
Louis ED, Huey ED, Gerbin M, Viner AS. Depressive traits in essential tremor: impact on disability, quality of life, and medication adherence. Eur J Neurol. 2012;19:1349–54.
Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine ED. Screening for depression in elderly primary care patients. A comparison of the Center for Epidemiologic Studies-Depression Scale and the Geriatric Depression Scale. Arch Intern Med. 1997;157:449–54.
Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med. 1999;159:1701–4.
Louis ED, Huey ED, Gerbin M, Viner AS. Apathy in essential tremor, dystonia, and Parkinson’s disease: a comparison with normal controls. Mov Disord. 2012;27:432–4.
Von Korff M, Simon G. The relationship between pain and depression. Br J Psychiatry Suppl. 1996:101–8.
Buist-Bouwman MA, Ormel J, de Graaf R, de Jonge P, van Sonderen E, Alonso J, et al. Mediators of the association between depression and role functioning. Acta Psychiatr Scand. 2008;118:451–8.
Tabrizi SJ, Scahill RI, Owen G, Durr A, Leavitt BR, Roos RA, et al. Predictors of phenotypic progression and disease onset in premanifest and early-stage Huntington’s disease in the TRACK-HD study: analysis of 36-month observational data. Lancet Neurol. 2013;12:637–49.
Chen JJ, Marsh L. Depression in Parkinson’s disease: identification and management. Pharmacotherapy. 2013;33:972–83.
Troeung L, Egan SJ, Gasson N. A meta-analysis of randomised placebo-controlled treatment trials for depression and anxiety in Parkinson’s disease. PLoS One. 2013;8:e79510.
Acknowledgements
None.
Funding
Dr. Louis has received research support from the National Institutes of Health: NINDS #R01 NS086736, #R01 NS094607 and #R01 NS076837. This funding body played no role in the design of the study, the collection, analysis, and interpretation of data, or the writing of the manuscript.
Availability of data and material
The dataset supporting the conclusions of this article is available in an SPSS file at Yale University, Department of Neurology.
Authors’ contributions
EDL designed the study, over-saw the collection of data, obtained funding, performed the initial statistical analyses, and prepared the initial manuscript. SC participated in the design of study, design of additional analyses, interpretation of data, and manuscript preparation. EDH participated in the design of study, design of additional analyses, interpretation of data, and manuscript preparation. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interest.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The CUMC Internal Review Board approved of all study procedures. Written informed consent was obtained upon enrollment. Analysis of data was also approved by the Internal Review Board at Yale School of Medicine. This manuscript does not involve the use of animal data or tissue.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Louis, E.D., Cosentino, S. & Huey, E.D. Depressive symptoms can amplify embarrassment in essential tremor. J Clin Mov Disord 3, 11 (2016). https://doi.org/10.1186/s40734-016-0039-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40734-016-0039-6