Abstract
Background
The National Comprehensive Cancer Network (NCCN) and the Society of Gynecologic Oncology (SGO) recommend lymph node sampling (LNS) as a key component in the surgical staging of high-grade endometrial cancer. Our goal was to examine surgical staging patterns for high-grade endometrial cancer in the United States.
Methods
The National Cancer Data Base (NCDB) was searched for patients who underwent surgery for serous, clear cell, or grade 3 endometrioid endometrial cancer. Outcomes were receipt of LNS and overall survival (OS). Multivariate logistic regression was used to examine receipt of LNS in Stage I–III disease based on race (White vs. Black), income, surgical volume, and distance traveled to care. Multivariate Cox proportional hazards regression modeling was used to assess OS based on stage, race, income, LNS, surgical volume, and distance traveled.
Results
Forty-two thousand nine hundred seventy-three patients were identified: 76% White, 53% insured by Medicare/Medicaid, 24% traveled >30 miles, and 33% stage III disease. LNS was similar among White and Black women (81% vs 82%). LNS was more common among >30 miles traveled (84% vs 81%, p < 0.001), higher surgical volume (83% vs 80%, p < 0.001), and academic centers (84% vs 80%, p < 0.001). In multivariate analysis, higher income, higher surgical volume, Charlson-Deyo score, and distance traveled were predictors of LNS. Stage III disease (HR 3.39, 95% CI 3.28–3.50), age (10-year increase; HR 1.63, 95% CI 1.61–1.66), lack of LNS (HR 1.64, 95% CI 1.56–1.69), and low income (HR 1.20, 95% CI 1.14–1.27) were predictors of lower survival.
Conclusions
Surgical care for high-grade endometrial cancer in the United States is not uniform. Improved access to high quality care at high volume centers is needed to improve rates of recommended LNS.
Similar content being viewed by others
Background
Endometrial cancer is the most common form of gynecologic cancer in the United States, with more than 60,000 new cases and 10,470 deaths estimated to occur in 2016 [1]. The majority of endometrial cancers are Type I, grade 1–2 endometrioid adenocarcinoma and have an excellent prognosis, most often presenting as low-grade and at an early stage. Conversely, Type II cancers, including uterine papillary serous carcinoma (UPSC), clear cell carcinoma (CC), and grade 3 endometrioid adenocarcinoma, often have a much worse prognosis, presenting with extra-uterine disease [2–5]. UPSC, CC, and grade 3 endometrioid adenocarcinoma represent 10–27% of incident endometrial cancer cases, but account for over 70% of endometrial cancer deaths [6].
The National Comprehensive Cancer Network (NCCN) and the Society of Gynecologic Oncology (SGO) support pelvic and para-aortic lymphadenectomy for patients with high-grade endometrial cancer, including UPSC, CC, and grade 3 endometrioid adenocarcinoma [7–9]. Although the surgical guidelines are clear, there is a demonstrated racial disparity between Whites and Blacks in de facto surgical management [10]. Black women are less likely to undergo surgery for endometrial cancer [11–13]. While many authors have examined associations between race and the epidemiology, treatment, and outcomes of endometrial cancer, no author has explored the relationship between race and the type of surgery performed. Disparities also exist for the distance traveled to receive care for endometrial cancer, although the available data are limited. In 2011, Benjamin et al. performed a statewide analysis of endometrial cancer care in Arizona and found that minorities travel farther than Whites to receive care, while patients with government-funded insurance travel farther than patients with other types of insurance [14]. There are no other regional or national studies examining the relationship between receipt of care for endometrial cancer and travel distance. Based on the NCCN and the SGO recommendations of lymph node sampling during the surgical staging of high-grade endometrial cancer, we explored surgical practice patterns and disparities in the treatment of UPSC, CC, and grade 3 endometrioid adenocarcinoma in the United States.
Methods
Data source
The National Cancer Data Base (NCDB) is a national oncology outcomes database in the United States, founded in 1989 by the American College of Surgeons (ACS) and its Commission on Cancer (CoC) Program. One of the largest cancer registries in the world, the NCDB collects data on 70% of all new cancer diagnoses in the U.S. from over 1,500 reporting hospitals [15]. The NCDB data coding process is standardized according to the CoC Registry Operations and Data Standards Manual, the American Joint Committee for Cancer (AJCC) Manual for Staging of Cancer, and the International Classification of Disease for Oncology, Third Edition (ICD-O3). For the current study, all data were extracted from medical records by trained and certified tumor registrars. Our Institutional Review Board granted this study an exemption status due to the de-identified nature of the dataset.
Case selection
The NCDB Participant User File was searched for all patients who underwent surgery for UPSC, CC, or grade 3 endometrioid adenocarcinoma. Data were available from the years 1998 to 2012. Demographic and socioeconomic information was recorded for each patient, including age, race, income, education and insurance status. Clinical and pathologic data collected included International Federation of Gynecology and Obstetrics (FIGO) staging, Charlson-Deyo comorbidity score, number of regional lymph nodes examined, number of para-aortic lymph nodes examined, peritoneal cytology status, and performance of omentectomy. While FIGO staging criteria were updated in 2009, we did not reclassify patients for our analysis. The FIGO 2009 staging criteria changes to Stage I would not alter our Stage I designation; and changes to Stage II and Stage III designation could not be fully addressed from data available in the NCDB. Patients were further categorized based on treatment center type (academic research center, community cancer program/other, comprehensive community cancer program), hospital endometrial cancer surgical volume, and distance travelled to receive care (≤ or > 30 miles). Surgical volume was defined based on strategies previously utilized in NCDB-related publications [16]. Hospital surgical volume was annualized based on the total number of endometrial cancer patients and the total number of years of reported data. Surgical volume groups were then categorized by quartile rank: 75th percentile = very-high volume (>31.7 cases/year); 51st–75th percentile = moderately-high volume (13.3–31.6 cases/year); 25th–50th percentile = intermediate volume (6.7–13.2 cases/year); and <25th percentile = low volume (<6.7 cases/year). While distance to care was recorded continuously in the NCDB, we stratified distance in two groups, ≤ 30 miles and > 30 miles, based on the overall mean distance traveled (mean = 30).
Statistical analysis
The main outcomes examined were the rates of lymph node sampling and overall survival (OS). Multivariate logistic regression was used to explore differences in receipt of lymph node sampling (LNS). Stage IV patients were excluded as LNS may not always be necessary or indicated in this patient population. Given that there is not a standard number of sampled lymph nodes to constitute ‘adequate’ staging, we performed a sensitivity analysis using replicate logistic models considering various cut points for the number of lymph nodes sampled: (1) 0 vs. 1+; (2) 0–1 vs. 2+; (3) 0–4 vs. 5+; (4) 0–9 vs. 10+; (5) 0–14 vs. 15+; (6) 0–19 vs. 20+. In addition, logistic regression modeling was used to explore a subset of patients with available data on para-aortic LNS. The following variables were assessed for possible associations with receipt of LNS (as categorized by the NCDB): race (White, Black, other), median-household income (defined based on a specific patient’s zip code at the time of diagnosis compared against 2012 American Community Survey data: <$38,000; $38,000 to $47,999; $48,000 to $62,999; or > $63,000), education (defined as the percentage of the population with a high school diploma as the highest degree obtained in a specific patient’s zip code: ≥21%, 13–20%, 7–12.9%, or <7%), insurance status (not insured, private insurance, Medicaid, Medicare, or other), Charlson-Deyo comorbidity score (Charlson score of 0, 1, or ≥2), type of treatment center (comprehensive community cancer program, community cancer program/other, or academic research center), hospital endometrial cancer surgical volume, and distance traveled to receive care. Receipt of peritoneal cytology and omentectomy were inconsistently reported, and therefore excluded from our assessment. Given limited numbers regarding minorities other than Blacks, we grouped additional minorities as ‘other’ for model parsimony. Table 1 lists patient and clinical characteristics based on race for patients with Stage I–III disease. Categorical variables were compared using chi-square tests. Multivariate Cox proportional hazards regression modeling and Kaplan Meier curves were used to assess associations between clinical variables and OS. OS models were explored utilizing distance to care as both continuous and dichotomous (≤30 miles and > 30 miles). Statistical significance was considered a priori at a two-sided p-value of <0.05. We defined a clinically significant difference between categorical groups to exist if a p-value of <0.05 was associated with a ≥5% difference. Statistical analyses were conducted using SAS v. 9.3 software (SAS Institute, Inc., Cary, NC) and survival plots were created using Spotfire S+ v. 8.1 (TIBCO, Palo Alto, CA).
Results
Patient and cancer characteristics
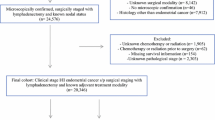
A total of 53,841 patients were identified who underwent surgery and had available lymph node status data between 1998 and 2012 for high-grade endometrial cancer, including UPSC, CC, and grade 3 endometrioid adenocarcinoma. Patients were excluded from our analysis if lymph node status was not available. After excluding Stage IV patients, 42,973 patients were available for analysis. Table 1 lists demographic, socioeconomic, and clinical characteristics. Grade 3 endometrioid adenocarcinoma accounted for 31,104 cases (72%), while UPSC accounted for 8,238 cases (19%), and CC accounted for 3,631 cases (9%). Sixty–seven percent (n = 28,940) had Stage I/II disease, while 33% (n = 14,033) had Stage III disease. Seventy–six percent of patients were White (n = 35,694), while 12% were Black (n = 5,285). The majority of patients were insured via Medicaid and Medicare (53%) or private insurance (41%). Most patients underwent surgery at a comprehensive community cancer program (52%) or at an academic/research center (42%). Seventy–one percent of patients received surgery at very-high volume centers (>31.7 cases/year). The mean distance traveled to care was 30 miles.
Receipt of surgical staging
In our cohort of 42,973 patients, 35,158 (82%) underwent regional LNS. In univariate analysis, receipt of care at an academic center (84% vs 70%, p < 0.001) and at a hospital with higher endometrial cancer surgical volume (>75th percentile, 83% vs 71% (all others), p < 0.001) were both associated with receipt of LNS (data not shown).
In multivariate analysis, income, distance traveled to care, Charlson-Deyo comorbidity score, and hospital surgical volume were all significant predictors of receipt of LNS. The sensitivity of these results were examined using replicate logistic models considering various cut points for the number of lymph nodes removed, which produced identical predictors of more complete staging to those reported above for all replicate models (0 vs. 1+; 0–1 vs. 2+; 0–4 vs. 5+; 0–9 vs. 10+; 0–14 vs. 15+; 0–19 vs. 20+). Surgical volume and type of cancer center were strongly associated with each other, and thus were not considered concomitantly in multivariate analysis: Surgical volume was incorporated into the multivariate model. Receipt of LNS was less likely in patients with a Charleson-Deyo comorbidity score of ≥1 (OR 0.73, 95% CI 0.68 to 0.78) (Table 2), or with an annual income ≤ $38,000 (38 k-$47,999: OR 1.08, 95% CI 0.98 to 1.18; $48 k-$62,999: OR 1.20, 95% CI 1.10 to 1.32; >$63 k: OR 1.33, CI 1.21 to 1.46). Compared to very-high volume hospitals (>31.7 cases/year), receipt of LNS was also less likely in patients receiving surgical care at moderately-high volume hospitals (OR 0.65, 95% CI 0.61 to 0.71), intermediate volume (OR 0.51, 95% CI 0.45 to 0.56), or low volume (OR 0.39, 95% CI 0.33 to 0.45). Receipt of LNS was more likely in patients who traveled >30 miles to receive their care (OR 1.12, 95% CI 1.04 to 1.21).
In our subset analysis of receipt of para-aortic LNS, there were 11,068 evaluable patients with para-aortic lymph node sampling status recorded. A total of 5,554 (50%) patients underwent para-aortic LNS. Significant predictors of receipt of para-aortic LNS were similar to our main model, including Black race not being associated with a difference in receipt of para-aortic LNS (OR 1.03, 95% CI 0.92 to 1.16) (Table 3).
Overall survival
Multivariate Cox proportional hazards analysis was performed to identify predictors of overall survival while controlling for patient age, race, income, receipt of lymph node staging, stage of disease, adjuvant chemotherapy or radiation, hospital surgical volume, and distance to care (Table 4). A total of 31,647 patients had sufficiently matured data available for survival analysis. Compared to Stage I/II disease, Stage III disease was associated with lower overall survival (HR 3.39, 95% CI 3.28 to 3.50) (Fig. 1a). Patients who received LNS had improved overall survival (HR 0.61, 95% CI 0.59 to 0.64) (Fig. 1b). Although LNS was more common at higher volume surgical centers, surgical volume was not a statistically significant predictor of overall survival (Table 4). Black women compared to White women had a poorer overall survival (HR 1.36, 95% CI 1.29 to 1.42) (Fig. 1c). While patients who traveled >30 miles were more likely to receive LNS, distance to care was not associated with overall survival (HR 1.00, 95% CI 0.99 to 1.00, p = 0.758) (Fig. 1d).
Multivariate predictors of overall survival in high-grade endometrial cancer. a. Overall survival curve based on stage of disease. b. Overall survival curve based on receipt of lymph node sampling. c. Overall survival curve based on race (White vs. Black). d. Overall survival curve based on distance to care (≤30 miles vs. >30 miles)
In our multivariate subset analysis of para-aortic LNS, significant predictors of OS were similar to our main model, including Black race (HR 1.27, 95% CI 1.10 to 1.46). Other significant predictors included Stage III/disease (HR 3.14, 95% CI 2.80 to 3.52) and receipt of para-aortic LNS (HR 0.65, 95% CI 0.59 to 0.73). Similar to our main cohort, surgical volume and distance to care were not associated with OS.
Discussion
The management of high-grade endometrial cancer relies on the cornerstone of surgical staging. The NCCN recommends that surgical staging for high-grade endometrial cancer, including UPSC, CC, and grade 3 endometrioid adenocarcinoma, consist of pelvic and para-aortic lymphadenectomy [7]. This removal of lymph nodes also affords the opportunity to appropriately tailor adjuvant therapy. In this cohort of high-grade endometrial cancer patients, our data, after controlling for the receipt of adjuvant therapy, demonstrate that receipt of regional LNS is associated with improved survival (HR 0.61, 95% CI 0.59 to 0.64). A number of observational studies have also shown that women who undergo lymph node staging have improved clinical outcomes [17–20]. While the interpretation of such observational studies is heavily limited by selection bias, and no randomized trials specific to a high-risk histology cohort have been performed, the removal of lymph nodes not only follows NCCN recommendations for women with UPSC, CC, and grade 3 endometrioid adenocarcinoma, but also guides the use of appropriate adjuvant therapy [7]. Therefore, the lower rates of NCCN-recommended staging of high-grade endometrial cancer at lower surgical volume centers and among lower income women is a point of concern.
Epidemiological studies have demonstrated that Black women, as compared to White women, are disproportionately affected by high-risk histologic types of endometrial cancer and are less likely to undergo surgical management [11–13, 21–24]. Our study is the first to examine factors associated with the receipt of LNS as part of surgical management, and demonstrates that receipt of LNS for high-grade endometrial cancer is similar among Blacks and Whites (81% vs 80%, respectively). While disparities in the surgical management of high-risk endometrial cancer have improved, Black women, compared to White women, have worse overall survival (Table 4) (OR 1.36, 95% CI 1.29 to 1.42).
Prior studies have also demonstrated that women with endometrial cancer are more likely to undergo lymph node dissection at high-volume hospitals compared to low-volume hospitals (66% vs 35%, p < 0.001) [25]. However, treatment at high-volume centers has not been shown to improve overall survival [25–27]. Our data support these prior findings with the highest surgical volume centers significantly associated with receipt of LNS, but not resulting in an improved survival. However, lymph node staging remains a key component of surgical staging for endometrial cancer; and allows for tailoring of adjuvant therapies. Adherence to similar treatment guidelines in ovarian cancer has been associated with proximity to care, although similar reports are not available for endometrial cancer [28]. In our analysis, women with high-grade endometrial cancer who traveled farther for their surgical care were more likely to receive LNS (OR 1.12, 95% CI 1.04 to 1.21). Interestingly, 84% of women who traveled >30 miles for care received care at the highest volume centers. Our findings suggest that patients may have traveled farther initially to seek the surgical expertise of higher volume centers, thereby explaining the higher rates of LNS observed among those who traveled farther.
Several limitations to our study are inherent in the use of large clinical and administrative databases. While the Charlson-Deyo score accounts for comorbidities, the NCDB does not record data on body mass index (BMI), which can influence surgical decision making. Additionally, there was inadequate reporting of omentectomy and peritoneal cytology to include in our analysis. Another limitation is interpretation of the number of lymph nodes examined. The NCDB reports the number of lymph nodes examined by a pathologist; however, information distinguishing between pelvic and para-aortic nodal basins is largely incomplete. As sentinel lymph node mapping is being utilized more often in endometrial cancer, the number of lymph nodes needed for adequate surgical staging is likely to decrease while lymph node status becomes even more vital to the management and prognosis of endometrial cancer. In order to broadly examine the surgical staging issue without focusing on nodal counts, we chose to examine lymph node staging as a dichotomous variable.
Conclusions
Lymph node staging for high-grade endometrial cancer, whether comprehensive lymphadenectomy or sentinel lymph node mapping, is not only recommended by the NCCN and the SGO, but can also assist in the tailoring of adjuvant therapies. While medical comorbidities (as captured here in the Charlson-Deyo score) may provide inherent difficulties to completing surgical staging, the receipt of guideline-based care should not be limited. High-volume centers are best equipped to provide guideline-based care to these high-risk women.
Abbreviations
- ACS:
-
American College of surgeons
- AJCC:
-
American joint committee on cancer
- BMI:
-
Body mass index
- CC:
-
Clear cell
- CoC:
-
Commission on cancer
- FIGO:
-
International federation of gynecology and obstetrics
- LNS:
-
Lymph node sampling
- NCCN:
-
National comprehensive cancer network
- NCDB:
-
National cancer data base
- OS:
-
Overall survival
- SGO:
-
Society of gynecologic oncology
- UPSC:
-
Uterine papillary serous carcinoma
References
Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2016. CA Cancer J Clin. 2016;66:7–30.
Alektiar KM, McKee A, Lin O, et al. Is there a difference in outcome between stage I–II endometrial cancer of papillary serous/clear cell and endometrioid FIGO Grade 3 cancer? Int J Radiation Oncology Biol Phys. 2002;54:79–85.
Goff BA, Kato D, Schmidt RA, et al. Uterine papillary serous carcinoma: Patterns of metastatic spread. Gynecol Oncol. 1994;54:264–8.
Abeler VM, Vergote IB, Kjorstad KE, Trope CG. Clear cell carcinoma of the endometrium: Prognosis and metastatic pattern. Cancer. 1996;78:1740–7.
Cirisano FD, Robboy SJ, Dodge RK, et al. The outcome of stage I–II clinically and surgically staged papillary serous and clear cell endometrial cancers when compared with endometrioid carcinoma. Gynecol Oncol. 2000;77:55–65.
Hamilton CA, Cheung MK, Osann K, et al. Uterine papillary serous and clear cell carcinomas predict for poorer survival compared to grade 3 endometrioid corpus cancers. BJOC. 2006;94:642–6.
National Comprehensive Cancer Network. Uterine Neoplasms (Version 2.2015). http://www.nccn.org/professionals/physician_gls/pdf/uterine.pdf. Accessed 6 Sept 2015
Boruta DM, Gehrig PA, Fader AN, Olawaiye AB. Management of women with uterine papillary serous cancer: A Society of Gynecologic Oncology (SGO) review. Gynecol Oncol. 2009;115:142–53.
Olawaiye AB, Boruta DM. Management of women with clear cell endometrial cancer: A Society of Gynecologic Oncology (SGO) review. Gynecol Oncol. 2009;113:277–83.
Madison T, Schottenfield D, James SA, Schwartz AG, Gruber SB. Endometrial cancer: Socioeconomic status and racial/ethnic differences in stage at diagnosis, treatment, and survival. Am J Public Health. 2004;94:2104–11.
Hicks ML, Phillips JL, Parham G, et al. The National Cancer Data Base report on endometrial carcinoma in African-American women. Cancer. 1998;83:2629–37.
Randall TC, Armstrong K. Differences in treatment and outcome between African-American and White women with endometrial cancer. J Clin Oncol. 2003;21:4200–6.
Rauh-Hain JA, Buskwofie A, Clemmer J, Boruta DM, Schorge JO, Del Carmen MG. Racial disparities in treatment of high-grade endometrial cancer in the Medicare population. Obstet Gynecol. 2015;125:843–51.
Benjamin I, Dalton H, Qiu Y, Cayco L, Johnson WG, Balducci J. Endometrial cancer surgery in Arizona: A statewide analysis of access to care. Gynecol Oncol. 2011;121:83–6.
Mohanty S, Bilimoria KY. Comparing national cancer registries: The National Cancer Data Base (NCDB) and the Surveillance, Epidemiology, and End Results (SEER) program. J Surg Oncol. 2014;109:629–30.
Bristow RE, Palis BE, Chi DS, Cliby WA. The National Cancer Database report on advanced-stage epithelial ovarian cancer: Impact of hospital surgical case volume on overall survival and surgical treatment paradigm. Gynecol Oncol. 2010;118:262–7.
Mariani A, Webb MJ, Galli L, Podratz KC. Potential therapeutic role of para-aortic lymphadenectomy in node-positive endometrial cancer. Gynecol Oncol. 2000;76:348–56.
Kilgore LC, Partridge EE, Alvarez RD, et al. Adenocarcinoma of the endometrium: Survival comparisons of patients with and without pelvic node sampling. Gynecol Oncol. 1995;56:29–33.
Havrilesky LJ, Cragun JM, Calingaert B, et al. Resection of lymph node metastases influences survival in Stage IIIC endometrial cancer. Gynecol Oncol. 2005;99:689–95.
Todo Y, Kato H, Kaneuchi M, Watari H, Tokeda M, Sakuragi N. Survival effect of para-aortic lymphadenectomy in endometrial cancer (SEPAL) study: a retrospective cohort analysis. Lancet. 2010;375:1165–72.
Long B, Liu FW, Bristow RE. Disparities in uterine cancer epidemiology, treatment, and survival among African Americans in the United States. Gynecol Oncol. 2013;130:652–9.
Matthews RP, Hutchinson-Colas J, Maiman N, et al. Papillary serous and clear cell type lead to poor prognosis of endometrial carcinoma in Black women. Gynecol Oncol. 1997;65:206–12.
Barrett 2nd RJ, Harlan LC, Wesley MN, et al. Endometrial cancer: stage at diagnosis and associated factors in Black and White patients. Am J Obstet Gynecol. 1995;173:414–23.
Connell PP, Rotmensch J, Waggoner SE, Mundt AJ. Race and clinical outcome in endometrial carcinoma. Obstet Gynecol. 1999;94:713–20.
Wright JD, Hershman DL, Burke WM, et al. Influence of surgical volume on outcome for laparoscopic hysterectomy for endometrial cancer. Ann Surg Oncol. 2012;19:948–58.
Becker JH, Ezendam NPM, Boll D, van der Aa M, Pigenborg JMA. Effects of surgical volumes on the survival of endometrial cancer. Gynecol Oncol. 2015;139:306–11.
Wright JD, Lewin SN, Deutsch I, Burke WM, Sun X, Herzog TJ. Effect of surgical volume on morbidity and mortality of abdominal hysterectomy for endometrial cancer. Obstet Gynecol. 2011;117:1051–9.
Bristow RE, Chang J, Ziogas A, Anton-Culver H, Vieira VM. Spatial analysis of adherence to treatment guidelines for advanced-stage ovarian cancer and the impact of race and socioeconomic status. Gynecol Oncol. 2014;134:60–7.
Acknowledgments
Not applicable.
Funding
No funding.
Availability of data and material
The data that support the findings of this study are available from the National Cancer Data Base, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the National Cancer Data Base.
Authors’ contributions
All authors contributed to the planning (conceptualization and methodology) of this research. JF, LH, and GB conducted the main investigation, while GB provided formal analysis of the data. All authors contributed to the writing and revision of this manuscript. While all authors have agreed to be accountable for this research, JF and LH are both guarantors of the overall content of this research. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Required statement by the national cancer data base
The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society. The data used in the study are derived from a de-identified NCDB file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed, or the conclusions drawn from these data by the investigator.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Foote, J.R., Gaillard, S., Broadwater, G. et al. Disparities in the surgical staging of high-grade endometrial cancer in the United States. gynaecol oncol res pract 4, 1 (2017). https://doi.org/10.1186/s40661-016-0036-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40661-016-0036-3