Abstract
Background
Sepsis, the life-threatening host response to infection, is a major cause of mortality. Obesity increases vulnerability to sepsis; however, some degree of obesity may be protective, called the “obesity paradox”. This scoping review systematically maps the literature on outcomes associated with diet-induced obesity and sepsis-induced organ injury, focusing on non-transgenic murine models.
Methods
A literature search of primary articles was conducted from database inception to June 2023. Eligible articles compared diet-induced obesity to non-obese mice in sepsis models involving live pathogens. Two reviewers screened articles and extracted data on obesogenic and sepsis models utilized, and organ injury outcomes, including physiological dysfunction, histological alterations, and biochemical changes.
Results
Seventeen studies met eligibility criteria; 82% used male C57BL/6 mice, and 88% used cecal ligation and puncture to induce sepsis. Most studies used 60% high-fat diets compared to 10–16% fat in controls. Seven (64%) studies reported increased mortality in obese septic mice, one (9%) observed a decrease, and three (37%) found no significant difference. The liver, lungs, and kidneys were the most studied organs. Alanine transaminase results were inconclusive. Myeloperoxidase levels were increased in the livers of two studies and inconclusive in the lungs of obese septic mice. Creatinine and neutrophil gelatinase-associated lipocalin were elevated in obese septic mice.
Conclusions
There is variability in the methodology and measured outcomes in murine models of diet-induced obesity and sepsis and a lack of studies in female mice. The absence of standardized models has produced conflicting findings on the impact of obesity on sepsis outcomes.
Similar content being viewed by others
Take-home message
This scoping review highlights the varied use of murine models in studying sepsis and obesity's effects on organ injury, leading to inconsistent data and hindering progress. Standardizing mouse models, incorporating both sexes, and agreeing on outcome measures are essential for enhancing comprehension of obesity's influence on sepsis response.
Introduction
Sepsis, the life-threatening response to infection resulting in organ damage and dysfunction, is the leading cause of death worldwide [1, 2]. The substantial healthcare burden is evident, with intensive care unit (ICU) stays costing billions in Canada [3]. Despite advancements in sepsis understanding, treatment remains supportive due to the diverse disease trajectory among patients. Co-existing conditions such as obesity, diabetes, heart disease, renal failure, and alcohol use disorder further complicate sepsis, altering the immune response [4]. Yet, the specific impact of these co-morbidities on sepsis outcomes remains elusive.
Obesity, characterized by a BMI exceeding 30, is a widespread issue globally, disregarding socioeconomic differences [5]. Overweight and obese patients are increasingly represented in critical care, accounting for a significant proportion of ICU admissions [6]. Paradoxically, observational studies suggest that obesity might confer a survival advantage in sepsis, defying conventional health implications [7,8,9,10]. However, pre-clinical research outcomes on obesity's influence in sepsis are inconsistent, hampering effective translation to clinical practice. It imperative to establish relevant models mimicking human scenarios to unravel obesity's intricate role, encompassing its impact on sepsis occurrence, organ dysfunction, and mortality. Such insights hold the key to innovative therapeutic strategies in sepsis management.
Murine models are pivotal for comprehending sepsis–obesity dynamics, driven by their simplicity, reproducibility, and cost-effectiveness in sepsis research [11, 12]. The established "gold-standard" sepsis model is cecal ligation and puncture (CLP), involving cecal puncture and fecal introduction into the peritoneal cavity [13]. Another model, fecal-induced peritonitis (FIP), injects bacterial inoculum from a donor animal's cecal contents into the peritoneal cavity [14]. Murine obesity research employs genetic (monogenic or polygenic) or non-genetic models, such as diet-induced obesity (DIO). While genetic models unravel gene mechanisms, they might lack translational relevance due to rare or non-existent human-equivalent mutations [15]. In contrast, DIO mirrors human dietary imbalances contributing to obesity more faithfully. However, the lack of consensus on optimal pre-clinical model combinations leads to conflicting findings and literature gaps.
This scoping review aims to comprehensively explore the literature on the effects of live pathogens in murine models of diet-induced obesity (DIO) and sepsis, with the objective of systematically assessing and synthesizing available research to elucidate the impact of DIO on sepsis-related organ injury. Additionally, this review intends to evaluate methodological aspects and identify knowledge gaps, thereby contributing to the enhancement of research quality and understanding.
Methods
This scoping review adheres to the PRISMA–ScR guidelines [16] and follows a five-stage process based on the framework by Arksey and O’Malley [17], as well as advancements by Levac et al. [18]. The stages encompassed defining the research question, identifying pertinent studies, selecting studies, data charting, and summarizing and reporting results. The review's protocol is available on Open Science Framework with the identifier https://doi.org/10.17605/OSF.IO/FE7KY.
Stage 1: identifying a research question
-
Primary: In murine models of DIO and pathogen-driven sepsis, what are the reported outcomes on the impact of obesity on sepsis-induced organ injury?
-
Secondary: In murine sepsis models, is there evidence that DIO protects against sepsis-induced organ dysfunction?
Stage 2: identifying relevant studies
Relevant studies were identified by searching PubMed, Medline, EMBASE, Web of Science, and CINAHL from inception to June 2023. Search terms included sepsis, septicemia, bacteremia, murine model, mouse model, obesity, and high-fat diet. The search terms were adapted to each database as needed. Additional file 1 presents a sample search strategy.
Stage 3: study selection
Relevant studies were screened by title and abstract, followed by full-text review using Covidence (Veritas Health Innovation, Melbourne, Australia) [19]. Two reviewers conducted independent screenings, resolving discrepancies through discussion or a third reviewer's input.
A modified SYRCLE tool with 21 sub-items was used, (excluding sub-item 17 due to lack of relevance) (Additional file 2: Table S1). This aimed to evaluate each study's quality, bias, strengths, and limitations in murine sepsis and obesity research. Despite its uncommon use in scoping reviews, risk of bias assessment was conducted to enhance discussions on study quality and inform future research, involving two independent reviewers and resolving disagreements through a third reviewer's consultation.
Stage 4: eligibility
This scoping review included non-transgenic murine models investigating the impact of high-fat and/or diet-induced obesity (DIO) on sepsis outcomes. Eligible sepsis models encompassed bacterial sepsis, polymicrobial sepsis, and cecal ligation and puncture. Included studies explored histological, biochemical, physiological, and immune changes associated with organ injury. Excluded were studies involving humans, rats, other animal models, lipopolysaccharide sepsis models, obesity knock-out models (ob/ob, db/db), and solely in vitro approaches. Publications such as editorials, abstracts, commentaries, letters, systematic reviews, and meta-analyses were excluded, though their reference lists were reviewed for relevant articles.
Stage 5: charting the data
Key information from the included studies was abstracted, independently and in duplicate, using standardized data abstraction forms (Additional file 1: Data extraction file). The following information was extracted:
-
1.
Author(s).
-
2.
Year of publication.
-
3.
Country of publication.
-
4.
Breed, supplier, sex, and age of mice.
-
5.
Organs evaluated.
-
6.
Type of diet (composition, percent of kcal).
-
7.
Method of diet delivery.
-
8.
Length of time on the diet.
-
9.
Body weight and fat mass.
-
10.
The method by which sepsis was induced, site of infection, and dose.
-
11.
Endpoint time.
-
12.
Antibiotics, fluids, and analgesia.
-
13.
Outcomes including glucose and insulin response, mortality, biomarkers of organ dysfunction, myeloperoxidase, and cytokine changes.
The data abstraction form was tested on three studies, and then data extraction was conducted independently and in duplicate by two reviewers, with discrepancies resolved through discussion or third-party arbitration.
Stage 6: collating, summarizing, and reporting the results
The study presented results summarizing the impact of DIO on sepsis outcomes, using tables to organize bibliographic, obesogenic, and sepsis model data. The narrative synthesis highlighted DIO model development, sepsis induction methods, and outcomes, assessing whether DIO offers sepsis protection. Similar outcome studies reported in parallel, and conflicting evidence was compared.
Results
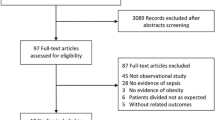
A total of 393 articles were initially identified through the search. After removing duplicates, 348 articles underwent initial screening, resulting in 88 articles based on title and abstract. Following further evaluation, 71 articles were excluded for not meeting inclusion criteria, leading to a final selection of 17 articles that met the criteria (Fig. 1) [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36].
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Flow Chart. A chart representation of the process used to collect relevant literature from a set of databases and criteria. Beginning with the identification process, this chart displays how 393 collected studies were screened to determine which articles should be included in the review. The screening and inclusion process provided a total of 17 studies that met all the desired criteria
Study characteristics
Table 1 summarizes the characteristics of the 17 included studies, originating from eight different countries, predominantly the United States (41%). Most studies (88%) utilized male C57BL/6 background mice, while exceptions included one study (6%) involving male Swiss mice [31], another (6%) with 57BL/6JRj mice [23], and one study (6%) exclusively using female mice [22]. Mice ages ranged from three to 24 weeks, with a notable proportion (53%) initiating diet at 6 weeks [20, 21, 24, 25, 27, 29, 32, 34, 35]. Most studies obtained mice from commercial suppliers, although three (18%) employed in-house bred mice [22, 28, 31], and another three (18%) did not specify the source [29, 33, 36]. The liver was the most frequently evaluated organ (71%), followed by the lungs (29%) and kidney (24%).
Models of sepsis
Table 2 provides an overview of the sepsis induction methods utilized, with 82% of studies employing cecal ligation and puncture (CLP) [20,21,22,23,24,25,26, 28,29,30,31, 33,34,35,36]. The prevalent CLP techniques included double-puncture with a 22G needle (18%) [20, 25, 35] and single puncture using a 23G needle (18%) [30, 33, 36]. A live-bacteria model was used in one (6%) study [32], and another (6%) [27] induced sepsis with fecal slurry. Post-sepsis evaluations were conducted between 6 h and 28 days, with 76% of studies not reporting antibiotic use [21, 22, 24,25,26,27,28,29,30,31,32,33, 36]. However, three (18%) studies [20, 34, 35] administered imipenem, one (6%) in combination with cilastatin [34]. One study (6%) [23] mentioned antibiotic use without specifying type or dosage. Fluid resuscitation was performed in 71% of studies [20, 22,23,24,25,26, 29, 30, 33,34,35,36], commonly using either 0.6 ml or 1 ml of saline (35%) [20, 24, 25, 29, 30, 35]. Conversely, analgesics were not used throughout the sepsis timeline in 65% of studies [20,21,22, 24, 25, 27, 29,30,31,32, 35].
Models of obesity
Table 3 summarizes the obesity models employed in the studies, with 53% using a high-fat diet comprising 60% kilocalories (kcal) of fat [20, 21, 24, 25, 27, 31, 33, 35, 36]. Other studies specified diet composition in terms of percent butterfat [26], gram percent fat [32], g/kg of butterfat [29], kilojoule % of fat [34], w/w [28], or percent lipids not converted to %kcal fat [22]. Control diets ranged from 10 to 16% kcal of fat, and 24% of studies used normal or standard chow [26, 31, 33, 36] as controls. Diet duration varied from 3 days to 27 weeks, with 6 [25, 26, 35] or 12 weeks [23, 30, 34] being common. Mice on high-fat diets typically exhibited increased body weight or fat mass at the study’s end [20, 22, 24,25,26,27,28,29,30, 32,33,34,35,36], although 65% did not report fat mass [21,22,23,24, 26, 28,29,30,31, 35, 36], and 18% did not report body weight or fat mass [21, 23, 31]. While high-fat diets were used across all studies, two (12%) also employed genetic knock-out models for obesity induction [32, 34], with this review focusing exclusively on high-fat diet-induced obesity models.
Key findings
The key outcomes of each study are summarized in Table 4. Six (35%) studies reported glucose intolerance before sepsis induction [22, 25,26,27,28, 34]. Of those studies, five (83%) found that obese mice had significantly higher glucose levels than their non-obese counterparts, while one (17%) reported no difference [22]. There were inconsistent results when reporting the impact of a high-fat diet on sepsis mortality. Eleven out of the 17 (65%) studies [21,22,23,24,25, 27, 28, 30,31,32, 34] reported mortality. Of these studies, seven (64%) reported an increase in mortality in their obese septic mice [21, 22, 24, 25, 30,31,32], one (9%) observed a decrease in mortality [27], and three (27%) studies did not see any difference [23, 28, 34]. Among the investigations that documented elevated mortality in obese septic, four studies (57%) utilized saline for fluid resuscitation; however, none of them reported the administration of antibiotics or analgesics [22, 24, 25, 30]. The study that observed a reduction in mortality did not document the use of fluid resuscitation, antibiotics nor analgesics [27]. Of the three studies that reported no discernible difference in mortality, two studies (66%) disclosed the utilization of fluid resuscitation without specifying the type or volume of fluids [23, 34], while the final publication failed to mention any use of fluid resuscitation [28]. Intriguingly, all three papers that did not identify a disparity in mortality were the only studies to reporting mortality outcomes and analgesic usage [23, 28, 34]. Finally, the use of antibiotics and mortality were only reported in two studies [23, 34] in which both studies observed no difference in mortality. Vankrunkelsven [34] reported the use of imipenem/cilastin and Goossens [23] reported the use of antibiotics without disclosing further information.
Liver impacts were explored in three (18%) studies through histology [22, 26, 30]. Two (67%) indicated greater liver damage in obese septic mice compared to non-obese septic mice [22, 26], but one (33%) found no distinctions [30]. Alanine transaminase (ALT) findings were inconsistent among four (24%) studies [22, 25, 28, 35]. Two (50%) reported no differences between obese and non-obese septic mice, whether in serum [22] or plasma at 18 h [35]. Conversely, one (25%) study showed elevated plasma ALT in obese septic mice compared to non-obese mice post-sepsis and obese non-septic mice at 6 h [25], and another showed increased serum ALT in obese septic mice compared to obese and non-obese mice 24-h post-sepsis [28]. Myeloperoxidase (MPO), a damage surrogate [37], was assessed in three (18%) studies [24, 25, 35]. Two (67%) saw higher liver MPO levels in obese septic mice at 6-h post-sepsis compared to non-obese septic mice [24, 25], and one showed an increase at 18 h [24]. One (33%) found no MPO differences at 18 h [35]. Among three (18%) studies measuring liver IL-6 levels [22, 26, 32], no distinctions were seen between obese and non-obese septic mice at 6 h [26]. Yet, two (67%) showed significant differences between obese septic and non-septic mice, at 6 h [22] and 7 days [26], while one (33%) found no differences among any cohort at 5–7 days [32]. Similarly, two (12%) studies detected no differences in hepatic TNFɑ between septic groups at 6 h [26] or 4–7 days [32]. However, two (12%) studies noted higher levels in obese septic mice compared to obese non-septic mice at 6 h [29] and 7 days [22].
Histological evaluation of lungs occurred in two (12%) studies [24, 30]. One study found no inflammation at 6-h post-sepsis in both obese and non-obese mice, noting interstitial and alveolar edema increase at 24 and 48 h in non-obese septic mice compared to obese septic mice [30]. Conversely, the other study showed higher lung injury scores in obese septic mice at 6 h, with alveolar congestion, hemorrhage, neutrophil infiltration, and aggregation, and hyaline membrane formation [24]. Lung MPO levels were assessed in four studies (24%) [24, 26, 35, 36]. One study showed increased MPO in obese mice at 1-, 6-, and 18-h post-sepsis compared to non-obese mice [24]. Another noted MPO elevation at 12 and 24 h in obese septic mice compared to obese non-septic mice [36], and a third observed MPO increase at 18 h in obese mice compared to non-obese mice post-sepsis and obese non-septic mice [35]. The fourth study found higher MPO in non-obese septic mice than obese septic mice at 6-h post-sepsis after 15- or 27-week diets, with no difference after 6 weeks [26]. No studies reported lung IL-6 or TNFɑ levels.
Biomarkers for kidney damage, including creatinine, neutrophil gelatinase-associated lipocalin (NGAL), and blood urea nitrogen (BUN) were assessed. Creatinine levels were evaluated in three (18%) studies [27, 28, 33]; two saw an increase in obese septic mice compared to non-obese septic controls at 24-h post-sepsis in plasma [27] and serum [28], while the third [33] found an increase in plasma creatinine levels in obese septic mice at 12-, 24-, and 48-h post-sepsis compared to non-obese non-septic mice. NGAL, evaluated in two (12%) studies, increased in the kidney tissue of obese septic mice compared to non-obese septic mice at 24 h [27] and in the plasma of obese septic mice compared to non-obese non-septic mice at 12, 24 and 48 h [33]. Plasma BUN levels were measured in two studies (12%); one found it increased at 12-, 24-, and 48-h post-sepsis in obese septic mice compared to non-obese non-septic mice [33] but decreased in another [34]. One (6%) study also showed increased IL-6 levels in obese septic mice compared to non-obese non-septic mice at 12-, 14- and 48-h post-sepsis [33]. TNFɑ levels in the kidney were not reported in any study.
Risk of bias results
The risk of bias in the studies was assessed using a modified version of the SYRCLE tool, consisting of 21 sub-items as signaling questions (Fig. 2). Responses of "yes" indicated low risk, "no" indicated high risk and "unclear" indicated unclear risk. Across all studies, two sub-items were deemed high risk (9.5%), six were unclear risk (29%), while four (19%) were categorized as low risk. High-risk sub-items included "caregiver blinding" due to visual differentiation between obese and non-obese mice and "presence of study protocol," as no study had a registered protocol. For the "random sequence generation" sub-item, eight studies were marked as low risk as they mentioned animal randomization but lacked a method description. In almost all cases of unclear risk sub-items, it was impossible to evaluate due to insufficient reporting in the methods sections. However, for the “distribution of baseline characteristics” sub-item, two studies [24, 28] were evaluated as unclear risk as baseline weight data was shown graphically but not described explicitly. Sub-items that were considered low risk in all studies pertained to “adequate timing of disease induction,” as outcome assessment methods were the same for both obese and non-obese mice; “missing outcome data,” as this was not assumed unless explicitly stated; “outcome assessor blinding,” as all animals were evaluated for all outcomes; and “inappropriate influence of funders,” as determined by examining funding and disclosure statements. The “matched methods and results” sub-item was low risk in all studies except Gomes et al. [22] which did not report results associated with chemokine ligand 2, despite being mentioned in the methods. The “design-specific risk of bias” sub-item was low risk in all studies except Su et al. [33], as it did not induce sepsis in non-obese mice.
Discussion
Sepsis, a life-threatening condition, is influenced by obesity, but its impact remains inconclusive, possibly showing a survival benefit within a specific weight range [38]. A prior review [39] assessed obesity's effect on murine sepsis survival and organ injury using diverse animal models, complicating the synthesis and interpretation of its translational relevance. This scoping review aimed to clarify outcomes in murine models involving DIO and pathogen-induced sepsis. The primary aim was to identify the reported variables in current sepsis and obesity literature. Within included studies, disparities in observed outcomes, divergent evaluated outcomes, methodological variations, and limitations in sepsis and obesity models were identified. Few studies reported mortality, lacking consensus on whether murine models support or contradict the clinically observed obesity paradox. Inconsistent results extended to parameters, such as histological lung and liver damage evaluations, with reported outcomes varying from organ dysfunction to inflammatory cytokines. Diverse outcome investigation compounded result synthesis difficulties. Methodological disparities, including sepsis induction methods and specific high-fat and control diets, hindered comparisons even among studies evaluating similar outcomes. The sepsis and obesity models suffered limitations: sepsis standard misalignment, improper control diets, unstandardized murine obesity criteria, and lack of consideration of experiment timing and season. These limitations contributed to result variability. Furthermore, the lack of inclusion of both sexes limits generalizability. For these reasons, the secondary objective to determine whether DIO offers protection against sepsis-induced organ dysfunction could not be achieved, due to a lack of consensus on the effects of obesity and sepsis. Given the significant variability in various aspects of pre-clinical models related to sepsis and obesity, summarized in Table 5, this scoping review pinpointed crucial elements that need consensus within the broader field to improve outcome comprehension.
A 2017 global study found higher age-standardized sepsis incidence in females than males [1], but all studies reviewed used only male mice except one, limiting translational value. Differences in myocardial and immune responses between male and female mice emphasize the need for both sexes in sepsis research [40]. Biological sex impacts obesity, with distinct adipose patterns and metabolic traits; in particular, women generally have more subcutaneous adipose tissue (SAT); while men have greater visceral adipose tissue (VAT) [41]. Increased VAT in men has been associated with worse glucose, lipid, and inflammatory outcomes than women [42, 43]. In addition, a high VAT/SAT ratio has been shown to influence sepsis survival negatively [44]. Additional mechanisms that are known to be impacted by both obesity and sepsis in a sex-dependent manner including the impact of nitric oxide on vasomotor tone and function should also be considered. Estrogen has been shown to enhance nitric oxide production, which is impaired by both obesity [45] and sepsis [46]. The nitric oxide pathway is a crucial factor that, to date, has been examined independently. However, the existing literature strongly supports further investigation within a co-morbidity model encompassing both sepsis and obesity. Investigating sex's role in the interplay between sepsis and obesity is crucial due to their sex-dependent variations.
The translational applicability of the studied murine sepsis models was diminished due to a lack of alignment with current clinical standards. The Surviving Sepsis Campaign, a set of international guidelines for sepsis clinical care, recommends antibiotic administration within 1 h for patients with septic shock or suspected sepsis with shock and within 3 h for suspected septic patients without shock [47]. The Minimum Quality Threshold in Pre-Clinical Sepsis Studies (MQTiPSS), recommendations developed by an expert group to improve animal models of sepsis, considers fluid administration essential [48, 49]. In contrast, many evaluated studies did not provide antibiotics or fluid resuscitation throughout the sepsis course. Accounting for the six studies published after MQTiPSS fluid administration guidelines were published in 2019, only four studies reported fluid administration [22, 33, 34, 36], while only one reported the use of antibiotics [34]. Clinical sepsis treatment, based on physiological parameters, differs from immediate administration in murine models [27]. Among the reviewed studies, the timing of antibiotic administration differed, possibly due to a lack of characterization of the difference in temporal kinetics between clinical and murine sepsis, as the condition progresses much faster in mice than in humans [50]. Antibiotic timing variations can impact outcomes, influenced by differences in sepsis progression between mice and humans. Administering antibiotics too early in murine models may hinder proper illness induction, affecting host response. Delayed antibiotic administration post-sepsis induction has shown different mortality rates and pathology outcomes. It has been shown in a cecal slurry model that providing antibiotics at 1- or 6-h post-sepsis induction showed low mortality and did not lead to sepsis-associated pathology while delaying antibiotic administration to either 12- or 16-h post-sepsis induction led to higher mortality [51].
The variability in diets used across studies presents challenges in determining the exclusive impact of a high-fat diet versus ingredient-related effects. Control diets are often vaguely labeled as "normal" or "standard" chow, with differing compositions of refined and unrefined plant ingredients [52]. This leads to variations in dietary fiber, with refined diets lacking soluble fiber that promotes beneficial bacterial growth, potentially leading to disruptions in colonic microbiota and obesogenic effects [53]. One option in DIO studies is to use control diets matched in the types of nutritional ingredients to the high-fat diet [54]. A high-fat and low-fat diet, matched in composition, both showed an increased Fimircutes:Bacteriodetes ratio and reduced diversity in the intestinal microbiota compared to the chow diet, but still maintained differences in body weight and fat mass between diet cohorts [52]. However, caution is needed if a matched control diet uses sugar as a fat-derived calorie source, as this could impact observations. The intricate interplay between the gut microbiota and immune responses adds complexity to studying conditions, such as sepsis and obesity [55], emphasizing the need for careful diet selection.
All but three studies used CLP for sepsis induction. Although this is the current gold standard in murine sepsis studies, this method has issues, such as high inter-operator variability and challenges in standardizing between individual mice [56]. In DIO research, CLP's reliance on cecal contents exacerbates variability. CLP often lacks characterization of cecal matter composition, potentially overlooking confounding effects [57]. Fecal-induced peritonitis (FIP) a newer model, offers better reproducibility without CLP's technical challenges, but lacks a continuous polymicrobial focus as seen in appendicitis/diverticulitis, leading to an intense initial immune response that does not reflect sepsis-associated hemodynamic and metabolic changes [58]. Nonetheless, FIP worsens outcomes dose-dependently, upregulating pro-inflammatory gene expression such as chemokine ligand 2 and interleukin-6 [56]. FIP and CLP display similar physiological, histopathological, and immunological alterations similar to observed clinical sepsis alterations with FIP showing less variation [59]. This review highlights the prevalent focus on abdominal sepsis in pre-clinical models. It is crucial to broaden investigations to include other clinically relevant sepsis models, especially those in the obese population from respiratory and urinary origins [60]. The selection of models that mimic clinical features while ensuring benchmarks for reproducibility is essential for inter-laboratory comparisons.
The characterization of obesity in numerous studies varied significantly, assessed through body weight, body composition, glucose tolerance, and insulin tolerance. Weight measurement alone overlooks body composition differences. For example, a low-carbohydrate, high-fat diet, compared to standard chow, elicited similar weight gain, but showed a decrease in lean mass and organ deterioration [61]. In addition, as observed in our review, glucose tolerance tests (GTTs) differed in glucose administration route and fasting duration, convoluting comparisons. Intraperitoneal (IPGTT) and oral gavage (OGTT) tests show differing insulin levels and glucose release patterns [62]. Obesity in humans is categorized primarily according to body mass index (BMI); however, there are no corresponding criteria for mice [12]. Proposed murine obesity characterization combines weight, composition, inflammation, glucose, liver health, hormones, and lipids [63]. The absence of standardized obesity criteria hinders accurate sepsis–obesity effect investigations.
Seasonal and daily times of sepsis induction can also determine sepsis outcomes, but the time of day in which sepsis was induced was only reported in one study [30]. Among clinical cases of sepsis, winter has been associated with higher incidence and mortality than summer [64]. Even in consistently maintained conditions of animal facilities, mice subjected to CLP have been shown to exhibit season-dependent outcomes [65, 66]. Both male and female C57BL/6 J mice that underwent CLP show circadian rhythm-dependent severity—mortality is higher when sepsis is induced at night compared to the day [67, 68]. Due to this, future studies should evaluate seasonality as an experimental factor in murine models of sepsis and obesity.
This study is subject to several important limitations. Firstly, the exclusion of studies without measures of organ dysfunction restricts the inclusion of mechanistic investigations. Secondly, the generalizability of our findings is limited by focusing solely on murine models. Omitting diverse preclinical models, such as rats and pigs, may constrain translational relevance and study generalizability. Thirdly, the inclusion criterion of English-language studies may have excluded relevant non-English publications. Despite these limitations, the review adheres to standardized PRISMA–ScR guidelines [16], and its inclusion of risk of bias assessments highlights methodological considerations essential for addressing translational challenges in animal models of sepsis. The review effectively underscores methodological inconsistencies and knowledge gaps in murine sepsis–obesity models that require resolution for advancing research. Moreover, the review's identification of reported outcomes in these models offers valuable insights for developing a standardized set of reportable outcomes for future studies advancing comparability to synthesize outcomes.
Conclusion
The absence of co-morbidity representation, particularly obesity, in pre-clinical sepsis studies has impeded their translation into effective treatments, resulting in conflicting data and methodological inconsistencies that hinder consensus and applicability. To address the complexity of sepsis, utilizing various animal models that replicate clinically observed sepsis is crucial. Despite inherent limitations, this review underscores the importance of standardized protocols to synthesize the impact of obesity on sepsis outcomes. Collaborative initiatives such as the National Pre-clinical Sepsis Platform are striving to establish uniform practices and comparability across laboratories [69, 70]. Standardization in murine sepsis–obesity models will enhance insights into pathophysiology and improve pre-clinical therapeutic translation.
Availability of data and materials
Source data for this study are available through the corresponding author.
Change history
05 June 2024
A Correction to this paper has been published: https://doi.org/10.1186/s40635-024-00637-4
References
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, Colombara DV, Ikuta KS, Kissoon N, Finfer S, Fleischmann-Struzek C, Machado FR, Reinhart KK, Rowan K, Seymour CW, Watson RS, West TE, Marinho F, Hay SI, Lozano R, Lopez AD, Angus DC, Murray CJL, Naghavi M (2020) Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. The Lancet 395:200–211. https://doi.org/10.1016/S0140-6736(19)32989-7
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche J-D, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent J-L, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315:801–810. https://doi.org/10.1001/jama.2016.0287
Farrah K, McIntyre L, Doig CJ, Talarico R, Taljaard M, Krahn M, Fergusson D, Forster AJ, Coyle D, Thavorn K (2021) Sepsis-associated mortality, resource use, and healthcare costs: a propensity-matched cohort study. Crit Care Med 49:215–227. https://doi.org/10.1097/CCM.0000000000004777
Esper AM, Moss M, Lewis CA, Nisbet R, Mannino DM, Martin GS (2006) The role of infection and comorbidity: factors that influence disparities in sepsis. Crit Care Med 34:2576–2582. https://doi.org/10.1097/01.CCM.0000239114.50519.0E
Global Burden of Disease Collaborative Network (2020) Global Burden of Disease Study 2019 (GBD 2019) Covariates 1980–2019
Pépin JL, Timsit JF, Tamisier R, Borel JC, Lévy P, Jaber S (2016) Prevention and care of respiratory failure in obese patients. Lancet Respir Med 4:407–418. https://doi.org/10.1016/S2213-2600(16)00054-0
Trivedi V, Bavishi C, Jean R (2015) Impact of obesity on sepsis mortality: a systematic review. J Crit Care 30:518–524. https://doi.org/10.1016/j.jcrc.2014.12.007
Papadimitriou-Olivgeris M, Aretha D, Zotou A, Koutsileou K, Zbouki A, Lefkaditi A, Sklavou C, Marangos M, Fligou F (2016) The role of obesity in sepsis outcome among critically ill patients: a retrospective cohort analysis. Biomed Res Int 2016:5941279. https://doi.org/10.1155/2016/5941279
Prescott HC, Osterholzer JJ, Langa KM, Angus DC, Iwashyna TJ (2016) Late mortality after sepsis: propensity matched cohort study. BMJ 353:i2375. https://doi.org/10.1136/bmj.i2375
Pepper DJ, Demirkale CY, Sun J, Rhee C, Fram D, Eichacker P, Klompas M, Suffredini AF, Kadri SS (2019) Does obesity protect against death in sepsis? A retrospective cohort study of 55,038 adult patients. Crit Care Med 47:643–650. https://doi.org/10.1097/CCM.0000000000003692
Geiger BM, Pothos EN (2019) Chapter 1—translating animal models of obesity and diabetes to the clinic. In: Nomikos GG, Feltner DE (eds) Handbook of behavioral neuroscience. Elsevier, pp 1–16
Martins T, Castro-Ribeiro C, Lemos S, Ferreira T, Nascimento-Gonçalves E, Rosa E, Oliveira PA, Antunes LM (2022) Murine models of obesity. Obesities 2:127–147. https://doi.org/10.3390/obesities2020012
Toscano MG, Ganea D, Gamero AM (2011) Cecal ligation puncture procedure. J Vis Exp. https://doi.org/10.3791/2860
Rudiger A, Jeger V, Arrigo M, Schaer CA, Hildenbrand FF, Arras M, Seifert B, Singer M, Schoedon G, Spahn DR, Bettex D (2018) Heart rate elevations during early sepsis predict death in fluid-resuscitated rats with fecal peritonitis. Intensive Care Med Exp 6:28. https://doi.org/10.1186/s40635-018-0190-5
Kleinendorst L, Abawi O, van der Kamp HJ, Alders M, Meijers-Heijboer HEJ, van Rossum EFC, van den Akker ELT, van Haelst MM (2020) Leptin receptor deficiency: a systematic literature review and prevalence estimation based on population genetics. Eur J Endocrinol 182:47–56. https://doi.org/10.1530/EJE-19-0678
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169:467–473. https://doi.org/10.7326/M18-0850
Arksey H, O’Malley L (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8:19–32. https://doi.org/10.1080/1364557032000119616
Levac D, Colquhoun H, O’Brien KK (2010) Scoping studies: advancing the methodology. Implement Sci 5:69. https://doi.org/10.1186/1748-5908-5-69
Veritas Health Innovation Covidence systematic review software
DeMartini T, Nowell M, James J, Williamson L, Lahni P, Shen H, Kaplan JM (2017) High fat diet-induced obesity increases myocardial injury and alters cardiac STAT3 signaling in mice after polymicrobial sepsis. Biochim Biophys Acta 1863:2654–2660. https://doi.org/10.1016/j.bbadis.2017.06.008
Frydrych LM, Bian G, Fattahi F, Morris SB, O’Rourke RW, Lumeng CN, Kunkel SL, Ward PA, Delano MJ (2019) GM-CSF administration improves defects in innate immunity and sepsis survival in obese diabetic mice. J Immunol 202:931–942. https://doi.org/10.4049/jimmunol.1800713
Gomes SV, Dias BV, Júnior PAM, Pereira RR, De Souza DMS, Breguez GS, de Lima WG, Magalhães de CLB, Cangussú SD, Talvani A, Queiroz KB, Calsavara AJC, Costa DC (2023) High-fat diet increases mortality and intensifies immunometabolic changes in septic mice. J Nutr Biochem 116:109315. https://doi.org/10.1016/j.jnutbio.2023.109315
Goossens C, Weckx R, Derde S, Dufour T, Vander Perre S, Pauwels L, Thiessen SE, Van Veldhoven PP, Van den Berghe G, Langouche L (2019) Adipose tissue protects against sepsis-induced muscle weakness in mice: from lipolysis to ketones. Crit Care 23:236. https://doi.org/10.1186/s13054-019-2506-6
Kaplan JM, Nowell M, Lahni P, O’Connor M, Hake PW, Zingarelli B (2012) Short-term high fat feeding increases organ injury and mortality after polymicrobial sepsis. Obesity (Silver Spring) 20:1995–2002. https://doi.org/10.1038/oby.2012.40
Kaplan JM, Nowell M, Lahni P, Shen H, Shanmukhappa SK, Zingarelli B (2016) Obesity enhances sepsis induced liver inflammation and injury in mice. Obesity (Silver Spring) 24:1480–1488. https://doi.org/10.1002/oby.21504
Khan M, Patrick AL, Fox-Robichaud AE, Translational Biology Group TCCC (2014) Development of a murine model of early sepsis in diet-induced obesity. BioMed Res Int 2014:e719853. https://doi.org/10.1155/2014/719853
Lewis ED, Williams HC, Bruno MEC, Stromberg AJ, Saito H, Johnson LA, Starr ME (2022) Exploring the obesity paradox in a murine model of sepsis: improved survival despite increased organ injury in obese mice. Shock 57:151–159. https://doi.org/10.1097/SHK.0000000000001856
Panpetch W, Sawaswong V, Chanchaem P, Ondee T, Dang CP, Payungporn S, Tumwasorn S, Leelahavanichkul A (2020) Candida administration worsens cecal ligation and puncture-induced sepsis in obese mice through gut dysbiosis enhanced systemic inflammation, impact of pathogen-associated molecules from gut translocation and saturated fatty acid. Front Immunol
Rivera CA, Gaskin L, Singer G, Houghton J, Allman M (2010) Western diet enhances hepatic inflammation in mice exposed to cecal ligation and puncture. BMC Physiol 10:20. https://doi.org/10.1186/1472-6793-10-20
Siegl D, Annecke T, Johnson BL, Schlag C, Martignoni A, Huber N, Conzen P, Caldwell CC, Tschöp J (2014) Obesity-induced hyperleptinemia improves survival and immune response in a murine model of sepsis. Anesthesiology 121:98–114. https://doi.org/10.1097/ALN.0000000000000192
Souza ACP, Souza CM, Amaral CL, Lemes SF, Santucci LF, Milanski M, Torsoni AS, Torsoni MA (2019) Short-term high-fat diet consumption reduces hypothalamic expression of the nicotinic acetylcholine receptor α7 subunit (α7nAChR) and affects the anti-inflammatory response in a mouse model of sepsis. Front Immunol 10:565. https://doi.org/10.3389/fimmu.2019.00565
Strandberg L, Verdrengh M, Enge M, Andersson N, Amu S, Önnheim K, Benrick A, Brisslert M, Bylund J, Bokarewa M, Nilsson S, Jansson J-O (2009) Mice chronically fed high-fat diet have increased mortality and disturbed immune response in sepsis. PLoS ONE 4:e7605. https://doi.org/10.1371/journal.pone.0007605
Su L-H, Lin M-T, Yeh S-L, Yeh C-L (2021) Glutamine administration attenuates kidney inflammation in obese mice complicated with polymicrobial sepsis. Mediators Inflamm 2021:5597118. https://doi.org/10.1155/2021/5597118
Vankrunkelsven W, Derde S, Gunst J, Vander Perre S, Declerck E, Pauwels L, Derese I, Van den Berghe G, Langouche L (2022) Obesity attenuates inflammation, protein catabolism, dyslipidaemia, and muscle weakness during sepsis, independent of leptin. J Cachexia Sarcopenia Muscle 13:418–433. https://doi.org/10.1002/jcsm.12904
Williamson L, Ayalon I, Shen H, Kaplan J (2019) Hepatic STAT3 inhibition amplifies the inflammatory response in obese mice during sepsis. Am J Physiol Endocrinol Metab 316:E286–E292. https://doi.org/10.1152/ajpendo.00341.2018
Yeh C-L, Wu J-M, Su L-H, Yang P-J, Lee P-C, Chen K-Y, Yeh S-L, Lin M-T (2021) Intravenous calcitriol administration regulates the renin–angiotensin system and attenuates acute lung injury in obese mice complicated with polymicrobial sepsis. Biomed Pharmacother 141:111856. https://doi.org/10.1016/j.biopha.2021.111856
Carr AC, Spencer E, Hoskin TS, Rosengrave P, Kettle AJ, Shaw G (2020) Circulating myeloperoxidase is elevated in septic shock and is associated with systemic organ failure and mortality in critically ill patients. Free Rad Biol Med 152:462–468. https://doi.org/10.1016/j.freeradbiomed.2019.11.004
Marques MB, Langouche L (2013) Endocrine, metabolic, and morphologic alterations of adipose tissue during critical illness. Crit Care Med 41:317–325. https://doi.org/10.1097/CCM.0b013e318265f21c
Xu W, Pepper D, Sun J, Welsh J, Cui X, Eichacker PQ (2020) The effects of obesity on outcome in preclinical animal models of infection and sepsis: a systematic review and meta-analysis. J Obes 2020:1508764. https://doi.org/10.1155/2020/1508764
Lakbar I, Einav S, Lalevée N, Martin-Loeches I, Pastene B, Leone M (2023) Interactions between gender and sepsis—implications for the future. Microorganisms 11:746. https://doi.org/10.3390/microorganisms11030746
Schorr M, Dichtel LE, Gerweck AV, Valera RD, Torriani M, Miller KK, Bredella MA (2018) Sex differences in body composition and association with cardiometabolic risk. Biol Sex Differ 9:28. https://doi.org/10.1186/s13293-018-0189-3
Arner P (1995) Differences in lipolysis between human subcutaneous and omental adipose tissues. Ann Med 27:435–438. https://doi.org/10.3109/07853899709002451
McLaughlin T, Lamendola C, Liu A, Abbasi F (2011) Preferential fat deposition in subcutaneous versus visceral depots is associated with insulin sensitivity. J Clin Endocrinol Metab 96:E1756–E1760. https://doi.org/10.1210/jc.2011-0615
Lee JGH, Genga KR, Pisitsak C, Boyd JH, Leung AKK, Russell JA, Walley KR (2018) Survival benefit of a low ratio of visceral to subcutaneous adipose tissue depends on LDL clearance versus production in sepsis. Crit Care 22:58. https://doi.org/10.1186/s13054-018-1985-1
Stepp DW (2006) Impact of obesity and insulin resistance on vasomotor tone: nitric oxide and beyond. Clin Exp Pharmacol Physiol 33:407–414. https://doi.org/10.1111/j.1440-1681.2006.04381.x
Zhang M, Montroy J, Sharma R, Fergusson DA, Mendelson AA, Macala KF, Bourque SL, Schlechte JM, Eng MK, McDonald B, Gill SE, Fiest KM, Liaw PC, Fox-Robichaud A, Lalu MM (2021) The effects of biological sex on sepsis treatments in animal models: a systematic review and a narrative elaboration on sex- and gender-dependent differences in sepsis. Crit Care Explor 3:e0433. https://doi.org/10.1097/CCE.0000000000000433
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, Machado FR, Mcintyre L, Ostermann M, Prescott HC, Schorr C, Simpson S, Wiersinga WJ, Alshamsi F, Angus DC, Arabi Y, Azevedo L, Beale R, Beilman G, Belley-Cote E, Burry L, Cecconi M, Centofanti J, Coz Yataco A, De Waele J, Dellinger RP, Doi K, Du B, Estenssoro E, Ferrer R, Gomersall C, Hodgson C, HylanderMøller M, Iwashyna T, Jacob S, Kleinpell R, Klompas M, Koh Y, Kumar A, Kwizera A, Lobo S, Masur H, McGloughlin S, Mehta S, Mehta Y, Mer M, Nunnally M, Oczkowski S, Osborn T, Papathanassoglou E, Perner A, Puskarich M, Roberts J, Schweickert W, Seckel M, Sevransky J, Sprung CL, Welte T, Zimmerman J, Levy M (2021) Surviving sepsis campaign: international guidelines for management of sepsis and septic Shock 2021. Crit Care Med 49:e1063. https://doi.org/10.1097/CCM.0000000000005337
Osuchowski MF, Ayala A, Bahrami S, Bauer M, Boros M, Cavaillon J-M, Chaudry IH, Coopersmith CM, Deutschman C, Drechsler S, Efron P, Frostell C, Fritsch G, Gozdzik W, Hellman J, Huber-Lang M, Inoue S, Knapp S, Kozlov AV, Libert C, Marshall JC, Moldawer LL, Radermacher P, Redl H, Remick DG, Singer M, Thiemermann C, Wang P, Wiersinga WJ, Xiao X, Zingarelli B (2018) Correction to: Minimum quality threshold in pre-clinical sepsis studies (MQTiPSS): an international expert consensus initiative for improvement of animal modeling in sepsis. Infection 46:745–747. https://doi.org/10.1007/s15010-018-1197-2
Osuchowski MF, Ayala A, Bahrami S, Bauer M, Boros M, Cavaillon J-M, Chaudry IH, Coopersmith CM, Deutschman CS, Drechsler S, Efron P, Frostell C, Fritsch G, Gozdzik W, Hellman J, Huber-Lang M, Inoue S, Knapp S, Kozlov AV, Libert C, Marshall JC, Moldawer LL, Radermacher P, Redl H, Remick DG, Singer M, Thiemermann C, Wang P, Wiersinga WJ, Xiao X, Zingarelli B (2018) Minimum quality threshold in pre-clinical sepsis studies (MQTiPSS): an international expert consensus initiative for improvement of animal modeling in sepsis. Shock 50:377–380. https://doi.org/10.1097/SHK.0000000000001212
Stortz JA, Raymond SL, Mira JC, Moldawer LL, Mohr AM, Efron PA (2017) Murine models of sepsis and trauma: can we bridge the gap? ILAR J 58:90–105. https://doi.org/10.1093/ilar/ilx007
Steele AM, Starr ME, Saito H (2017) Late therapeutic intervention with antibiotics and fluid resuscitation allows for a prolonged disease course with high survival in a severe murine model of sepsis. Shock 47:726–734. https://doi.org/10.1097/SHK.0000000000000799
Dalby MJ, Ross AW, Walker AW, Morgan PJ (2017) Dietary uncoupling of gut microbiota and energy harvesting from obesity and glucose tolerance in mice. Cell Rep 21:1521–1533. https://doi.org/10.1016/j.celrep.2017.10.056
Chassaing B, Miles-Brown J, Pellizzon M, Ulman E, Ricci M, Zhang L, Patterson AD, Vijay-Kumar M, Gewirtz AT (2015) Lack of soluble fiber drives diet-induced adiposity in mice. APSselect 2:G528–G541. https://doi.org/10.1152/ajpgi.00172.2015@apsselect.2015.2.issue-11
Lang P, Hasselwander S, Li H, Xia N (2019) Effects of different diets used in diet-induced obesity models on insulin resistance and vascular dysfunction in C57BL/6 mice. Sci Rep 9:19556. https://doi.org/10.1038/s41598-019-55987-x
Zheng D, Liwinski T, Elinav E (2020) Interaction between microbiota and immunity in health and disease. Cell Res 30:492–506. https://doi.org/10.1038/s41422-020-0332-7
Steinhagen F, Hilbert T, Cramer N, Senzig S, Parcina M, Bode C, Boehm O, Frede S, Klaschik S (2021) Development of a minimal invasive and controllable murine model to study polymicrobial abdominal sepsis. All Life 14:265–276. https://doi.org/10.1080/26895293.2021.1909663
Alverdy JC, Keskey R, Thewissen R (2020) Can the cecal ligation and puncture model be repurposed to better inform therapy in human sepsis? Infect Immun 88:e00942-e1019. https://doi.org/10.1128/IAI.00942-19
Korneev KV (2019) Mouse models of sepsis and septic shock. Mol Biol 53:704–717. https://doi.org/10.1134/S0026893319050108
Tsuchida T, Wada T, Mizugaki A, Oda Y, Kayano K, Yamakawa K, Tanaka S (2022) Protocol for a sepsis model utilizing fecal suspension in mice: fecal suspension intraperitoneal injection model. Front Med 9
Yeo HJ, Kim TH, Jang JH, Jeon K, Oh DK, Park MH, Lim C-M, Kim K, Cho WH, Investigators on behalf of the KSA (KSA) (2023) Obesity paradox and functional outcomes in sepsis: a multicenter prospective study. Crit Care Med 51:742. https://doi.org/10.1097/CCM.0000000000005801
Nilsson J, Ericsson M, Joibari MM, Anderson F, Carlsson L, Nilsson SK, Sjödin A, Burén J (2016) A low-carbohydrate high-fat diet decreases lean mass and impairs cardiac function in pair-fed female C57BL/6J mice. Nutr Metab 13:79. https://doi.org/10.1186/s12986-016-0132-8
Small L, Ehrlich A, Iversen J, Ashcroft SP, Trošt K, Moritz T, Hartmann B, Holst JJ, Treebak JT, Zierath JR, Barrès R (2022) Comparative analysis of oral and intraperitoneal glucose tolerance tests in mice. Mol Metab 57:101440. https://doi.org/10.1016/j.molmet.2022.101440
de Moura e Dias M, dos Reis SA, da Conceição LL, Sediyama de CMNO, Pereira SS, de Oliveira LL, Gouveia Peluziodo MC, Martinez JA, Milagro FI (2021) Diet-induced obesity in animal models: points to consider and influence on metabolic markers. Diabetol Metab Syndr 13:32. https://doi.org/10.1186/s13098-021-00647-2
Danai PA, Sinha S, Moss M, Haber MJ, Martin GS (2007) Seasonal variation in the epidemiology of sepsis. Crit Care Med 35:410–415. https://doi.org/10.1097/01.CCM.0000253405.17038.43
Garcia LF, Singh V, Mireles B, Dwivedi AK, Walker WE (2023) Common variables that influence sepsis mortality in mice. J Inflamm Res 16:1121–1134. https://doi.org/10.2147/JIR.S400115
Kiank C, Koerner P, Keler W, Traeger T, Maier S, Heidecke C-D, Schuett C (2007) Seasonal variations in inflammatory responses to sepsis and stress in mice. Crit Care Med 35:2352–2358. https://doi.org/10.1097/01.CCM.0000282078.80187.7F
Heipertz EL, Harper J, Lopez CA, Fikrig E, Hughes ME, Walker WE (2018) Circadian rhythms influence the severity of sepsis in mice via a TLR2-dependent, leukocyte-intrinsic mechanism. J Immunol 201:193–201. https://doi.org/10.4049/jimmunol.1701677
Silver AC, Arjona A, Walker WE, Fikrig E (2012) The circadian clock controls toll-like receptor 9-mediated innate and adaptive immunity. Immunity 36:251–261. https://doi.org/10.1016/j.immuni.2011.12.017
Mendelson AA, Lansdell C, Fox-Robichaud AE, Liaw P, Arora J, Cailhier J-F, Cepinskas G, Charbonney E, dos Santos C, Dwivedi D, Ellis CG, Fergusson D, Fiest K, Gill SE, Hendrick K, Hunniford VT, Kowalewska PM, Krewulak K, Lehmann C, Macala K, Marshall JC, Mawdsley L, McDonald B, McDonald E, Medeiros SK, Muniz VS, Osuchowski M, Presseau J, Sharma N, Sohrabipour S, Sunohara-Neilson J, Vázquez-Grande G, Veldhuizen RAW, Welsh D, Winston BW, Zarychanski R, Zhang H, Zhou J, Lalu MM (2021) National preclinical sepsis platform: developing a framework for accelerating innovation in Canadian sepsis research. Intensive Care Med Exp 9:14. https://doi.org/10.1186/s40635-020-00366-4
Sharma N, Chwastek D, Dwivedi DJ, Schlechte J, Yu I-L, McDonald B, Arora J, Cani E, Eng M, Engelberts D, Kuhar E, Medeiros SK, Bourque SL, Cepinskas G, Gill SE, Jahandideh F, Macala KF, Panahi S, Pape C, Sontag D, Sunohara-Neilson J, Fergusson DA, Fox-Robichaud AE, Liaw PC, Lalu MM, Mendelson AA, Platform NPS, Canada S (2023) Development and characterization of a fecal-induced peritonitis model of murine sepsis: results from a multi-laboratory study and iterative modification of experimental conditions. Intensive Care Med Exp 11:45. https://doi.org/10.1186/s40635-023-00533-3
Acknowledgements
This study was reviewed by Dr. Manoj Lalu prior to submission. Dr. Lalu, Dr. Asher Mendelson and Dr. Braedon McDonald are the leaders of the National Preclinical Sepsis Platform. The executive of Sepsis Canada includes Dr. Fox-Robichaud, Dr. Osama Loubani (co-Scientific Director), Dr. Saad Salim (Managing Director) and Ms. Kristine Russell (Communications Manager).
Funding
ME and FS were supported by Ontario Graduate Scholarships. KS was supported by the Canadian Graduate Scholarship and the Ontario Graduate Scholarship.
Author information
Authors and Affiliations
Consortia
Contributions
The article was conceived and designed by AFR and ME. Database search was performed by ME and FS. Article screening was conducted by ME, KS, and LN. The paper was written by ME and KS. Tables were produced by ME and figures were produced by ME, LN and KS. Manuscript was edited and revised by AFR, ME, KS, and FS. All authors have approved the final version of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
AFR has received funding from the Canadian Institute of Health Research and is the Scientific Director of Sepsis Canada.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Example search strategy.
Additional file 2: Table S1.
Modified SYRCLE risk of bias signaling questions.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eng, M., Suthaaharan, K., Newton, L. et al. Sepsis and obesity: a scoping review of diet-induced obesity murine models. ICMx 12, 15 (2024). https://doi.org/10.1186/s40635-024-00603-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-024-00603-0