Abstract
Background
Continuous measurement of urinary PO2 (PuO2) is being applied to indirectly monitor renal medullary PO2. However, when applied to critically ill patients with shock, its measurement may be affected by changes in FiO2 and PaO2 and potential associated O2 diffusion between urine and ureteric or bladder tissue. We aimed to investigate PuO2 measurements in septic shock patients with a fiberoptic luminescence optode inserted into the urinary catheter lumen in relation to episodes of FiO2 change. We also evaluated medullary and urinary oxygen tension values in Merino ewes at two different FiO2 levels.
Results
In 10 human patients, there were 32 FiO2 decreases and 31 increases in FiO2. Median pre-decrease FiO2 was 0.36 [0.30, 0.39] and median post-decrease FiO2 was 0.30 [0.23, 0.30], p = 0.006. PaO2 levels decreased from 83 mmHg [77, 94] to 72 [62, 80] mmHg, p = 0.009. However, PuO2 was 23.2 mmHg [20.5, 29.0] before and 24.2 mmHg [20.6, 26.3] after the intervention (p = 0.56). The median pre-increase FiO2 was 0.30 [0.21, 0.30] and median post-increase FiO2 was 0.35 [0.30, 0.40], p = 0.008. PaO2 levels increased from 64 mmHg [58, 72 mmHg] to 71 mmHg [70, 100], p = 0.04. However, PuO2 was 25.0 mmHg [IQR: 20.7, 26.8] before and 24.3 mmHg [IQR: 20.7, 26.3] after the intervention (p = 0.65). A mixed linear regression model showed a weak correlation between the variation in PaO2 and the variation in PuO2 values. In 9 Merino ewes, when comparing oxygen tension levels between FiO2 of 0.21 and 0.40, medullary values did not differ (25.1 ± 13.4 mmHg vs. 27.9 ± 15.4 mmHg, respectively, p = 0.6766) and this was similar to urinary oxygen values (27.1 ± 6.17 mmHg vs. 29.7 ± 4.41 mmHg, respectively, p = 0.3192).
Conclusions
Changes in FiO2 and PaO2 within the context of usual care did not affect PuO2. Our findings were supported by experimental data and suggest that PuO2 can be used as biomarker of medullary oxygenation irrespective of FiO2.
Similar content being viewed by others
Background
Critically ill patients with sepsis develop acute kidney injury (AKI) in 20 to 50% of cases [1]. Despite its clinical importance, available methods for early detection of kidney damage have major limitations. One of the mechanisms implicated in the pathophysiology of this condition is hypoxia of renal tissue, particularly in the renal medulla [2]. Selective hypoxia in the renal medulla was observed in an ovine model of sepsis, despite the presence of global renal hyperemia [3]. In clinical practice, it is not feasible to measure renal medullary tissue oxygen tension in the intensive care unit (ICU). Nevertheless, it is possible to measure oxygen tension of bladder urine (PuO2) by the introduction of a fiber-optic probe in the bladder catheter [4, 5]. A number of experimental investigations have been performed to evaluate this technique and have documented a robust correlation between urinary PO2 and medullary PO2 [6].
One of the caveats for the understanding of relationship between urinary and medullary PO2 is that it may be cofounded by several factors. A concern arising from experimental and computational models is that systemic arterial oxygen tension (PaO2) may affect ureteric and bladder wall oxygenation which, in turn, may influence PuO2 [7,8,9,10]. Experimental observations in anesthetized rabbits suggested that oxygen exchange within the urinary tract is slow and is unlikely to be a major confounder of the relationship between renal medullary tissue PO2 and PuO2 [7]. Nevertheless, the potential for such confounding in human sepsis, where PuO2 measurement might be applied to guide management of risk of AKI and therapeutic interventions, remains unknown. Therefore, to assess whether systemic oxygenation has a potentially confounding impact on urinary oxygenation, we aimed to evaluate PuO2 in critically ill patients with sepsis during the periods before and after changes in fractional inspired oxygen (FiO2) instituted to manage PaO2 within clinically acceptable levels. Also, to support our clinical findings, we investigated the medullary and urinary oxygen tension levels in a sheep experiment within a similar range of FiO2 variation.
Methods
Observational study in septic patients
Study design
We performed a prospective observational cohort study in the ICU of a tertiary care hospital located in Melbourne, Australia, from January 2017 to March 2018. The protocol was approved by the Human Research Ethics Committee of the Austin Hospital (HREC/16/Austin/26). Written informed consent was obtained from all participants or their legal representatives.
Participants
A convenience sample of adult patients (18 years old or older) with suspected or confirmed septic shock was enrolled in the study. We excluded patients who were anuric, on chronic dialysis, pregnant, or who were kidney transplant recipients.
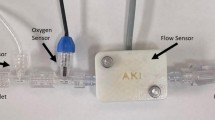
Measurement of PuO 2
For each patient, a fiberoptic luminescence optode (NX-LAS-1/O/E-5 m, Oxford Optronix, Abingdon, UK) was inserted into the lumen of the urinary catheter via a sterile procedure, as described in detail previously [11]. In brief, the sensing tip of the probe was advanced to the distal tip of the catheter so that the probe was placed inside the bladder. The fiberoptic probe was connected to a luminescence lifetime oximeter (Oxylite Pro, Oxford Optronix, UK) interfaced with a laptop computer running LabChart software (Version 8, ADInstruments, Bella Vista, NSW, Australia). PuO2 was recorded every minute from the time of the probe insertion until the removal of the urinary catheter by the treating medical team or at ICU discharge, whichever occurred first.
FiO 2 settings and measurement of PaO 2 and PuO 2
FiO2 was modified at the discretion of bedside clinicians to maintain a peripheral oxygen saturation level greater than 90%. Episodes of FiO2 change were documented in the laptop computer software by the bedside nurse at the moment the intervention took place and were verified against observation charts. To describe arterial oxygen levels, we identified arterial blood gases (ABG) that were collected before and after FiO2 modification (Fig. 1). To make before and after periods distinctive, we restricted the analysis to ABG samples that were obtained within a time difference from FiO2 change of 30 min or more. For each PaO2 measurement, we obtained the mean value of 30 PuO2 measurements centerd around the exact time when the ABG was collected (15 min before and 15 min after the blood was drawn). Blood gas analysis was performed with an ABL800 FLEX blood gas machine (Radiometer, Copenhagen, Denmark). No specific method was used to ascertain the ABG stability for the purposes of the study. However, the unit where the study was conducted is a world-class intensive care with a 1:1 nurse-to-patient ratio. The ABG analyzer is located inside the unit and the team is trained to obtain reliable measurements according to the institutional protocol.
Data extraction
Aside from the abovementioned variables, we collected information on age, gender, baseline creatinine, infection source, comorbidities and ICU severity scores. We also recorded data on duration of mechanical ventilation, number of hours in mandatory and spontaneous modes, mechanical ventilation parameters, end-tidal partial pressure of carbon dioxide (EtCO2), ICU and hospital length of stay, and hospital mortality.
Experimental study using healthy adult sheep
Animal preparation
We obtained data from 9 healthy adult Merino ewes included in an experimental study of sheep undergoing aseptic surgical procedures under general anesthesia [18]. The study was approved by the Animal Ethics Committee of the Florey Institute of Neuroscience and Mental Health under guidelines laid down by the National Health and Medical Research Council of Australia. A similar fiberoptic luminescence optode (Oxford Optronix, Abingdon, UK) used in human patients was inserted into the lumen of the urinary catheter and surgically inserted into the renal medulla. The tissue oxygen tension was continuously recorded at 100 Hz on a computer using a CED micro 1401 interface with Spike 2 software (Cambridge Electronic Design, Cambridge, United Kingdom).
Experimental protocol for the variation of FiO 2
The protocol had 4 components of 20-min duration: a 10-min period to allow oxygen levels to stabilize followed by a 10-min experimental period. Our primary experimental stabilization criteria included renal medullary PO2 and urinary PO2. This timing was determined by assessing the medullary and urinary PO2 values over time. A block randomization was used to set FiO2 at 0.21, 0.40, 0.60 and 1.0. The total gas flow on the mechanical ventilator was maintained at a constant rate of 1.5 L/min, whilst the ratio of the individual oxygen-to-air gas volumes was altered to achieve the target FiO2. For the current analysis, we obtained data from the periods when FiO2 levels were 0.21 and 0.40.
Statistical analyses
Continuous variables are reported as median (quartile 1, quartile 3) and categorical variables are reported as number (%). An aggregate measure was calculated per patient and the paired-sample Wilcoxon test was used to compare median values between the two time periods (before and after FiO2 change). Proportions were compared using Fisher’s exact test. To account for multiple episodes of FiO2 change per patient, we performed a mixed linear regression model to assess the relationship between the variation of PaO2 (ΔPaO2) and the variation of PuO2 (ΔPuO2).
In the sheep experiment, values for each FiO2 setting were calculated and a comparison between groups was performed by using Kruskal–Wallis test.
Statistical analysis was performed using R version 4.0.5. Two-tailed p ≤ 0.05 was considered statistically significant.
Results
Human septic patients
We studied 10 patients, whose clinical characteristics are reported in Table 1. During the study period, patients were mechanically ventilated for 733 h (88.9% of total duration), of which 459 h were in spontaneous mode (55.6%). The mechanical ventilation parameters during the study period are described in Table 2. Arterial blood gases were obtained in 233 occasions. Across the cohort of 10 patients there was a weak but statistically significant positive association between PaO2 and PuO2 (Fig. 2, r2 = 0.022, p = 0.004). This relationship was plotted for each patient (Additional file 1: Fig. S1).
We observed 63 episodes of changes in the FiO2 setting: on 32 occasions FiO2 was decreased and on 31 FiO2 was increased. In the episodes where FiO2 decreased, the median [Q1, Q3] pre-intervention FiO2 was 0.36 [0.30, 0.39] and the median post-intervention FiO2 was 0.30 [0.23, 0.30] (p = 0.006). When FiO2 increased, the median FiO2 before the intervention was 0.30 [0.21, 0.30] and the median FiO2 after the intervention was 0.35 [0.30, 0.40], p = 0.008. There were 14 episodes of successive increase/decrease in the same patient. Such episodes were successive and conditional on the presence of a PaO2 measurement and the time difference between these episodes was 4.29 [2.49, 5.38] hours.
In the episodes when FiO2 was decreased, PaO2 fell from 83 [77, 94] mmHg to 72 [62, 80] mmHg (p = 0.009, Fig. 3). Nevertheless, PuO2 did not vary significantly across the two time points, being 23.2 [20.5, 29.0] mmHg before the intervention and 24.2 [20.6, 26.3] mmHg after the intervention (p = 0.557, Fig. 4). In such episodes, ΔPaO2 was − 14 [− 22.2, − 3.0] mmHg and ΔPuO2 was − 0.02 [− 4.3, 2.9] mmHg.
When FiO2 was increased, PaO2 increased from 64 [58, 72] mmHg to 71 [70, 100] mmHg (p = 0.038, Fig. 3). The corresponding PuO2 measurements were 25.0 [20.7, 26.8] mmHg before the intervention and 24.3 [20.7, 26.3] mmHg after the intervention (p = 0.652, Fig. 4). ΔPaO2 was 8 [− 5.5, 14.0] mmHg and ΔPuO2 was 0.5 [− 2.6, 4.1] mmHg. A mixed linear regression model showed a weak relationship between the change in PaO2 and the change in PuO2 (r2 = 0.003, p = 0.652, Fig. 5) Also, we obtained of an aggregated measure per patient and observed that ΔPuO2 was − 0.532 [− 1.410, 0.331] mmHg and ΔPaO2 was − 3.25 [− 8.880, − 0.125] mmHg, p = 0.1431.
Other laboratory parameters measured before and after FiO2 change were similar between the two time points (Table 3). The urine output before FiO2 change was 63.8 [32.5, 95.0] ml and 70.5 [30.6, 95.0] after FiO2 change, p = 0.9396 (Additional file 2: Fig. S2).
Experimental study
In the sheep experiment, we evaluated urinary and medullary tissue oxygen measurements in four FiO2 levels: 0.21, 0.40, 0.60 and 1.00 (Table 4). For each variable, a total of 36 measurements were obtained. The median PaO2 value at 0.21 FiO2 was 54.5 [51.3, 74.4] mmHg, 209 [181, 223] mmHg at 0.40 FiO2, p < 0.001. When comparing 0.21 and 0.40 FiO2, we found no statistically significant difference in oxygen tension measurements. The medullary oxygen tension was 25.3 [15.3, 30.5] mmHg at 0.21 FiO2 and 28.3 [15.9, 43.4] mmHg at 0.40 FiO2, p = 0.6766; and the urinary oxygen tension was 25.5 [21.6, 32.6] mmHg at 0.21 FiO2 and 30.0 [27.4, 33.6] mmHg at 0.40 FiO2, p = 0.3192.
At higher FiO2 levels, PaO2 values increased (303 [282, 306] mmHg at 0.60 FiO2 and 510 [499, 525] mmHg at 1.00 FiO2. Furthermore, medullary oxygen tension tended to increase at these levels (33.4 [22.6, 45.0] mmHg at 0.60 FiO2 and 40.0 [34.0, 46.8] mmHg at 1.00 FiO2 (p = 0.087) while urinary oxygen tension values significantly increased (59.4 [36.5, 66.0] mmHg at 0.60 FiO2 and 87.9 [66.1, 99.8] mmHg at 1.00 FiO2 (p < 0.001).
For a larger change in FiO2 (from 0.21 to 0.60), medullary oxygen tension values were similar (25.3 [15.3, 30.5] mmHg vs. 33.4 [22.6, 45.0] mmHg, p = 0.2224) but urinary oxygen tension values increased (25.5 [21.6, 32.6] mmHg vs. 59.4 [36.5, 66.0] mmHg, p = 0.001).
Discussion
Key findings
We conducted an observational study in human septic patients to determine whether PuO2 is affected by changes in systemic oxygenation during routine care of patients with septic shock. As expected, changes of FiO2 resulted in significant changes in PaO2. However, we found no significant differences between PuO2 measured before and after the interventions occurred. We supported our clinical findings with data from an experimental sheep experiment showing that medullary and urinary oxygen tension measurements did not differ within a similar range of FiO2 variation.
Relationship to previous studies
To our knowledge, there have been no previous investigations of the relationship between systemic and urinary oxygenation in human patients with septic shock. Ngo et al. addressed this issue in a group of patients undergoing cardiac surgery, finding no significant relationship between PaO2 and PuO2 during cardiopulmonary bypass [6]. Importantly, however, these observations were obtained in a unique physiological state with non-pulsatile flow, an extracorporeal circuit and mild hypothermia. Our current observations are likely more generally applicable to patients in a critical care setting. They are also very consistent with the outcomes of a retrospective analysis of three 3 studies involving a total of 28 adult Merino ewes during experimental sepsis [4, 12, 13], in which only a weak linear relationship was found between PaO2 and PuO2, accounting for ≤ 6% of the variation of PuO2 [6].
The absence of detectable changes in PuO2 in response to modest but clinically significant changes in FiO2 and thus PaO2 indicate that renal medullary tissue PO2 was not markedly affected by these clinical maneuvers. Experimental evidence supports the concept that extreme variations in FiO2 and/or PaO2 lead to corresponding changes in the oxygen tension of renal tissue. For example, in anesthetized rats a reduction in FiO2 from 1.0 to 0.1 resulted in a decline in cortical and medullary microvascular PO2 as assessed by dual-wavelength phosphorimetry [14]. Likewise, studies using fluorescence optodes in anesthetized rabbits demonstrated variations in both cortical and medullary tissue PO2 with variations in FiO2 [7, 15,16,17]. These findings provide support to our experimental findings that greater FiO2 variation is associated with greater PuO2 response, in particular at 0.60 and 1.00 FiO2.
Our ovine study sample derived from a larger experiment comprising 18 healthy sheep undergoing abdominal surgery under total intravenous or volatile anesthesia. In this study, increasing FiO2 from 0.21 to 1.00 increased cortical and medullary tissue PO2 [18]. However, it is also well-established that renal medullary tissue PO2 is less responsive to changes in PaO2 than the renal cortical tissue PO2 [16, 18, 19]. This appears to be a consequence of counter-current diffusive shunting of oxygen between descending and ascending vasa recta, which acts to reduce delivery of oxygen to renal medullary tissue [20]. Consequently, small but physiologically (and clinically) significant changes in FiO2 and/or PaO2 may not appreciably alter renal medullary tissue PO2. In support of this concept, no appreciable difference was observed in medullary tissue PO2 in our group’s preceding experiment when FiO2 was varied from 0.4 to 0.6 [18]. Similarly, in anesthetized rats outer medullary microvascular PO2 did not vary significantly when FiO2 was varied from 0.21 and 0.30 [21]. We cannot directly measure renal medullary tissue PO2 in patients and can only draw indirect inferences from measurement of PuO2 and consideration of available experimental evidence. However, the most parsimonious interpretation of our current findings is that modest changes in FiO2 and thus PaO2 neither markedly alter renal medullary tissue PO2 in patients with sepsis nor confounded the relationship between medullary tissue PO2 and PuO2.
Study implications
Our findings suggest that commonly performed adjustments to FiO2 settings in patients with sepsis do not result in significant changes in PuO2. In consonance of these findings, we observed that variations of FiO2 between 0.21 and 0.40 did not alter either medullary or urinary oxygen tension measurements in a sheep experiment. Thus, variations of systemic oxygenation seem unlikely to confound or affect the utility of urinary oxygenation as a biomarker for risk of AKI. Nevertheless, at higher FiO2 (0.60 and 1.00), significantly increased PuO2 values were obtained. One possible explanation is that in our septic patients, the FiO2 gap was far smaller in comparison to the experimental study. Also, one could argue that a type 2 error was present in the observational study which may have been controlled for during the experimental protocol.
Additional investigation is needed to explore whether the lack of PuO2 variation in face of PaO2 changes derives from the presence of confounding factors affecting medullary oxygen values. Also, further studies in critically ill patients are needed to elucidate whether sustained differences in oxygen exposure [22, 23] influence renal related outcomes. Thus, changes in PaO2, as a consequence of altered FiO2 in routine care of patients with septic shock, is unlikely to be a major confounder of the relationship between renal medullary tissue PO2 and PuO2. In the current study, PaO2 was used as a measure of systemic oxygenation because it reflects the balance between oxygen delivery and consumption. Had SpO2 been used, the accuracy would have been affected by peripheral tissue perfusion, use of vasoactive agents and altered cardiac output. Finally, continuous measurement of PuO2 might be useful for monitoring the impact on renal medullary oxygenation.
Strengths and limitations
We evaluated systemic and urinary oxygenation in human septic patients and assisted our proposition with experimental data. Our findings are consistent with previous observations in sepsis [6] and provide additional evidence that the relationship between renal medullary tissue PO2 and PuO2 is unlikely to be confounded by changes in FiO2 or PaO2 in the range commonly encountered in the ICU. As such, they provide further support for the use of PuO2 as a clinical surrogate of renal medullary PO2.
Our study has several limitations. First, the clinical component was an observation designed to assess the effects on PuO2 where the observed intervention (change of FiO2) was not protocolized. Moreover, controlling for variables such as creatinine or urine output was not feasible due to technical limitations and the limited number of patients. However, we aimed to undertake an exploratory analysis to generate a preliminary hypothesis to guide advanced studies. Moreover, we added data from a sheep experiment where FiO2 variation was protocolized. Also, due to the lower number of measurements in the experimental study, greater heterogeneity was observed. Second, the inclusion of septic patients in our clinical study did not occur in the early stage of resuscitation. On the other hand, the instances of FiO2 change we captured took place in a stable state with lower propensity for PuO2 to be affected by additional confounding effects of interventions intended to optimize oxygen delivery to the tissues. Furthermore, changes in FiO2 performed under stable conditions might have reduced the likelihood of reverse causation or provided mitigation of any potential effect of other interventions. Third, the observational nature of the study may have led to confounding by indication. For instance, the reasons motivating the clinician to change FiO2 settings could have affected the relationship between FiO2 and PuO2. However, a larger degree of FiO2 change would be expected if optimization measures capable of affecting such relationship were in place. Our patients were enrolled in the stabilization phase of sepsis, a time when, in general, only limited interventions are performed to achieve physiologic parameters aiming to prevent organ dysfunction. Finally, we addressed only the variation of systemic oxygenation within the normoxemic range. However, such a normoxemic range is typical in the care of patients in the ICU.
Conclusions
Changes in FiO2 and PaO2 within the context of usual care did not appreciably affect PuO2. Our findings suggest that, within the values reported, PuO2 measured in a clinical and experimental setting is not confounded by changes in inspired oxygen fraction or arterial oxygen tension and that PuO2 can be used as biomarker of medullary oxygenation irrespective of FiO2.
Availability of data and materials
Data are available by contacting the corresponding author.
Abbreviations
- ABG:
-
Arterial blood gas test
- AKI:
-
Acute kidney injury
- EtCO2 :
-
End-tidal partial pressure of carbon dioxide
- FiO2 :
-
Fraction of inspired oxygen.
- ICU:
-
Intensive Care Unit
- PaO2 :
-
Arterial oxygen tension
- PuO2 :
-
Urinary oxygen tension
References
Schrier RW, Wang W (2004) Acute renal failure and sepsis. N Engl J Med 351(2):159–169
Ow CPC, Ngo JP, Ullah MM, Hilliard LM, Evans RG (2018) Renal hypoxia in kidney disease: cause or consequence? Acta Physiol 222(4):e12999
Calzavacca P, Evans RG, Bailey M, Bellomo R, May CN (2015) Cortical and medullary tissue perfusion and oxygenation in experimental septic acute kidney injury. Crit Care Med 43(10):e431-439
Lankadeva YR, Kosaka J, Evans RG, Bellomo R, May CN (2018) Urinary oxygenation as a surrogate measure of medullary oxygenation during angiotensin II therapy in septic acute kidney injury. Crit Care Med 46(1):e41–e48
Zhu MZL, Martin A, Cochrane AD et al (2018) Urinary hypoxia: an intraoperative marker of risk of cardiac surgery-associated acute kidney injury. Nephrol Dial Transplant 33(12):2191–2201
Ngo JP, Lankadeva YR, Zhu MZL et al (2019) Factors that confound the prediction of renal medullary oxygenation and risk of acute kidney injury from measurement of bladder urine oxygen tension. Acta Physiol 227(1):e13294
Sgouralis I, Kett MM, Ow CP et al (2016) Bladder urine oxygen tension for assessing renal medullary oxygenation in rabbits: experimental and modeling studies. Am J Physiol Regul Integr Comp Physiol 311(3):R532-544
Rennie DW, Reeves RB, Pappenheimer JR (1958) Oxygen pressure in urine and its relation to intrarenal blood flow. Am J Physiol 195(1):120–132
Evans RG, Smith JA, Wright C, Gardiner BS, Smith DW, Cochrane AD (2014) Urinary oxygen tension: a clinical window on the health of the renal medulla? Am J Physiol Regul Integr Comp Physiol 306(1):R45-50
Lee CJ, Gardiner BS, Evans RG, Smith DW (2021) Predicting oxygen tension along the ureter. Am J Physiol Renal Physiol 321(4):F527–F547
Osawa EA, Cutuli SL, Bitker L et al (2019) Effect of furosemide on urinary oxygenation in patients with septic shock. Blood Purif 48(4):336–345
Lankadeva YR, Kosaka J, Evans RG, Bailey SR, Bellomo R, May CN (2016) Intrarenal and urinary oxygenation during norepinephrine resuscitation in ovine septic acute kidney injury. Kidney Int 90(1):100–108
Lankadeva YR, Kosaka J, Iguchi N et al (2019) Effects of fluid bolus therapy on renal perfusion, oxygenation, and function in early experimental septic kidney injury. Crit Care Med 47(1):e36–e43
Johannes T, Mik EG, Ince C (2006) Dual-wavelength phosphorimetry for determination of cortical and subcortical microvascular oxygenation in rat kidney. J Appl Physiol 100(4):1301–1310
Leong CL, Anderson WP, O’Connor PM, Evans RG (2007) Evidence that renal arterial-venous oxygen shunting contributes to dynamic regulation of renal oxygenation. Am J Physiol Renal Physiol 292(6):F1726-1733
Evans RG, Goddard D, Eppel GA, O’Connor PM (2011) Factors that render the kidney susceptible to tissue hypoxia in hypoxemia. Am J Physiol Regul Integr Comp Physiol 300(4):R931-940
Cheng HL (2012) Effect of hyperoxia and hypercapnia on tissue oxygen and perfusion response in the normal liver and kidney. PLoS ONE 7(7):e40485
Iguchi N, Kosaka J, Iguchi Y et al (2020) Systemic haemodynamic, renal perfusion and renal oxygenation responses to changes in inspired oxygen fraction during total intravenous or volatile anaesthesia. Br J Anaesth 125(2):192–200
Aperia AC (1969) The influence of arterial PO2 on renal tissue PO2. Acta Physiol Scand 75(3):353–359
Zhang W, Edwards A (2002) Oxygen transport across vasa recta in the renal medulla. Am J Physiol Heart Circ Physiol 283(3):H1042-1055
Chin K, Cazorla-Bak MP, Liu E et al (2021) Renal microvascular oxygen tension during hyperoxia and acute hemodilution assessed by phosphorescence quenching and excitation with blue and red light. Can J Anaesth 68(2):214–225
Suzuki S, Eastwood GM, Glassford NJ et al (2014) Conservative oxygen therapy in mechanically ventilated patients: a pilot before-and-after trial. Crit Care Med 42(6):1414–1422
Investigators ICU-ROX, The Australian New Zealand Intensive Care Society Clinical Trials Group et al (2020) Conservative oxygen therapy during mechanical ventilation in the ICU. N Engl J Med 382(11):989–998
Acknowledgements
We are grateful to Leah Peck, Helen Young and the ICU staff of the Austin Hospital for contributing to the development of this project.
Funding
A financial support for this study was received from Anaesthesia and Intensive Care Trust Fund, Austin Hospital. The funding source was not involved in study design; in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
RB, GME, EAO and SLC: conception or design of the work. EAO, SLC, FY, NI and LB: acquisition, analysis and interpretation of data. EAO, SLC and ATM: drafting of the manuscript. YRL, CNM, RGE, GME and RB: critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol conducted in human patients was approved by the Human Research Ethics Committee of the Austin Hospital (HREC/16/Austin/26) and was performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants or their legal representatives. The protocol conducted in Merino ewes was approved by the Animal Ethics Committee of the Florey Institute of Neuroscience and Mental Health under guidelines laid down by the National Health and Medical Research Council of Australia.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Relationship between PaO2 and PuO2 values in each individual study patient.
Additional file 2.
Box plot illustrating the hourly urinary output before and after a change in FiO2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Osawa, E.A., Cutuli, S.L., Yanase, F. et al. Effects of changes in inspired oxygen fraction on urinary oxygen tension measurements. ICMx 10, 52 (2022). https://doi.org/10.1186/s40635-022-00479-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40635-022-00479-y