Abstract
Purposes
to study the effect of titanium particles on MLO-Y4 and the effects of osteocytes alterations on osteoblasts.
Methods
cultured MLO-Y4 osteocytes were exposed to different concentrations of titanium (Ti) particles, cell viability was measured using the Cell Counting Kit-8 (CCK-8) assay, apoptosis of MLO-Y4 cells was evaluated by flow cytometry, Real-time PCR quantification of mRNA expression of SOST, at the same time with Western Blot detection sclerosteosis protein expression levels.MC3T3-E1 cells culture with MLO-Y4 cells exposed to different concentrations of titanium (Ti) particles in vitro, in order to detection of osteoblast osteogenetic activity.
Results
Our results showed that Ti particles inhibited cell viability of MLO-Y4 osteocytes in a dose-dependent manner. Incubation with Ti particles caused apoptosis of MLO-Y4cells.Treatment with Ti particles significantly increased expression of the osteocytic marker SOST/sclerostin. Furthermore, treatment of MLO-Y4 cells with Ti particles produced a dose-dependent decrease in ALP activity and decreased mineralization of MC3T3-E1 cells through direct cell-cell contact.
Conclusions
Titanium particles damage osteocytes and inhibit osteoblast differentiation.
Similar content being viewed by others
Background
With the rapid increase in the number of joint replacements, the problem of aseptic loosening of the prosthesis is becoming more serious [22]. Periprosthetic osteolysis, in which wear particles induce a biological reaction in histiocytes, is the most important factor in aseptic loosening. Wear particles generated from prosthetic implant materials can activate a wide variety of cell types surrounding the prosthesis, including fibroblasts, monocytes, macrophages, and osteoclasts [7, 15, 33], which release IL-1, IL-6, TNF-α, and other pro-inflammatory cytokines. These pro-inflammatory mediators further stimulate osteoclast differentiation and maturation, leading to bone resorption [2, 18, 34]. Wear debris not only disturbs the proliferation and differentiation of osteoblasts but also stimulate the expression of proinflammatory mediators involved in the interaction between osteoblasts and osteoclasts, such as MMPs and RANKL, suppressing bone formation [10, 12, 28]. Chronic cell activation upsets the delicate balance between bone formation and bone resorption, leading to periprosthetic osteolysis, a form of abnormal bone remodeling. However, the precise etiology of aseptic loosening still remains unclear.
Osteocytes, which are the predominant type of bone cell sand comprise 90%–95% of all bone cells, are terminally differentiated cells that are embedded in the mineralized matrix. They can send signals that regulate bone modeling and remodeling and communicate with other osteocytes via cell processes to convey local signals directly to osteoblasts or osteoclasts [17]. Accumulating evidence [26, 3, 11]has shown that apoptosis of osteocytes promotes osteoclastic remodeling, with increased osteoclast number and activity. Osteocytes can express RANKL in greater quantities than osteoblasts and have a much greater capacity to induce osteoclast formation from precursor cells. Osteocyte activities result in mineralization of osteoids laid down by osteoblasts. In particular, the production of SOST/sclerostin in bone exclusively by osteocytes has gained attention because of its strong association with bone formation and bone mass [4]. Loss of function of SOST, which occursin sclerosteosis, is characterized by high bone mass [36].
The discovery that osteocytes play a key role in regulation of osteoblasts and osteoclasts provided a new way to study the mechanism of periprosthetic osteolysis. Lohmann et al. [24] reported that the addition of UHMWPE(Ultra-High Molecular Weight Polyethylene Particles) to MLO-Y4 osteocytes in culture significantly increased levels of prostaglandin E2 and nitric oxide. Kanaji et al. [20] showed that metal particles also significantly triggered apoptosis of osteocytes, and was partially dependent on TNF-α. Zhang et al. [41]found that tricalciumphosphate wear particles could cause dysfunction in MLO-Y4 osteocytes, mediated by apoptosis and Akt inactivation. However, only a limited number of studies [20, 26] have been performed on the effects of wear debris on osteocytes, and further research is necessary.
In this study, we challenged MLO-Y4 osteocytes with commercial titanium (Ti) particles, and investigated their direct biological effects on osteocytes. Furthermore, we studied the effects of osteocyte alterations on MC3T3-E1 osteoblasts using a co-culture system.
Materials and methods
Ti particle preparation
Commercial pure Ti particles were obtained from Johnson Matthey (catalog #00681; Ward Hill, MA). The average diameter of the Ti particles was 5.34 μm and 90% of the particles were < 10.0 μm in size, according to the manufacturer. Such commercially available particles have been shown to effectively mimic wear particles retrieved from periprosthetic tissue when used in cell culture experiments. The occurrence of osteolysis around the prosthesis is closely related to the composition, number, size, distribution and physical and chemical properties of the wear particles. Willert et al. [39] found that osteolysis has a clear correlation with the number of particles. Only when the number of particles in the boundary membrane tissue exceeds 1 × 10 / g, osteolysis will occur. Yan etal’s [40] research on the extraction and analysis of wear particles in the osteolytic tissue around the prosthesis showed that wear particles with a diameter of less than 10 um can be phagocytosed by phagocytic cells to produce osteolytic media; particles with a diameter of more than 10um cannot be phagocytic cells. Phagocytosis can only be encapsulated by multinuclear foreign body macrophages.
The particles were prepared as previously described [10]. Briefly, the absence of endotoxin was confirmed using a commercial detection kit (QCL-1000; Biowhittaker, Walkersville, MD). The concentration of the endotoxin-free Ti particles was10 mg/mL, and the particles were stored at 4 °C in PBS. For experiments, the particle stock solution was sonicated and diluted with medium to 0.1 mg/mL or 1.0 mg/mL.
Cell culture and treatments
MLO-Y4 osteocytes and MC3T3-E1 subclone 14 osteoblasts were purchased from the Chinese Academy of Sciences Cell Bank (Shanghai, China). MLO-Y4 cells were cultured on collagen-coated dishes (rat tail collagen type I, 0.15 mg/mL, Collaborative Biomedical Products, Bedford, MA) and maintained in modified essential medium (α-MEM) supplemented with 10% fetal bovine serum (FBS, Gibco, Gaithersburg, MD) and 1% penicillin and streptomycin, in a humidified 5% CO2 atmosphere at 37 °C [10]. After 24 h of incubation, the MLO-Y4 cells were treated with Ti particles at concentrations of 0 (control), 0.1 mg/mL, or 1.0 mg/mL; fresh medium was supplied every 3 days. The time at which the Ti particles were added was designated as day 0.
The in vitro model for co-culture of osteocytes and osteoblasts was established using a Millicell-6 Cell Culture Insert Plate (Millipore, Billerica, MA) comprised of a polyethylene terephthalate (PET) membrane perforated with 1-μm pores, as previously described [13]. Basal medium for co-culture experiments was comprised of α-MEM supplemented with 10% FBS, 1% penicillin, and 1% streptomycin. The osteogenic differentiation medium consisted of 10% FBS, 50 μg/mL ascorbic acid, and 10 mM β-glycerophosphate (Sigma-Aldrich, St. Louis, MO).
In the “Cell Contact” co-culture model, inserts were inverted, and the basal side of the membrane (bottom side of insert) was seeded with 5 × 104 MC3T3-E1 osteoblasts in 500 μL of basal medium and incubated for 6 h at 37 °C to permit cellular adhesion. Inserts were then inserted into 6-well tissue culture plates containing 1 mL of basal medium. Then, 1 × 104 MLO-Y4 osteocytes were seeded on the apical side of the membrane (top side of insert) with 1 mL of basal medium and incubated overnight (Fig. 1a). The MLO-Y4 cells on the upper side were treated with Ti particles at concentrations of 0 (control), 0.1 mg/mL, or 1.0 mg/mL, diluted with basal medium. The time at which the Ti particles were added was designated as day 0. The medium was replaced with osteogenic medium after 3 days and was subsequently changed every 3 days.
Schematic diagram showing seeding of the two cell types in the co-culture system. a “Cell Contact” model: MC3T3-E1 osteoblasts were seeded on the basal surface of the membrane andMLO-Y4 osteocytes were then seeded on the apical surface of the membrane. The two cell types were permitted to come into direct contact. b “No Cell Contact” model: MC3T3-E1 osteoblasts were seeded on the bottom of the wells, and MLO-Y4 osteocytes were seeded on the apical surface of the membrane. The two cell types could not come into direct contact
For the “No Cell Contact” model, 5 × 104 MC3T3-E1 osteoblasts were seeded directly on the bottom of the wells instead of on the basal surface of the membrane. MLO-Y4 cells (1 × 104) were subsequently seeded on the apical surface of the membrane with basal medium and incubated overnight (Fig. 1b). All other conditions were as described for the “Cell Contact” model.
Cell viability assay
Cell viability was measured using the Cell Counting Kit-8 (CCK-8) assay (Dojindo Shanghai, China). MLO-Y4 osteocytes were seeded at a density of 3 × 103 cells on 96-well plates, and cultured for 24 h. The cells were treated with 0 (control), 0.1 mg/mL, or 1.0 mg/mL of Ti particles. Cell proliferation was examined at 24 h, 48 h, and 72 h after treatment with Ti particles. Briefly, α-MEM (100 μL) with 10 μL of CCK-8 was added to each pre-cultured well, and then the plates were incubated for 2 h at 37 °C. The absorbance at a wavelength of 450 nm was determined using a TECAN Infinite M200 microplate reader (Tecan Group, Mannedorf, Switzerland).
Detection of cellular apoptosis
MLO-Y4 osteocytes were plated at a density of 5 × 104 cells/well into 6-well plates and treated with Ti particles (0, 0.1 mg/mL, and 1.0 mg/mL) for 24 h and 48 h. Apoptosis of MLO-Y4 cells was evaluated by flow cytometry. The cells were resuspended, and195 μL of the cell suspension was collected and 10μLof Annexin V-FITC (BD Biosciences, San Diego, CA) was added; cells were incubated in the dark at room temperature for 15 min, and 5 μL of propidium iodide (PI) was added. Binding buffer (200 μL) was added to each tube and cells were analyzed using a FACSCalibur flow cytometer (BD Biosciences, San Jose, CA). In each case, 10,000 cells were subjected to flow cytometric analysis.
Real-time PCR quantification of mRNA expression of SOST
MLO-Y4 osteocytes were plated at a density of 5 × 104 cells/well into 6-well plates and treated with Ti particles (0, 0.1 mg/mL,or 1.0 mg/mL) for 24 h or 48 h. Total RNA was extracted from MLO-Y4 cells using Trizol reagent (Invitrogen, Carlsbad, CA). Reverse-transcription was performed to generate first-strand DNA (Thermo) and used as a template for PCR. Then real-time PCR was performed as previously described and SYBR Green I (Roche, Shanghai, China) was used to label the synthesized DNA. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was used as an internal control. The primers sequences were as follows: SOST (Forward, 5′-ATCCCAGGGCTTGGAGAGTA-3′; Reverse, 5′-ACATCTTTGGCGTCATAGGG-3′), and GAPDH (Forward 5′-GTGTGGTCACTATTTGCCTGTC-3′; Reverse5′-AAGCAGTTGGTGGTGCAGGA-3′). The PCR profile began with a temperature of 95 °C for 5 min to activate the DNA polymerase, followed by 55 cycles of 30s at 95 °C and 30s at 57 °C,followed by a melting curve test. The relative amount of mRNA expression normalized to GAPDH was expressed as a fold change, which was calculated by the comparative Ct (2-△△Ct) relative to the control group, using the following formula: 2-△△Ct = 1.
Western-blot analysis for protein expression of sclerostin
MLO-Y4 osteocytes were plated at a density of 5 × 104 cells/well into 6-well plates and treated with Ti particles (0, 0.1 mg/mL, or1.0 mg/mL) for 24 h or 48 h. Cells were washed twice with PBS, treated with lysis buffer, and put on ice for 30 min, then centrifuged at 15,000×g for 30 min. The supernatant was collected and the protein concentration was determined using a BCA protein assay kit (Beyotime, Jiangsu, China). The protein samples were subjected to SDS-PAGE electrophoresis on 10–15% gels, transferred to a nitrocellulose membrane, blocked in 5% fat-free milk for 1 h at room temperature and incubated with primary antibodies (1:400 dilution for sclerostin, CTS) overnight at 4 °C. After washing 4 times with TBST (Tris-buffered saline with Tween), the membranes were incubated with horseradish peroxide (HRP) goat anti-mouse IgG for 30 min at room temperature. Samples were washed with TBST and illuminated with electrochemiluminescence (ECL), and analyzed using a GIS image analysis system.
Alkaline phosphatase activity and staining
Alkaline phosphatase (ALP) activity in the co-culture supernatant (“Cell Contact” and “No Cell Contact”) was measured on day 7 after challenge with Ti particles. In preparation for this assay, medium was collected and centrifuged twice at 4000×g for 10 min to remove cell debris and Ti particles. ALP activity was assayed using an Alkaline Phosphatase Assay Kit (Sigma-Aldrich, St. Louis, MO). In brief, the assay mixtures contained 2-amino-2-methyl-1-propanol, MgCl2, p-nitrophenyl phosphate disodium, and cell homogenates. After incubation, the reaction was stopped with NaOH, and the absorbance was read at 405 nm.
The “Cell Contact” and “No Cell Contact” co-cultures were maintained as described above. Similarly, ALP staining was performed on day 7 after challenge with Ti particles. Osteoblasts were washed three times with PBS prior to staining with an Alkaline Phosphatase Stain Kit (Jiancheng, Jiangsu, China). In brief, cells were fixed in methanol and overlaid with 5-bromo-4-chloro-3-indolyl phosphate plus nitroblue tetrazolium chloride in Tris-HCl, NaOH, and MgCl2, followed by incubation at room temperature for 2 h in the dark.
Mineralized nodule staining and detection of Ca2+ levels
The “Cell Contact” and “No Cell Contact” co-cultures were maintained as described above. Formation of calcified nodules was monitored on day 21 by visualization with alizarin red S (Sigma-Aldrich St. Louis, MO) staining. Briefly, after 3 weeks, osteoblasts were washed with PBS prior to fixation with 70% ethanol, and stained with 1% (w/v) alizarin red solution (pH 4.3) at room temperature. To quantify the amount of alizarin red, the deposition was dissolved in 10% (w/v) cetylpyridinium chloride prepared in double-distilled H2O (ddH2O) and quantified by measuring the OD value at 562 nm.
Statistical analysis
Statistical analyses were performed with SPSS version 17.0. All data are expressed as the mean ± SD, and a minimum of three independent experiments were performed for each assay. One-way analysis of variance (ANOVA) and post-hoc multiple comparisons were used for statistical analysis. A difference was considered significant if p < 0.05.
Results
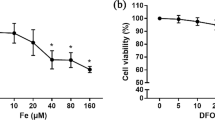
Ti wear particles inhibited cell viability of MLO-Y4 osteocytes in a dose- and time-dependent manner
After MLO-Y4 cells were treated with various concentrations of Ti particles for 24 h, 48 h, and 72 h, cell viability was measured by CCK-8 assay. As shown in Fig. 2, Ti particles significantly inhibited the viability of MLO-Y4 cells, and the inhibition was dose- and time-dependent. In particular, treatment with 1.0 mg/mL of Ti particles for 72 h significantly induced osteocyte death, resulting in cell viability of only 37.21% that of the control. The group treated with 0.1 mg/mL showed a weaker decrease in cell growth than the 1.0 mg/mL group, but both groups differed significantly from the control. Similarly, treatment with Ti particles for 48 h significantly inhibited cell viability, and cell viability was lower at 48 h than at 24 h. These results clearly indicate that Ti particles can reduce cell viability and cause osteocyte death.
Titanium (Ti) wear particles inhibited cell viability of MLO-Y4 cells in a dose- and time-dependent manner. MLO-Y4 cells were treated with various concentrations of Ti particles for 24 h, 48 h, or 72 h, and cell viability was measured by CCK-8 assay. Data are expressed as cell viability of control group (mean ± SD). The viability of cells exposed to 0.1 mg/mL Ti particles was significantly lower than that of the control, and inhibitory effects increased as the Ti particle concentration increased (* p < 0.05). Following treatment with the same concentration of particles, cell viability was lower at 72 h than at 24 h or 48 h
Ti particles caused apoptosis of MLO-Y4 osteocytes
To ascertain the extent of the Ti particle-induced injuries, we measured apoptosis of MLO-Y4 cells by flow cytometry, using an Annexin V-FITC kit. After 24 h or 48 h of incubation, the rate of apoptosis increased rapidly, and was dependent on the Ti particle concentration (Fig. 3). After 24 h, the percentage of apoptotic cells increased to 9.1% (at 0.1 mg/mL) and 34.47% (at 1.0 mg/mL), and the 1.0 mg/mL group differed significantly from the control. In the control group, apoptosis began to decrease after 48 h, whereas the percentages of apoptosis remained high in the 0.1 mg/mL and 1.0 mg/mL groups and differed significantly from the control. These results suggested that Ti particles can cause apoptosis of MLO-Y4 osteocytes in a dose-dependent manner.
Flow cytometric analysis of Ti particle-induced apoptosis in MLO-Y4 osteocytes by Annexin V/PI staining. Cells were treated with Ti particles (0 (control), 0.1 mg/mL, and 1.0 mg/mL) for 24 h (a) and 48 h (b), and stained with FITC-conjugated Annexin V. Apoptosis of cells was quantified by flow cytometry. Q4 represents apoptotic cells. c Data from (a) and (b) are as a percentage of apoptotic MLO-Y4 cells (mean ± SD). At 24 h, apoptosis rates of the cells exposed to 1.0 mg/mL Ti particles were higher than those of the control group and the 0.1 mg/mL group (* p < 0.05). At 48 h, rates of apoptosis were higher in cells exposed to 0.1 mg/mL or 1.0 mg/mL Ti particles than in the control group (* p < 0.05)
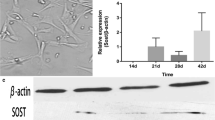
Ti particles increased SOST/sclerostin expression
We further examined expression of the osteocytic marker, SOST/sclerostin. Our real-time PCR data showed that Ti particles at 1.0 mg/mL at 24 h, and 0.1 mg/mL and 1.0 mg/mL at 48 h significantly increased SOST mRNA expression compared with the control. However, in the group treated with 0.1 mg/mL Ti particles, mRNA expression of SOSTdid not differ significantly from the control at 24 h (Fig. 4). To verify the expression of SOST mRNA, we further analyzed the protein expression of sclerostin. Protein expression was generally consistent with mRNA expression, and Ti particles at 1.0 mg/mL at 24 h, 0.1 mg/mL and 1.0 mg/mL at 48 h resulted in a clear increase in sclerostin protein levels (Fig. 5).
mRNA expression of SOST in MLO-Y4 cells treated with Ti particles (0 (control), 0.1 mg/mL and 1.0 mg/mL) for 24 h and 48 h. Real-time PCR was performed, and GAPDH was used as an endogenous control. Results are expressed as the fold change relative to the control group. a At 24 h, treatment with 1.0 mg/mL of Ti particles significantly increased SOST mRNA expression compared with the control group (*p < 0.05). b At 48 h, treatment with 0.1 mg/mL or 1.0 mg/mL of Ti particles significantly increased SOST mRNA expression compared with the control group (*p < 0.05). The group treated with 1.0 mg/mL of Ti particles also differed significantly from the group treated with 0.1 mg/mL (*p < 0.05)
Sclerostin protein expression of MLO-Y4 cells treated with Ti particles (0 (control), 0.1 mg/mL, or 1.0 mg/mL) for 24 h and 48 h. Levels of sclerostin protein were detected by Western blot, and GAPDH was used as an endogenous control. b The quantitative datafor sclerostin levels is expressed as band-density ratios compared to the control group at 24 h. Sclerostin expression was significantly higher in the 1.0 mg/mL group than the control group or the 0.1 mg/mL group (*p < 0.05). c The quantitative data for sclerostin levels is expressed as band-density ratios compared to the control group at 48 h. Treatment with 0.1 mg/mL or 1.0 mg/mL of Ti particlessignificantly increased sclerostin expression compared with the control group (*p < 0.05)
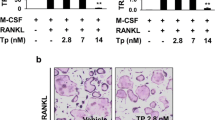
Ti-treated MLO-Y4 cells decreased the ALP activity of MC3T3-E1 cells through direct cell-cell contact
To ascertain the effects of Ti-treated MLO-Y4 cells on MC3T3-E1 osteoblasts, ALP activity and staining were performed on day 7. The MLO-Y4 cells in the “Cell Contact” and “No Cell Contact” co-culture models were simultaneously challenged with different concentrations of Ti particles. The ALP activity of MC3T3-E1 cells in the “Cell Contact” model significantly decreased as the concentration of Ti particles increased (p < 0.05). However, ALP activity in the “No Cell Contact” group did not differ significantly from the control. Similarly, ALP staining of the “Cell Contact” model showed fewer positive cells (cytosol red coloration) in the 0.1 mg/mL and 1.0 mg/mL groups compared with the control. In the “No Cell Contact” model, no changesin ALP staining were observed in groups treated with Ti particles compared with the control (Fig. 6).
Effects of Ti particle-induced changes in MLO-Y4 cells on ALP activity and staining of MC3T3-E1 cells in two co-culture models on day 7. Data showing ALP activity are expressed as mean ± S.D. a In the “Cell Contact” model, ALP activity of MC3T3-E1 cells significantly decreased as the concentration of Ti particles increased (*p < 0.05, **p < 0.01). b In the “No Cell Contact” model, the ALP activity of MC3T3-E1 cells treated with 0.1 mg/mL and 1.0 mg/mL Ti particles did not differ significantly from the control. c ALP staining in the “Cell Contact” model showed fewer positive cells (cytosol red coloration) in the 0.1 mg/mL and 1.0 mg/mL groups compared with the control. In the “No Cell Contact” model, no significant differences in ALP staining were observed in any group
Ti-treated MLO-Y4 cells inhibited mineralization of MC3T3-E1 cells through direct cell-cell contact
To further examine the effects of Ti-treated MLO-Y4 osteocytes on the mineralization of MC3T3-E1 cells, mineralized nodule staining and colorimetrical quantitative analysis of alizarin red, which detects Ca2+ levels, were performed on day 21. The “Cell Contact” and “No Cell Contact” co-cultures were maintained as previously described. The number of mineralized nodules observed in MC3T3-E1 cells in the “Cell Contact” group decreased significantly as the concentration of Ti particles increased (p < 0.05). However, the number of mineralized nodules in the “No Cell Contact” groups did not differ significantly from the control. Similarly, Ca2+ levels in the “Cell Contact” groups treated with 0.1 mg/mL or 1.0 mg/mL differed significantly from the control (*p ≤ 0.05). Accordingly, Ca2+ levels in the “No Cell Contact” groups treated with Ti particles did not differ significantly from the control (Fig. 7).
Effects of Ti particle-induced changes in MLO-Y4 cells on mineralization of MC3T3-E1 cells in two co-culture models on day 21. a MC3T3-E1 cells were stained with alizarin red S. In the “Cell Contact” model, the number of mineralized nodulessignificantly decreased as the concentration of Ti particles increased. The number of mineralized nodules in the “No Cell Contact” model did not differ significantly from the control. b In the “Cell Contact” model, quantitative results of alizarin red differed significantly between the 0.1 mg/mL and 1.0 mg/mL groups and the control (*p < 0.05). In the “No Cell Contact” model, no significant differences in Ca2+ levels were observed in any group
Discussion
The friction of each part of the artificial joint or the friction between the bone cement and the bone interface can produce wear particles. The wear particles are mainly divided into: ultrahigh modulus polyethylene (UHMPE), bone cement particles (polymethylmethacrylate, PMMA), metal particles (Such as titanium alloy particles and chrome-molybdenum alloy particles), ceramic particles,etc. When debris enters the joint space, three-body friction can occur on the joint surface of the prosthesis, and particles can also be generated when the prosthesis collides with each other.The occurrence of osteolysis around the prosthesis is closely related to the composition, number, size, distribution and physical and chemical properties of the wear particles [39, 40].Our present study demonstrated that Ti wear particles injure MLO-Y4 osteocytes in vitro. To confirm the effects of Ti particles on osteocytes, we used a co-culture system to study the effects of osteocytes injured by wear particles on osteoblasts. Theinjured osteocytes suppressed differentiation and mineralization of MC3T3-E1cells through direct cell–cell contact. Our evidence suggests thatosteocytes may play a role in implant loosening, since osteocytes on the bone surface are in direct contact with implants via the canalicular system [6].
To understand the mechanism of aseptic loosening, many studies have investigated expression of pro-inflammatory cytokines induced in response to wear particles [16, 19] and the biological effects of peri-implant cells such as macrophages, osteoblasts, and osteoclasts [23, 29, 34]. However, little attention has been paid to osteocytes compared with the cell types mentioned above. Accumulating evidence indicates that osteocytes play an important role in controlling bone formation and bone resorption. Osteocytes regulate bone formation, including mineral deposition through the BMP [8] and Wnt signaling pathways [5]. Osteocytes also regulate bone resorption by expressing greater quantities of RANKL than osteoblasts, to induce osteoclast formation from precursor cells [26]. Osteocyte death is associated with increased RANKL expression and increased osteoclast formation [21]. Thus, we investigated the interaction between wear debris and MLO-Y4 osteocytes in vitro.
MLO-Y4 cells were challenged with different concentrations of Ti particles. The viability of MLO-Y4 cells, measured by CCK-8 assay, was strongly suppressed in a dose- and time-dependent manner. Apoptosis of MLO-Y4 cells increased in a dose-dependent manner. Some evidence has shown that apoptosis of osteocytes can contribute to the modulation of bone resorption and initiate signaling to recruit osteoclasts [1, 9, 11]. Our data provide some evidence thatwear debris induce apoptosis of osteocytes, perhaps in association with the process of osteoclast activation and bone resorption.
To further examine the effects of Ti particles on MLO-Y4 cells, we examined the expression of an osteocytic marker at the gene and protein levels. Sclerostin, the product of SOST, is produced almost exclusively by osteocytes in bone [31]. In our study, 0.1 mg/mL and 1.0 mg/mL of Ti particles clearly increased mRNA expression of SOSTat 48 h. Analysis of sclerostin protein expression supported the results of gene expression analysis. SOST/sclerostin is strongly associated with bone formation and bone mass via inhibition of canonical Wnt signaling. Sutherland et al. found that sclerostin-mediated control of osteoblastic cells is partially dependent on BMPs [35]. However, sclerostin has also been identified as a catabolic agent in bone. Wijenayaka et al. [38] showed that sclerostin promotes osteoclast formation and osteocyte activity, in a RANKL-dependent manner. Padhi et al. [30] reported that addition of a sclerostin-neutralizing antibody (AMG 785) resulted in a rapid and significant reduction of the serum resorption marker, serum C-telopeptide of collagen (sCTx).
Overall, Ti particles significantly suppressed cell viability, triggered apoptosis, and increased SOST/sclerostin expression of osteocytes, consistent with previous studies [3, 20, 41], which suggested that osteocytes may participate in periprosthetic osteolysis induced in response to wear particles. The differences between our and other studies might be due to differences in the type, shape, or size of wear particles used.
To further examine the effects of osteocyte injuries, we co-cultured MC3T3-E1 osteoblasts with osteocytes injured by wear particles. In “Cell Contact” co-cultures, osteoblasts and osteocytes were seeded on opposing sides of a porous membrane, allowing cell contact, and therefore permitting communication via dendritic processes extending through the pores. However, cellular migration through the pores was not possible. In the “No Cell Contact” model, MC3T3-E1 cells were seeded on the bottom of the wells instead of on the basal surface of the membrane, and the two cell types could therefore communicate through the media only.
It was widely accepted that ALP is an early phenotypic marker of osteoblast differentiation [14, 37]. Formation of mineralized nodules is the ultimate expression of the osteogenic phenotype in vitro and a characteristic marker of mineralization [25]. It should be noted that the colors of ALP and alizarin red S staining in the “Cell Contact” model differed from those in the “No Cell Contact” model: in the different ways of cell seeding. We also examined ALP activity and Ca2+ levels, to ensure accuracy of the experimental results. In the “Cell Contact” model, 0.1 mg/mL and 1.0 mg/mL of Ti particles decreased ALP activity. The number of alizarin red S-positive mineralized nodules significantly decreased as the concentration of Ti particles increased. Similarly, Ca2+ levels were decreased compared with the control. However, in the “No Cell Contact” model, no changes in ALP activity or mineralization of MC3T3-E1osteoblasts were observed in any group. Hence, we concluded that Ti particle-induced osteocyte injuries could cause osteoblast dysfunction through direct cell–cell contact. The mechanism of communication between osteocytes and osteoblasts remains unclear, but may involve gap junction proteins. Nishikawa et al. found that MLO-Y4 cells upregulate terminal differentiation of MC3T3-E1 cells via gap junctions [27]. Gja1 hemichannels have been identified as an important mediator of cellular communication in bone through direct cell–cell contact [32]. In this study, we also assayed TNF-α and IL-1 in the media of the “No Cell Contact” co-culture system using ELISA. Levels of TNF-α increased slightly in the 1.0 mg/mL group compared with the control (data not shown). However, the increase in TNF-α didnot alter ALP activity or mineralization of MC3T3-E1 cells. The evidence presented here does not indicate that osteocytes injured by Ti particles can indirectly affect osteoblasts.
Conclusions
Through in vitro tests we found that Titanium particles can inhibit the proliferation of MLO-Y4 cells and promote their apoptosis and this effect has a significant time-dose dependence; When MLO-Y4 cells were co-cultured with different concentrations of titanium particles at different time points, the expression of genes and proteins (SOST\sclerosteosis) in the intervention group of titanium particles was significantly higher than that of the control group, indicating that osteocytes participated in the process of osteolysis; further research found that when titanium particles intervene with osteocytes and co-culture with osteoblasts, the osteoblasts activity in contact co-culture decreases more significantly, indicating that osteocytes are mainly involved in osteolysis through gap junctions.
Strengths and limitations
This is the first report to show that osteocytes injured by wear particles can inhibit differentiation of osteoblasts through direct cell–cell contact, using a cell co-culture model. These results provide insight into a potential role of osteocytes in prosthetic aseptic loosening.
We are aware of the limitations of in vitro studies; general conclusions cannot be drawn from experiments performed in cell lines alone. Further studies should be undertaken to clarify the mechanism underlying the effects of wear particle-injured osteocytes on osteoblasts.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Change history
03 November 2020
An amendment to this paper has been published and can be accessed via the original article.
References
Al-Dujaili SA, Lau E, Al-Dujaili H, Tsang K, Guenther A, You L (2011) Apoptotic osteocytes regulate osteoclast precursor recruitment and differentiation in vitro. J Cell Biochem 112(9):2412–2423
AlSaffar N, Revell PA (1994) Interleukin-1 production by activated macrophages surrounding loosened orthopaedic implants: a potential role in osteolysis. Br J Rheumatol 33(4):309–316
Atkins GJ, Findlay DM (2012) Osteocyte regulation of bone mineral: a little give and take. Osteoporos Int 23(8):2067–2079
Baron R, Rawadi G, Roman-Roman S (2006) Wnt signaling: a key regulator of bone mass. Curr Top Dev Biol 76:103–127
Bonewald LF (2011) The amazing osteocyte. J Bone Miner Res 26(2):229–238
Bonewald LF, Johnson ML (2008) Osteocytes, mechanosensing and Wnt signaling. Bone. 42(4):606–615
Brooks RA, Sharpe JR, Wimhurst JA, Myer BJ, Dawes EN, Rushton N (2000) The effects of the concentration of high-density polyethylene particles on the bone-implant interface. J Bone Joint Surg Br 82(4):595–600
Canalis E, Economides AN, Gazzerro E (2003) Bone morphogenetic proteins, their antagonists, and the skeleton. Endocr Rev 24(2):218–235
Cardoso L, Herman BC, Verborgt O, Laudier D, Majeska RJ, Schaffler MB (2009) Osteocyte apoptosis controls activation of intracortical resorption in response to bone fatigue. J Bone Miner Res 24(4):597–605
Chen M, Chen PM, Dong QR, Huang Q, She C, Xu W (2014) p38 signaling in titanium particle-induced MMP-2 secretion and activation in differentiating MC3T3-E1 cells. J Biomed Mater Res A 102(8):2824–2832
Cheung WY, Simmons CA, You L (2012) Osteocyte apoptosis regulates osteoclast precursor adhesion via osteocytic IL-6 secretion and endothelial ICAM-1 expression. Bone. 50(1):104–110
Chiu R, Ma T, Smith RL, Goodman SB (2009) Ultrahigh molecular weight polyethylene wear debris inhibits osteoprogenitor proliferation and differentiation in vitro. J Biomed Mater Res 89(1):242–247
Fujita K, Xing Q, Khosla S, Monroe DG (2014) Mutual enhancement of differentiation of osteoblasts and osteocytes occurs through direct cell-cell contact. J Cell Biochem 115(11):2039–2044
Fukayama S, Tashjian AH Jr (1994) Involvement of alkaline phosphatase in the modulation of receptor signaling in osteoblast: Evidence for a difference between human parathyroid hormone-related protein and human parathyroid hormone. J Cell Physiol 158(3):391–397
Grandjean-Laquerriere A, Laquerriere P, Guenounou M, Laurent-Maquin D, Phillips TM (2005) Importance of the surface area ratio on cytokines production by human monocytes in vitro induced by various hydroxyapatite particles. Biomaterials. 26(15):2361–2369
Greenfield EM, Bechtold J (2008) What other biologic and mechanical factors might contribute to osteolysis? J Am Acad Orthop Surg 16(Suppl 1):S56–S62
Henriksen K, Neutzsky-Wulff AV, Bonewald LF, Karsdal MA (2009) Local communication on and within bone controls bone remodeling. Bone 44(6):102610–102633
Holding CA, Findlay DM, Stamenkov R, Neale SD, Lucas H, Dharmapatni AS(2006), et al. The correlation of RANK, RANKL and TNFalpha expression with bone loss volume and polyethylene wear debris around hip implants. Biomaterials 27(30): 5212–5219
Holt G, Murnaghan C, Reilly J, Meek RM (2007) The biology of aseptic osteolysis. Clin Orthop Relat Res 460:240–252
Kanaji A, Caicedo MS, Virdi AS, Sumner DR, Hallab NJ, Sena K (2009) Co-Cr-Mo alloy particles induce tumor necrosis factor alpha production in MLO-Y4 osteocytes: a role for osteocytes in particle-induced inflammation. Bone. 45(3):528–533
Kurata K, Heino TJ, Higaki H, Vaananen HK (2006) Bone marrow cell differentiation induced by mechanically damaged osteocytes in 3D gel-embedded culture. J Bone Miner Res 21(4):616–625
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89(4):780–785
Lange T, Schilling AF, Peters F, Haag F, Morlock MM, Rueger JM, Amling M (2009) Proinflammatory and osteoclastogenic effects of betatricalciumphosphateand hydroxyapatite particles on human mononuclear cellsin vitro. Biomaterials 30(29):5312–5318
Lohmann CH, Dean DD, Bonewald LF, Schwartz Z, Boyan BD (2002) Nitric oxide and prostaglandin E2 production in response to ultra-high molecular weight polyethylene particles depends on osteoblast maturation state. J Bone Joint Surg Am 84(3):411–419
Luppen CA, Leclerc N, Noh T, Barski A, Khokhar A, Boskey AL, Smith E, Frenkel B (2003) Brief bone morphogenetic protein 2 treatment of glucocorticoid-inhibited MC3T3-E1 osteoblasts rescues commitmentassociated cell cycle and mineralization without alteration of Runx2. J Biol Chem 278(45):44995–45003
Nakashima T, Hayashi M, Fukunaga T, Kurata K, Oh-Hora M, Feng JQ, Bonewald LF, Kodama T, Wutz A, Wagner EF, Penninger JM, Takayanagi H (2011) Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med 17(10):1231–1234
Nishikawa Y, Akiyama Y, Yamamoto K, Kobayashi M, Watanabe E, Watanabe N, Shimizu N, Mikami Y, Komiyama K (2015) Osteocytes up-regulate the terminal differentiation of pre-osteoblasts via gap junctions. Biochem Biophys Res Commun 456(1):1–6
Noordin S, Masri B (2012) Periprosthetic osteolysis: genetics, mechanisms and potential therapeutic interventions. Can J Surg 55(6):408–417
Ota K, Quint P, Ruan M, Pederson L, Westendorf JJ, Khosla S, Oursler MJ (2013) Sclerostin is expressed in osteoclasts from aged mice and reduces osteoclast-mediated stimulation of mineralization. Cell Biochem 114(8):1901–1907
Padhi D, Jang G, Stouch B, Fang L, Posvar E (2011) Single-dose, placebo-controlled, randomized study of AMG 785, a sclerostin monoclonal antibody. J Bone Miner Res 26(1):19–26
Poole KE, van Bezooijen RL, Loveridge N, Hamersma H, Papapoulos SE, Lowik CW, Reeve J (2005) Sclerostin is adelayed secreted product of osteocytes that inhibits boneformation. FASEB J 19(13):1842–1844
Ren J, Wang XH, Wang GC, Wu JH (2013) 17beta estradiol regulation of connexin 43-based gap junction and mechanosensitivity through classical estrogen receptor pathway in osteocyte-like MLO-Y4 cells. Bone 53:587–596
Sabokbar A, Pandey R, Quinn JM, Athanasou NA (1998) Osteoclastic differentiation by mononuclear phagocytes containing biomaterial particles. Arch Orthop Trauma Surg 117(3):136–140
Shimizu S, Okuda N, Kato N, Rittling SR, Okawa A, Shinomiya K, Muneta T, Denhardt DT, Noda M, Tsuji K, Asou Y (2010) Osteopontin deficiency impairs wear debris-induced osteolysis via regulation of cytokine secretion from murine macrophages. Arthritis Rheum 62(5):1329–1337
Sutherland MK, Geoghegan JC, Yu C, Turcott E, Skonier JE, Winkler DG, Latham JA (2004) Sclerostin promotes the apoptosis of human osteoblastic cells: a novel regulation of bone formation. Bone. 35(4):828–835
Ten Dijke P, Krause C, de Gorter DJ, Lowik CW, van Bezooijen RL (2008) Osteocyte-derived sclerostin inhibits bone formation: its role in bone morphogenetic protein and Wnt signaling. J Bone Joint Surg Am 90(Suppl 1):31–35
Torii Y, Hitomi K, Yamagishi Y, Tsukagoshi N (1996) Demonstration of alkaline phosphatase participation in the mineralization of osteoblasts by antisense RNA approach. Cell Biol Int 20(7):459–464
Wijenayaka AR, Kogawa M, Lim HP, Bonewald LF, Findlay DM, Atkins GJ (2011) Sclerostin stimulates osteocyte support of osteoclast activity by a RANKL-dependent pathway. PLoS One 6(10):e25900
Willert HG, Buchhorn GH, Hess T (1989) The significance of wear and material fatigue in loosening of hip prostheses. Orthopade 18(5):350–369
Yan MN, Dai KR, Jia QW et al (2005) The abstraction and analysis of wear particles in osteolysis tissue surrounding the prosthesis. J Clinical Orthopaedics 8(1):70–73
Zhang Y, Yan M, Yu A, Mao H, Zhang J (2012) Inhibitory effects of β-tricalciumphosphate wear particles on osteocytes via apoptotic response and Akt inactivation. Toxicology. 297(1–3):57–67
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
WZY participated in the experimental study of the titanium particles intervening MLO-Y4 cells and collected relevant data; XW participated in the project design and gave technical guidance during the experiment;DQR participated in project design and revision of manuscript content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that we have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1186/s40634-020-00304-z
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, L., Wang, Z., Xu, W. et al. RETRACTED ARTICLE: Titanium particles damage osteocytes and inhibit osteoblast differentiation. J EXP ORTOP 7, 47 (2020). https://doi.org/10.1186/s40634-020-00268-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-020-00268-0