Abstract
A growing body of evidence supports the use of extracorporeal membrane oxygenation (ECMO) for severe acute respiratory distress syndrome (ARDS) refractory to maximal medical therapy. ARDS may develop in a proportion of patients hospitalized for coronavirus disease 2019 (COVID-19) and ECMO may be used to manage patients refractory to maximal medical therapy to mitigate the risk of ventilator-induced lung injury and provide lung rest while awaiting recovery. The mortality of COVID-19-related ARDS was variously reassessed during the pandemic. Veno-venous (VV) ECMO was the default choice to manage refractory respiratory failure; however, with concomitant severe right ventricular dysfunction, venoarterial (VA) ECMO or mechanical right ventricular assist devices with extracorporeal gas exchange (Oxy-RVAD) were also considered. ECMO has also been used to manage special populations such as pregnant women, pediatric patients affected by severe forms of COVID-19, and, in cases with persistent and seemingly irreversible respiratory failure, as a bridge to successful lung transplantation. In this narrative review, we outline and summarize the most recent evidence that has emerged on ECMO use in different patient populations with COVID-19-related ARDS.
Similar content being viewed by others
COVID-19-related ARDS
The clinical presentation of coronavirus disease 2019 (COVID-19) is notably heterogeneous, ranging from no symptoms to potentially fatal acute respiratory distress syndrome (ARDS) and, in a small minority of cases, from myocardial inflammation (e.g., myocarditis) to cardiogenic shock [1, 2]. ARDS is characterized by an increase in the anatomical shunt (e.g., increase in noncardiogenic pulmonary edema) and by a reduction of functioning lung size (i.e., “baby lung”), which accounts for high respiratory system elastance. In these patients, increasing lung size by recruiting or maintaining the patency of previously collapsed lung units is often achieved using moderate-to-high levels of positive end-expiratory pressure (PEEP), prone positioning, and occasionally via lung recruitment maneuvers [3]. In patients with early COVID-19-related ARDS, hypoxemia could be explained by an increase in the physiologic shunt due to loss of hypoxic pulmonary vasoconstriction and by an increase in dead space fraction due to development of pulmonary vascular microthrombi [4, 5]. Of note, preliminary hyper-inflammatory and hypo-inflammatory sub-phenotypes, defined by unique clinical features and biomarkers, have been described in COVID-19-related ARDS. The hyper-inflammatory sub-phenotype has higher inflammatory and lactate markers than the hypo-inflammatory sub-phenotype and is associated with significantly higher 90-day mortality than the hypo-inflammatory sub-phenotype (75% vs. 48%) [6]. The two sub-phenotypes may respond differently to corticosteroid treatment, with the suggestion of an improved survival in the hyper-inflammatory sub-phenotype, but not in the hypo-inflammatory sub-phenotype [6, 7].
Regarding respiratory mechanics, recently Reddy et al. found no evidence of distinct clinical phenotypes [8]. In a well-conducted systematic review and meta-analysis of 37 studies of COVID-19-related ARDS published between 2019 and 2022, the mean compliance of the respiratory system (CRS) was inversely proportional to the severity of ARDS (39.3 mL/cm H2O [36.6–42.0] in mild ARDS, 34.9 mL/cm H2O [32.8–36.9] in moderate ARDS, and 27.3 mL/cm H2O [23.3–31.2] in severe ARDS). Therefore, the mean CRS measured close to the time of the initiation of invasive mechanical ventilation was normally distributed in these patients just like in conventional ARDS, with no evidence of distinct clinical phenotypes based on respiratory mechanics. Based on these findings, traditional lung protective ventilation strategies tailored to the patient’s lung mechanics are recommended in patients with severe COVID-19 ARDS. [8, 9]. However, COVID‐19 patients seem to have a higher extravascular lung water index (EVLWi) and pulmonary vascular permeability index (PVPI) values than non-COVID-19 patients, from the beginning of the disease [10].
Extracorporeal membrane oxygenation (ECMO)
ECMO is currently used to manage severe respiratory and/or cardiac failure unresponsive to optimal conventional management. In general, veno-venous (VV) ECMO is used to manage severe respiratory failure, while venoarterial (VA) ECMO is used to manage severe cardiac failure [11]. In VV ECMO, deoxygenated blood is drained from a central vein and is pumped through a membrane lung in which gas exchange occurs. Oxygenated blood is then reinfused back into the venous system [11, 12]. Conversely, in VA ECMO, blood is reinfused directly back into the arterial system, augmenting the cardiac output provided by the native heart [11]. In general, patients with COVID-19-related ARDS refractory to medical therapy have been supported with VV ECMO, while patients presenting with both respiratory failure and right ventricular dysfunction (or COVID-19 myocarditis) have potential required support with VA ECMO or a combination of both [13, 14].
Evidence for ECMO in the management of ARDS
The use of ECMO to manage patients with severe ARDS has increased in recent years, in part due to the experience with patients supported by ECMO during the 2009 influenza A(H1N1) pandemic [15, 16]. Despite several methodological limits, the randomized controlled trial and parallel economic evaluation of Conventional ventilatory support versus Extracorporeal membrane oxygenation for Severe Adult Respiratory failure (CESAR) trial provided evidence of likely benefit from the use of ECMO in patients with acute hypoxemic respiratory failure [16]. Therefore, the Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome (EOLIA) trial was designed to better define the role of ECMO in the management of severe ARDS [17]. In this study, patients were randomized to ECMO or standard care (protocolized mechanical ventilation). Although this trial was stopped for futility (despite reporting a non-significant 11% absolute difference in 60-day mortality), a post hoc analysis using a Bayesian approach suggested a survival benefit with the use of ECMO [17, 18]. Supported by the results of these studies and subsequent meta-analyses, VV ECMO has achieved a role in the management of patients with severe ARDS when the ratio of arterial oxygen partial pressure to fractional inspired oxygen (PaO2/FIO2 ratio) is lower than 50 mmHg for more than three hours, the PaO2/FIO2 is lower than 80 mmHg for more than six hours and the pH is lower than 7.25 with a partial pressure of carbon dioxide (PaCO2) greater than or equal to 60 mmHg for more than six hours [17, 19] (Table 1).
VV ECMO and COVID-19-related ARDS
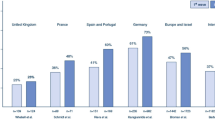
Despite dismal outcomes reported from preliminary reports on the use of ECMO [20, 21], data collected by international registries and larger cohort studies highlighted that outcomes for patients with COVID-19-related ARDS supported with ECMO were similar to those reported in patients with non-COVID-19-related ARDS [22]. Further data also highlighted that both ECMO duration and mortality were unexpectedly increasing over time [23,24,25,26,27,28,29]. At the beginning of the pandemic (“first wave”), several studies have reported a 90-day mortality rate between 36 and 47% [23,24,25,26].
From mid-2020, studies reported higher mortality with the use of ECMO for COVID-19, raising concerns about patient selection [25,26,27,28,29,30,31,32]. This apparent worsening of mortality could be explained by several factors: the potential self-induced lung injury caused by prolonged use of non-invasive respiratory support before endotracheal intubation, more liberal ECMO use, the increase in bacterial superinfections due to more frequent use of COVID-19 immunosuppressive treatments over time, and the use of ECMO in less experienced centers [27]. Of note, the use of ECMO for COVID-19-related ARDS was associated with a high number of thrombotic complications in the extracorporeal circuit compared to non-COVID-19 related ARDS [33, 34]. In general management of anticoagulation is complex during ECMO and requires special attention in COVID-19 patients who have a greater risk of thrombosis than other etiologies [35]. Based on these data, many centers have tried to increase their anticoagulation targets and have also tried alternative drugs (e.g., bivalirudin), however, the bleeding risk remained a concern [36]. So far, there are insufficient data to suggest deviation from usual anticoagulation practices for patients with COVID-19 receiving ECMO [37].
Propensity score matching analysis [38] and recent systematic reviews and meta-analyses have supported the positive results of these cohort studies conducted at the beginning of pandemic; however, since the causes of temporal increase in mortality observed in the later phase of pandemic were not addressed in these meta-analyses, the effectiveness of ECMO for COVID-19 remained controversial [39, 40].
Using observational data to emulate a randomized controlled trial represents an established statistical approach to estimate treatment effectiveness of an intervention in an uncontrolled setting when randomized controlled trials cannot be performed because of restrictive inclusion criteria, likelihood of crossover among treatments, costs, slow enrollment rate, lack of equipoise, and ethical issues [41, 42]. Investigating the effectiveness of ECMO during a global pandemic has been challenging and emulation trials have been used for this purpose. These new statistical analyses represent an attractive alternative to randomized trials to answer the question of interest, using available observational data.
Three target emulation trials (Table 2) have been recently developed to evaluate the efficacy of ECMO versus conventional mechanical ventilation in patients with severe COVID-19-related ARDS [43,44,45]. Shaefi et al., including patients with severe hypoxemia (PaO2/FIO2 < 80 mmHg), observed a reduction in 60-day hospital mortality associated with ECMO (hazard ratio 0.55; 95% confidence interval (CI) 0.40–0.77) [43]. Hajage et al. observed that patients with severe hypoxemia (PaO2/FIO2 < 80 mmHg) receiving ECMO had a higher survival probability on day 7 compared to the alternative strategy without ECMO (87% vs 83%, risk difference, 4%; 95% CI, 0–9%), but worsened at day 90 (63% on ECMO versus 65% on conventional arm, risk difference: − 2%; 95% CI, − 10 to 5%) [44]. Of note, this apparent reversal of the efficacy of ECMO at 90 days was no longer present when the analysis was performed including only high-volume centers. The authors concluded that VV ECMO should be started early (within the first 4 days of invasive mechanical ventilation) and only in severe hypoxemic patients (PaO2/FIO2 < 65) [44]. In this cohort, ECMO was associated with higher survival when performed in high-volume ECMO centers or in regions where specific inter-institutional ECMO networks were set up to handle high demand. This suggests that centralization of regional ECMO services to high-volume centers may represent the optimal approach. A third and larger emulated target trial from the COVID-19 Critical Care Consortium Investigators [45], including 7345 COVID-19 patients of whom 844 patients received ECMO [39], showed that patients with severe hypoxemia (PaO2/FIO2 < 80 mmHg) supported with ECMO reported a 60-day mortality lower than that of patients managed only with mechanical ventilation (26% versus 33.2%; risk difference: − 7.1%, 95% CI: − 8.2% to − 6.1%, RR 0.78; CI: 0.75–0.82). Factors associated with favorable outcome included age < 65 years, PaO2/FiO2 < 80, duration of invasive mechanical ventilation ≤ 10 days and driving pressure > 15 cm H2O [45]. Contrarily, we do not have any data to suggest a specific ventilatory setting during ECMO for COVID-19 ARDS patients. Since COVID-19 ARDS has similar lung mechanic characteristics of non-COVID-19 ARDS, a recent consensus statement suggested to use “lung rest settings” (very low-pressure, low-volume ventilation, low rate ventilation and a moderate PEEP to avoid the increase of lung collapse) for COVID-19 patients receiving ECMO for ARDS [37]. In summary, evidence provided by these emulated targeted trials supported the role of ECMO for patients with severe ARDS due to COVID-19. Greater benefit was seen in patients who received ECMO earlier in their course of mechanical ventilation, those with severe hypoxemia, or in those receiving high-intensity mechanical ventilation.
VA ECMO and COVID-19-related ARDS
ARDS was the most common clinical presentation of COVID-19 patients in critical care, and VV ECMO was the most commonly used ECMO configuration (> 95%) [26]. Among patients with COVID-19-related ARDS, heart failure occurred as a complication of various intercurrent factors: sepsis-related injury, cytokine storm, microvascular thrombosis, severe hypoxia, and direct cardiomyocyte damage [46,47,48]. Right ventricular (RV) dysfunction occurred in one-fifth of patients with COVID-19 related ARDS and was associated with a threefold increase in mortality [47]. Despite increasing knowledge about cardiac involvement in COVID-19, there are few data on the use of mechanical circulatory support in COVID-19 patients. Furthermore, VA-ECMO may have been underutilized during the pandemic [49]. Mortality and the rate of complications was higher in COVID-19-related ARDS patients with heart failure, especially in those supported with VA ECMO or where a change in configuration was delayed (3.1%) [50]. In ARDS patients who developed right ventricular dysfunction, a promising approach was the use of a right ventricular assist device with an oxygenator (Oxy-RVAD). Cain et al. compared 18 COVID-19 ARDS patients on Oxy-RVAD with 18 similar patients on invasive mechanical ventilation alone [51]. Patients treated with Oxy-RVAD reported a significantly lower in-hospital mortality and 30-day mortality than control patients [51].
Special populations
Use of ECMO in pregnant patients
ARDS is the most frequent cause of both admission to ICU in pregnant women and of life-threatening events for both the mother and fetus [52]. Pregnancy is an independent risk factor for ARDS and its incidence is between 70 and 120 cases per 100.000 deliveries [53]. Other pregnancy-specific risk factors for ARDS include preeclampsia, amniotic fluid embolism, tocolytic-associated pulmonary edema, and peripartum sepsis [54]. Several physiologic changes may increase the risk of ARDS in pregnant women, including the reduction of functional residual capacity (FRC) and the increase in plasma volume [55]. SARS-CoV-2 may further increase this risk by impairing the immune system, respiratory function, and coagulation system [56]. During the 2009 influenza A(H1N1) pandemic, ECMO was widely and successfully used as a rescue strategy for refractory ARDS and this was replicated during the COVID-19 pandemic [57]. In general, outcomes of pregnant and peripartum patients supported on ECMO are good and comparable to or better than many of the other cohorts [58]. In a retrospective cohort study, O’Neil et al. described 100 COVID-19 pregnant or peripartum patients supported by VV ECMO. ECMO-related complications, in particular renal complications, and hospital mortality were lower than in non-pregnant patients supported with VV ECMO for ARDS [59]. Based on these findings, the Society for Maternal–Fetal Medicine guidelines recommended the use of ECMO in refractory COVID-19-related ARDS in pregnant patients less than 32 weeks of gestation to facilitate fetal development in utero or after delivery [60]. Of note, pregnant women with severe COVID-19 should be referred early to an experienced ECMO center. In pregnant patients, ECMO blood flow should be kept high to maintain maternal SaO2 > 90% and thus preserve adequate fetal oxygenation. PaCO2 should be targeted between 28 and 32 mmHg to facilitate fetal CO2 elimination and oxygen intake. Resting ventilation (e.g., plateau pressure < 25 cmH2O, PEEP 10–15 cmH2O, FiO2 30–40%, and a respiratory rate of 5–10 breaths/min) should be used during ECMO to mitigate the risk of ventilator-induced lung injury (VILI) and facilitate lung recovery [60]. Multidisciplinary discussion is essential when evaluating the timing and mode of delivery.
ECMO in pediatric patients
Evidence from the first two years of the COVID-19 pandemic showed that children were less affected than adults and usually developed mild disease which was less likely to require hospital admission [61]. However, when children required hospital admission, up to one-quarter required pediatric intensive care unit (PICU) admission [61]. The mortality rate of pediatric COVID-19 was significantly lower compared with adults (< 1% in children); however, a higher mortality (up to 10%) was observed in low- and middle-income countries and in patients with pre-existing health problems [62]. In general, children with severe acute COVID-19 are admitted to PICU for pediatric ARDS (PARDS) or multisystem inflammatory syndrome (MISC) related to COVID-19. PARDS related to COVID-19 is not different from other etiologies of PARDS, therefore, the general principles of management and end goals of respiratory therapy are the same as other causes of PARDS [63]. Recent data suggest that patients with refractory hypoxemia or cardiogenic shock related to MIS-C may benefit from ECMO; however, precise ECMO indications remain unclear due to the limited number of patients treated so far [64, 65]. Although these studies may be affected by publication bias, ECMO survival in PARDS-related to COVID-19 was higher than that of PARDS from other etiologies. Of note, ECMO survival for PARDS-related to COVID-19 was higher and ECMO complications were lower in children than adults receiving ECMO for COVID-19 [66].
Prolonged ECMO and lung transplantation
Few data exist on long-term pulmonary function in COVID-19-related ARDS patients receiving ECMO support [67]. Despite this, lung transplantation has been used as a potentially life-saving therapy in COVID-19 patients with persistent lung failure and inability to wean from ECMO, despite several weeks or months of support in the intensive care unit [68]. Clear evidence and guidelines on the indications, timing and patient selection for lung transplantation in COVID-19 patients with irreversible ARDS are scant. Some authors have suggested the use of lung transplantation in patients: (1) aged < 65 years, (2) with only single organ dysfunction, and (3) at least 4–6 weeks after the onset of respiratory failure. Good neurological status and ability to participate in a physical rehabilitation program are essential points for postoperative success (Table 3) [69]. Despite these suggestions, lung transplant candidacy remains controversial in COVID-19 patients receiving prolonged ECMO. Mohanka et al. compared the outcomes of 10 patients who required ECMO for less than 30 days with 10 patients who received prolonged ECMO support (> 30 days) [70]. Mohanka et al. observed that patients supported with prolonged ECMO for COVID-19-related ARDS recovered without the need of a lung transplant beyond the 6-week period and suggested a more conservative timeline when considering lung transplantation [70]. Based on these findings, a multidisciplinary approach should be used to assess whether patients with COVID-19-related ARDS receiving ECMO may have the potential for recovery or not, since healing without transplantation is obviously more beneficial [71]. Of note, in the past two pandemic years, several concerns have emerged regarding the use of lung transplantation in COVID-19 patients, such as the shortage of donors, the penalization of patients on the waiting list, the lack of follow-up data beyond one year after lung transplant and the potential discrimination in organ allocation systems, along with underestimation of the potential for lung parenchyma healing even after prolonged ECMO support [72,73,74,75]. Lastly, there may be ethical dilemmas surrounding candidacy for lung transplantation in those who have declined COVID-19 vaccination [76].
Conclusions
ECMO is a well-established strategy for supporting patients with acute respiratory failure and has been successfully used in the management of COVID-19-related ARDS. Patients undergoing ECMO for COVID-19-related ARDS appear to have worse outcomes than those with non-COVID-19-related ARDS. Nonetheless, evidence provided by emulated targeted trials have highlighted a probably beneficial effect of ECMO in selected patients with severe COVID-19-related ARDS. A higher benefit was observed in patients with severe hypoxemia and those receiving high-intensity mechanical ventilation earlier in the course of illness. A greater likelihood of success was seen in high-volume, specialized centers. In patients with COVID-19-related ARDS and right heart failure, VV ECMO has been also used to improve myocardial contractility (e.g., pH normalization and PaCO2 reduction favoring a decrease in pulmonary vascular resistance); however, in refractory cases, VA ECMO and hybrid configurations have been successfully used. Several studies also observed a potential benefit of ECMO in pregnancy and in children. Furthermore, in prolonged respiratory failure, ECMO has also been used as a bridge to lung transplantation. Studies are needed to identify early interventions that may improve in-hospital outcomes and reduce the pressure on health systems due to health complications later.
Availability of data and materials
Not applicable.
Abbreviations
- FIO2 :
-
High fraction of inspired oxygen
- VV-ECMO:
-
Veno-venous extracorporeal membrane oxygenation
- VA-ECMO:
-
Veno-arterial extracorporeal membrane oxygenation
- COVID-19:
-
Coronavirus infectious disease 2019
- SARS-Cov2:
-
Severe acute respiratory syndrome coronavirus 2
- PaO2/FIO2ratio:
-
Ratio of arterial oxygen partial pressure to fractional inspired oxygen
- PaCO2 :
-
Partial pressure of carbon dioxide
- SpO2 :
-
Peripheral oxygen saturation
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324(8):782–93.
Alessandri F, Pugliese F, Ranieri VM. The role of rescue therapies in the treatment of severe ARDS. Respir Care. 2018;63(1):92–101.
Gattinoni L, Chiumello D, Rossi S. COVID-19 pneumonia: ARDS or not? Crit Care. 2020;24:154.
Xie Y, Wang X, Yang P, Zhang S. COVID-19 complicated by acute pulmonary embolism. Radiol Cardiothorac Imaging. 2020;2: e200067.
Sinha P, Furfaro D, Cummings MJ, Abrams D, Delucchi K, Maddali MV, et al. Latent class analysis reveals COVID-19-related acute respiratory distress syndrome subgroups with differential responses to corticosteroids. Am J Respir Crit Care Med. 2021;204(11):1274–85.
Tran A, Fernando SM, Rochwerg B, Barbaro RP, Hodgson CL, Munshi L, et al. Prognostic factors associated with mortality among patients receiving venovenous extracorporeal membrane oxygenation for COVID-19: a systematic review and meta-analysis. Lancet Respir Med. 2022; 10:S2213-2600(22)00296-X.
Reddy MP, Subramaniam A, Chua C, Ling RR, Anstey C, Ramanathan K, et al. Respiratory system mechanics, gas exchange, and outcomes in mechanically ventilated patients with COVID-19-related acute respiratory distress syndrome: a systematic review and meta-analysis. Lancet Respir Med. 2022; 3: S2213-2600(22)00393-9.
Schultz MJ, van Meenen DM, Bos LD. COVID-19-related acute respiratory distress syndrome: lessons learned during the pandemic. Lancet Respir Med. 2022; 3:S2213-2600(22)00401-5.
Shi R, Lai C, Teboul JL, Dres M, Moretto F, De Vita N, et al. COVID-19 ARDS is characterized by higher extravascular lung water than non-COVID-19 ARDS: the PiCCOVID study. Crit Care. 2021;25(1):186.
Combes A, et al. Extracorporeal life support for adults with acute respiratory distress syndrome. Intensive Care Med. 2020;46(12):2464–76.
Schmidt M, Tachon G, Devilliers C, Muller G, Hekimian G, Brechot N, et al. Blood oxygenation and decarboxylation determinants during venovenous ECMO for respiratory failure in adults. Intensive Care Med. 2013;39(5):838–46.
Maharaj V, Alexy T, Agdamag AC, Kalra R, Nzemenoh BN, Charpentier V, Bartos JA, Brunsvold ME, Yannopoulos D. Right ventricular dysfunction is associated with increased mortality in patients requiring venovenous extracorporeal membrane oxygenation for coronavirus disease 2019. ASAIO J. 2022;68(6):772–8.
Bhardwaj A, Kirincich J, Rampersad P, Soltesz E, Krishnan S. Fulminant myocarditis in COVID-19 and favorable outcomes with VA-ECMO. Resuscitation. 2022;175:75–6.
Pham T, Combes A, Rozé H, Chevret S, Mercat A, Roch A, et al. Extracorporeal membrane oxygenation for pandemic influenza A(H1N1)-induced acute respiratory distress syndrome: a cohort study and propensity-matched analysis. Am J Respir Crit Care Med. 2013;187(3):276–85.
Peek GJ, Elbourne D, Mugford M, Tiruvoipati R, Wilson A, Allen E, et al. A Randomized controlled trial and parallel economic evaluation of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR). Health Technol Assessment (Winchester, England). 2010;14:1–46.
Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–75.
Goligher EC, Tomlinson G, Hajage D, Wijeysundera DN, Fan E, Juni P, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome and posterior probability of mortality benefit in a post hoc Bayesian analysis of a randomized clinical trial. JAMA. 2018;320:2251–9.
Combes A, Peek GJ, Hajage D, Hardy P, Abrams D, Schmidt M, et al. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020;46:2048–57.
Ñamendys-Silva SA. ECMO for ARDS due to COVID-19. Heart Lung. 2020;49(4):348–9.
Henry BM, Lippi G. Poor survival with extracorporeal membrane oxygenation in acute respiratory distress syndrome (ARDS) due to coronavirus disease 2019 (COVID-19): pooled analysis of early reports. J Crit Care. 2020;58:27–8.
Bartlett RH, Ogino MT, Brodie D, McMullan DM, Lorusso R, MacLaren G, et al. Initial ELSO guidance document: ECMO for COVID-19 patients with severe cardiopulmonary failure. ASAIO J. 2020;66:472–4.
Schmidt M, Hajage D, Lebreton G, Monsel A, Voiriot G, Levy D, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir Med. 2020;8(11):1121–31.
Lorusso R, Combes A, Lo Coco V, De Piero ME, Belohlavek J, EuroECMO COVID-19 WorkingGroup; Euro-ELSO Steering Committee. ECMO for COVID-19 patients in Europe and Israel. Intensive Care Med. 2021;47(3):344–8.
Lorusso R, De Piero M, Mariani M, Di Mauro M, Folliguet T, Taccone FS et al. In-hospital and 6-month outcomes in patients with COVID-19 supported with extracorporeal membrane oxygenation (EuroECMO-COVID): a multicentre, prospective observational study Lancet Respir Med. 2022. https://doi.org/10.1016/S2213-2600(22)00403-9.
Barbaro RP, MacLaren G, Boonstra PS, Iwashyna TJ, Slutsky AS, Fan E, Extracorporeal Life Support Organization, et al. Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the Extracorporeal Life Support Organization registry. Lancet. 2020;396:1071–8.
Broman LM, Eksborg S, Lo Coco V, De Piero ME, Belohlavek J, Lorusso R, et al. Extracorporeal membrane oxygenation for COVID-19 during first and second waves. Lancet Respir Med. 2021;9:e80–1.
Riera J, Roncon-Albuquerque R Jr, Fuset MP, Alcantara S, Blanco-Schweizer P, ECMOVIBER Study Group. Increased mortality in patients with COVID-19 receiving extracorporeal respiratory support during the second wave of the pandemic. Intensive Care Med. 2021;47:1490–3.
Barbaro RP, MacLaren G, Boonstra PS, Combes A, Agerstrand C, Annich G, Extracorporeal Life Support Organization, et al. Extracorporeal membrane oxygenation for COVID-19: evolving outcomes from the international Extracorporeal Life Support Organization registry. Lancet. 2021;398:1230–8.
Ohshimo S, Liu K, Ogura T, Iwashita Y, Kushimoto S, Shime N, et al. Trends in survival during the pandemic in patients with critical COVID-19 receiving mechanical ventilation with or without ECMO: analysis of the Japanese national registry data. Crit Care. 2022;26(1):354.
Karagiannidis C, Strassmann S, Merten M, Bein T, Windisch W, Meybohm P, et al. High in-hospital mortality rate in patients with COVID-19 receiving extracorporeal membrane oxygenation in Germany: a critical analysis. Am J Respir Crit Care Med. 2021;204:991–4.
Karagiannidis C, Slutsky AS, Bein T, Windisch W, Weber-Carstens S, Brodie D. Complete countrywide mortality in COVID patients receiving ECMO in Germany throughout the first three waves of the pandemic. Crit Care. 2021;25:413.
Bemtgen X, Zotzmann V, Benk C, Rilinger J, Steiner K, Asmussen A, et al. Thrombotic circuit complications during venovenous extracorporeal membrane oxygenation in COVID-19. J Thromb Thrombolysis. 2021;51(2):301–7.
Parzy G, Daviet F, Puech B, Sylvestre A, Guervilly C, Porto A, et al. Venous thromboembolism events following venovenous extracorporeal membrane oxygenation for severe acute respiratory syndrome coronavirus 2 based on CT scans. Crit Care Med. 2020;48(10):e971–5.
Guo Z, Sun L, Li B, Tian R, Zhang X, Zhang Z, Clifford SP, et al. Anticoagulation management in severe coronavirus disease 2019 patients on extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2021;35(2):389–97.
Seelhammer TG, Rowse P, Yalamuri S. Bivalirudin for maintenance anticoagulation during venovenous extracorporeal membrane oxygenation for COVID-19. J Cardiothorac Vasc Anesth. 2021;35(4):1149–53.
Badulak J, Antonini MV, Stead CM, Shekerdemian L, Raman L, Paden ML, et al. Extracorporeal membrane oxygenation for COVID-19: updated 2021 guidelines from the extracorporeal life support organization. ASAIO J. 2021;67(5):485–95.
Mustafa AK, Joshi DJ, Alexander PJ, Tabachnick DR, Cross CA, Jweied EE, Mody NS, Huh MH, Fasih S, Pappas PS, Tatooles AJ. Comparative propensity matched outcomes in severe COVID-19 respiratory failure-extracorporeal membrane oxygenation or maximum ventilation alone. Ann Surg. 2021;274(5):e388–94.
Bertini P, Guarracino F, Falcone M, Nardelli P, Landoni G, Nocci M, Paternoster G. ECMO in COVID-19 patients: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2022;36(8 Pt A):2700–6.
Ramanathan K, Shekar K, Ling RR, Barbaro RP, Wong SN, Tan CS, et al. Extracorporeal membrane oxygenation for COVID-19: a systematic review and meta-analysis. Crit Care. 2021;25(1):211.
Hernán MA. How to estimate the effect of treatment duration on survival outcomes using observational data. BMJ. 2018;360: k182.
Hernán MA, Robins JM. Using big data to emulate a target trial when a randomized trial is not available. Am J Epidemiol. 2016;183:758–64.
Shaefi S, Brenner SK, Gupta S, O’Gara BP, Krajewski ML, Charytan DM, et al. Extracorporeal membrane oxygenation in patients with severe respiratory failure from COVID-19. Intensive Care Med. 2021;47:208–21.
Hajage D, Combes A, Guervilly C, Lebreton G, Mercat A, Pavot A, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: an emulated target trial analysis. Am J Respir Crit Care Med. 2022;206(3):281–94.
Urner M, Barnett AG, Bassi GL, Brodie D, Dalton HJ, Ferguson ND, et al. Venovenous extracorporeal membrane oxygenation in patients with acute covid-19 associated respiratory failure: comparative effectiveness study. BMJ. 2022;377: e068723.
Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli- Berg FM, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116:1666–87.
Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–10.
Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5:831–40.
Musher DM, Abers MS, Corrales-Medina VF. Acute infection and myocardial infarction. N Engl J Med. 2019;380:171–6.
Mariani S, De Piero ME, Ravaux JM, Saelmans A, Kawczynski MJ, van Bussel BCT, et al. Temporary mechanical circulatory support for COVID-19 patients: a systematic review of literature. Artif Organs. 2022;46(7):1249–67.
Cain MT, Smith NJ, Barash M, Simpson P, Durham LA 3rd, Makker H, et al. Extracorporeal membrane oxygenation with right ventricular assist device for COVID-19 ARDS. J Surg Res. 2021;264:81–9.
Pollock W, Rose L, Dennis CL. Pregnant and postpartum admissions to the intensive care unit: a systematic review. Intensive Care Med. 2010;36(9):1465–74.
Vasquez DN, Estenssoro E, Canales HS, Reina R, Saenz MG, Das Neves AV, et al. Clinical characteristics and outcomes of obstetric patients requiring ICU admission. Chest. 2007;131(3):718–24.
Pham T, Rubenfeld GD. Fifty years of research in ARDS. The epidemiology of acute respiratory distress syndrome. A 50th birthday review. Am J Respir Crit Care Med. 2017;195(7):860–70.
Hegewald MJ, Crapo RO. Respiratory physiology in pregnancy. Clin Chest Med. 2011;32(1):1–13.
Kumar R, Yeni CM, Utami NA, Masand R, Asrani RK, Patel SK, et al. SARS-CoV-2 infection during pregnancy and pregnancy-related conditions: concerns, challenges, management and mitigation strategies-a narrative review. J Infect Public Health. 2021;14(7):863–75.
Wong MJ, Bharadwaj S, Galey JL, Lankford AS, Galvagno S, Kodali BS. Extracorporeal membrane oxygenation for pregnant and postpartum patients. Anesth Analg. 2022;135(2):277–89.
Ramanathan K, Tan CS, Rycus P, Anders M, Lorusso R, Zhang JJY, MacLaren G. Extracorporeal membrane oxygenation in pregnancy: an analysis of the extracorporeal life support organization registry. Crit Care Med. 2020;48(5):696–703.
O’Neil ER, Lin H, Shamshirsaz AA, Naoum EE, Rycus PR, Alexander PM. Pregnant/peripartum women with COVID-19 high survival with ECMO: an ELSO registry analysis. Am J Respir Crit Care Med. 2022;205(2):248–50.
Kalyanaraman M, Anderson MR. COVID-19 in Children. Pediatr Clin North Am. 2022;69(3):547–71.
Gonzalez-Dambrauskas S, Vasquez-Hoyos P, Camporesi A, Cantillano EM, Dallefeld S, Dominguez-Rojas J, Critical Coronavirus and Kids Epidemiological (CAKE) Study Investigators, et al. Paediatric critical COVID-19 and mortality in a multinational prospective cohort. Lancet Reg Health Am. 2022;12:100272.
Rimensberger PC, Cheifetz IM, Pediatric Acute Lung Injury Consensus Conference Group. Ventilatory support in children with pediatric acute respiratory distress syndrome: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015;16(51):S51-60.
Di Nardo M, Hoskote A, Thiruchelvam T, Lillie J, Horan M, Belda Hofheinz S, et al. Extracorporeal membrane oxygenation in children with coronavirus disease 2019: preliminary report from the collaborative European chapter of the extracorporeal life support organization prospective survey. ASAIO J. 2021;67(2):121–4.
Di Nardo M, De Piero ME, Hoskote A, Belohlavek J, Lorusso R, EuroECMO neonatal and paediatric COVID-19 Working Group and EuroELSO Steering Committee. Extracorporeal membrane oxygenation in children with COVID-19 and PIMS-TS during the second and third wave. Lancet Child Adolesc Health. 2022;6(4):e14–5.
Brodie D, Abrams D, MacLaren G, Brown CE, Evans L, Barbaro RP, et al. Extracorporeal membrane oxygenation during respiratory pandemics: past, present, and future. Am J Respir Crit Care Med. 2022;205(12):1382–90.
Lang C, Ritschl V, Augustin F, Lang G, Moser B, Taghavi S, et al. Clinical relevance of lung transplantation for COVID-19 ARDS: a nationwide study. Eur Respir J. 2022;60(3):2102404.
Magnusson JM, Silverborn M, Broomé M, Riise GC, Dellgren G. Long-term extracorporeal membrane oxygenation bridge to lung transplantation after COVID-19. Ann Thorac Surg. 2022;113(1):e5–8.
Bharat A, Machuca TN, Querrey M, Kurihara C, Garza-Castillon R Jr, Kim S, et al. Early outcomes after lung transplantation for severe COVID-19: a series of the first consecutive cases from four countries. Lancet Respir Med. 2021;9(5):487–97.
Mohanka MR, Joerns J, Lawrence A, Bollineni S, Kaza V, Cheruku S, et al. ECMO long haulers: a distinct phenotype of COVID-19-associated ARDS with implications for lung transplant candidacy. Transplantation. 2022;106(4):e202–11.
Martin AK, Shah SZ, Guru PK, Chaudhary S, Franco PM, Makey I, et al. Multidisciplinary approach for lung transplantation due to COVID-19. Mayo Clin Proc Innov Qual Outcomes. 2022;6(3):200–8.
Kurihara C, Manerikar A, Gao CA, Watanabe S, Kandula V, Klonis A, et al. Outcomes after extracorporeal membrane oxygenation support in COVID-19 and non-COVID-19 patients. Artif Organs. 2022;46(4):688–96.
Bharat A, Querrey M, Markov NS, Kim S, Kurihara C, Garza-Castillon R, et al. Lung transplantation for patients with severe COVID-19. Sci Transl Med. 2020;12:eabe4282.
Lepper PM, Langer F, Wilkens H, Schäfers HJ, Bals R. Lung transplantation for COVID-19-associated ARDS. Lancet Respir Med. 2021;9(9): e88.
Riou J, Boëlle PY, Christie JD, Thabut G. High emergency organ allocation rule in lung transplantation: a simulation study. ERJ Open Res. 2017;3(4):00020–2017.
Messika J, Schmidt M, Tran-Dinh A, Mordant P. Lung transplantation for COVID-19-associated ARDS. Lancet Respir Med. 2021;9: e89.
Raciborski F, Jankowski M, Gujski M, Pinkas J, Samel-Kowalik P. Changes in attitudes towards the COVID-19 vaccine and the willingness to get vaccinated among adults in Poland: analysis of serial, cross-sectional, representative surveys, January-April 2021. Vaccines (Basel). 2021;9:832.
Acknowledgements
Not applicable.
Funding
There was no funding support for this study.
Author information
Authors and Affiliations
Contributions
FA and MDN performed the literature review and wrote the first draft. KR, DB, and GM critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
References list of table 2 in order of appearance.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alessandri, F., Di Nardo, M., Ramanathan, K. et al. Extracorporeal membrane oxygenation for COVID-19-related acute respiratory distress syndrome: a narrative review. j intensive care 11, 5 (2023). https://doi.org/10.1186/s40560-023-00654-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-023-00654-7