Abstract
Background
We examined whether high lactate level in septic patients was associated with 90-day mortality based on the patients’ disseminated intravascular coagulation (DIC) status.
Methods
We conducted a multicenter, retrospective, observational study of patients admitted to the intensive care unit (ICU) with a suspicion of severe infection and diagnosed with sepsis. Regression analyses were performed to estimate the interaction effect between DIC status and the lactate level. Then, the association between the lactate level and 90-day mortality was assessed in the DIC and non-DIC subgroups.
Results
The data of 415 patients were analyzed. We found a significant interaction between DIC status and the lactate level for predicting 90-day mortality (pinteraction = 0.04). Therefore, we performed a subgroup analysis and found that high lactate concentration was significantly associated with 90-day mortality in the DIC group (odds ratio = 2.31, p = 0.039) but not in the non-DIC group.
Conclusions
In patients with DIC, a high lactate level significantly predicted 90-day mortality; no such association was found in the non-DIC group. Thus, DIC status may serve as a possible effect modifier of lactate level in predicting mortality in patients with sepsis.
Similar content being viewed by others
Background
Sepsis is among the most common causes of death among hospitalized patients [1], and its incidence has been increasing annually [2]. However, remarkable advances in the management of sepsis have been made in recent years, leading to significant improvements in survival [3]. As the recent Sepsis-3 definition includes the presence of organ dysfunction as a diagnostic criterion [4], increased attention has been paid to the management of organ dysfunction.
Organ dysfunction can be identified as an acute change of ≥ 2 points in the total Sequential (sepsis-related) Organ Failure Assessment (SOFA) score [5] resulting from infection. Although the prevention and management of infection-induced organ dysfunction is a key to the treatment of septic patients, the pathophysiological mechanisms underlying organ dysfunction in patients with sepsis are not entirely known. Among the causes of organ dysfunction in sepsis, disseminated intravascular coagulation (DIC) is considered to be partly involved [6]. The Japanese Association for Acute Medicine—disseminated intravascular coagulation (JAAM-DIC) diagnostic criteria consist of the prothrombin time ratio, systemic inflammatory response syndrome (SIRS) score, fibrin degradation product, and the count and/or reduction rate of platelets [7]. This scoring system was created for diagnosing septic DIC and was shown to have a good prognostic value for predicting mortality in patients with sepsis [8]. The defining characteristic of this score is that it reflects the intensity of inflammation and severity of coagulopathy based on the concept of crosstalk between coagulation and inflammation [9].
Although lactate is known to be an anaerobic metabolite and is considered to be a good predictor of sepsis severity, its elevation can occur for various other causes aside from sepsis. However, lactate level elevation coupled with severe inflammation and coagulopathy may reflect the early phase of organ dysfunction as microcirculatory dysfunction caused by persistent microthrombosis can induce a reduction in blood flow to the tissues and cause organ dysfunction in a later phase. Therefore, we hypothesized that using the lactate value in predicting mortality varies according to coagulation condition. In this study, we evaluated the usefulness of the lactate level in predicting mortality among patients with sepsis, based on the presence or absence of DIC.
Methods
This retrospective observational study was conducted at a Japanese university hospital and a Japanese community hospital (Fujita Health University Hospital and Nishichita General Hospital, respectively). A total of 415 patients aged ≥ 18 years who were admitted to the intensive care unit (ICU) with the suspicion of severe infection and diagnosed with sepsis with the use of the Sepsis-3 definition between January 2013 and December 2017 were selected for this study (between May 2015 and December 2017 in Nishichita General Hospital since the ICU in the hospital was established in May 2015). Our primary endpoint was 90-day mortality, and our secondary endpoint was 28-day mortality. Based on previous literature, we defined a suspicion of severe infection based on a combination of culture sampling and the initiation of antibiotic treatment. If the antibiotic was given prior to the culture, the culture sample must have been obtained within 24 h. If the culture sampling occurred first, the antibiotic must have been ordered within 72 h [10]. The exclusion criterion was unknown outcomes (alive or dead within 90 days).
We collected data on the patients’ medical history, physical examination results, and laboratory results from a retrospective review of medical records. Table 1 shows the classification according to the JAAM-DIC scoring system [7].
SIRS was defined according to the American College of Chest Physicians/Society of Critical Care Medicine [11] criteria. Scoring ≥ 4 points on the JAAM-DIC scale was the qualifying criterion for a diagnosis of DIC.
Lactate levels were measured at the time of admission to the intensive care unit, and we chose a cutoff value of 4 mmol/L for lactate because a lactate value equal or more than 4 mmol/L was demonstrated to be an independent risk factor for mortality in sepsis [12]. We classified patients with a lactate value ≥ 4 mmol/L as “high lactate.” Similarly, we classified patients with a lactate value < 4 mmol/L as “low lactate.”
Our hypothesis was to examine whether the effect of lactate on 90-day mortality depends on DIC/non-DIC status. In this study, this corresponds to the interaction effect between lactate and DIC status. Thus, we assessed for an interaction effect in the multivariable logistic regression model adjusted for age, sex, and SOFA score. To examine the actual relationship between lactate and 90-day mortality, additional subgroup analysis stratified by DIC status is required [13]. In addition, we conducted Cox proportional hazard regression analysis to confirm the main effect of lactate performance on mortality in each DIC/non-DIC group, with survival up to 90 days as the time variable. Covariates included age, sex, and SOFA score, which were identical to those included in the multiple logistic regression model [13]. The numerical values in the text and tables represent the median (interquartile range) unless otherwise noted. A p value < 0.05 was considered statistically significant. All statistical analyses were performed using EZR (version 1.31; Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (version 3.2.2; R Foundation for Statistical Computing, Vienna, Austria) [14].
Due to the anonymous nature of the data, the requirement for informed consent was waived. The study protocol was approved by the institutional review board of Fujita Health University and Nishichita General Hospital (approval no. HM18–190 and 30–25, respectively).
Results
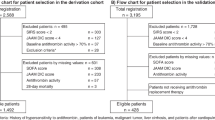
On the basis of the exclusion criteria, 76 patients were excluded (57 patients from Fujita Health University Hospital and 19 from Nishichita General Hospital), and finally, 415 patients were included in this study (346 patients from Fujita Health University Hospital and 69 from Nishichita General Hospital). Figure 1 shows a flow diagram of this research. Table 2 displays the baseline characteristics of all patients included in this study by DIC status.
The subjects included 281 men and 134 women with a median age of 72 (range, 62.5–78) years. Their median SOFA score was 7.0 (4.0–11); the median Acute Physiology and Chronic Health Evaluation (APACHE) II score [15] was high, at 23 (17–30). The patients’ median lactate level was also high, at 1.7 (1.1–3.3) mmol/L. The 28-day and 90-day mortality rates were 14.5% and 26.3%, respectively.
Tables 3 and 4 show the adjusted odds ratios (ORs) for DIC defined by JAAM-DIC score and high lactate value in predicting 28- and 90-day mortality, respectively.
After adjusting for age, sex, and SOFA score, the DIC defined by JAAM-DIC score ≥ 4 was significantly associated with 90-day mortality (OR = 2.2, 95% CI 1.27–3.8, p = 0.005). By contrast, a high lactate value was not significantly associated with either 28- or 90-day mortality (OR = 0.73, 95% CI 0.2–2.67, p = 0.635 and OR = 0.54, 95% CI 0.18–1.68, p = 0.289, respectively). The results further revealed a statistically significant interaction between the DIC status and lactate value for predicting 90-day mortality (pinteraction = 0.04) (Table 4).
Therefore, we performed subgroup analyses classified by the presence or absence of DIC. Tables 5 and 6 display the adjusted ORs for the lactate value as a predictor of 28- and 90-day mortality, respectively, in the DIC group using the multivariable logistic regression model.
Although high lactate level was not significantly associated with 28-day mortality (OR = 1.47, 95% CI 0.6–3.59, p = 0.4), it was significantly associated with 90-day mortality in the DIC group (OR = 2.31, 95% CI 1.04–5.13, p = 0.039).
Tables 7 and 8 show the adjusted ORs for a high lactate value in predicting 28- and 90-day mortality, respectively, in the non-DIC group using the multivariable logistic regression model.
Similar to the DIC group, a high lactate value was not significantly associated with 28-day mortality in the non-DIC group (OR = 0.67, 95% CI 0.18–2.5, p = 0.555). It was also not significantly associated with 90-day mortality in the non-DIC group (OR = 0.49, 95% CI 0.16–1.54, p = 0.223). As for the results of the Cox proportional hazard regression analysis with 90-day follow-up periods, the hazard ratio for lactate in the DIC group was 1.82 (95% CI 1.07–3.10, p = 0.028), whereas the hazard ratio for lactate in the non-DIC group was 0.58 (95% CI 0.20–1.62, p = 0.296).
Discussion
We examined whether changes in lactate level were useful for predicting mortality based on the patient’s DIC status, as defined by the JAAM-DIC diagnostic criteria. We found that a high lactate value was associated with 90-day mortality in the DIC group only.
Although we did not find a statistically significant relationship between lactate level and 90-day mortality, which some previous studies have found, we detected a difference in the association between lactate and 90-day mortality between the DIC and non-DIC groups. Since previous studies did not clarify the proportion of septic DIC patients based on Sepsis-3 and JAAM-DIC diagnostic criteria, it may be possible that previous studies which found an association between lactate and predicted mortality included a higher proportion of septic DIC patients compared to studies which did not detect lactate’s predictive value of mortality. To the best of our knowledge, this is the first reported study to have investigated the predictive value of lactate for mortality based on DIC status in septic patients. Previous studies have focused on a single parameter; thus, a strength of our investigation is that we examined the ability of lactate level to predict mortality based on stratification by DIC status.
Although the mechanisms underlying organ dysfunction in patients with sepsis remain poorly understood, DIC is thought to be partly involved in organ dysfunction pathogenesis in sepsis [6]. The Sepsis-3 guidelines define sepsis as life-threatening organ dysfunction caused by a dysregulated host response to infection [4]. Recently, researchers investigated the possible molecular biologic mechanisms of organ dysfunction caused by a dysregulated host response to infection. As one of the innate immune response systems, neutrophil extracellular traps (NETs) [16] released by neutrophils seem to play a role in early host defense against bacterial dissemination. NETs capture bacteria by forming immunothrombosis in local areas [17]. However, uncontrolled, excessive immunothrombosis involving severe inflammation may lead to DIC and possibly cause organ dysfunction by preventing adequate blood supply to the tissues [18]. In addition, activated platelets induce NETs to ensnare bacteria in septic blood [19]. It has also been shown that platelets and NETs cooperate to form blood clots in vitro [20]. The JAAM-DIC score includes all concepts related to a dysregulated host response that can be caused by excessive immunothrombosis and subsequent microcirculatory disorder which, theoretically, could lead to organ dysfunction.
Lactate values can be elevated for various reasons in sepsis. In addition to hypoxemia, mitochondrial insufficiency in metabolizing pyruvate, caused by excessive stress, can cause an elevation of lactate levels in septic patients. However, by combining the lactate value with the JAAM-DIC score, patients with poor prognoses and potential subsequent organ dysfunction could be detected at an earlier phase. This could explain why hyperlactaemia was associated with mortality in the DIC but not in the non-DIC group. We believe that our findings can help elucidate the pathophysiology underlying organ dysfunction induced by sepsis.
The medication ART123 [21], or recombinant human thrombomodulin alpha, targets sepsis-induced coagulopathy; it has gone through a phase 2b study [22] and is now being investigated in a randomized, double-blinded, placebo-controlled, phase 3 study. Theoretically, this medication has the most impact on patients with microcirculatory dysfunction and subsequent organ dysfunction caused by immunothrombosis. Thus, the findings of our study may aid in identifying subgroups of patients that can benefit from this medication by stratifying them by lactate values and the JAAM-DIC score.
In this study, we did not observe any significant differences between the DIC and non-DIC groups when examining the association between lactate level and 28-day mortality. We assume that this could be explained by the unique Japanese critical care system. In Japan, most medical costs are covered by public health insurance, and treatment is seldom withdrawn for patients with dismal prognoses. Thus, it is possible that severely ill patients were still alive at 28 days but not at 90 days. In this sense, we believe that 90-day mortality is a more useful outcome in this study than 28-day mortality; thus, we chose 90-day mortality as the primary outcome.
This study is not without limitations. First, because this was a retrospective study with a limited sample size, the risk of residual confounding and the risk of type I error remain. Additional work is necessary to provide more definitive data. Second, all the patients analyzed in this study were Asians; therefore, it is unclear whether our findings apply to other ethnic groups. However, this was a preliminary study to identify possible associations. Multicenter prospective studies are warranted to confirm the findings of this study.
Conclusions
In septic patients with DIC, elevated lactate levels significantly predicted 90-day mortality; in contrast, the lactate value did not predict 28- or 90-day mortality in patients within the non-DIC group. Further studies are warranted to investigate the effect of lactate on mortality in patients with sepsis.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Change history
12 August 2019
An error occurred during the publication of a number of articles in Journal of Intensive Care. Several articles were published in volume 7 with a duplicate citation number.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- CI:
-
Confidence interval
- DIC:
-
Disseminated intravascular coagulation
- ICU:
-
Intensive care unit
- JAAM-DIC:
-
Japanese Association for Acute Medicine—disseminated intravascular coagulation
- NET:
-
Neutrophil extracellular trap
- OR:
-
Odds ratio
- SIRS:
-
Systemic inflammatory response syndrome
- SOFA:
-
Sequential (sepsis-related) Organ Failure Assessment
References
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10.
Prescott HC, Angus DC. Enhancing recovery from sepsis: a review. JAMA. 2018;319:62–75.
Levy MM, Rhodes A, Phillips GS, Townsend SR, Schorr CA, Beale R, et al. Surviving Sepsis Campaign: association between performance metrics and outcomes in a 7.5-year study. Intensive Care Med. 2014;40:1623–33.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801–10.
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26:1793–800.
Cecconi M, Evans L, Levy M, Rhodes A. Sepsis and septic shock. Lancet. 2018;392:75–87.
Gando S, Iba T, Eguchi Y, Ohtomo Y, Okamoto K, Koseki K, et al. A multicenter, prospective validation of disseminated intravascular coagulation diagnostic criteria for critically ill patients: comparing current criteria. Crit Care Med. 2006;34:625–31.
Gando S, Saitoh D, Ogura H, Fujishima S, Mayumi T, Araki T, et al. A multicenter, prospective validation study of the Japanese Association for Acute Medicine disseminated intravascular coagulation scoring system in patients with severe sepsis. Crit Care. 2013;17:R111.
Esmon CT. Inflammation and thrombosis. J Thromb Haemost. 2003;1:1343–8.
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:762–74.
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864–74.
Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M, Fuchs BD, Shah CV, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009;37:1670–7.
Nishikimi M, Ogura T, Nishida K, Takahashi K, Fukaya K, Liu K, et al. Differential effect of mild therapeutic hypothermia depending on the findings of hypoxic encephalopathy on early CT images in patients with post cardiac arrest syndrome. Resuscitation. 2018;128:11–5.
Kanda Y. Investigation of the freely available easy-to use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann, Weiss DS, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303:1532–5.
Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol. 2013;13:34–45.
Ito T. PAMPs and DAMPs as triggers for DIC. J Intensive Care. 2014;2:67.
Clark SR, Ma AC, Tavener SA, McDonald B, Goodarzi Z, Kelly MM, et al. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nat Med. 2007;13:463–9.
McDonald B, Davis RP, Kim SJ, Tse M, Esmon CT, Kolaczkowska E, et al. Platelets and neutrophil extracellular traps collaborate to promote intravascular coagulation during sepsis in mice. Blood. 2017;129:1357–67.
Moll S, Lindley C, Pescatore S, Morrison D, Tsuruta K, Mohri M, et al. Phase I study of a novel recombinant human soluble thrombomodulin, ART-123. J Thromb Haemost. 2004;2:1745–51.
Vincent JL, Ramesh MK, Ernest D, LaRosa SP, Pachl J, Aikawa N, et al. A randomized, double-blind, placebo-controlled, phase 2b study to evaluate the safety and efficacy of recombinant human soluble thrombomodulin, ART–123, in patients with sepsis and suspected disseminated intravascular coagulation. Crit Care Med. 2013;41:2069–79.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
DH and ON were responsible for the conception of the article and drafted and revised the manuscript. YH, TK, and DN helped gather the clinical data and draft the manuscript. KN helped develop the study design. KM, YS, and HK helped draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hasegawa, D., Nishida, K., Hara, Y. et al. Differential effect of lactate in predicting mortality in septic patients with or without disseminated intravascular coagulation: a multicenter, retrospective, observational study. j intensive care 7, 35 (2019). https://doi.org/10.1186/s40560-019-0389-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-019-0389-x