Abstract
The prognostic impact of TERT mutations has been controversial in IDH-wild tumors, particularly in glioblastomas (GBM). The controversy may be attributable to presence of potential confounding factors such as MGMT methylation status or patients’ treatment. This study aimed to evaluate the impact of TERT status on patient outcome in association with various factors in a large series of adult diffuse gliomas. We analyzed a total of 951 adult diffuse gliomas from two cohorts (Cohort 1, n = 758; Cohort 2, n = 193) for IDH1/2, 1p/19q, and TERT promoter status. The combined IDH/TERT classification divided Cohort 1 into four molecular groups with distinct outcomes. The overall survival (OS) was the shortest in IDH wild-type/TERT mutated groups, which mostly consisted of GBMs (P < 0.0001). To investigate the association between TERT mutations and MGMT methylation on survival of patients with GBM, samples from a combined cohort of 453 IDH-wild-type GBM cases treated with radiation and temozolomide were analyzed. A multivariate Cox regression model revealed that the interaction between TERT and MGMT was significant for OS (P = 0.0064). Compared with TERT mutant-MGMT unmethylated GBMs, the hazard ratio (HR) for OS incorporating the interaction was the lowest in the TERT mutant-MGMT methylated GBM (HR, 0.266), followed by the TERT wild-type-MGMT methylated (HR, 0.317) and the TERT wild-type-MGMT unmethylated GBMs (HR, 0.542). Thus, patients with TERT mutant-MGMT unmethylated GBM have the poorest prognosis. Our findings suggest that a combination of IDH, TERT, and MGMT refines the classification of grade II-IV diffuse gliomas.
Similar content being viewed by others
Introduction
Extensive genomic analyses have recently revealed that the biology of brain tumors, therefore patients’ clinical outcomes, is often determined by combinations of specific genetic and/or epigenetic alterations. The latest edition of the World Health Organization (WHO) Classification of Tumours of the Central Nervous System (revised 4th edition) incorporated molecular classification as a part of the integrated diagnosis, adding this to conventional histopathology and WHO grading [19]. This is a highly significant step in the diagnostic pathology, considering that the conventional histopathological diagnosis may suffer from morphological ambiguity and inter-observer discordance, most typically exemplified by oligoastrocytoma [33]. For molecular classification to best help standardize diagnoses, it is critical to test the efficacy of molecular markers to define specific entities.
Diffuse astrocytoma (DA) and anaplastic astrocytoma (AA) are best characterized by the presence of IDH1/IDH2 mutations (“IDH mutation”), most often (but not always) accompanied by mutations in TP53 and ATRX [12, 17, 31]. It has been suggested that the IDH mutation is a founder mutation that precedes TP53 and ATRX mutations [31]. The presence of IDH mutation is associated with significantly longer overall survival in astrocytoma patients diagnosed, according to the WHO 2007 Classification [11, 36]. Oligodendroglioma is defined by the concurrent deletions of entire 1p/19q (“1p/19q codeletion”), which is invariably accompanied by IDH mutation. The 1p/19q codeletion is caused by an unbalanced t(1;19)(q10;p10) translocation resulting in total loss of one copy of 1p and 19q [8]. Mutations of FUBP1 (1p31.1) and/or CIC (19q13.2) are found in 52–66 % of oligodendrogliomas [4, 12]. The spatial/temporal distribution of FUBP1/CIC mutations may be heterogeneous, whereas the 1p/19q codeletion is homogeneously found within the tumor tissue [31], and a considerable number of 1p/19q codeleted tumors have no mutations to FUBP1/CIC [31]. Thus, astrocytomas and oligodendrogliomas will be diagnosed based on molecular characterization of the IDH and 1p/19q statuses; diffuse astrocytomas are defined by the presence of IDH1/IDH2 mutations without 1p/19q codeletion, whereas the diagnosis of oligodendrogliomas requires the presence of both IDH mutation and 1p/19q codeletion. Molecular classification of IDH-wildtype gliomas is somewhat elusive. The great majority of primary GBMs are IDH wild-type. It has been suggested that most astrocytomas with wild-type IDH may resolve into other tumor entities, mostly glioblastomas (GBMs) [28]. For better definition of GBMs in IDH-wild-type tumors, further classification of molecular markers is needed.
TERT promoter mutations are very common in GBMs and oligodendroglial tumors [1, 14]. Mutations occur at either of the two hotspots (conventionally referred to as C228T and C250T for their chromosomal coordinates in the hg19 assembly) in a mutually exclusive manner. The mutations create de novo GA Binding Protein Transcription Factor Alpha Subunit (GABPA) binding sites [3], causing an increase in TERT mRNA transcription in GBM [1, 3], a mechanism that would lead to telomerase upregulation and telomere elongation. The TERT promoter mutations almost always coincide with IDH mutations and 1p/19q codeletion in oligodendrogliomas, whereas a combination of TERT mutation and wild-type IDH is the most common genotype observed in GBM. These findings suggest that the combination of IDH and TERT mutations may be useful to define glioma subclasses. The prognostic impact of TERT mutation in diffuse gliomas appears to be bivalent, unlike IDH mutation or 1p/19q codeletion. Concurrent mutations of TERT and IDH predict good prognosis, as an alternative hallmark of oligodendroglioma, whereas TERT promoter mutation with wild-type IDH tends to be associated with poor prognosis, although its use in predicting outcomes in GBM is controversial [1, 6, 13, 15, 26, 30]. One of the potential confounding factors in the prognostication of GBM is the methylation status of the MGMT promoter. MGMT promoter methylation (“MGMT methylation”) is a well-established prognostic marker for primary GBM and a predictive marker for the response to temozolomide in elderly GBM [9, 22, 34].
In this study, we examined the utility of molecular classification based on the IDH and TERT statuses to predict clinical courses of patients in association with various clinical factors, histological diagnosis, and grading in a large series of newly diagnosed WHO grade II-IV adult gliomas. We specifically focused on the potential interaction between MGMT promoter methylation and TERT mutational statuses to further refine the clinical value of molecular diagnosis. We found that TERT mutation identifies a subset of GBM patients who are most resistant to the conventional radiochemotherapy when MGMT is unmethylated.
Materials and methods
Patient selection
Two cohorts were collected in this study. Cohort 1 was formed to evaluate the prognostic impact of molecular classification based on IDH and TERT statuses in adult diffuse gliomas. The inclusion criteria for the Cohort 1 were as follows: 18 years of age or older, histological diagnosis of grade II-IV diffuse glioma originating in the cranium, genomic DNA available for molecular analysis (extracted from frozen tumor tissues taken at the time of the initial surgery), and clinical data available for survival analysis. Out of 881 cases initially collected from 13 institutions in Japan, 758 cases met the criteria and enrolled in the study as Cohort 1 (the diagram of case selection is shown in Fig. 1). To further analyze the impact of TERT promoter mutation and MGMT methylation status on survival, Cohort 2 was collected as an independent set of locally diagnosed GBM. The inclusion criteria for the Cohort 2 were: 18 years of age or older, histological diagnosis of GBM, treatment with local irradiation of 50 – 65 Gy and concurrent chemotherapy with temozolomide after initial surgery, absence of clinically apparent preceding lower grade gliomas, no IDH1/2 mutations, clinical data available for survival analysis, and genomic DNA available for molecular analysis (extracted from frozen tissues taken at the time of the initial surgery). Out of 218 cases collected from four institutions in Japan, 193 cases met the criteria described above and were enrolled in Cohort 2. Clinical data collected from each institution included the detailed information as follows: age, sex, preoperative Karnofsky Performance status (KPS), extent of resection, radiation dose, and chemotherapeutic regimen in initial treatment. The study was approved by the Institutional Review Board (IRB) at National Cancer Center (No. 2013–042) and the corresponding local IRB of the participating centers.
Flowchart of patient selection. For Cohort 1, 758 out of 881 Grade II-IV cases collected met the eligibility criteria and were analyzed for the prognostic impact of IDH and TERT status in adult diffuse gliomas. From Cohort 1, 260 GBM patients concurrently treated with TMZ and RT were further selected (Cohort 1 GBM). For Cohort 2, 193 IDH wild-type GBM cases treated with TMZ plus RT were selected (Cohort 2 GBM). Cohort 1 GBM and Cohort 2 GBM were analyzed for the influences of TERT and MGMT status on survival. GBM, glioblastoma; NF, neurofibromatosis; RT, radiation therapy; TMZ, temozolomide
Central pathology review
All cases of Cohort 1 were subjected to central pathology review by three senior neuropathologists (T.K., M.S., and H.S.). Histological diagnosis was made as a consensus of the 3 pathologists based on the fourth edition of WHO Classification (WHO 2007) [18]. Although the cases of the Cohort 2 were not subjected to these review procedures, the local diagnoses were based on the WHO 2007 criteria, similar to Cohort 1.
Molecular analysis
Tumor DNA was extracted from frozen tumor tissues for all cases using a DNeasy Blood & Tissue Kit (Qiagen, Tokyo, Japan). The details of genetic analysis, including PCR and sequencing for each gene status, are described in the Additional file 1: Supplementary materials. The presence of hotspot mutations in IDH1 (R132) and IDH2 (R172) was assessed by pyrosequencing for all cases included in this study, as previously reported [2]. The two mutation hotspots in the TERT promoter were analyzed in all tumors by Sanger sequencing and/or pyrosequencing, as previously reported [1]. The mutation hotspots at codons 27 and 34 of H3F3A and at codon 600 of BRAF were analyzed by Sanger sequencing and/or pyrosequencing. The copy number statuses of 1p and 19q were determined by multiplex ligation-dependent probe amplification (MLPA), Microarray-based comparative genomic hybridization (aCGH) or microsatellite analysis [1, 24, 32]. The copy number status of CDKN2A was also assessed using MLPA or aCGH [1]. The methylation status of the MGMT promoter was analyzed by pyrosequencing after bisulfite modification of genomic DNA extracted from tumor specimens as described [25], with some modifications in the thermal cycling conditions. Based on an outcome-based study to determine an optimal cutoff to judge MGMT promoter methylation in a series of 276 newly diagnosed GBMs, we used a cut-off of ≥ 16 % for MGMT methylation. The details of this study will be described elsewhere (Ichimura, manuscript in preparation).
Statistical analysis
Statistical analysis was performed using an SAS package and JMP version 10 (SAS Institute, Cary, NC, USA). Categorized data were compared between subgroups using the chi-square test. The comparison for age distribution was examined with the Student’s t test. The survival data were analyzed with the log-rank test and univariate and multivariate Cox regression analyses. Stepwise procedure was used in multivariate Cox regression. In multivariate Cox proportional hazard models for GBM cases including TERT and MGMT, a term of interaction between them was also incorporated. A P-value < 0.05 was considered significant in statistical analyses.
Results
Molecular classification based on IDH and TERT defines distinct subgroups of adult gliomas in Cohort 1
All 758 tumor samples from Cohort 1 were screened for mutations in IDH1/2 and TERT hotspots and the copy number status of 1p/19q. The data were determined for all cases but one, in which the 1p/19q status was not determined. The frequencies of each molecular status for each histology are shown in Table 1. The molecular status, patient background, and clinical information for each case are provided in Additional file 2: Table S1. IDH1/2 mutations were present in 38 % of tumors, mostly a c.395G > A transition in IDH1 (R132H; 274/286, 96 %). TERT promoter mutations were observed in 51 % (390/758) of tumors. IDH1/2 mutations were common in grade II-III gliomas (38–96 %), whereas TERT promoter mutations were frequently observed in oligodendrogliomas (74–83 %) and GBMs (58 %).
The combined IDH/TERT classification divided the Cohort 1 into four molecular groups, each showing distinct patient characteristics, histology, or clinical outcome. The patient backgrounds and molecular status of each group are summarized in Table 2 and Fig. 2. The group with mutations in both IDH and TERT (Group A) mainly consisted of oligodendrogliomas or oligoastrocytomas (82 %). The group with mutation in IDH but not TERT (Group B) mostly consisted of astrocytomas and grade II-III oligoastrocytomas. The group with no detectable IDH or TERT hotspot mutations (Group C) included all types of histology, GBM being the most common (57 %). Tumors exhibiting TERT mutation with wild-type IDH (Group D) were mostly GBMs (79 %) or AAs (12 %).
A diagram of molecular classification of Cohort 1. All 758 tumors in Cohort 1 are sorted according to their molecular classification based on their IDH and TERT statuses. The mutation statuses of IDH, TERT, H3F3A, the copy number statuses of 1p/19q and CDKN2A/B BRAF, and MGMT methylation are shown. Centrally reviewed histology is indicated at the bottom. Gray or colored cells indicate absence or presence of alterations, respectively. Blank cells denote no data. Group A, IDH mutated-TERT mutated; Group B, IDH mutated-TERT wild-type; Group C, IDH wild-type-TERT wild-type; Group D, IDH mutated-TERT mutated. AA, anaplastic astrocytoma; AO, anaplastic oligodendroglioma; AOA, anaplastic oligoastrocytoma; DA, diffuse astrocytoma; Del, Deletion; GBM, glioblastoma; OA, oligoastrocytoma; OL, oligodendroglioma
There was a significant difference in overall survival (OS) and progression-free survival (PFS) between each group (p < 0.0001, Log-rank test; Fig. 3). Group A showed the most favorable prognosis (median OS, not reached; median PFS, 113.4 months), followed by group B (median OS, not reached; median PFS, 66.5 months). Group D showed significantly shorter OS or PFS than any other group. Multivariate analysis using Cox regression models including clinicopathological information also revealed the significant prognostic impact of molecular classification, histological diagnosis, age, sex, and surgery (Table 3).
Kaplan-Meier analysis of progression free survival (PFS) and overall survival (OS) of molecular groups in Cohort 1. a. PFS of each molecular group (n = 734). Median PFS was 113.4 months for Group A, 66.5 months for Group B, 11.7 months for Group C, and 8.2 months for Group D (P < 0.0001, Log-rank test). Notably, Group D showed significantly shorter PFS than other groups (P < 0.0001, Log-rank test). b. OS of each molecular group (n = 758). Median OS was not reached for Groups A and B, 25.3 months for Group C, and 16.3 months for Group D (P < 0.0001, Log-rank test). Group D showed significantly shorter survival than any other groups (P < 0.0001, Log-rank test). Group A, IDH mutated- TERT mutated; Group B, IDH mutated-TERT wild-type; Group C, IDH wild-type-TERT wild-type; Group D, IDH mutated-TERT mutated
The molecular groups were also associated with patient age, spatial distribution, and other specific genetic profiles. The IDH-mutated groups (Groups A and B) comprised younger patients than the IDH wild-type groups (Groups C and D; 43.3 vs. 60.0 years, respectively; p < 0.0001, Student’s t-test). Among the IDH-wild-type groups, Group C patients were younger than those in Group D (56.7 vs. 63.4 years, respectively; p < 0.0001, Student’s t-test). Tumors in the IDH-mutant groups commonly involved the frontal lobe. Thalamic or infratentorial tumors were the most common in Group C (72 and 85 %, respectively). The great majority of the Group A tumors showed 1p19q codeletion (93 %). Among the IDH-wild-type tumors, mutations in H3F3A or HIST1H3B (“histone H3 mutations”) were mostly observed in Group C. Deletion of CDKN2A was predominantly observed in IDH-wild-type groups (Groups C and D). The frequency of TERT mutation-type (C250T or C228T) did not differ between Group A and Group D (p = 0.11, chi-square test).
Multivariate Cox regression models revealed differences in prognostic impact of WHO grade among molecular groups
We performed Cox regression analysis in each group to investigate whether the molecular groups are prognostic markers independent of the histological diagnosis. In Group A, only the patients’ clinical backgrounds (age, KPS, and surgical history) were associated with overall survival after multivariate analysis, suggesting that this group was homogeneous regardless of the WHO grade (Additional file 2: Table S3). The 1p19q status was not significantly associated with survival by univariate Cox regression analysis, although the number of 1p19q intact tumors (n = 11/155) was too small for statistically conclusive results (Additional file 2: Table S3; Additional file 3: Figure S2). On the other hand, the WHO grade (II or III) was associated with OS and PFS in both univariate and multivariate analysis for Group B (Additional file 2: Table S4). In Group C, the WHO grade was significantly associated with OS and PFS in univariate analysis, whereas it was not prognostic in multivariate analysis (Additional file 2: Table S5). The WHO grade did not have significant impact on OS in both univariate and multivariate analysis for Group D (Additional file 2: Table S6). Collectively, the impact of WHO grade differed according to the molecular groups.
Interaction between TERT and MGMT in IDH-wild-type GBM
To investigate the impact of the TERT mutations and MGMT methylation in IDH-wild-type GBMs, we selected IDH-wild-type GBM cases from Cohort 1 who received concurrent temozolomide and radiation therapy with a dose of 50 – 65 Gy, and whose clinical information and MGMT status were available. In total, 260 GBM cases met these criteria (“Cohort 1 GBM”) and were further analyzed (Fig. 1).
In univariate analysis of Cohort 1 GBM, the TERT mutation status was not associated with either OS or PFS, whereas the MGMT methylation status was strongly associated with longer survival (Additional file 2: Table S7a). However, multivariate analysis revealed that TERT mutation was associated with OS and PFS. The discordance in these results suggested that the prognostic impact of TERT mutation may be affected by other factors. We next performed a multivariate Cox regression analysis incorporating TERT and MGMT interaction. This analysis revealed a significant interaction between TERT and MGMT for both OS and PFS (P = 0.0002 and 0.0342, respectively; Additional file 2: Table S7b). When compared with the TERT mutated-MGMT unmethylated group, the hazard ratio (HR) for OS incorporating the interaction was the lowest in the TERT mutated/MGMT methylated group (HR, 0.186), then the TERT wild-type/MGMT methylated group (HR, 0.392), finally the TERT wild-type/MGMT unmethylated group (HR, 0.476).
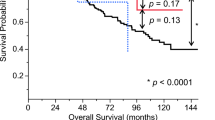
To validate the findings in a larger series, we collected an independent cohort of 193 GBM cases as Cohort 2 (Fig. 1). This cohort was selected using the same criteria as the Cohort 1 GBMs (see above and Fig. 1), except that local histological diagnosis was employed. The frequency of TERT promoter mutations in Cohort 2 (60 %) was comparable to the GBMs from Cohort 1. The Cohort 1 and Cohort 2 GBMs were then combined and analyzed (Table 4). When stratified by TERT and MGMT statuses, their association with OS and PFS were as follows: 1) In the patients with MGMT methylated tumors, TERT status was not associated with either OS or PFS (P > 0.05, Log-rank test) 2) In the patients with MGMT unmethylated tumors, those with TERT mutant tumors showed shorter OS and PFS than those with TERT wild-type tumors (P < 0.05, Log-rank test); 3) lack of MGMT promoter methylation was associated with shorter OS and PFS in both TERT wild-type (Group C GBM) and TERT mutant (Group D GBM) groups (P < 0.05, Log-rank test; Fig. 4). As a result, patients with the TERT mutated-MGMT unmethylated GBMs had the shortest survival (median OS, 14.6 months), whereas those with TERT mutated-MGMT methylated GBMs survived the longest (median OS, 30.0 months).
Kaplan-Meier analysis for survival, stratified by TERT and MGMT statuses in 453 GBM cases treated with radiation plus temozolomide. a. PFS of GBM cases (see text for definition). Median PFS was 14.5 months for TERT mutated-MGMT methylated (Mut/Met), 12.8 months for TERT wild-type-MGMT methylated (WT/Met), 9.8 months for TERT wild-type-MGMT unmethylated (WT/Un-met), and 7.2 months for TERT mutated-MGMT unmethylated (Mut/Un-met) (P < 0.0001, Log-rank test). The Mut/Un-met group showed shorter PFS than WT/Un-met (P = 0.0003, Log-rank test), whereas the differences in PFS between the MGMT methylated groups (between Mut/Met and WT/Met) was not significant (P = 0.62, Log-rank test). b. OS of the GBM cases. Median OS was 30.0 months for Mut/Met, 26.5 months for WT/Met, 18.8 months for WT/Un-met, and 14.6 months for Mut/Un-met (P < 0.0001, Log-rank test). The Mut/Un-met group had shorter OS than WT/Un-met (P < 0.0001, Log-rank test), whereas the difference in OS between Mut/Met and WT/Met was not significant (P = 0.83, Log-rank test). GBM, glioblastoma; OS, overall survival; PFS, progression free survival
A multivariate Cox regression model incorporating age, gender, cohort, KPS, tumor location, surgical history, TERT, and MGMT revealed that the interaction between TERT and MGMT was significant for OS in the combined GBM cohort of 453 cases. Against a reference of the TERT mutant-MGMT unmethylated GBMs, the HR for OS incorporating the interaction was the lowest in the TERT mutant-MGMT methylated GBM (HR, 0.266), followed by the TERT wild-type-MGMT methylated (HR, 0.317), and the TERT wild-type-MGMT unmethylated GBMs (HR, 0.542). For PFS, TERT and MGMT independently influenced survival (Table 5).
When Cohort 2 was analyzed separately, univariate and multivariate Cox regression analysis for OS and PFS showed that the TERT and MGMT statuses were independent prognostic factors. Interaction between TERT and MGMT was not statistically significant in this cohort (Additional file 2: Table S8).
Discussion and conclusions
In this study, we investigated the efficacy of TERT promoter mutation as a diagnostic and/or prognostic marker in combination with IDH mutation and MGMT methylation in a large series of newly diagnosed adult gliomas with detailed clinical information and a relatively homogeneous background, including postoperative treatment, in particular for GBM. Our results indicated that molecular classification based on the IDH and TERT statuses defines four groups within adult diffuse gliomas of grade II-IV, each showing distinct clinical-pathological features such as histological type, age, or tumor location. TERT promoter mutation was a favorable prognostic factor in IDH mutated tumors, whereas it was an unfavorable prognostic factor in IDH wild-type tumors. The most striking finding was that the prognostic impact of TERT promoter mutation may depend not only on the IDH status but also on the MGMT methylation status.
The prognostic value of TERT mutation in GBMs has been controversial. Some have suggested that TERT status did not have an impact on OS in IDH wild-type GBMs after adjusting by age and gender [6, 26], whereas others found an adverse prognostic impact of TERT mutation by multivariate analysis including treatment [16, 30]. This discrepancy may be due to insufficient cohort size or uneven treatment in some of the cohorts. Clinical background may also be a confounding factor. For example, TERT mutation is strongly associated with higher age, which in itself is a well-known prognostic factor and affects treatment choice. In the present study, the prognostic impact of TERT was validated in two independent cohorts of GBMs with similar clinical backgrounds in which molecular tests were thoroughly performed.
A potentially more significant possibility is the presence of additional confounding factors that influence survival of GBM patients in association with the TERT status. MGMT methylation is a well-established favorable prognostic marker for survival in GBM patients, and predicts the response to temozolomide in elderly GBM patients [9, 22, 34]. We therefore investigated the potential interaction between TERT mutation and MGMT methylation status in newly diagnosed GBM patients who received a standard treatment with concomitant temozolomide and radiation therapy in Cohort 1 as well as the combined GBM cohort. Our results indicate that the prognostic impact of TERT mutation is strongly influenced by the MGMT methylation status. The limitation of this study is that the interaction was validated in the combined cohort but not in the Cohort 2 alone, most likely because of the insufficient cohort size. A further validation in a larger cohort is warranted.
Our finding that the subset of GBMs defined as having TERT mutation and unmethylated MGMT have the poorest prognosis has important clinical implications. Our results conclusively demonstrated that TERT mutation is one of the most powerful predictors of survival in GBM patients, along with the MGMT methylation status. It has been shown that temozolomide is effective for GBM with methylated MGMT. Patients with MGMT unmethylated GBM who receive only minimal benefit from current standard treatments including temozolomide are the primary population who require new therapeutic agents [10]. TERT may thus serve as an alternative therapeutic target for these patients.
Currently, Imetelstat is the only telomerase inhibitor that has been tested in clinical trials [23]. Imetelstat is an oligonucleotide inhibitor to TERC, an RNA subunit of telomerase, but not a direct inhibitor of TERT. Clinical anti-oncogenic activity of Imetelstat has yet to be demonstrated. In addition to its activity as the reverse transcriptase for telomerase, TERT is reported to have activity as an RNA-dependent RNA polymerase (RdRP) [20]. RdRP plays an essential role in RNA silencing by generating double-stranded RNAs, which are processed into microRNAs [20, 21]. It has been suggested that TERT is involved in diverse cellular functions, such as heterochromatin formation or maintenance of tumor-initiating cells through its RdRP activity. Recently, a specific inhibitor for RdRP that suppresses growth of platinum-resistant ovarian cancer cell lines with TERT mutation and upregulation has been proposed [35]. A pre-clinical study in GBM is underway (Takahashi, in preparation).
The biological mechanism for the interaction between TERT mutation and MGMT methylation that influences patient survival is currently unclear. A broad spectrum of the biological consequences of TERT activation, for example by microRNAs generated through TERT-RdRP, may affect the response to chemotherapy and/or radiotherapy.
One of the major challenges of the integrated diagnosis system for adult gliomas is whether histological diagnosis or WHO grading still have survival impact after stratification by molecular information. In our study, a multivariate analysis revealed that the histological diagnosis continues to be a significant predictor of survival. We further investigated the prognostic value of histological diagnosis in relation to clinical information in each subgroup.
We found that the WHO grade had no significant impact on OS in either Groups A or D, suggesting that each of these groups may be regarded as clinically homogeneous (Additional file 2: Table S10). Virtually all tumors allocated to Group A are molecularly scored as oligodendroglial tumors, because the great majority of them presented total 1p19q codeletion. There remains a controversy whether or not TERT-IDH co-mutated, but not 1p19q codeleted, tumors are oligodendrogliomas. Along with a large-scale analysis reported by Eckel-Passow et al. [6], those paradoxical cases showed prognosis comparable to the codeleted tumors, suggesting that those tumors could be regarded as oligodendrogliomas. Group D tumors showed universally dismal prognosis regardless of the histological subtype, indicating that this group is biologically bona fide GBM and that grade II-III tumors in this group should be regarded as under-diagnosed GBM.
On the other hand, a univariate analysis identified WHO grade as a factor significantly associated with survival in Group B (IDH mutated-TERT wild-type, representing astrocytomas), and a multivariate analysis for survival in Group B also identified WHO grade (II or III) as a prognostic factor in the present study. These results are in contrast to recent reports that found no survival impact of WHO grade in IDH mutated astrocytomas [27, 29]; however, it supports the results of another study [6]. So far, there are no molecular markers that define WHO grades. Our results and others, however, suggest that WHO grade may still be relevant in some types of gliomas. The limitation of these studies is that the treatment of low-grade astrocytomas may be inconsistent and have potentially confounded the results. A prospective study with homogeneously treated patients in clinical trials would be needed to clarify the significance of WHO grade in the era of molecular diagnostics.
The Group C remains enigmatic. This triple negative group has highly heterogeneous backgrounds, including histological diagnosis, tumor location, and other genetic traits. This group mainly consists of adult GBMs, however it also contains pediatric types of GBM that harbor H3F3A mutations and indolent tumors resembling pediatric lower grade gliomas with BRAF mutations. A large scale analysis based on genome-wide methylation analysis identified tumors exhibiting methylation profiles similar to pilocytic astrocytomas, as well as tumors resembling pediatric GBMs in the IDH wild-type group [5]. Although WHO grade II and III tumors in Group C showed slightly better outcomes compared with the grade IV counterparts, the prognoses of the grade IV tumors in Group C were comparable with Group D. This shows that at least histologically proven GBMs in Group C are clinically relevant GBMs. The question remains whether the triple negative grade II-III tumors are biologically under-diagnosed GBMs, or if at least some of them form a separate sub-entity of genuine “Diffuse (Anaplastic) astrocytoma, IDH wild-type” tumors with an intermediate prognosis between those with IDH mutations and GBM. Further studies to establish molecular markers that unequivocally define GBM (e.g., EGFR amplification, monosomy 10/trisomy 7, or co-gain of chromosomes 19/20 [7, 28]) on a larger collection of the triple negative/Group C tumors are warranted.
In this study, using a large cohort of newly diagnosed adult gliomas with precise clinical information, we demonstrated that molecular classification using IDH and TERT statuses is a strong prognostic marker of adult gliomas. The IDH-TERT classification efficiently identifies molecularly defined oligodendrogliomas and astrocytomas equivalent to the IDH-1p/19q-based classification. Although an accurate determination of total 1p/19q codeletion may require laborious and expensive molecular tests, examination of two hotspots in the TERT promoter is comparatively simple. Moreover, we found that a combination of TERT mutation and the MGMT methylation status classified GBMs into clinically relevant subgroups, identifying TERT mutated-MGMT unmethylated tumors as having the most severe outcome, and thus highlighting TERT as a primary target for novel therapies. Thus, by using TERT mutation as an additional biomarker, the molecular classification presented in this study will refine the integrated diagnostic system and prognostication of glioma patients. Our results emphasize the importance of combining molecular markers such as IDH, 1p/19q, TERT, and MGMT for accurate molecular diagnosis, prognostication, and the choice of treatment in clinical trials, as well as in routine clinical practice for glioma patients.
References
Arita H, Narita Y, Fukushima S, Tateishi K, Matsushita Y, Yoshida A, Miyakita Y, Ohno M, Collins VP, Kawahara N, Shibui S, Ichimura K. Upregulating mutations in the TERT promoter commonly occur in adult malignant gliomas and are strongly associated with total 1p19q loss. Acta Neuropathol. 2013;126:267–76.
Arita H, Narita Y, Matsushita Y, Fukushima S, Yoshida A, Takami H, Miyakita Y, Ohno M, Shibui S, Ichimura K. Development of a robust and sensitive pyrosequencing assay for the detection of IDH1/2 mutations in gliomas. Brain Tumor Pathol. 2015;32:22–30.
Bell RJ, Rube HT, Kreig A, Mancini A, Fouse SD, Nagarajan RP, Choi S, Hong C, He D, Pekmezci M, Wiencke JK, Wrensch MR, Chang SM, Walsh KM, Myong S, Song JS, Costello JF. Cancer. The transcription factor GABP selectively binds and activates the mutant TERT promoter in cancer. Science. 2015;348:1036–9.
Bettegowda C, Agrawal N, Jiao Y, Sausen M, Wood LD, Hruban RH, Rodriguez FJ, Cahill DP, McLendon R, Riggins G, Velculescu VE, Oba-Shinjo SM, Marie SK, Vogelstein B, Bigner D, Yan H, Papadopoulos N, Kinzler KW. Mutations in CIC and FUBP1 contribute to human oligodendroglioma. Science. 2011;333:1453–5.
Ceccarelli M, Barthel FP, Malta TM, Sabedot TS, Salama SR, Murray BA, Morozova O, Newton Y, Radenbaugh A, Pagnotta SM, Anjum S, Wang J, Manyam G, Zoppoli P, Ling S, Rao AA, Grifford M, Cherniack AD, Zhang H, Poisson L, Carlotti Jr CG, Tirapelli DP, Rao A, Mikkelsen T, Lau CC, Yung WK, Rabadan R, Huse J, Brat DJ, Lehman NL, Barnholtz-Sloan JS, Zheng S, Hess K, Rao G, Meyerson M, Beroukhim R, Cooper L, Akbani R, Wrensch M, Haussler D, Aldape KD, Laird PW, Gutmann DH, Network TR, Noushmehr H, Iavarone A, Verhaak RG. Molecular Profiling Reveals Biologically Discrete Subsets and Pathways of Progression in Diffuse Glioma. Cell. 2016;164:550–63.
Eckel-Passow JE, Lachance DH, Molinaro AM, Walsh KM, Decker PA, Sicotte H, Pekmezci M, Rice T, Kosel ML, Smirnov IV, Sarkar G, Caron AA, Kollmeyer TM, Praska CE, Chada AR, Halder C, Hansen HM, McCoy LS, Bracci PM, Marshall R, Zheng S, Reis GF, Pico AR, O'Neill BP, Buckner JC, Giannini C, Huse JT, Perry A, Tihan T, Berger MS, Chang SM, Prados MD, Wiemels J, Wiencke JK, Wrensch MR, Jenkins RB. Glioma Groups Based on 1p/19q, IDH, and TERT Promoter Mutations in Tumors. N Engl J Med. 2015;372:2499–508.
Geisenberger C, Mock A, Warta R, Rapp C, Schwager C, Korshunov A, Nied AK, Capper D, Brors B, Jungk C, Jones D, Collins VP, Ichimura K, Backlund LM, Schnabel E, Mittelbron M, Lahrmann B, Zheng S, Verhaak RG, Grabe N, Pfister SM, Hartmann C, von Deimling A, Debus J, Unterberg A, Abdollahi A, Herold-Mende C. Molecular profiling of long-term survivors identifies a subgroup of glioblastoma characterized by chromosome 19/20 co-gain. Acta Neuropathol. 2015;130:419–34.
Griffin CA, Burger P, Morsberger L, Yonescu R, Swierczynski S, Weingart JD, Murphy KM. Identification of der(1;19)(q10;p10) in five oligodendrogliomas suggests mechanism of concurrent 1p and 19q loss. J Neuropathol Exp Neurol. 2006;65:988–94.
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JE, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352:997–1003.
Hegi ME, Stupp R. Withholding temozolomide in glioblastoma patients with unmethylated MGMT promoter--still a dilemma? Neuro Oncol. 2015;17:1425–7.
Ichimura K, Pearson DM, Kocialkowski S, Backlund LM, Chan R, Jones DT, Collins VP. IDH1 mutations are present in the majority of common adult gliomas but rare in primary glioblastomas. Neuro Oncol. 2009;11:341–7.
Jiao Y, Killela PJ, Reitman ZJ, Rasheed AB, Heaphy CM, de Wilde RF, Rodriguez FJ, Rosemberg S, Oba-Shinjo SM, Nagahashi Marie SK, Bettegowda C, Agrawal N, Lipp E, Pirozzi C, Lopez G, He Y, Friedman H, Friedman AH, Riggins GJ, Holdhoff M, Burger P, McLendon R, Bigner DD, Vogelstein B, Meeker AK, Kinzler KW, Papadopoulos N, Diaz LA, Frequent YH, ATRX. CIC, and FUBP1 mutations refine the classification of malignant gliomas. Oncotarget. 2012;3:709–22.
Killela PJ, Pirozzi CJ, Healy P, Reitman ZJ, Lipp E, Rasheed BA, Yang R, Diplas BH, Wang Z, Greer PK, Zhu H, Wang CY, Carpenter AB, Friedman H, Friedman AH, Keir ST, He J, He Y, McLendon RE, Herndon 2nd JE, Yan H, Bigner DD. Mutations in IDH1, IDH2, and in the TERT promoter define clinically distinct subgroups of adult malignant gliomas. Oncotarget. 2014;5:1515–25.
Killela PJ, Reitman ZJ, Jiao Y, Bettegowda C, Agrawal N, Diaz Jr LA, Friedman AH, Friedman H, Gallia GL, Giovanella BC, Grollman AP, He TC, He Y, Hruban RH, Jallo GI, Mandahl N, Meeker AK, Mertens F, Netto GJ, Rasheed BA, Riggins GJ, Rosenquist TA, Schiffman M, Shih Ie M, Theodorescu D, Torbenson MS, Velculescu VE, Wang TL, Wentzensen N, Wood LD, Zhang M, McLendon RE, Bigner DD, Kinzler KW, Vogelstein B, Papadopoulos N, Yan H. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc Natl Acad Sci U S A. 2013;110:6021–6.
Labussiere M, Boisselier B, Mokhtari K, Di Stefano AL, Rahimian A, Rossetto M, Ciccarino P, Saulnier O, Paterra R, Marie Y, Finocchiaro G, Sanson M. Combined analysis of TERT, EGFR, and IDH status defines distinct prognostic glioblastoma classes. Neurology. 2014;83:1200–6.
Labussiere M, Di Stefano AL, Gleize V, Boisselier B, Giry M, Mangesius S, Bruno A, Paterra R, Marie Y, Rahimian A, Finocchiaro G, Houlston RS, Hoang-Xuan K, Idbaih A, Delattre JY, Mokhtari K, Sanson M. TERT promoter mutations in gliomas, genetic associations and clinico-pathological correlations. Br J Cancer. 2014;111:2024–32.
Liu XY, Gerges N, Korshunov A, Sabha N, Khuong-Quang DA, Fontebasso AM, Fleming A, Hadjadj D, Schwartzentruber J, Majewski J, Dong Z, Siegel P, Albrecht S, Croul S, Jones DT, Kool M, Tonjes M, Reifenberger G, Faury D, Zadeh G, Pfister S, Jabado N. Frequent ATRX mutations and loss of expression in adult diffuse astrocytic tumors carrying IDH1/IDH2 and TP53 mutations. Acta Neuropathol. 2012;124:615–25.
Louis DN, Ohgaki H, Wiestler O, Cavenee W. World Health Organization histological classification of tumours of the central nervous system. International Agency for Research on Cancer. 2007.
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Ellison DW, Figarella-Branger D, Perry A, Reifenberger G, von Deimling A. World health organization histological classification of tumours of the central nervous system. International Agency for Research on Cancer. 2016.
Maida Y, Yasukawa M, Furuuchi M, Lassmann T, Possemato R, Okamoto N, Kasim V, Hayashizaki Y, Hahn WC, Masutomi K. An RNA-dependent RNA polymerase formed by TERT and the RMRP RNA. Nature. 2009;461:230–5.
Maida Y, Yasukawa M, Masutomi K. De novo RNA synthesis by RNA-dependent RNA polymerase activity of telomerase reverse transcriptase. Mol Cell Biol. 2016;36:1248–59.
Malmstrom A, Gronberg BH, Marosi C, Stupp R, Frappaz D, Schultz H, Abacioglu U, Tavelin B, Lhermitte B, Hegi ME, Rosell J, Henriksson R, Nordic Clinical Brain Tumour Study G. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol. 2012;13:916–26.
Man RJ, Chen LW, Zhu HL. Telomerase inhibitors: a patent review (2010–2015). Expert Opin Ther Pat. 2016;26:679–88.
Mukasa A, Takayanagi S, Saito K, Shibahara J, Tabei Y, Furuya K, Ide T, Narita Y, Nishikawa R, Ueki K, Saito N. Significance of IDH mutations varies with tumor histology, grade, and genetics in Japanese glioma patients. Cancer Sci. 2012;103:587–92.
Mulholland S, Pearson DM, Hamoudi RA, Malley DS, Smith CM, Weaver JM, Jones DT, Kocialkowski S, Backlund LM, Collins VP, Ichimura K. MGMT CpG island is invariably methylated in adult astrocytic and oligodendroglial tumors with IDH1 or IDH2 mutations. Int J Cancer. 2012;131:1104–13.
Nonoguchi N, Ohta T, Oh JE, Kim YH, Kleihues P, Ohgaki H. TERT promoter mutations in primary and secondary glioblastomas. Acta Neuropathol. 2013;126:931–7.
Olar A, Wani KM, Alfaro-Munoz KD, Heathcock LE, van Thuijl HF, Gilbert MR, Armstrong TS, Sulman EP, Cahill DP, Vera-Bolanos E, Yuan Y, Reijneveld JC, Ylstra B, Wesseling P, Aldape KD. IDH mutation status and role of WHO grade and mitotic index in overall survival in grade II-III diffuse gliomas. Acta Neuropathol. 2015;129:585–96.
Reuss DE, Kratz A, Sahm F, Capper D, Schrimpf D, Koelsche C, Hovestadt V, Bewerunge-Hudler M, Jones DT, Schittenhelm J, Mittelbronn M, Rushing E, Simon M, Westphal M, Unterberg A, Platten M, Paulus W, Reifenberger G, Tonn JC, Aldape K, Pfister SM, Korshunov A, Weller M, Herold-Mende C, Wick W, Brandner S, von Deimling A. Adult IDH wild type astrocytomas biologically and clinically resolve into other tumor entities. Acta Neuropathol. 2015;130:407–17.
Reuss DE, Mamatjan Y, Schrimpf D, Capper D, Hovestadt V, Kratz A, Sahm F, Koelsche C, Korshunov A, Olar A, Hartmann C, Reijneveld JC, Wesseling P, Unterberg A, Platten M, Wick W, Herold-Mende C, Aldape K, von Deimling A. IDH mutant diffuse and anaplastic astrocytomas have similar age at presentation and little difference in survival: a grading problem for WHO. Acta Neuropathol. 2015;129:867–73.
Simon M, Hosen I, Gousias K, Rachakonda S, Heidenreich B, Gessi M, Schramm J, Hemminki K, Waha A, Kumar R. TERT promoter mutations: a novel independent prognostic factor in primary glioblastomas. Neuro Oncol. 2015;17:45–52.
Suzuki H, Aoki K, Chiba K, Sato Y, Shiozawa Y, Shiraishi Y, Shimamura T, Niida A, Motomura K, Ohka F, Yamamoto T, Tanahashi K, Ranjit M, Wakabayashi T, Yoshizato T, Kataoka K, Yoshida K, Nagata Y, Sato-Otsubo A, Tanaka H, Sanada M, Kondo Y, Nakamura H, Mizoguchi M, Abe T, Muragaki Y, Watanabe R, Ito I, Miyano S, Natsume A, Ogawa S. Mutational landscape and clonal architecture in grade II and III gliomas. Nat Genet. 2015;47:458–68.
Ueki K, Nishikawa R, Nakazato Y, Hirose T, Hirato J, Funada N, Fujimaki T, Hojo S, Kubo O, Ide T, Usui M, Ochiai C, Ito S, Takahashi H, Mukasa A, Asai A, Kirino T. Correlation of histology and molecular genetic analysis of 1p, 19q, 10q, TP53, EGFR, CDK4, and CDKN2A in 91 astrocytic and oligodendroglial tumors. Clin Cancer Res. 2002;8:196–201.
van den Bent MJ. Interobserver variation of the histopathological diagnosis in clinical trials on glioma: a clinician's perspective. Acta Neuropathol. 2010;120:297–304.
Wick W, Platten M, Meisner C, Felsberg J, Tabatabai G, Simon M, Nikkhah G, Papsdorf K, Steinbach JP, Sabel M, Combs SE, Vesper J, Braun C, Meixensberger J, Ketter R, Mayer-Steinacker R, Reifenberger G, Weller M. Society NOASGoN-oWGoGC. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol. 2012;13:707–15.
Yamaguchi S, Maida Y, Yasukawa M, Kato T, Yoshida M, Masutomi K. Eribulin mesylate targets human telomerase reverse transcriptase in ovarian cancer cells. PLoS One. 2014;9:e112438.
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, Kos I, Batinic-Haberle I, Jones S, Riggins GJ, Friedman H, Friedman A, Reardon D, Herndon J, Kinzler KW, Velculescu VE, Vogelstein B, Bigner DD. IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009;360:765–73.
Acknowledgement
The authors thank all clinicians who took care of patients and made a great contribution to this study by providing specimen and clinical information. The authors also thank Ms. Ema Yoshioka and Mr. Daisuke Kanematsu (Institute for Clinical Research, Osaka National Hospital) for the generous assistance in genetic tests. This work was supported partially by JSPS KAKENHI Grant Number 25462283 (K.I.) and 26861171 (H.A.), and the Research award of Osaka Cancer Society (H.A.).
Disclosure
HA received research grant from MSD K.K..
KI received research grant from SRL Inc., EPS and Chugai Pharmaceutical Co.Ltd.
Author information
Authors and Affiliations
Corresponding authors
Additional files
Additional file 1:
Supplementary Information. (DOCX 141 kb)
Additional file 2: Table S1.
Molecular and clinical characteristics of Cohort 1 (n = 758). Table S2. Molecular and clinical characteristics of GBM cohort (n = 453). Table S3. Univariate and multivariate Cox regression analyses for Group A (IDH mutated-TERT mutated) tumors in Cohort 1 (n = 155). Table S4. Univariate and multivariate Cox regression analyses for Group B (IDH mutated-TERT wild-type) tumors in Cohort 1 (n = 131). Table S5. Univariate and multivariate Cox regression analyses for Group C (IDH wild-type-TERT wild-type) tumors in Cohort 1 (n = 237). Table S6. Univariate and multivariate Cox regression analyses for Group D (IDH wild-type-TERT mutated) tumors in Cohort 1 (n = 235). Table S7. Univariate and multivariate Cox regression analyses for GBM in Cohort 1 (n = 260). Table S8. Univariate and multivariate Cox regression analyses for GBM in Cohort 2 (n = 193). Table S9. Background of combined GBM cohort stratified by TERT and MGMT status (n = 453). Table S10. Survival time and WHO grade in each molecular subgroup of Cohort 1 (n = 758). (XLSX 254 kb)
Additional file 3: Figure S1.
Distributions of molecular alterations according to histology in Cohort 1. Figure S2. Kaplan-Meier analysis for Group A cases stratified by 1p/19q status. Figure S3. Kaplan-Meier analyses for GBM cases in Cohorts 1 and 2. (PPTX 172 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Arita, H., Yamasaki, K., Matsushita, Y. et al. A combination of TERT promoter mutation and MGMT methylation status predicts clinically relevant subgroups of newly diagnosed glioblastomas. acta neuropathol commun 4, 79 (2016). https://doi.org/10.1186/s40478-016-0351-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-016-0351-2