Abstract
Background
Gender bias is behavior that shows favoritism towards one gender over another. Microaggressions are defined as subtle, often unconscious, discriminatory, or insulting actions that communicate demeaning or negative attitudes. Our objective was to explore how female otolaryngologists experience gender bias and microaggressions in the workplace.
Methods
Anonymous web-based cross-sectional Canadian survey was distributed to all female otolaryngologists (attendings and trainees) using the Dillman’s Tailored Design Method from July to August of 2021. Quantitative survey included demographic data, validated 44-item Sexist Microaggressions Experiences and Stress Scale (MESS) and validated 10-item General Self-efficacy scale (GSES). Statistical analysis included descriptive and bivariate analysis.
Results
Sixty out of 200 participants (30% response rate) completed the survey (mean age 37 ± 8.3 years, 55.0% white, 41.7% trainee, 50% fellowship-trained, 50% with children, mean 9.2 ± 7.4 years of practice). Participants scored mild to moderate on the Sexist MESS—Frequency (mean ± standard deviation) 55.8 ± 24.2 (42.3% ± 18.3%), Severity 46.0 ± 23.9 (34.8% ± 18.1%), Total 104.5 ± 43.7 (39.6% ± 16.6%) and high on GSES (32.7 ± 5.7). Sexist MESS score was not associated with age, ethnicity, fellowship-training, having children, years of practice, or GSES. In the sexual objectification domain, trainees had higher frequency (p = 0.04), severity (p = 0.02) and total MESS (p = 0.02) scores than attendings.
Conclusions
This was the first multicenter, Canada-wide study exploring how female otolaryngologists experience gender bias and microaggressions in the workplace. Female otolaryngologists experience mild to moderate gender bias, but have high self-efficacy to manage this issue. Trainees had more severe and frequent microaggressions than attendings in the sexual objectification domain. Future efforts should help develop strategies for all otolaryngologists to manage these experiences, and thereby improve the culture of inclusiveness and diversity in our specialty.
Graphical Abstract

Similar content being viewed by others
Background
Gender bias is behavior that shows favoritism toward one gender over another [1]. Gender refers to the socially constructed expectations and roles of women and men [1]. Gender bias may be implicit and affect one’s actions/decision in an unconscious manner [2]. Gender bias can lead to sexism, which is prejudice, stereotyping, or discrimination, on the basis of gender [3].
Studies have identified gender bias as a factor that discourages women from pursuing surgical specialties. Although there are now equal numbers of male and female identifying medical students, fewer women are entering surgical fields, ranging from 14.8% in orthopedics to 40.1% in general surgery [4, 5]. In academic medicine, women comprised only 25% of assistant professors, 17% of associate professors, and 9% of full professors in surgery in 2013 [6]. Gender bias may delay promotions and tenure and discourage rising female leaders [7,8,9,10].
Otolaryngology, like most surgical fields in medicine, is traditionally male dominated. The Royal College of Physicians and Surgeons of Canada report that 23.8% of the Canadian Otolaryngology workforce was comprised of women in 2019 [11]. A similar American statistic from the American Association of Medical Colleges reported that 17.1% of practicing American otolaryngologists were women in 2017 [12]. Unfortunately, there are still inequalities for women in otolaryngology. Female otolaryngologists are underrepresented in compensation [13], National Institute of Health funding [14], financial relationships with industry [15], on otolaryngology journal editorial boards [16], and in research productivity [17].
Gender bias has evolved with time. Most scholars concur that overt sexism, like sexual harassment, has become less prevalent since the civil rights movement [18, 19]. More covert, subtle, or “modern” gender discrimination still exists [18, 19]. Originally coined by a Harvard psychiatrist, “microaggressions” are defined as subtle, often unconscious, discriminatory, or insulting actions that communicate demeaning or negative attitudes towards an individual or group [18,19,20]. Microaggressions have been applied to gender disparity in medicine/surgery [18, 19, 21]. Microaggressions are not benign and have been shown to negatively affect individuals who experience them. Mental health studies have reported increased rates of anxiety, depression, somatic symptoms, decreased well-being, and increased binge drinking among individuals who experience microaggressions [22,23,24,25,26].
The mental health effect of microaggressions on women has been quantified in the literature with the Sexist Microaggressions Experiences and Stress Scale (Sexist MESS) [18]. This validated tool was created as a PhD psychology dissertation. The Sexist MESS correlated significantly with the Mood and Anxiety Symptom Questionaire-Dutch-30 (MASQD30), indicating a positive relationship between sexist microaggressions and general distress, depression, and anxiety. This tool was used in three previous studies exploring microaggressions in female surgeons at a single institution in the United States [19, 27, 28]. In all of these studies, otolaryngologists comprised a very low percentage of the study population—12%, 6%, and 7.7% respectively [19, 27, 28]. Since otolaryngology is a distinct and unique surgical specialty, our goal was to use the Sexist MESS tool to study the effect of gender bias and microaggressions in female otolaryngologists across multiple institutions in Canada.
Self-efficacy (SE) is an optimistic self-belief that one can perform a novel and specific task [29, 30]. Similar to concepts of self-esteem and locus of control, SE describes an individual’s ability to cope with adversity [29, 30]. SE has been shown to be associated with well-being and protective against burnout [31,32,33]. SE can be quantitated by the validated General Self-Efficacy Scale (GSES) [29].
We hypothesized that: 1. Female otolaryngologists and trainees will score high on Sexist MESS scores. 2. Higher self-efficacy as quantified by the GSES will be associated with lower Sexist MESS scores. 3. Female otolaryngologists and trainees will have high GSES. 4. Trainees will have higher Sexist MESS scores than attendings.
Methods
This study was approved by the University of British Columbia (UBC) Behavioural Research Ethics Board (REB # H20-04,063). Demographic data, the validated 44-item Sexist Microaggressions Experiences and Stress Scale (Sexist MESS) and the validated 10-item General Self-efficacy scale (GSES) were administered. These tools were adapted from previously published studies that evaluated gender bias in surgery [1, 9, 27, 28].
The Sexist Microaggressions Experiences and Stress Scale (Sexist MESS) was a 44-item validated questionnaire that assessed gender-based microaggressions [18]. This scale explored seven domains: (1) leaving gender at the door (i.e. downplaying of femininity to succeed), (2) sexual objectification, (3) environmental invalidations (i.e. discrimination in the physical environment or systemic policies), (4) invalidation of the reality of women (i.e. denying that gender bias exists), (5) assumptions of traditional gender roles, (6) expectations of physical appearance, and (7) inferiority (compared to men). Each of the 44 items were ranked on a scale from 0 to 3, on two dimensions—a frequency and severity subscore. Previous studies reported that a score of > 2 on any item in the Sexist MESS was considered “commonly occurring” or “moderately bothersome or stressful” [27]. Each dimension subscore ranged from 0 to 132 (i.e. 3 × 44 = 132), with a total Sexist MESS reported as a sum of the frequency and severity subscores, yielding a total score of 0–264 (132 + 132 = 264). A higher score indicated a higher degree of microaggressions, although there was no abnormal cut-off. Since the scale for this outcome measure (out of 264) is a bit awkward and difficult to interpret, our statistician recommended converting it to a scale that is more easily interpreted by the reader. For the purposes of this study, the raw scores were converted to percentages and categories were defined as the following: mild 0–30%, mild to moderate 30–40%, moderate 40–60%, moderate to severe 60–70%, and severe 70–100%.
The General Self-Efficacy Scale (GSES) was a 10-item validated questionnaire that measured self-efficacy [29]. GSES was self-administered and completed in 4 min. Participants rated items on a scale of 1 to 4; scores ranged from 10 to 40. Higher scores indicated higher degrees of SE, although there was no abnormal cut-off. For the purposes of this study, low was defined as 10–20, moderate 20–30, and high 30–40. There are no scores from 0 to 9; thus, our statistician did not recommend displaying the scores as percentages.
Practicing Canadian female otolaryngologists and otolaryngology trainees (fellows and residents) were eligible for this study. For the purposes of this study, a binary definition of gender as male versus female was used; the full spectrum of gender identities could not be explored in the context of this study. Email addresses were gathered from the 17 academic otolaryngology departments and from the Canadian Society of Otolaryngology Women In Otolaryngology group. Exclusion criteria included invalid email addresses and addresses blocked by spam. The survey was administered with the UBC Survey Tool, provided by Qualtrics. This program complies with British Columbia’s Freedom of Information and Protection of Privacy Act (FIPPA) [34]. The survey was distributed by the Dillman’s Tailored Design Method [35]. This methodology was used by the US Census Bureau and Gallup Organization and has been shown to enhance response rates [34]. Participants were contacted four times over an 8-week period (weeks 1, 2, 4 and 7) through email invitations. After week 8, survey enrollment closed. The survey was administered from July to August, 2021. No renumeration was offered for participation. This project was supported by the American Academy of Otolaryngology – Head & Neck Surgery (AAO-HNS), Women in Otolaryngology Endowment Grant, the Canadian Society of Otolaryngology– Head & Neck Surgery, Dr. Elena M. O’Connell Memorial Grant, and the British Columbia Otolaryngology Society Research Grant.
Statistical analysis
Statistical analysis was conducted by a Masters level statistician with commercial software (SAS 9.4, Cary, NC, USA). Descriptive statistics were used to summarize the characteristics of the study cohort and were displayed as mean (standard deviation) for continuous variables and as counts (%) for categorical variables. Student’s t test was performed to determine if demographic or practice factors were associated with the Sexist MESS. The association between the Sexist MESS and GSES was evaluated with the Spearman correlation coefficient. All p-values were two-sided. P-value < 0.05 was considered statistically significant.
Results
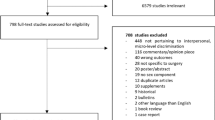
The study started with 206 eligible email addresses. Five were invalid and one was blocked by spam filter. Of the remaining 200, 60 participants completed the survey, yielding a response rate of 30%. Table 1 shows the demographic data of the study population. Table 2 shows the Sexist MESS scores for the study population. Participants scored mild to moderate on the Sexist MESS – Frequency (mean ± standard deviation) 55.8 ± 24.2 (42.3% ± 18.3%), Severity 46.0 ± 23.9 (34.8% ± 18.1%), Total 104.5 ± 43.7 (39.6% ± 16.6%). Participants scored high on GSES 32.7 ± 5.7 (scores range from 10–40) and there was no difference in GSES scores between attendings 32.1 ± 3.7 and trainees 34.2 ± 3.7 (p = NS). Table 3 lists the five most common and five most bothersome/stressful items in the Sexist MESS. Table 4 shows that the sexist MESS scores were not associated with age, ethnicity, fellowship-training, having children, or years of practice. Analysis of the seven domains of Sexist MESS was conducted with each demographic factor. The only factor that was significant was attending vs trainee, as shown in Table 5. Trainees had higher frequency (p = 0.04), severity (p = 0.02), and total (p = 0.02) MESS scores than attendings in the domain of sexual objectification. Spearman correlation coefficient showed that there was no correlation between GSES and Sexist MESS Frequency (ƿ = − 0.11, 95% CI − 0.37 to 0.17), Severity (ƿ = − 0.17, 95% CI -0.44 to 0.12), and Total Score (ƿ = − 0.09, 95% CI − 0.37 to 0.21).
Figure 1 shows the most common sources of gender bias reported by the participants: 1. patients (92%), 2. Operating room nurses (75%), and 3. Physician in authority position (67%). Figure 2 shows the participants’ feelings and responses towards gender bias: 1. felt offended (53%), 2. ignored it (49%), 3. got frustrated/angry (49%). About 1/3 of participants felt that men were also subject to gender bias. No physical harm or adverse events were encountered, although this topic may have triggered psychological distress among participants.
Discussion
Three previous single institutional studies used the same outcome measure, the Sexist MESS, to explore gender bias experiences in female surgeons [19, 27, 28]. The first Barnes et al. study of female surgical trainees had 33/50 participants (response rate 66%) [27]. They divided the trainees into female-dominate field (obstetrics/gynecology) and male-dominate fields (all other surgical specialties). Female trainees in male-dominant fields reported more frequent, severe, and stressful microaggression experiences than female trainees in female-dominant fields. Their study had five items in the Sexist MESS that scored over 2, indicating a more severe or significant result, in comparison to our study that only identified one item (Table 2). The second Barens et al. study of female surgeons of all specialties had 65/101 participants (response rate 64%) [19]. The frequency and severity of Sexist MESS scores were higher for trainees than attendings. The variables of non-White ethnicity, having children under 18, and fellowship training were not associated with the Sexist MESS scores. The third Sudol et al. study’s objective was to determine the prevalence of sexist and racial/ethnic microaggressions against female surgeons and anesthesiologists and to assess its’ association with burnout [28]. Using the Sexist MESS, they defined the prevalence of microaggressions as at least 1 mean subscale score for frequency. They also employed the Racial Microaggression Scale and Maslach Burnout Inventory. With a sample size of 652/1609 (response rate 41%) conducted at a single health maintenance organization, they reported that 94% of female respondents reported sexist microaggression and 81% of racial/ethnic minority physicians reported racial/ethnic microaggression. Microaggression was significantly associated with physician burnout, an important mental health and human resource issue in the health care system. This study was able to study the intersectionality of gender and race/ethnicity with microaggression.
This current study reinforces the previous literature that trainees are more at risk for gender bias and microaggressions [27, 36,37,38]. In the domain analysis of the current study, the frequency severity, and total MESS score was higher for trainees than attendings in the domain of sexual objectification. In the second Barnes et al. study, trainees had higher frequency MESS scores in six of the seven domains and higher severity MESS scores in three of the seven domains [27]. A recent multi-institutional, national survey of American general surgery and surgical specialty residents revealed that the majority (72.2%) of residents had experienced microaggression, most commonly from patients (64.1%) [36]. Only 7% reported these events and nearly one-third (30.8%) of residents experienced retaliation due to reporting of microaggressions [36]. Further studies in plastic surgery and emergency medicine confirmed these results [37, 38]. For example, misidentification as a non-clinician staff, the most common form of microaggression in the emergency medicine study, occurred more commonly with trainees than attendings, more commonly with women than men, and more commonly with non-White than White respondents [38].
In the medical hierarchy, attending physicians may have more authority and power than trainees, who are more vulnerable in experiencing and addressing microaggressions. Attending physicians may be bystanders when these microaggressions occur to trainees. Bystanders are defined as “anyone who becomes aware of and/or witnesses unjust behavior or practices that are worthy of comment or action” [39, 40]. Education and faculty development on how to manage these experiences are crucial and the goal is to support bystanders to become “upstanders”. “Upstanders” are those who take action, intervene, and speak up for trainees/colleagues who are experiencing microaggressions [37, 40]. Universities and teaching faculty members have an ethical and legal obligation to provide a safe learning environment for their trainees. Speaking up for trainees in the face of microaggressions is one aspect of advocating of them.
The current study also investigated the concept of self-efficacy. Self-efficacy has been studied in surgical trainees in relation to well-being and burn out [30,31,32]. A large cross-sectional survey of all surgical residents at Stanford reported that high self-efficacy was predictive of well-being [30]. Another multicenter study of general surgery residents reported that lower burnout was associated with higher self-efficacy and lower perceived stress scores [31]. A third multicenter study of vascular surgery residents reported that burnout was associated with lower self-efficacy and higher levels of depression [32]. Higher levels of self-efficacy were also found to prevent burnout in other first line responders, like nurses and firefighters [41, 42].
Our study showed that female otolaryngologists have high degrees of self-efficacy, but there was no significant association between GSES and Sexist MESS scores. There may be several explanations for the lack of statistical significance. First, there was a narrow range of GSES scores, so it may be difficult to show a statistical association with another variable. Second, there may be survivorship bias in this study [43]. Female otolaryngologists who survived the rigours of surgical training and stayed practicing in this field were surveyed. Those with lower self-efficacy may have left the field and not been eligible for the study. We do not know the self-efficacy of women who did not complete the study. Lastly, there were no senior full professors who completed the study; albeit, women comprise a very small proportion of full professors in academic medicine [6].
Figure 1 showed that the top source of microaggressions experienced by female otolaryngologists was patients (90%). This was confirmed in three previous studies, which rated patients as the top source of microaggressions experienced by 94% of female surgical residents [27], 80% of all female surgeons [19], and 64.1% of all American surgical residents [36]. Addressing microaggressions that were perpetrated by patients is problematic on multiple levels. Although the conduct of health care providers is directly regulated by industry and hospital standards of professionalism, the conduct of patients is not regulated. Furthermore, patients seek care when they or their loved ones are ill and at their most vulnerable state. Patients and their caregivers often feel they need to advocate for themselves or their loved ones, and they may strike out against health care providers. Health care professionals may feel an ethical obligation to maintain the physician–patient relationship, even in the face of gender bias and microaggressions, and even more egregious behaviour.
Addressing microaggressions and managing gender bias can be challenging. Barriers for physicians to address these issues include fear of retaliation, fear of situational escalation, further discrimination, jeopardizing personal/physical safety, and exclusion by coworkers [44, 45]. Some advocate that the first step to addressing microaggressions is recognizing it [44]. The perpetrator may not be aware of the transgression and may not have had any malicious intent. On a system level, implicit bias and diversity training have been implemented by multiple institutions to reduce these biases. Evidence of successful changes in the workplace, unfortunately, are slow, as it takes a long time to change organizational culture [46, 47].
Figure 2 shows that these microaggressions caused negative feelings and responses in about half of respondents. About half of female otolaryngologists felt offended, got angry, or frustrated. About half of respondents ignored the microaggressions, which is an unhealthy response as it does not address the issue and builds up negative emotions in the victims. Instead, ignoring the microaggressions enables the perpetrator to continue the inappropriate behaviour. Only about one fifth of respondents were empowered to confront the perpetrator. This may educate the perpetrator about the transgression and hopefully break the cycle. Previous qualitative studies have reported that female surgeons have developed resilience—“toughness” or “thick skin” [19, 27]. Some developed coping strategies like using humour; others used increased effort to adapt [19, 27].
One study recommended that future directions should explore how to address these microaggressions in a healthy and productive manner [19]. The Mayo Clinic has developed the GRIT (Gather, Restate, Inquire, Talk It Out) Framework for Addressing Microaggressions: [48] 1. Gather your thoughts. Do not overreact with anger. Decide if it is the appropriate juncture to address the perceived microaggression. 2. Restate the comment or ask the speaker to restate it. Allow the person to clarify or realize the potential negative impact of the comment. 3. Inquire. Dig deeper and seek clarification: Be nonjudgmental. Address the comment rather than making it personal. 4. Talk it out. Discuss the potential impact on others and your own perception. This framework aims to promote open, productive communication between all parties, recognizing that we may all be recipients, witnesses, and perpetrators of microaggression.
Gender bias can have potential impact on the hiring process of potential candidates. These unconscious stereotypes have been found to have negative consequences for women who apply for jobs traditionally held by men [49,50,51]. For example, a systematic review of reference letters for residency and academic medicine faculty positions reported that reference letters for female applicants had more frequent use of doubt raisers and mentions of applicant’s personal life and/or physical appearance [50]. Women were more likely to be described with communal adjectives, like “compassionate”, while men were more likely to be described with agentic adjectives, like “leader”. During interviews, applicants who displayed gender incongruent behaviours (e.g. women who were self-promoting) were rated lower than applicants who behaved in a more gender-congruent manner [51]. Employers are becoming aware of this gender bias and a systematic review discussed interventions to mitigate this [49]. Interventions included providing only job relevant information to raters (e.g. not including parental or marital status), being aware of gender stereotyped behaviour and appearances, and instituting explicit employment equity policies.
We recognize some limitations in this study. Gender is a fluid concept and some otolaryngologists may not fully identify with the binary distinction of cis-man or cis-woman. The authors attempted to build a comprehensive mailing list of all practicing female otolaryngologists by contacting the 17 otolaryngology departments across Canada and the Canadian Society of Otolaryngology Women in Otolaryngology group. Some private practice or community otolaryngologists may have been inadvertently left off the distribution list. Although Table 1 reports that 50.0% (30/60) of the respondents were fellowship trained, the study population included trainees (19 residents and 6 fellows); thus, only 35 respondents were attending surgeons who would have been eligible for completing fellowship training. The proportion of fellowship trained attending surgeons (30/35 = 85.7%) was much higher, so there may have been a higher representation of academic surgeons who have completed a fellowship. Despite employing the Dillman’s Tailored Design Method [34] for survey distribution, the response rate of 30% could be improved upon. The previous studies were all single institution studies [19, 27, 28]. Our sample size of 60 was larger than the first Barnes et al. study (n = 33) and comparable to the second Barnes et al. study (n = 65) [19, 27]. The response rate of 30% is less than the previous two studies’ response rates of 64–66% and the third study’s response rate of 41%, which likely reflects the challenges of a multi-institution study [19, 27, 28]. There may have been a selection bias in which female otolaryngologists who felt strongly about the topic decided to complete the survey. The opinions of those who did not participate were unknown. Since there were no senior full professors who answered this survey, we were unable to comment if more senior female otolaryngologists experienced microaggressions differently than junior female otolaryngologists. About one third of participants felt that men were also subject to gender bias, and this would be an area for future research. Studying the intersectionality of gender with race/ethnicity, religion, and sexual orientation and its effect on microaggression was outside of scope of this current study.
Conclusions
This was the first multicenter, Canada-wide study exploring how female otolaryngologists experience gender bias and microaggressions in the workplace. These experiences have been shown to have negative effects on individuals who experience them. Validated outcome measures and rigorous survey methodology were used in this study. Female otolaryngologists experience mild to moderate gender bias, but have high self-efficacy to manage this issue. Trainees had more severe and frequent microaggressions than attendings in the sexual objectification domain. Future efforts should help develop skills and strategies for all otolaryngologists to address gender and racial bias experiences, become “up-standers”, and thereby improve the culture of inclusiveness and diversity in our specialty.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Sexist MESS:
-
Sexist Microaggressions Experiences and Stress Scale
- MASQD30:
-
Mood and Anxiety Symptom Questionaire-Dutch-30
- SE:
-
Self-efficacy
- UBC:
-
University of British Columbia
- REB:
-
Research ethics board
- GSES:
-
General Self-efficacy Scale
- FIPPA:
-
Freedom of Information and Protection of Privacy Act
- AAO-HNS:
-
American Academy of Otolaryngology—Head and Neck Surgery
- GRIT:
-
Gather, Restate, Inquire, Talk It Out Framework for Addressing Microaggressions
- NS:
-
Not significant
- SD:
-
Standard deviation
References
Rothchild J. Gender bias. The Blackwell Encyclopedia of Sociology. Wiley. Wiley Online Library. Published Nov 7 ,2014. Accessed Dec 23, 2021. https://doi.org/10.1002/9781405165518.wbeosg011.pub2
Ohio State University. Understanding implicit bias. Updated 2015. Accessed Dec 27, 2020. http://kirwaninstitute.osu.edu/research/understanding-implicit-bias/
Sexism". New Oxford American Dictionary (3 ed.). Oxford University Press. 2010. ISBN 9780199891535.
Association of American Medical Colleges. Table A-7.2: Applicants, first-time applicants, acceptees, and matriculants to U.S. medical schools by sex, 2010–2011 through 2019–2020. https://www.aamc.org/system/files/2019-10/2019_FACTS_Table_A-7.2.pdf. Updated October 4, 2019. Accessed Dec 27, 2020.
Association of American Medical Colleges. Table B3: Number of active residents, by type of medical school, GME specialty, and sex: 2017–18 active residents. https://www.aamc.org/data-reports/students-residents/interactive-data/table-b3-number-activeresidents-type-medical-school-gmespecialty-and-sex. Accessed Dec 27, 2020.
Association of American Medical Colleges. The state of women in academic medicine: The pipeline and pathways to leadership, 2013–14. https://www.hopkinsmedicine.org/women_science_medicine/_pdfs/the%20state%20of%20women%20in%20 academic%20medicine%202013–2014%20final.pdf. Accessed June 2, 2020.
Sexton KW, Hocking KM, Wise E, et al. Women in academic surgery: the pipeline is busted. J Surg Educ. 2012;69:84–90.
Greenberg CC. Association for academic surgery presidential address: sticky floors and glass ceilings. J Surg Res. 2017;219:ix–xvii.
Hill E, Vaughan S. The only girl in the room: How paradigmatic trajectories deter female students from surgical careers. Med Educ. 2013;47:547–56.
Mueller C, Wright R, Girod S. The publication gender gap in US academic surgery. BMC Surg. 2017;17:16.
Royal College of Physicians and Surgeons of Canada. Royal College Medical Workforce Knowledgebase. 2021. Accessed August 16, 2021. Available at: https://www.royalcollege.ca/rcsite/health-policy/medical-workforce-knowledgebase-e
Association of American Medical Colleges. Active Physicians by Sex and Specialty, 2017. Table 1.3. Number and Percentage of Active Physicians by Sex and Specialty, 2017.
Grandis JR, Gooding WE, Zamboni BA. The gender gap in a surgical subspecialty: analysis of career and lifestyle factors. Arch Otolaryngol Head Neck Surg. 2004;130:695–702.
Lennon CJ, Hunter JB, Mistry AM, et al. NIH funding within otolaryngology: 2005–2014. Otolaryngol Head Neck Surg. 2017;157:774–80.
Eloy JA, Bobian M, Svider PF, et al. Association of gender with financial relationships between industry and academic otolaryngologists. JAMA Otolaryngol Head Neck Surg. 2017;143:796–802.
Litvack JR, Wick EH, Whipple ME. Trends in female leadership at high profile otolaryngology journals, 1997–2017. Laryngoscope. 2019;129:2031–5.
Eloy JA, Svider PF, Cherla DV, et al. Gender disparities in research productivity among 9952 academic physicians. Laryngoscope. 2013;123:1865–75.
Derthick AO. The Sexist MESS: Development and Initial Validation of the Sexist Microaggressions Experiences and Stress Scale and the Relationship of Sexist Microaggressions to Women’s Mental Health [dissertation]. Anchorage, AK: University of Alaska Anchorage; 2015. https://search.proquest.com/docview/1752638981/abstract/ 86CB284661 5345E9PQ/1. Accessed Dec 27, 2020.
Barnes KL, Dunivan G, Sussman AL, McGuire L, McKee R. Behind the mask: an exploratory assessment of female surgeons’ experiences of gender bias. Acad Med. 2020;95:1529–38.
Pierce C, Carew J, Pierce-Gonzalez D, Willis D. An experiment in racism: TV commercials. In: Pierce C, editor. Television and education. Beverly Hills, CA: Sage; 1978. p. 62–88.
Torres MB, Salles A, Cochran A. Recognizing and reacting to microaggressions in medicine and surgery. JAMA Surg. 2019;154:868–72.
Fredrickson B, Roberts T. Objectification theory: toward understanding women’s lived experiences and mental health risks. Psychol Women Quart. 1997;21:173–206.
Swim JK, Hyers LL, Cohen LL, Ferguson MJ. Everyday sexism: evidence for its incidence, nature, and psychological impact from three daily diary studies. J Soc Issues. 2001;57:31–53.
Moore KM. The Mental Health Implications of Experiencing Racial/Ethnic Microaggressions Among Latina/os: Cognitive, Affective, and Behavioral Components [dissertation]. Milwaukee, WI: Marquette University; 2009. https://epublications.marquette.edu/dissertations_mu/218. Accessed May 12, 2020.
Landrine H, Klonoff EA, Gibbs J, Manning V, Lund M. Physical and psychiatric correlates of gender discrimination: an application of the schedule of sexist events. Psychol Women Quart. 1995;19:473–92.
Blume AW, Lovato LV, Thyken BN, Denny N. The relationship of microaggressions with alcohol use and anxiety among ethnic minority college students in a historically White institution. Cult Divers Ethn Min. 2012;18:45–54.
Barnes KL, McGuire L, Dunivan G, Sussman AL, McKee R. Gender bias experiences of female surgical trainees. J Surg Educ. 2019;76(6):e1–14.
Sudol NT, Guaderrama NM, Honsberger P, Weiss J, Li Q, Whitcomb EL. Prevalence and nature of sexist and racial/ethnic microaggressions against surgeons and anesthesiologists. JAMA Surg. 2021;156(5):e210265. https://doi.org/10.1001/jamasurg.2021.0265.
Schwarzer R, Jerusalem M, Weinman J, et al. Generalized Self-Efficacy Scale. Measures in Health Psychology: A Users Portfolio. Causal and Control Beliefs. Windsor: NFERNELSON; 1995.
Bandura A. Self-efficacy: the exercise of control. New York: Freeman; 1997.
Milam LA, Cohen GL, Mueller C, Salles A. The relationship between self-efficacy and well-being among surgical residents. J Surg Educ. 2019;76(2):321–8.
Smeds MR, Janko MR, Allen S, Amankwah K, Arnell T, et al. Burnout and its relationship with perceived stress, self-efficacy, depression, social support, and programmatic factors in general surgery residents. Am J Surg. 2020;219(6):907–12.
Janko MR, Smeds MR. Burnout, depression, perceived stress, and self-efficacy in vascular surgery trainees. J Vasc Surg. 2019;69(4):1233–42.
Freedom of Information and Protection of Privacy Act. Updated Mar 17, 2021. Accessed Mar 25, 2021. https://www.bclaws.gov.bc.ca/civix/document/id/complete/statreg/96165_00
Dillman DA. Mail and internet surveys: the tailored design method. New York: Wiley & Sons; 2000.
Alimi Y, Bevilacqua LA, Snyder RA, Walsh D, Jackson PG, DeMaria EJ, Tuttle-Newhall JE, Altieri MS. An undocumented but pervasive phenomenon. Ann Surg. 2021. https://doi.org/10.1097/sla.0000000000004917. (PMID: 33843793).
Goulart MF, Huayllani MT, Samora JB, Moore AM, Janis JE. Assessing the prevalence of microaggressions in plastic surgery training: a national survey. Plast Reconstr Surg Glob Open. 2019;9(12):e4062. https://doi.org/10.1097/GOX.0000000000004062.
Brown C, Daniel R, Addo N, Knight S. The experiences of medical students, residents, fellows, and attendings in the emergency department: Implicit bias to microaggressions. AEM Educ Train. 2021;5(Suppl 1):S49–56. https://doi.org/10.1002/aet2.10670.eCollection.
Scully M, Rowe M. Bystander training within organizations. J Int Ombudsman Assoc. 2009;2:1–9.
Sue DW, Alsaidi S, Awad MN, et al. Disarming racial microaggressions: microintervention strategies for targets, White allies, and bystanders. Am Psychol. 2019;74:128–42.
Yao Y, Zhao S, Gao X, An Z, Wang S, et al. General self-efficacy modifies the effect of stress on burnout in nurses with different personality types. BMC Health Serv Res. 2018;18(1):667.
Makara-Studzińska M, Golonka K, Izydorczyk B. Self-efficacy as a moderator between stress and professional burnout in firefighters. Int J Environ Res Public Health. 2019;16(2):183.
Thomas J. Bullet Holes & Bias: The Story of Abraham Wald. Mcdreeamie-musings. April 23, 2019. Accessed December 12, 2021. https://mcdreeamiemusings.com/blog/2019/4/1/survivorship-bias-how-lessons-from-world-war-two-affect-clinical-research-today
Nadal KL. A guide to responding to microaggressions. CUNY Foren. 2014;2(1):71–6.
Yoon H. How to Respond to Microaggressions. The New York Times. Published March 3, 2020. Accessed Mar 27, 2021. https://www.nytimes.com/2020/03/03/smarter-living/how-to-respond-to-microaggressions.html
Carnes M, Devine PG, Isaac C, et al. Promoting institutional change through bias literacy. J Divers High Educ. 2012;5:63–77.
Rudman LA, Ashmore RD, Gary ML. “Unlearning” automatic biases: the malleability of implicit prejudice and stereotypes. J Pers Soc Psychol. 2001;81:856–67.
Warner NS, Njathi-Ori CW, Orien EK. The GRIT (gather, restate, inquire, talk it out) framework for addressing microaggressions. JAMA Surg. 2020;155(178–179):49.
Isaac C, Lee B, Carnes M. Interventions that affect gender bias in hiring: a systematic review. Acad Med. 2009;84:1440–6.
Khan S, Kirubarajan A, Shamsheri T, Clayton A, Mehta G. Gender bias in reference letters for residency and academic medicine: a systematic review. Postgrad Med J. 2021. https://doi.org/10.1136/postgradmedj-2021-140045.
Rudman LA. Self-promotion as a risk factor for women: the costs and benefits of counterstereotypical impression management. J Pers Soc Psychol. 1998;74:629–45.
Acknowledgements
We would like acknowledge Hong Qian, M.Sc., a paid statistician at the Centre for Health Evaluation & Outcome Sciences (CHÉOS), for her statistical support on this project.
Funding
1. American Academy of Otolaryngology – Head & Neck Surgery Women In Otolaryngology Endowment Grant. 2. British Columbia Otolaryngology Society Research Grant. 3. Canadian Society of Otolaryngology– Head & Neck Surgery, Dr. Elena M. O’Connell Memorial Grant. These funding sources had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
AH: (1) conception and design, acquisition of data, analysis and interpretation of data; (2) drafting and revising the article; (3) final approval; and (4) accountable for all aspects. KN: (1) acquisition of data; (2) revising article (3) final approval of the version to be published; and (4) accountable for all aspects. TM: (1) conception and design, analysis and interpretation of data; (2) revising the article; (3) final approval; and (4) accountable for all aspects. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University of British Columbia (UBC) Behavioural Research Ethics Board (REB # H20-04063) and consent was obtained from each participant prior to survey initiation.
Consent for publication
Not applicable.
Competing interests
AH is the recipient of honorarium for a chronic cough educational presentation from Merck Inc., is on the advisory board for a stroboscopy machine with Pentax Medical, and has grant funding for another project from the Michael Smith Foundation for Health Research. KN and TM declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, A.C., Nguyen, K. & Meyer, T.K. Exploring female otolaryngologists’ experiences with gender bias and microaggressions: a cross sectional Canadian survey. J of Otolaryngol - Head & Neck Surg 52, 22 (2023). https://doi.org/10.1186/s40463-022-00618-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40463-022-00618-1