Abstract
Introduction
Diagnosis and treatment of obstructive sleep apnea (OSA) in children is often delayed due to the high prevalence and limited physician and sleep testing resources. As a result, children may be referred to multiple specialties, such as pediatric sleep medicine and pediatric otolaryngology, resulting in long waitlists.
Method
We used data from our pediatric OSA clinic to identify predictors of tonsillectomy and/or adenoidectomy (AT). Before being seen in the clinic, parents completed the Pediatric Sleep Questionnaire (PSQ) and screening questionnaires for restless leg syndrome (RLS), nasal rhinitis, and gastroesophageal reflux disease (GERD). Tonsil size data were obtained from patient charts and graded using the Brodsky-five grade scale. Children completed an overnight oximetry study before being seen in the clinic, and a McGill oximetry score (MOS) was assigned based on the number and depth of oxygen desaturations. Logistic regression, controlling for otolaryngology physician, was used to identify significant predictors of AT. Three triage algorithms were subsequently generated based on the univariate and multivariate results to predict AT.
Results
From the OSA cohort, there were 469 eligible children (47% female, mean age = 8.19 years, SD = 3.59), with 89% of children reported snoring. Significant predictors of AT in univariate analysis included tonsil size and four PSQ questions, (1) struggles to breathe at night, (2) apneas, (3) daytime mouth breathing, and (4) AM dry mouth. The first triage algorithm, only using the four PSQ questions, had an odds ratio (OR) of 4.02 for predicting AT (sensitivity = 0.28, specificity = 0.91). Using only tonsil size, the second algorithm had an OR to predict AT of 9.11 (sensitivity = 0.72, specificity = 0.78). The third algorithm, where MOS was used to stratify risk for AT among those children with 2+ tonsils, had the same OR, sensitivity, and specificity as the tonsil-only algorithm.
Conclusion
Tonsil size was the strongest predictor of AT, while oximetry helped stratify individual risk for AT. We recommend that referral letters for snoring children include graded tonsil size to aid in the triage based on our findings. Children with 2+ tonsil sizes should be triaged to otolaryngology, while the remainder should be referred to a pediatric sleep specialist.
Graphical abstract

Similar content being viewed by others
Introduction
Sleep-disordered breathing describes a set of ventilatory disorders ranging from snoring to obstructive sleep apnea (OSA; 1). Prolonged OSA symptoms have been associated with learning difficulties, emotional dysregulation, and behavioural concerns, as well as cardiovascular and metabolic complications [1,2,3]. Reducing the time between initial investigation and intervention may help prevent these adverse outcomes [4]. An earlier age of onset, and longer duration of sleep-related breathing disorder (SRBD) symptoms is associated with greater behavioral problems, emphasizing the need for earlier identification and treatment [5].
Children may present with OSA due to enlarged adenoids and tonsils, craniofacial abnormalities, obesity, abnormal muscle tone of the upper airway, and abnormal drive to breathe [1]. As a result, the multiple causes of childhood OSA make it challenging to determine which specialty should first see the OSA patient. The most common cause of childhood OSA is adenotonsillar hypertrophy. In addition to adenotonsillar hypertrophy, children who snore for greater than 3 months are more likely to be male, experience obesity, and are breastfed [6]. As such, tonsillectomy and/or adenoidectomy (AT) by an otolaryngologist is the most common treatment for OSA [7, 8]. Children with OSA may also present with associated comorbidities such as allergic and non-allergic rhinitis, restless leg syndrome (RLS [9];) and gastroesophageal reflux (GERD [10];). As a result of these multiple overlapping causes of OSA, physicians with specialty training in respirology may also see and treat OSA patients. Otolaryngology – head and neck surgery residents, while knowledgeable on OSA, had variable confidence in managing OSA surgeries [11] highlighting the complexity and importance of effective triaging and referral protocols for OSA patients. Further, wait-times for patients can be reduced by identifying which specialty the OSA patient should be referred to first [1, 12,13,14].
Polysomnography (PSG) is the golden standard for diagnosing OSA in children [7]. Unfortunately, PSG is a time-consuming and expensive test with limited resources in pediatric centers worldwide [13]. Overnight oximetry studies are often used to screen for OSA [7, 15, 16], although they have limited sensitivity. Both PSG and overnight oximetry do not determine the cause of an individual’s OSA. While not diagnostic for OSA, tonsil size and adenoid size may help determine which children are AT surgical candidates [17]. We used data from our pediatric OSA clinic to identify predictors of AT, including tonsil and adenoid size and overnight oximetry [12]. We subsequently developed an algorithm for triaging patients to either pediatric respirology or otolaryngology.
Method
Study population
Children seen at the pediatric OSA clinic at the Stollery Children’s Hospital in Edmonton, Alberta, Canada, between August 2012 and May 2020, who consented to have their charts reviewed for research purposes, were included in this analysis [12]. Children with comorbidities were excluded at triage. Details of the processes and questionnaires associated with the pediatric OSA clinic have been described previously [12]. Briefly, parents completed questionnaires and some testing, such as overnight oximetry, before being seen in the clinic. For clinical care purposes, clinic data collection was approved by the Alberta Office of Information and Privacy (004604). This analysis was approved by the University of Alberta ethics board (Pro00089369).
Study variables
AT (primary outcome variable)
AT history was obtained from the patient’s chart after their clinic visits or was parent-reported through our medical intake questionnaire.
Tonsil size (primary predictor variable)
Tonsil size data, obtained from patient charts, was graded using the Brodsky five-grade scale [17].
McGill oximetry score (MOS; secondary predictor variable)
Children completed an overnight oximetry study before being seen in the clinic (i.e., no treatment was started by the clinic team). A McGill oximetry score (MOS) was assigned to each study based on the number and depth of oxygen desaturations [15].
Additional predictor variables assessed by questionnaires
Before being seen in the clinic, parents were asked to complete the Pediatric Sleep Questionnaire (PSQ [18];) and screening questionnaires for Restless Leg Syndrome (RLS), Gastroesophageal Reflux Disease (GERD) and the (Nasal Obstruction Symptom Evaluation (NOSE) survey [19];). Participants were considered to be at risk for RLS if they endorsed at least one RLS symptom. Children with two or more GERD symptoms were considered to have GERD. Children with a NOSE score of 10 or greater were considered to have significant rhinitis symptoms [19].
Statistical analyses
Univariate and multivariate logistic regression analyses (controlling for otolaryngology physicians) were completed to identify predictors of AT (outcome variable). Three triage algorithms were generated based on the univariate and multivariate results to predict AT. The p-value was set at p < 0.05. Statistical analyses were performed using Stata/MP 15.1 (Stata Corporation).
Results
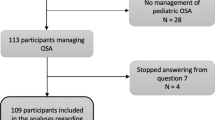
There were 469/801 patients included in this analysis as 259 children did not have a research consent (Fig. 1), one patient was incorrectly triaged to our clinic [1], and 72 refused consent for research. Of the 469 children included in the analyses, 46% (215/469) were referred from family medicine, 46% from pediatrics (216/469), with the remainder, referred from dentistry, otolaryngology, and other physician specialties [5]. There were 89% (418/469; Table 1) of children who reported ever snoring, and 65% (306/469) snored over half the night. The mean age at the time of the clinic visit was 8.2 years (SD = 3.6), and 207/436 (47%) of participants were female.
Univariate results
Children with tonsil sizes graded as 3 were 3.41 times more likely to have a AT compared to children with tonsils graded 1 (95% CI 1.57, 7.39; p < 0.05; Table 1) while children with tonsil sizes graded as 4 were 7.96 times more likely to have a AT compared to children with tonsils graded as 1 (95% CI 3.63, 17.45; p < 0.05). Children with three or more positive PSQ questions were significantly more likely to receive a AT. Four PSQ questions were significantly associated with a child having a AT: (1) struggles to breathe at night; (2) witnessed apneas; (3) mouth breathes during the day; and (4) has a dry mouth in the morning. Children with a MOS of 2 or greater were 3.42 times more likely to receive a T & A than those with a MOS less than 2 (95% CI 1.62, 7.21; p < 0.05).
Multivariate predictors of AT
Tonsil size was the only predictor of AT when controlling for ENT surgeons.
Triage algorithms
Three triage algorithms were developed based on the univariate and multivariate results. Algorithms were based on 1) four PSQ questions, 2) tonsil size and 3) tonsil size and oximetry. A model based on oximetry alone is available in the supplementary material. No children with a prior AT (n = 18) required a second AT intervention (0% AT) over our study timeframe. Therefore, children with a prior AT are always initially triaged to respirology in all three algorithms.
PSQ based algorithm (Fig. 2)
Children with four of four PSQ questions positive (identified from the univariate analysis; n = 66) were given a 'Tonsil Score' of four out of four, and were triaged to ENT (56% AT). Subsequently, children with at least one RLS symptom (n = 318) were triaged to respirology (25% AT). Children with two or more GERD symptoms or a NOSE score greater than or equal to 10 were also triaged to respirology (32% AT). Out of the remaining 34 children, children with three of four PSQ questions positive were given a 'Tonsil Score' of three out of four and were triaged to ENT (n = 3; 50% AT). The remaining 31 children were triaged to respirology (10% AT). The sensitivity for this model was 0.28, with a specificity of 0.91 (Table 2).
Tonsil size-based algorithm (Fig. 3)
Children with graded tonsils 0 or 1 were triaged to respirology (n = 63; 17% AT), while those with graded tonsils 2, 3, and 4 were triaged to ENT (n = 167; 56% AT). All remaining children were triaged to respirology. The sensitivity of this model was 0.72, and the specificity was 0.78.
Tonsil and oximetry-based algorithm (Fig. 4)
Oximetry did not impact which specialty children were triaged to. However, MOS was associated with AT rates. Among children with graded tonsils 2–4, those with a MOS score of 2–4 had a 78% AT rate (n = 21). Children with graded tonsils 2–4 and a MOS score of less than 2 had a 50% chance of a AT (n = 122). Children with graded tonsils 2–4 and no oximetry data (n = 24) had a 71% AT rate. The metrics for this model were identical to the metrics found in the model without oximetry data.
Discussion
Using data from our pediatric OSA clinic, we found that tonsil size was the strongest predictor of AT in otherwise healthy children. The MOS was useful for stratifying otherwise healthy children with OSA by risk for AT. The triage algorithms generated using this data had a high positive likelihood ratio for identifying children who will have a AT. Based on our findings, we recommend that physicians referring otherwise healthy children with OSA symptoms should i) Provide graded tonsil size in the referral letter and ii) Consider tonsil size when deciding whether to direct refer to ENT or respirology.
Tonsil size has been previously associated with AT despite previous research showing OSA severity was not linearly associated with tonsils size above grade 2 [20]. Consistent with this finding, our triage algorithm recommended referring children with OSA and tonsils grades 2–4 to ENT as they are more likely to be offered AT. As per the original MOS publication, we found that oximetry, and by extension MOS, simply stratified risk for AT rather than identify which specialty a patient should be referred to [15]. However, it was not the scope of this study to predict the improvement of OSA symptoms after AT. Surprisingly, the PSQ, a validated tool to identify children with OSA, did not help triage patients. The PSQ may not help triage patients due to the subjective nature of the PSQ, resulting in parental-report bias and the referral bias of the clinic sample.
The strength in these analyses come from the comprehensive data collected from a community sample of OSA cases. Limitations exist due to the subjective nature of parent-reported symptoms on the PSQ and incomplete data on whether patients received an adenoidectomy and/or tonsillectomy alone. Applying this algorithm to centers with different clinical practices or more complex pediatric populations, such as obese children or those with craniofacial abnormalities, are potential limitations. Additionally, nearly all participants snored, representing a pre-selected sample of children at higher risk for OSA.
Future work would include validating our triage algorithms in a separate clinic sample and follow-up to determine whether OSA symptoms and sleep concerns were resolved following AT. Modifying the algorithm with information from PSG or home sleep testing rather than oximetry alone may further improve the algorithms predictive capacity. Follow-up studies may explore long-term outcomes and comparing post-operative complications [21] for patients who were triaged based on the algorithm versus a control group.
Conclusion
We aimed to identify an efficient method of triaging pediatric cases of OSA to respirology or ENT. We created three algorithms to predict AT, all of which had similar positive likelihood ratios but different odds ratios. Our results highlight the importance of utilizing the PSQ to guide the referral process. The PSQ, a cost-effective, fast, reliable and valid measure of sleep-related issues [18], may be implemented in primary care to help alleviate long waitlists for sleep studies and initial specialist consultation. Unsurprisingly, tonsil size was the strongest predictor of AT, while oximetry MOS only stratified risk for AT. Based on our results, we recommend that pediatric OSA referral letters include graded tonsil size to aid in the triaging of suspected OSA cases.
Availability of data and materials
All data generated or analyzed during the present study are included in this published article.
Abbreviations
- AT:
-
Adenoidectomy/Tonsillectomy
- ENT:
-
Ear, Nose, Throat
- GERD:
-
Gastroesophageal reflux
- MOS:
-
McGill Oximetry Score
- NOSE:
-
Nasal Obstruction Symptom Evaluation
- OSA:
-
Obstructive Sleep Apnea
- PSG:
-
Polysomnography
- PSQ:
-
Pediatric Sleep Questionnaire
- RLS:
-
Restless Leg Syndrome
- SRDB:
-
Sleep Related Disordered Breathing
References
Narayanasamy S, Kidambi SS, Mahmoud M, Subramanyam R. Pediatric sleep disordered breathing: a narrative review. Pediatric Med. 2019;2:1–15.
Marcus CL, Carroll JL, Bamford O, Pyzik P, Loughlin GM. Supplemental oxygen during sleep in children with sleep-disordered breathing. Am J Respir Crit Care Med. 1995;152(4):1297–301. https://doi.org/10.1164/ajrccm.152.4.7551385.
Reyna M, Dai R, Moraes TJ, Becker AB, Azad M, Mandhane P, et al. Preschool BMI Trajectories, Breastfeeding Status and Their Association with Wheeze Phenotypes. A18 Factors associated with pediatric wheeze and asthma: American Thoracic Society; 2020.
Halbower AC, McGinley BM, Smith PL. Treatment alternatives for sleep-disordered breathing in the pediatric population. Curr Opin Pulm Med. 2008;14(6):551–8. https://doi.org/10.1097/MCP.0b013e3283130f80.
van Eeden C, Tamana SK, Narang I, Hammam N, Chikuma J, Lefebvre DL, et al. Development and validation of SDBeasy score as a predictor of behavioral outcomes in childhood. Am J Respir Crit Care Med. 2021;203(6):718–25. https://doi.org/10.1164/rccm.202002-0363OC.
Xu Z, Wu Y, Tai J, Feng G, Ge W, Zheng L, et al. Risk factors of obstructive sleep apnea syndrome in children. Journal of Otolaryngology - Head & Neck Surgery. 2020;49:1.
MacLean JE. Assessment and treatment of pediatric obstructive sleep apnea in Canada: history and current state of affairs. Sleep Med. 2019;56:23–8. https://doi.org/10.1016/j.sleep.2019.01.011.
Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome. Pediatrics. 2012;130(3):576–84. https://doi.org/10.1542/peds.2012-1671.
Guo S, Huang J, Jiang H, Han C, Li J, Xu X, et al. Restless legs syndrome: from pathophysiology to clinical diagnosis and management. Front Aging Neurosci. 2017;9:1–14.
Kamal M, Tamana SK, Smithson L, Ding L, Lau A, Chikuma J, et al. Phenotypes of sleep-disordered breathing symptoms to two years of age based on age of onset and duration of symptoms. Sleep Med. 2018;48:93–100. https://doi.org/10.1016/j.sleep.2018.04.008.
Ansari S, Hu A. Knowledge and confidence in managing obstructive sleep apnea patients in Canadian otolaryngology - head and neck surgery residents: a cross sectional survey. J Otolaryngology - Head & Neck Surgery. 2020;49:1.
Lau A, Ewing C, Gnanapragasam J, Majaesic C, MacLean J, Mandhane PJ. Changes to a pediatric sleep disordered breathing clinic improve wait-times and clinic efficiency. Pediatr Pulmonol. 2016;51(11):1234–41. https://doi.org/10.1002/ppul.23440.
Katz SL, Witmans M, Barrowman N, Hoey L, Su S, Reddy D, et al. Paediatric sleep resources in Canada: the scope of the problem. Paediatr Child Health. 2014;19(7):367–72. https://doi.org/10.1093/pch/19.7.367.
Marcus CL, Moore RH, Rosen CL, Giordani B, Garetz SL, Taylor HG, et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med. 2013;368(25):2366–76. https://doi.org/10.1056/NEJMoa1215881.
Nixon GM, Kermack AS, Davis GM, Manoukian JJ, Brown KA, Brouillette RT. Planning Adenotonsillectomy in children with obstructive sleep apnea: the role of overnight Oximetry. Pediatrics. 2004;113(1):e19–25. https://doi.org/10.1542/peds.113.1.e19.
Hang L-W, Wang H-L, Chen J-H, Hsu J-C, Lin H-H, Chung W-S, et al. Validation of overnight oximetry to diagnose patients with moderate to severe obstructive sleep apnea. BMC Pulmonary Med. 2015;15(1):1–13.
Ng SK, Lee DL, Li AM, Wing YK, Tong MC. Reproducibility of clinical grading of tonsillar size. Archives of Otolaryngology–Head & Neck Surgery. 2010;136(2):159–62. https://doi.org/10.1001/archoto.2009.170.
Chervin RD, Hedger K, Dillon JE, Pituch KJ. Pediatric sleep questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000;1(1):21–32. https://doi.org/10.1016/S1389-9457(99)00009-X.
Ishii L, Godoy A, Ishman SL, Gourin CG, Ishii M. The nasal obstruction symptom evaluation survey as a screening tool for obstructive sleep apnea. Arch of Otolaryngology–Head & Neck Surg. 2011;137(2):119–23. https://doi.org/10.1001/archoto.2010.251.
Tang A, Benke JR, Cohen AP, Ishman SL. Influence of Tonsillar Size on OSA Improvement in Children Undergoing Adenotonsillectomy. Otolaryngol Head Neck Surg. 2015;153(2):281–5.
Liu CC, Chaput KH, Kirk V, Yunker W. Overnight oximetry in children undergoing adenotonsillectomy: a single center experience. J Otolaryngology - Head & Neck Surgery. 2019;48:1.
Acknowledgements
Thank you for the children and families who participated in this research.
Funding
This research has been funded by the generous support of the Stollery Children’s Hospital Foundation through the Women and Children’s Health Research Institute at the University of Alberta.
Author information
Authors and Affiliations
Contributions
DSH and PJM conceived and designed the study, analyzed the data, and drafted this manuscript. HE, YA, EE, TCU, AI, MC, CG, and JM contributed to revising the manuscript. All authors were involved in manuscript preparation and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the local institutional review board (Pro00089369) and all of the participants parents consented to have their child’s medical information used for research purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare one competing interest. Author AI is a peer-reviewer for the Journal of Otolaryngology - Head & Neck Surgery.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Contains an additional triage model that uses oximetry data alone.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Heath, D.S., El-Hakim, H., Al-Rahji, Y. et al. Development of a pediatric obstructive sleep apnea triage algorithm. J of Otolaryngol - Head & Neck Surg 50, 48 (2021). https://doi.org/10.1186/s40463-021-00528-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40463-021-00528-8