Abstract
Background
Existing guidelines do not offer a quick, efficient alternative to the patient’s recollection of relevant clinical features during anamnesis and physical examination for chronic urticaria (CU). This study aimed to identify specific items reflecting the main characteristics of CU that should be included in a comprehensive medical history for patients with CU. We also aimed to clarify possible eliciting factors for CU to support accurate diagnosis of the disease.
Methods
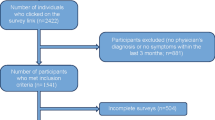
A panel of postgraduate dermatologists conducted a literature search for relevant studies on CU using Medline, the Cochrane database, and PubMed.
Results
We identified82 articles from which we drew a collection of items to inform development of an easy-to-use checklist and collection of items that should be included in a correct medical history. The final version of the checklist included42 items across two areas: essential clues for anamnesis and diagnosis of CU; and typical symptoms/parameters or characteristics according to subtype, etiology, and laboratory findings. Items included time of disease onset; duration, shape, size, color, and distribution of wheals; associated angioedema; atopy; and triggering factors.
Conclusions
Our guide provides an easy-to-use tool to support clinicians to focus, orient themselves, and save time in medical consultations for CU, allowing better diagnosis and management of this disease.
Similar content being viewed by others
Background
Urticaria is characterized by the development of wheals (hives), angioedema, or both [1]. Three common features of wheals are swelling and erythema, itching/burning sensations, and transient nature with the skin returning to a normal appearance within 1–24 h [2]. Angioedema is characterized by sudden localized, pronounced erythematous or skin-colored swelling of the lower dermis and subcutis, with frequent involvement below mucous membranes and sometimes pain rather than itching. Angioedema is slower to resolve than wheals, and can take up to 72 h [1, 3].
The prevalence of CU in the general population ranges from 0.5–5%, with the incidence of CU in Western countries estimated at 1.4% per year [1]. In Spain, CU ranks fourth among the allergic diseases after rhinitis, asthma, and drug allergy [4];the prevalence of CU is 0.6%, and is significantly higher in women than men. The average age of onset is 40 years [5]. A study in the United Kingdom showed that the prevalence of all forms of urticaria was 8.8% [4]. In Italy, the prevalence of chronic spontaneous urticaria (CSU) was 0.38% in 2013, with an incidence of 0.10–1.50 per 1000 person-years; female patients outnumbered males in both prevalence and incidence rates [6]. An Argentine guideline for urticaria and angioedema indicates 20% of the population have urticaria at some point in their life [7]. However, the point prevalence, cumulative prevalence, and lifetime prevalence of chronic urticaria (CU) in Latin America have not yet been established.
Urticaria is classified into two major types according to duration: acute urticaria (<6 weeks) and CU (≥6 weeks) [2]. For clinical purposes, CU is further classified into two subtypes: CSU and inducible urticaria (CINDU). CSU is characterized by the spontaneous appearance of wheals, angioedema, or both, resulting from unidentified causes and physiopathology that is not fully understood. Currently, the only identified aggravating factor is nonsteroidal anti-inflammatory drugs (NSAIDs). CSU also has spontaneous remission, making it difficult to prove cause-effect relationships.
There is a subgroup of CSU patients (40%) who has autoantibodies against the FcεRI, the high affinity receptor for IgE, that can stimulate and activate mast cells. The presence of these autoantibodies may be clinically important in a group of severely affected, treatment-resistant patients, where immunomodulatory treatments may be valuable. Patients with autoantibodies have no distinctive diagnostic clinical features. However, they do tend to have more severe urticaria [8].
In contrast, CINDU has known triggering stimuli, which can be classified as symptomatic dermographism, caused by cold, delayed pressure, sunlight, heat, vibration, cholinergic, contact, or water [1]. There is often an overlap between CSU and CINDU (e.g., a factitious component in CSU), and there is a tendency to sub-summarize both forms as CU [9].
We included urticarial vasculitis (UV) in this study. UV is not a form of CU, however is necessary to exclude it in patients with CU. In UV, the lesions are painful, burning, and tender, with plaques lasting for more than 24 h (sometimes up to 72 h). The wheals are associated with residual purpura or hyperpigmentation, and can have a central dark red or brown macule signifying underlying purpura and vasculitis. Other characteristics of UV are swelling, residual bruising, and edema from focused pressure; in such cases, skin biopsy would confirm or reject the diagnosis [10,11,12,13]. A study in Ecuador found that 10% of the population has UV [14].
This study aimed to determine a collection of items covering the main characteristics of CU that should be included in a comprehensive medical history to support thorough anamnesis and physical examination. We also evaluated possible eliciting factors of CU to aid accurate diagnosis of the disease and obtain comprehensive information on each patient that will then allow to select the best approach for treatment.
It is important to emphasize that this collection of items should not limit physical examination findings, which can vary and include features of other forms of urticaria; however, it provides a way to orient physicians in thinking about CU.
Methods
For the purpose of this study, a panel of postgraduate dermatologists conducted a literature search. Inclusion criteria were: studies on the approach for patients with urticaria, anamnesis, physical examination, clinical features, characterization of lesions, and factors triggering CU; studies in English and Spanish; and articles published before 2016. Databases searched included Medline, the Cochrane database, and PubMed. Studies about the prevalence and treatment of CU were excluded.
The criterion used to identify relevant items was specific patterns or features of lesions described in the selected studies that correlated with the forms of CU. For example, localized hives appearing after a temperature change (cold or heat urticaria), and those induced by pressure (e.g., delayed pressure urticaria).
These items were included in the first draft and subsequently, a medical history was performed. A new revision and agreement between authors was done until the final version of the checklist was designed.
Results
In total, 82 articles were selected and used to develop a 42-item checklist for taking a comprehensive medical history for CU. The guide and checklist are presented in Additional files 1 and 2. Checklist items covered two main areas:
-
1.
Essential features for anamnesis and diagnosis of CU.
-
2.
Typical symptoms/parameters or characteristics according to CU subtype, etiology, and laboratory findings.
Checklist items included:
-
1.
Time of disease onset
-
Very rapid (less than 2 h): CINDU: dermographism, 6–7 min; cold urticaria, 2–5 min; heat urticaria, a few minutes to hours [15]; aquagenic urticaria, 5–10 min [16]; urticaria from exercise, 6–25 min [17]; cholinergic urticaria, 6–25 min [17]; vibratory angioedema, 2–30 min; and solar urticaria, 2–15 min [18].
-
More than 2 h: Pressure urticaria, 4–8 h [19].
-
-
2.
Duration of wheals
-
Less than 24 h: CINDU (<2 h), which includes dermographism (<30 min), aquagenic urticaria (<60 min) [16], solar urticaria (<60 min) [18], contact urticaria (2 h), and the majority of urticaria subtypes.
-
More than 24 h: Pressure urticaria(24 h) [19]; UV(often 2–3 days, and may leave bruising) [2, 20].
-
-
3.
Shape, size, color, and distribution of wheals
-
Size 1–5 mm: cholinergic urticaria, heat urticaria, solar urticaria [21]. Greater than 5 mm: cold urticaria, chronic autoimmune urticaria. Coalescent: pressure urticaria [22]. Heat urticaria, solar and cold urticaria can come with small or large wheals depending on the area of skin that is exposed to the trigger.
-
Shape: UV courses with petechiae/ecchymosis, livedo reticularis/Raynaud’s phenomenon, and sometimes blisters [23, 24].
-
Color: erythematous (most hives); yellowish to red brown, urticaria pigmentosa (mastocytosis) [25]; erythematous with whitish halo, aquagenic urticaria [16] and CSU; purpuric, UV [23].
-
Distribution: CINDU from pressure, solar and dermographic stimuli share a localized distribution [17]. Pressure and dermographic urticaria involve feet, hands, buttocks, and shoulders; cold, heat, and solar urticaria affect exposed areas; UV mostly affects the lower limbs [2, 17, 19]. Otherwise, cholinergic urticaria can be generalized (with a predilection for the trunk and upper extremities).Cold urticaria can be generalized if the entire skin is exposed to cold.
-
-
4.
Onset symptoms
Dermographic urticaria can sometimes begin with erythema and hives [26]. Cold urticaria presents with erythema, edema, and pruritus at onset. Pruritus, edema, and burning in pressure urticaria, cold urticaria and UV [17, 24].
-
5.
Associated angioedema
Through inherited deficiency of C1 esterase inhibitor, maybe localized or generalized; triggered by physical trauma, stress, drugs, or food; gastrointestinal compromise (angioedema) [27]. Typically, hereditary angioedema is not associated with urticarial skin lesions.
-
6.
Associated subjective symptoms of lesions
Itching, pain, and burning in pressure urticaria and UV. Burning in UV [23] and cold urticaria [28].
-
7.
Family and personal history regarding urticaria and atopy
Some reports mention a marked prevalence of atopy in CSU and CINDU, with the most common cases being allergic asthma, rhinitis, and contact allergy [29, 30].
-
8.
Provoking factors for wheals
-
Physical stimuli in CINDU: Cold (cold urticaria); heat (heat urticaria); sunlight (solar urticaria); water (aquagenic urticaria); pressure (pressure urticaria), machines that transmit vibration such as mixers or pruners (vibratory urticaria); rubbing (dermographic urticaria); physical exercise (cholinergic urticaria); and stress (CSU). Surgical implantations and events during surgery: implants, intrauterine contraceptive devices [31], surgical clips, metal prostheses [32], orthopedic implants [33], femoral prosthesis (e.g., Smith-Petersen Vitallium nail) [34]
-
Infections: The association between infections and urticaria can be considered more direct in cases where urticaria disappears after treatment of infection. The role of infections in chronic urticaria as a causative agent in CU is still controversial however in a systematic review has been reported as an etiologic in approximately 6% of cases [35]. Identified etiologic agents are: bacteria (Streptococcus spp., Staphylococcus spp., Yersinia, Helicobacter pylori, Treponema pallidum); viruses(hepatitis B and C, cytomegalovirus, Epstein-Barr virus, norovirus); parasites,(Blastocystishominis, Giardia lamblia [adults], Toxocara canis [children], Strongyloides stercoralis, Trichinella, Trichomonas vaginalis, Anisakis, Enterobius vermicularis [pinworms]) [36]; and fungi (candidiasis, dermatophytosis) [35].
-
Contact: latex, nickel, animals, steam cooking, perfumes, and pollens (rare cases reported) [1, 9].
-
-
9.
Diurnal and nocturnal variation
Pruritus of urticaria in children and adults displays extensive temporal variability. It is worse nocturnally in chronic urticaria, often disturbing sleep, and is bothersome to a lesser extent upon awakening [38]. Recent findings suggest the circadian clock is an important regulatory component of local and systemic allergic reactions [39, 40].
-
10.
Psychosomatic and psychiatric diseases
Mainly anxiety and depression [41]. Patients with CU have higher scores in both the Beck Depression Inventory and the Beck Anxiety Inventory [42]. In addition, a reduction of productivity may be caused by sleep interference [43].
-
11.
Gastric/intestinal problems
Patients with symptoms of dyspepsia should undergo to a routine test to screen for H. pylori. Although H. pylori eradication has no discernible effects on CSU beyond that of standard CSU therapy, H. pylori eradication should only be initiated in accordance with currently accepted indications in its treatment guidelines [44].
-
12.
Relationship to the menstrual cycle
Menstrual Cycle is an aggravating factor in CSU. A rare form of urticaria is related to the menstrual cycle, appearing 7–10 days before menstruation [45, 46]. There are also pruritic urticarial papules and plaques of pregnancy occurring postpartum, related to skin stretching in the third trimester of pregnancy and characterized by the abrupt eruption of intensively pruritic papules (1–2 mm) that can coalesce to form plaques. These lesions spread over the distended abdomen [47].
-
13.
Smoking habits (especially use of perfumed tobacco products or cannabis)
Agents such as tobacco may aggravate CU [48].
-
14.
Type of work
Particularly vulnerable populations include healthcare workers, hairdressers, and food handlers [49]. Other vulnerable occupations are agricultural, dairy, and veterinary workers [50]. CU has also been reported during exposure to cyclic anhydrides (plumbers, packers, and painters) [51].
-
15.
Previous diagnostic procedures/results
Routine screening for malignancies in the diagnosis of underlying causes for urticaria is not suggested; however, if underlying causes are suspected, further research is necessary [1]. A prevalence of at least one anti-thyroid antibody has been described in 20% of patients with CSU, and is associated with more severe and prolonged urticaria progression. Urticaria has also been described as an initial finding for a patient with a carcinoid tumor [52]. Physicians should consider the possibility of neuroendocrine malignancies (specifically type I carcinoid tumors) when evaluating patients with rare urticaria presentations [52].
Discussion
Physicians must promptly detect problems to successfully weigh the importance of findings in clinical settings and react appropriately. A thorough history and physical examination to identify all possible eliciting factors and causes of CU are important for diagnosis [53].
International guidelines for the diagnosis and management of CU are available, with most recommending diagnostic procedures when a doctor has a clinical suspicion of CU. These existing guidelines provide example recommendations to differentiate between CSU, CINDU, and other differential diagnoses, and to measure disease activity and impact. However, they do not offer a quick or efficient alternative to a patient’s recollection of relevant clinical features during anamnesis and physical examination. Most existing guidelines are general, and not particularly useful for clinical practice and informing oriented history-taking in the first doctor-patient meeting.
Physicians need an easy-to-use tool that helps them to quickly and easily diagnose this pathology. Therefore, this checklist has general and specific parameters ordered according to the sequence of a comprehensive clinical history. In addition, the checklist is able to be used by physicians independent of specialty (e.g., emergency rooms, primary care, internal medicine, and allergy and dermatology departments) without causing confusion as to the various differential diagnoses. The checklist will also contribute to the proper management of patients with CU from the start of clinical occurrence, achieving better control of the disease and reducing its social and economic impact. Delay in diagnosis statistically significantly increases severity, correspondingly increasing healthcare costs (specifically outpatient visit costs) and wages lost because of absences from work [8].
We developed an easy-to-use tool to support the early correct diagnosis and management of CU and facilitate healthcare providers/physicians’ diagnostic workup, clinical approach and allow to select the best approach for treatment in patients with CU.
To our knowledge, this is the first checklist available for diagnostic workup and management of patients with CU since 2010. In 2014, a clinical history of CU was published that provided a model for questions directed to patients suspected of this pathology [14]. However, that model did not cover specific features important in the clinical diagnosis of CU subtypes (such as color, characteristics of lesions, distribution of wheals, associated symptoms, and other possible etiologic agents), and did not include supporting evidence for each question as detailed in the present checklist [3, 14, 54].
In the last 30 years, attention has been focused on new ways to understand and manage urticaria. This includes the recent addition of novel drugs to the therapeutic arsenal, updating of clinical practice guidelines, and publication of pathophysiologic insights. Three decades ago, it would not have been possible to develop easy-to-use clinical guidance such as that developed here.
There are some limitations to our checklist. First, in CU, etiology is a major challenge for physicians because the frequency and relevance of infectious diseases vary among patient groups and geographical regions. We recommend further research to develop specific tools adapted to the context of each country. In addition, our study does not provide a “real-world” evaluation of the checklist or its impact. The present study did not intend to validate the role of our checklist in the medical history; consequently, face validity and reliability need to be established in a future study. Future studies should also evaluate the usefulness of this checklist. The initial version of the checklist was in Spanish, and it is also necessary to explore the usefulness of the checklist in other languages. A final limitation is that the checklist may be considered too long for some physicians. However, the length of the checklist is justified by relevant parameters that cannot be omitted from a clinical history for a patient with CU.
A strength of our study was that we performed an extended literature search to identify semiological and interrogatory characteristics that permitted our checklist to include all items necessary to collect comprehensive information from patients with CU. In a previous study, we found that knowledge of guideline recommendations among physicians who treat patients with urticaria in Ecuador was low [55]. The diagnostic workup and treatment of patients with CU was largely inconsistent with guideline recommendations in actual practice settings. The development of our checklist will help physicians to collect important patient medical data and facilitate workup and diagnosis. In future, it may also support collaboration in increasing knowledge about CU and its actual frequency, as data about the prevalence of CU are not available in Latin America [7].
Conclusions
Urticaria consultations can be frustrating for both patients and physicians, because lesions may persist, factors that elicit urticaria are confusing, and there is a risk of misdiagnosis. The easy-to-use checklist developed in the present study should be adapted to the context of each country to reflect the most common CU etiology. Finally, this checklist will help focus and orient physicians, and save time in medical consultations, allowing physicians to perform better diagnosis and management of this disease.
Abbreviations
- CINDU:
-
Chronic Inducible urticaria
- CSU:
-
Chronic spontaneous urticaria
- CU:
-
Chronic Urticaria
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- UV:
-
Urticarial vasculitis
References
Zuberbier T, Aberer W, Asero R, Bindslev-Jensen C, Brzoza Z, Canonica GW, Church M, Ensina L, Giménez-Arnau A, Godse K, et al. The EAACI/GA2LEN/EDF/WAO guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update. Allergy. 2014;69:868–87.
Vestergaard C, Deleuran M. Chronic spontaneous urticaria: latest developments in aetiology, diagnosis and therapy. Ther Adv Chronic Dis. 2015;6:304–13.
Beck LA, Bernstein JA, Maurer M. A review of international recommendations for the diagnosis and management of chronic Urticaria. Acta Derm Venereol. 2017;97:149–58.
Champion RH, Roberts SOB, Carpenter RG, Roger JH. Urticaria and angio-oedema. Br J Dermatol. 1969;81:588–97.
Gaig P, Olona M, Lejarazu DM, Caballero M, Domínguez F, Echechipia S, Abujeta JG, Gonzalez M, Lleonart R, Cócera CM. Epidemiology of urticaria in Spain. J Investig Allergol Clin Immunol. 2004;14:214–20.
Lapi F, Cassano N, Pegoraro V, Cataldo N, Heiman F, Cricelli I, Levi M, Colombo D, Zagni E, Cricelli C. Epidemiology of chronic spontaneous urticaria: results from a nationwide, population-based study in Italy. Br J Dermatol. 2016;174:996–1004.
Máspero J, Cabrera H, Ardusso L, De Gennaro M, Fernández Bussy R, Galimany J, Galimberti D, Label M, La Forgia M, Medina I. Guía Argentina de urticaria y angioedema. Medicina (Buenos Aires). 2014;74:1–53.
Larenas Linnemann D, Medina Ávalos MA, Ortega Martell JA, Beirana Palencia AM, Rojo Gutiérrez MI, Morales Sánchez MA, Solorio Gómez H, MdL A-RP, Vargas Correa JB, Baez Loyol C. Guía Mexicana para el Diagnóstico y el Tratamiento de la Urticaria. Rev Alerg Mex. 2014;61:117–93.
Bernstein JA, Lang DM, Khan DA, Craig T, Dreyfus D, Hsieh F, Sheikh J, Weldon D, Zuraw B, Bernstein DI. The diagnosis and management of acute and chronic urticaria: 2014 update. J Allergy Clin Immunol. 2014;133:1270–7. e1266
Mehregan DR, Hall MJ, Gibson LE. Urticarial vasculitis: a histopathologic and clinical review of 72 cases. J Am Acad Dermatol. 1992;26:441–8.
Jachiet M, Flageul B, Deroux A, Le Quellec A, Maurier F, Cordoliani F, Godmer P, Abasq C, Astudillo L, Belenotti P. The clinical Spectrum and therapeutic Management of Hypocomplementemic Urticarial Vasculitis: data from a French Nationwide study of fifty-seven patients. Arthritis Rheumatol. 2015;67:527–34.
Dahl MV. Clinical pearl: diascopy helps diagnose urticarial vasculitis. J Am Acad Dermatol. 1994;30:481–2.
Venzor J, Lee WL, Huston DP. Urticarial vasculitis. Clin Rev Allergy Immunol. 2002;23:201–16.
Weller K, Zuberbier T, Maurer M. Chronic urticaria: tools to aid the diagnosis and assessment of disease status in daily practice. J Eur Acad Dermatol Venereol. 2015;29:38–44.
Pezzolo E, Peroni A, Gisondi P, Girolomoni G. Heat urticaria: a revision of published cases with an update on classification and management. Br J Dermatol. 2016;175:473–8.
Rothbaum R, McGee JS. Aquagenic urticaria: diagnostic and management challenges. J Asthma Allergy. 2016;9:209–13.
Montgomery SL. Cholinergic Urticaria and exercise-induced anaphylaxis. Current Sports Medicine Reports. 2015;14:61–3.
Pérez-Ferriols A, Barnadas M, Gardeazábal J, de Argila D, Carrascosa J, Aguilera P, Giménez-Arnau A, Rodríguez-Granados T, de Gálvez M, Aguilera J. Urticaria solar. Epidemiología y fenotipos clínicos en una serie española de 224 pacientes. Actas Dermo-Sifiliográficas. 2017;108:132–9.
Cassano N, Mastrandrea V, Vestita M, Vena G. An overview of delayed pressure urticaria with special emphasis on pathogenesis and treatment. Dermatol Therapy. 2009;22:S22–S26. doi:10.1111/j.1529-8019.2009.01268.x.
Gimenez-Arnau A, Maurer M, De La Cuadra J, Maibach H. Immediate contact skin reactions, an update of contact Urticaria, contact Urticaria syndrome and protein contact dermatitis -- "a never ending story". Eur J Dermatol. 2010;20:552–62.
Bindslev-Jensen C, Finzi A, Greaves M, Camarasa J, Ortonne JP, Schöpf E, Tennstedt D. Chronic urticaria: diagnostic recommendations. J Eur Acad Dermatol Venereol. 2000;14:175–80.
Beltrani VS. Urticaria: reassessed. Allergy Asthma Proc. 2004;25:143–9.
Davis MDP, Brewer JD. Urticarial vasculitis and hypocomplementemic urticarial vasculitis syndrome. Immunol Allergy Clin N Am. 2004;24:183–213.
Schaefer P. Urticaria: evaluation and treatment. Am Fam Physician. 2011;83:1078–84.
Bulat V, Mihic LL, Situm M, Buljan M, Blajic I, Pusic J. Most common clinical presentations of cutaneous mastocytosis. Acta Clin Croat. 2009;48:59–64.
Schoepke N, Doumoulakis G, Maurer M. Diagnosis of urticaria. Indian J Dermatol. 2013;58:211–8.
Sánchez-Borges M, Asero R, Ansotegui IJ, Baiardini I, Bernstein JA, Canonica GW, Gower R, Kahn DA, Kaplan AP, Katelaris C, et al. Diagnosis and treatment of Urticaria and angioedema: a worldwide perspective. World Allergy Organization Journal. 2012;5:125.
Singleton R, Halverstam CP. Diagnosis and management of cold urticaria. Cutis. 2016;97:59–62.
Sánchez J, Amaya E, Acevedo A, Celis A, Caraballo D, Cardona R. Prevalence of inducible Urticaria in patients with chronic spontaneous Urticaria: associated risk factors. J Allergy Clin Immunol Pract. 2017;5:464–70.
Altrichter S, Koch K, Church M, Maurer M. Atopic predisposition in cholinergic urticaria patients and its implications. J Eur Acad Dermatol Venereol. 2016;30:2060–5.
Dry J, Leynadier F, Bennani A, Piquet P, Salat J. Intrauterine copper contraceptive devices and allergy to copper and nickel. Annals of allergy. 1978;41:194.
Lyell A. Metal allergy and metallic prostheses. Int J Dermatol. 1979;18:805–7.
Kubba R, Taylor JS, Marks KE. Cutaneous complications of orthopedic implants: a two-year prospective study. Arch Dermatol. 1981;117:554–60.
McKenzie AW, Aitken CV, Ridsdill-Smith R. Urticaria after insertion of smith-Petersen Vitallium nail. Br Med J. 1967;4:36–7.
Wedi B, Raap U, Kapp A. Chronic urticaria and infections. Curr Opin Allergy Clin Immunol. 2004;4:387–96.
Wedi B, Raap U, Wieczorek D, Kapp A. Infektfokus und chronische spontane Urtikaria. Hautarzt. 2010;61:758–64.
Chérrez Ojeda I, Loayza E, Greiding L, Calderón JC, Cherrez A, Adum F. Urticarial vasculitis induced by OTC diet pills: a case report. World Allergy Organ J. 2015;8:12.
Smolensky MH, Portaluppi F, Manfredini R, Hermida RC, Tiseo R, Sackett-Lundeen LL, Haus EL. Diurnal and twenty-four hour patterning of human diseases: acute and chronic common and uncommon medical conditions. Sleep Med Rev. 2015;21:12–22.
Nakao A. Circadian regulation of urticaria and anaphylaxis. Nihon Rinsho Japanese J Clin Med. 2013;71:2153–7.
Maurer M, Ortonne JP, Zuberbier T. Chronic urticaria: an internet survey of health behaviours, symptom patterns and treatment needs in European adult patients. Br J Dermatol. 2009;160:633–41.
Tsintsadze N, Beridze L, Tsintsadze N, Krichun Y, Tsivadze N, Tsintsadze M. Psychosomatic aspects in patients with dermatologic diseases. Georgian Med News. 2015;70
O'Donnell B, Lawlor F, Simpson J, Morgan M, Greaves M. The impact of chronic urticaria on the quality of life. Br J Dermatol. 1997;136:197–201.
Thompson AK, Finn AF, Schoenwetter WF. Effect of 60 mg twice-daily fexofenadine HCl on quality of life, work and classroom productivity, and regular activity in patients with chronic idiopathic urticaria. J Am Acad Dermatol. 2000;43:24–30.
Curth H-M, Dinter J, Nigemeier K, Kütting F, Hunzelmann N, Steffen H-M. Effects of helicobacter pylori eradication in chronic spontaneous urticaria: results from a retrospective cohort study. Am J Clin Dermatol. 2015;16:553–8.
Farah FS, Shbaklu Z. Autoimmune progesterone urticaria. J Allergy Clin Immunol. 1971;48:257–61.
Deacock SJ. An approach to the patient with urticaria. Clin Exp Immunol. 2008;153:151–61.
Stöckli SS, Bircher AJ. Generalized pruritus in a patient sensitized to tobacco and cannabis. JDDG: Journal der Deutschen Dermatologischen Gesellschaft. 2007;5:303–4.
Williams J, Lee A, Matheson MC, Frowen K, Noonan A, Nixon R. Occupational contact urticaria: Australian data. Br J Dermatol. 2008;159:125–31.
Burns T, Breathnach S, Cox N, Griffiths C. Rook's Textbook of Dermatology. 8th ed.: Wiley-Blackwell Publishers; c2013. p. 4432, ISBN: 978-1-118-69775-7.
Helaskoski E, Kuuliala O, Aalto-Korte K. Occupational contact urticaria caused by cyclic acid anhydrides. Contact Dermatitis. 2009;60:214–21.
Madgaonkar, CS. Diagnosis: A System-Based Approach in Internal Medicine, 1st ed. India: Jaypee Brothers Medical Publishers; c2011. ISBN 13:9789380704753.
DeLong LK, Culler SD, Saini SS, Beck LA, Chen SC. Annual direct and indirect health care costs of chronic idiopathic urticaria: a cost analysis of 50 nonimmunosuppressed patients. Arch Dermatol. 2008;144:35–9.
Kulthanan K, Tuchinda P, Chularojanamontri L, Chanyachailert P, Korkij W, Chunharas A, Wananukul S, Limpongsanurak W, Benjaponpitak S, Wisuthsarewong W. Clinical practice guideline for diagnosis and management of urticaria. Asian Pac J Allergy Immunol. 2016;34:190.
Maurer M, Weller K, Bindslev-Jensen C, Giménez-Arnau A, Bousquet P, Bousquet J, Canonica G, Church M, Godse K, Grattan C. Unmet clinical needs in chronic spontaneous urticaria. A GA2LEN task force report. Allergy. 2011;66:317–30.
Cherrez-Ojeda I, Tafur A, Cazar T, Uraga E, Mantilla R, Guerrero T, Chica L, Soria J. Diagnóstico de urticaria crónica en Guayaquil. Archivos de alergia e inmunología clínica. 2007;38:73–8.
Acknowledgements
We acknowledge the following people who worked on the first version of the checklist: Vladimir Preciado, MD; Gladys Zambrano, MD; María Seminario MD; María Arevalo, MD; Analia Pasquel, MD; and Silvania Naranjo, MD.
Dr. Ivan Cherrez Ojeda is a candidate in the Doctorate Program of Biomedical Research and Public Health, at the Universitat Autonoma de Barcelona. The authors acknowledge the guidance and knowledge imparted by the MECOR Program, especially Sonia Buist, MD, and Ana Menezes, MD, for their guidance and support over many years. We also thank the Respiralab team for their day-to-day support, especially Juan Calderon, MD. Finally, We thank Audrey Holmes, MA, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Funding
This study was partially supported by an unrestricted grant from the Universidad de Especialidades Espíritu Santo. The sponsor had no role in the design of the study or in the collection, analysis, and interpretation of data.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
CHOI, RVK, and BRP developed the research question and participated in the data collection process. CHOI, in coordination with CHS, CF, CE, and CHA performed the analysis. CHOI, RVK, BRF, SGP, and BTP wrote the manuscript and, CE and CHA checked for grammatical and syntax errors in English. All authors approved this manuscript before submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Chronic urticaria medical history (DOCX 2047 kb)
Additional file 2:
Checklist for a complete chronic urticaria medical history (DOCX 1489 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Cherrez-Ojeda, I., Robles-Velasco, K., Bedoya-Riofrío, P. et al. Checklist for a complete chronic urticaria medical history: an easy tool. World Allergy Organ J 10, 34 (2017). https://doi.org/10.1186/s40413-017-0165-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40413-017-0165-0