Abstract
Background
Children with birth defects (BD) are more likely to develop cancer and the increased risk of cancer persists into adulthood. Prior population-based assessments have demonstrated that even non-chromosomal BDs are associated with at least two-fold increase of cancer risk. Identification of variants that are associated with malignant tumor in BD patients without chromosomal anomalies may improve our understanding of the underlying molecular mechanisms and provide clues for early cancer detection in children with BD.
Methods
In this study, whole genome sequencing (WGS) data of blood-derived DNA for 1653 individuals without chromosomal anomalies were acquired from the Kids First Data Resource Center (DRC), including 541 BD probands with at least one type of malignant tumors, 767 BD probands without malignant tumor, and 345 healthy family members who are the parents or siblings of the probands. Recurrent variants exclusively seen in cancer patients were selected and mapped to their corresponding genomic regions. The targeted genes/non-coding RNAs were further reduced using random forest and forward feature selection (ffs) models.
Results
The filtered genes/non-coding RNAs, including variants in non-coding areas, showed enrichment in cancer-related pathways. To further support the validity of these variants, blood WGS data of additional 40 independent BD probands, including 25 patients with at least one type of cancers from unrelated projects, were acquired. The counts of variants of interest identified in the Kid First data showed clear deviation in the validation dataset between BD patients with cancer and without cancer. Furthermore, a deep learning model was built to assess the predictive abilities in the 40 patients using variants of interest identified in the Kids First cohort as feature vectors. The accuracies are ~ 75%, with the noteworthy observation that variants mapped to non-coding regions provided the highest accuracy (31 out of 40 patients were labeled correctly).
Conclusion
We present for the first time a panorama of genetic variants that are associated with cancers in non-chromosomal BD patients, implying that our approach may potentially serve for the early detection of malignant tumors in patients with BD.
Similar content being viewed by others
Background
Birth defects (BD) affect 1 in every 33 babies (~ 3%) born in the United States each year based on the statistics by the Centers for Disease Control and Prevention (CDC, https://www.cdc.gov/ncbddd/birthdefects/index.html ). BDs contribute to long-term disability, which takes a significant toll on affected individuals, families, health care systems and societies world-widely (https://www.who.int/news-room/fact-sheets/detail/birth-defects ). Risk of cancer is significantly increased in BD patients with either non-chromosomal or chromosomal anomalies [1]. Based on a population-based assessment of 10 million live births, children with chromosomal anomalies are over 11 times more likely to be diagnosed with cancer compared with children without any BD, and the likelihood for children with non-chromosomal BD increases 2.5-fold [2]. Accordingly, the cancer risk in BD children with non-chromosomal anomalies cannot be neglected considering the large effect size.
The co-occurrence of BD in patients with pediatric cancer may share common nexus in the gene pathways governing signal transduction and cell growth, e.g., the Wnt signaling pathway [3]. Unfortunately, few pathways or corresponding genes/variants have been identified in this context due to limited research efforts. Based on the multi-hit theory of childhood cancer [4], the efforts in this study focused on identifying genomic mutations, in both coding and non-coding regions, which are enriched in BD patients with cancers compared to BD patients without cancers based on the Whole Genome Sequencing (WGS) analysis. In this regard, we assembled one of the largest pediatric oncology and birth defect projects in children, as a part of the Gabriella Miller Kids First program project (https://kidsfirstdrc.org/). The major objective was to identify the functional molecular pathways and evaluate the performance of risk prediction with genomic information based on the mutations identified.
Methods
Discovery and validation cohorts
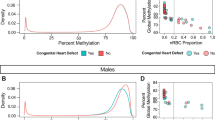
The patients with or without co-occurrence of pediatric onset cancers were selected from the Center for Applied Genomics (CAG) Biorepository for birth defects (BD). The BD and cancer diagnosis were based on the International Classification of Diseases (ICD) codes ICD-9 and ICD-10. All the CAG patients were recruited at the Children’s Hospital of Philadelphia (CHOP) and coupled to Electronic medical records (EMRs) of CHOP established in 2003. Altogether, 1308 probands with non-chromosomal anomalies were studied, including 541 BD patients with at least one type of malignant tumors and 767 BD patients without any known cancers. In addition, 345 healthy controls without BD or cancer who are parents/siblings of the probands were also investigated in comparison (Fig. 1a). The patients’ counts for malignant cancers and demographic information including gender and ethnicities were shown in Fig. 1c and d.
The patients in the validation dataset were also recruited by CAG at CHOP, including research participants who had undergone WGS through the NHLBI Trans Omics for Precision Medicine (TOPMed) Program (https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs001661.v2.p1) in a different project. In total, 40 BD patients were identified in the CAG biobank, including 25 with at least one type of cancer diagnosis (Fig. 1b).
All the patients were recruited during regular hospital visits at multiple clinics, including the emergency room, ambulatory settings or surgical settings, through the general pediatric clinics or CHOP’s specialty pediatric practices. The patients were in the age range of 0–21 years and receiving health care at CHOP. Parental consent was obtained for individuals under 18 years of age and assent was also obtained for subjects aged 7–17 years. The consent allows samples to be obtained and analyzed using the genomic technologies included herein, to address the research questions proposed.
Electronic medical record (EMR) and electronic health record (EHR) data
CAG at CHOP maintains a de-identified extract of clinical data from the CHOP EMR and EHR databases of consented patients. This database contains longitudinal information about visits, diagnoses, medical history, prescriptions, procedures, and lab tests with all information coded and de-identified. For this study the health status of de-identified individuals was classified based on the International Classification of Diseases (ICD) codes (ICD-9 and ICD-10) associated with clinical visits and entered in the medical health record.
Processing and variant detection by WGS
Whole genome sequencing (WGS) was done at 30X coverage for the 1653 individuals from the Gabriella Miller Kids First project, by the genomics platform of the Broad Institute. The variant call format (VCF) files of WGS were generated using the Illumina DRAGEN (Dynamic Read Analysis for GENomics) Bio-IT Platform (Illumina, San Diego, CA), aligned to the GRCh38/hg38 human genome assembly. For the validation dataset, WGS VCF files of participating individuals were extracted from the TOPMED database directly. The annotations for the variants were generated using the ANNOVAR software developed by our group [5], and the variants were further divided into three groups based on their genomic locations, i.e., variants in coding regions, variants in non-coding variants including intronic variants, variants in untranslated regions (UTR) or in non-coding RNAs, and variants in intergenic regions.
Genetic variants correlated with malignant tumors in BD patients
A variant is considered as “same” or “identical” if the mutation is at the same genomic locus with the same alternative allele. Variants that occur in at least three individuals in the 541 BD patients with malignant tumors, and were absent in the 767 BD-only patients and the 345 healthy family controls, were identified as recurrent variants of interest. Selected variants were then mapped to the corresponding genes/non-coding RNAs based on their genomic location. The number of the variants of interest in BD patients with malignant tumors were considered as the “weight” for each corresponding gene/non-coding RNA.
Multiple machine learning algorithms including random forest and forward feature selection (ffs) were applied to further select the informative gene/non-coding RNA features. Random forest is one of the most widely used algorithms for feature selection, which computes relative importance or contribution of each gene feature in the prediction model, then scales the relevance down so that the sum of all scores is 1. All the genes/non-coding RNAs with relative importance less than 1E-5 were removed. The second algorithm ffs is one of the most common methods to reduce number of features for machine learning inputs by trying to find the best features which improve the performance of the prediction model. The modeling codes were based on the Scikit-learn package in Python language [6] and functional enrichment analysis was performed using WebGestalt (WEB-based Gene SeT AnaLysis Toolkit) [7].
Validation of selected variants using the independent dataset
Variants of interest in genes/non-coding RNAs identified in the discovery cohort were examined in the validation dataset, and mutation load boxplots of BD patients with cancers (group A) versus BD patients without cancers (group B) were generated. These included variants in coding regions, intronic regions, untranslated regions (UTR), non-coding RNA regions, and intergenic regions, respectively.
Multi-layer perceptron (MLP) from the Scikit-learn package (version 0.21.3) [6] was applied as the deep learning model based on multiple different types of coding/non-coding variants. Parameters for deep learning model, including maximum iterations, alpha value in L2 regularization, activation functions, solvers, learning rate, number of layers, and numbers of neurons per layer, were optimized using ‘gp_minimize’ function from the scikit-optimise 0.7.2 python library. The prediction has been made for each patient to label either BD patient with cancer or BD patient without cancer.
Results
Functional enrichment of genes with selected variants
A total of 158,493 variants were selected as variants of interest based on the criteria described in the method section. Variants in coding regions were mapped to 611 genes, variants in non-coding regions were mapped to 1,829 genes/non-coding RNAs, and variants in intergenic regions were mapped to 1,719 genes/non-coding RNAs after filtering by machine learning models (Supplementary Table 2). The identified genes/non-coding RNAs were further analyzed using multiple functional enrichment algorithms including Gene Ontology (GO) (9), Kyoto Encyclopedia of Genes and Genomes (KEGG) (10), Wiki Pathways (11), Gene-Disease Associations Dataset (GAD)[8], and BDdb: a comprehensive platform for exploration and utilization of birth defect multi-omics data [9]. Multiple molecular function categories were identified with significantly statistical p values based on genes/non-coding RNAs corresponding to genomic variants in non-coding areas such as intronic, untranslated region (UTR), non-coding RNAs, and intergenic regions. Several oncology-based functional pathways showed significance of adjusted p values of less than 0.05 (Fig. 2). Genes containing multiple selected variants, including variants in coding/non-coding regions, were listed in Supplementary Table 3.
Functional pathway enrichment of genes in -log10 (adjusted p value) scale. a Genes with variants mapped to coding regions; b Genes with variants mapped to non-coding regions, including intronic variants, variants in untranslated region (UTR) or in non-coding RNAs; c Genes with variants mapped to intergenic regions Disease category enrichment of genes in -log10 (adjusted p value) scale. d Genes with variants mapped to coding regions; e Genes with variants mapped to non-coding regions
Mutation load in the validation dataset
The number of variants of interest was counted for each individual in the validation dataset, including 25 BD patients with cancer. While the selected variants are exclusively seen in BD patients with cancer in the Kid First discovery set, as expected, similar patterns of mutation loads were seen in the validation dataset. The boxplots (Fig. 3) shows that the counts of the selected variants are higher in BD patients with cancers compare to patients with only BD, indicating that the variants of interest have the potential to serve as biomarkers for the risk prediction of cancer in BD patients.
Labeling accuracy in the validation cohort
To generate quantitative measures of the biomarkers, we built a deep learning model to test the labeling accuracies as described in the method section. In the validation cohort, we assessed whether BD patients with/without cancers could be labeled correctly based on the identified genes/non-coding RNAs using variant counts as the weight factor. As shown in this study, labelling accuracies are similar for variants in coding regions (30 out of 40 labeling correctly), non-coding regions (31 out of 40 labeling correctly), and intergenic regions (29 out of 40 labeling correctly), whereas the missed targets are inconsistent (Fig. 4). An interesting finding is that if we combine the prediction results using the majority vote algorithm, the accuracy increased to 80% (32 out of 40 labeling correctly) and all the mis-labeling are BD patients without cancer.
Discussion
Studies show that children with non-chromosomal birth defects (BD) are at least 2.5 times more likely to be diagnosed with cancer before 18 years of age, and the risk increases if more severe BDs are identified [2]. While this is of concern conceptually, it should be noted that the absolute risk remains low (< 1%) [2, 10], which means that biomarkers that are associate with malignant tumors in BD patients are likely to be important for the evaluation of cancer risk. This study is the first to evaluate variants of interest in BD patients with malignant tumors in comparison with BD patients without any cancers, based on 1,653 individuals with WGS data from the KidFirst DRC. The primary goal of this study is to explore the molecular functions of candidate variants for potential disease-causing effects and provide new information of how well these biomarkers may be applied to capture cancer risk as tested in the independent validation sample.
To select the informative variants from blood DNA samples, we required the variants to be exclusively occurring in BD patients with malignant tumors, and BD patients without any cancers having none. There are several potential issues that need to be addressed. First is the false positive hits, such as isolated variants identified in cancer patients by chance alone. To address this issue, we required the variants must occur in at least three unrelated cancer patients, and with none existing in any of the 345 family-based control subjects, who are healthy parents/siblings of the BD probands. The second issue is that acquired variation secondary to treatment couldn’t be differentiated in this study while we had limited access to patients’ treatment information. To help with this issue, we searched all variants of interests identified in this study through the Catalogue of Somatic Mutations In Cancer (COSMIC) database [11], no overlapped variant was identified. Since acquired somatic variants are mosaic, they might be removed in the QC processes of sequencing data. Therefore, it is reasonable to assume variants of interest in the study as causal variants. The last issue is overfitting due to the magnitude differences of DNA variants and experimental samples. To reduce the number of variants significantly while keeping the informative signals, selected variants of interest were first mapped to corresponding genes/non-coding RNA genomic regions, while the count of the variants serves as the weight in the corresponding gene/non-coding RNA. Consequently, two layers of filters (random forest plus forward feature selection) were applied to further select the most informative signals based on the weight, which is the mutation load. These steps reduced the gene/non-coding RNAs signals to acceptable size compared to data sample magnitude (611 genes for variants in coding regions; 1,829 genes/non-coding RNAs for variants in non-coding regions; and 1,719 genes/non-coding RNAs for variants in non-coding regions). The variant number was also reduced by ~ 30%, from 158,493 to 116,554.
Multiple cancer related networks/pathways were identified using functional enrichment analysis for the corresponding genes/non-coding RNAs containing variants of interest (Fig. 2a-c). For variants identified in coding regions, focal adhesion kinases (FDR = 0.029) are important mediators of growth-factor signaling in cell proliferation, survival, and migration[12], and have been considered as important therapeutic targets for immunotherapy in cancer [13, 14]. The miRNA targets in extracellular matrix (ECM) and membrane receptors (FDR = 0.0013) are believed to mediate migration, invasion, and metastasis of cancer cells[15]. For variants in non-coding genomic regions, such as intronic, untranslated region (UTR), and non-coding RNA regions, multiple pathways have been identified including Glutamatergic synapse (FDR = 1.66E-6), Circadian entrainment (FDR = 1.48E-5), Rap1 signaling pathway (FDR = 2.27E-4), Oxytocin signaling pathway (FDR = 2.67E-4), and ErbB Signaling Pathway (FDR = 0.008). Glutamatergic synapse is related to the progression and excitotoxicity of glioblastomas [16]. Circadian rhythm plays a key role in maintaining homeostasis of multiple physiological processes, and its disruption promotes tumorigenesis; therefore, it has been considered as a new target for cancer prevention and treatments [17]. Rap1 signaling regulates cell invasion/metastasis [18] and central nervous system (CNS) neuropeptide hormone oxytocin isa cancer biomarker found to link to multiple type of cancers through interactions with a number of factors in the microenvironment [19]. Multiple pathways enriched for intergenic variants corresponding genes/non-coding RNAs are overlapping with the enriched pathways for genes/non-coding RNAs with variants in intronic, untranslated region (UTR), and non-coding RNA regions, including Axon guidance (FDR = 9.07E-4 & 4.31E-8, respectively), Cell adhesion (FDR = 4.76E-3 & 2.69E-4), Pathways Regulating Hippo Signaling (FDR = 3.74E-4 & 6.52E-10), Splicing factor NOVA regulated synaptic proteins (FDR = 0.003 & 1.56E-6), Hippo-Merlin Signaling Dysregulation (FDR = 0.003 & 1.78E-6), and Ectoderm Differentiation (FDR = 0.008 & 3.8E-5). Genetic variants and observed altered expression of the Hippo pathway have the unique capacity to lead to tumorigenesis and thereby, promote the migration, invasion, and malignancy of cancer cells through cell cycle regulation [20, 21]. NOVA factors promote cell proliferation, colony formation, migration, and invasion by interacting with miRNA in cancer cells [22]. It is worth to mention that genes/non-coding RNAs with non-coding region variants present in a number of functionally enriched pathways/gene-sets with statistical significance (Fig. 2), indicating variants in non-coding genomic regions may play important roles in pediatric cancers in birth defect patients. Meanwhile, multiple disease categories, especially those related to birth defects, were significantly enriched (e.g., metabolic diseases, cardiovascular diseases, psychiatric diseases) (Fig. 2d and e).
There are 119 genes with at least two variants in coding regions and 478 genes with at least 20 variants in their non-coding regions (Supplementary Table 3). Genes with multiple coding variants are enriched in diseases associated with glycosylation, including Termination of O-glycan biosynthesis (FDR = 0.00012), O-glycosylation of proteins (FDR = 0.00077), and O-linked glycosylation (FDR = 0.012). Congenital disorders of glycosylation (CDG) is an umbrella term for a rapidly expanding group of over 130 rare genetic, metabolic disorders, associated with birth defects and cancers. For genes with multiple identified non-coding variants, they are enriched in biological pathways related to neural systems, including glutamatergic synapse (FDR = 0.0053) and axon guidance (FDR = 0.0053); cardiovascular system (cardiomyopathy, FDR = 0.0053); and pathways related to tumorigenesis, such as phospholipase D signaling pathway (FDR = 0.0053), ErbB signaling pathway (FDR = 0.033) and Cadherin signaling pathway (FDR = 0.015). In addition, enrichment of gene-set is identified in Autistic Disorder (FDR = 2.8e-10), Chagas Cardiomyopathy (FDR = 1.04e-11), as well as multiple types of cancers based on the OMIM database.
Six hundred eleven genes with coding variant were searched by the GAD and BDdb databases to identify previously reported associations with birth defects and cancers. Five genes, AXIN2, BMP1, CR1, ERBB2, and RYR1, have been recorded of association with birth defects and cancer (Table 1). AXIN2 was reported of association with cleft lip [23] and mutations of this genes are associated with multiple types of cancers; mutations of BMP1 were reported in patients with gastroschisis [24] and may serve as a therapeutic biomarker for gastric cancer patients [25]; CR1 is related to tetralogy of Fallot [26], a type of congenital heart defects, associated with susceptibility to gallbladder cancer, and a prognosis predictor in non-small cell lung cancer [27]; ERBB2, a well-studied biomarker in breast invasive ductal carcinoma, lung adenocarcinoma, colon adenocarcinoma, bladder urothelial carcinoma, and invasive breast carcinoma, is also related to neural tube defect [28]; RYR1 is a major contributor to nonsyndromic Tetralogy of Fallot [29], and higher expression level of RYR1 in tumor is associated with advanced stage of the uterine serous cancer [30].
We validated the identified variants by evaluating their prediction ability in an independent cohort. We selected 40 BD patients from an independent project, including 25 patients diagnosed with at least one type of cancer. The number of variants of interest were calculated for each patient. If the selected variants of interest from the 1,653 subjects in the discovery cohort represent the biological/medical characters of pediatric cancers in BD patients, similar patterns would be expected in the independent validation cohort. The boxplots in the validation cohort (Fig. 3) show clearly larger numbers of selected variants in BD patients with cancers compared to BD patients without cancers, for both variants in coding regions and those in non-coding regions. A deep learning model was further applied to assess the predictive abilities of the biomarkers. The labelling accuracies were stable at around 75% (30 out of 40 patients labeling correctly), and the mis-labeling individuals were inconsistent when using different feature factors in three different types of genomic regions (Fig. 4). Notably, combining labeling results using majority vote algorithms increased the accuracy to 80% with all eight mis-labeling patients belonging to the BD patients without cancer, leaving the overall accuracy in predicting this particular phenotype to random guess (7 out of 15 labelled correctly). The potential reasons may be due to genetic heterogeneity or incomplete penetrance underlying the molecular mechanisms of birth defects without cancer. In this regard, birth defects without cancer may be more difficult to be identified and captured comprehensively due to fewer phenotype terms (i.e. without cancers which have higher predictability).
Conclusion
In conclusion, we conducted the first study to identify genetic variants of interest related to malignant tumors in patients with coexisting BD, leveraging one of the largest pediatric BD and oncology resources assembled. The results were validated in an independent cohort study of unrelated patients. Further research of the variants of interest identified in this study could unveil new insights into the underlying molecular mechanisms of BD with cancer and may offer new insight into optimal use of biomarkers in predicting and diagnosing cancer in BD patients at early stage.
Availability of data and materials
The KidFirst data could be accessed at Kids First Data Resource Portal (DRC) (https://portal.kidsfirstdrc.org/login).
The TOPMED data has been uploaded to the database of Genotypes and Phenotypes (dbGaP, https://www.ncbi.nlm.nih.gov/gap/) with the accession number phs001661.v2.p1.
References
Daltveit DS, Klungsoyr K, Engeland A, Ekbom A, Gissler M, Glimelius I, Grotmol T, Madanat-Harjuoja L, Ording AG, Saether SMM, et al. Cancer risk in individuals with major birth defects: large Nordic population based case-control study among children, adolescents, and adults. BMJ. 2020;371:m4060.
Lupo PJ, Schraw JM, Desrosiers TA, Nembhard WN, Langlois PH, Canfield MA, Copeland G, Meyer RE, Brown AL, Chambers TM, et al. Association Between Birth Defects and Cancer Risk Among Children and Adolescents in a Population-Based Assessment of 10 Million Live Births. JAMA Oncol. 2019;5:1150–8.
Yang Y. Wnts and wing: Wnt signaling in vertebrate limb development and musculoskeletal morphogenesis. Birth Defects Res C Embryo Today. 2003;69:305–17.
Al Hajri Q, Dash S, Feng WC, Garner HR, Anandakrishnan R. Identifying multi-hit carcinogenic gene combinations: Scaling up a weighted set cover algorithm using compressed binary matrix representation on a GPU. Sci Rep. 2020;10:2022.
Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38:e164.
Pedregosa FV, Gramfort G, Michel A, Thirion V, Grisel B, Blondel O, Prettenhofer M, Weiss P, Dubourg R, Vanderplas V, Passos J, Cournapeau A, Brucher D, M. and Perrot M, Duchesnay E. Scikit-learn: Machine Learning in Python. J Mach Learn Res. 2011;12:2825–30.
Liao Y, Wang J, Jaehnig EJ, Shi Z, Zhang B. WebGestalt 2019: gene set analysis toolkit with revamped UIs and APIs. Nucleic Acids Res. 2019;47:W199–205.
Becker KG, Barnes KC, Bright TJ, Wang SA. The genetic association database. Nat Genet. 2004;36:431–2.
Zhang D, Zhou S, Zhou Z, Jiang X, Chen D, Sun HX, Huang J, Qu S, Yang S, Gu Y, et al. BDdb: a comprehensive platform for exploration and utilization of birth defect multi-omics data. BMC Med Genomics. 2021;14:260.
Botto LD, Flood T, Little J, Fluchel MN, Krikov S, Feldkamp ML, Wu Y, Goedken R, Puzhankara S, Romitti PA. Cancer risk in children and adolescents with birth defects: a population-based cohort study. PLoS ONE. 2013;8:e69077.
Tate JG, Bamford S, Jubb HC, Sondka Z, Beare DM, Bindal N, Boutselakis H, Cole CG, Creatore C, Dawson E, et al. COSMIC: the Catalogue Of Somatic Mutations In Cancer. Nucleic Acids Res. 2019;47:D941–7.
McLean GW, Carragher NO, Avizienyte E, Evans J, Brunton VG, Frame MC. The role of focal-adhesion kinase in cancer - a new therapeutic opportunity. Nat Rev Cancer. 2005;5:505–15.
Thiyagarajan V, Tsai MJ, Weng CF. Antroquinonol Targets FAK-Signaling Pathway Suppressed Cell Migration, Invasion, and Tumor Growth of C6 Glioma. PLoS ONE. 2015;10:e0141285.
Serrels A, Frame MC. FAK goes nuclear to control antitumor immunity-a new target in cancer immuno-therapy. Oncoimmunology. 2016;5:e1119356.
Grzywa TM, Klicka K, Wlodarski PK. Regulators at Every Step-How microRNAs Drive Tumor Cell Invasiveness and Metastasis. Cancers (Basel). 2020;12(12):3709. https://doi.org/10.3390/cancers12123709.
Lange F, Hornschemeyer J, Kirschstein T. Glutamatergic Mechanisms in Glioblastoma and Tumor-Associated Epilepsy. Cells. 2021;10(5):1226. https://doi.org/10.3390/cells10051226.
Sulli G, Lam MTY, Panda S. Interplay between Circadian Clock and Cancer: New Frontiers for Cancer Treatment. Trends Cancer. 2019;5:475–94.
Zhang YL, Wang RC, Cheng K, Ring BZ, Su L. Roles of Rap1 signaling in tumor cell migration and invasion. Cancer Biol Med. 2017;14:90–9.
Lerman B, Harricharran T, Ogunwobi OO. Oxytocin and cancer: An emerging link. World J Clin Oncol. 2018;9:74–82.
Han Y. Analysis of the role of the Hippo pathway in cancer. J Transl Med. 2019;17:116.
Xiao Y, Dong J. The Hippo Signaling Pathway in Cancer: A Cell Cycle Perspective. Cancers (Basel). 2021;13(24):6214. https://doi.org/10.3390/cancers13246214.
Meldolesi J. Alternative Splicing by NOVA Factors: From Gene Expression to Cell Physiology and Pathology. Int J Mol Sci. 2020;21(11):3941. https://doi.org/10.3390/ijms21113941.
de Araujo TK, Secolin R, Felix TM, de Souza LT, Fontes MI, Monlleo IL, de Souza J, Fett-Conte AC, Ribeiro EM, Xavier AC, et al. A multicentric association study between 39 genes and nonsyndromic cleft lip and palate in a Brazilian population. J Craniomaxillofac Surg. 2016;44:16–20.
Komuro H, Mori M, Hayashi Y, Fukagawa M, Makino S, Takahara K, Greenspan DS, Momoi MY. Mutational analysis of the BMP-1 gene in patients with gastroschisis. J Pediatr Surg. 2001;36:885–7.
Rafi JH, Jafar T, Pathan MT, Reza R, Islam S, Sourna IJ, Alam R, Samad A, Ahammad F. High expression of bone morphogenetic protein 1 (BMP1) is associated with a poor survival rate in human gastric cancer, a dataset approaches. Genomics. 2021;113:1141–54.
Kobylinska J, Dworzanski W, Cendrowska-Pinkosz M, Dworzanska A, Hermanowicz-Dryka T, Kiszka J, Staroslawska E, Burdan F. [Morphological and molecular bases of cardiac development]. Postepy Hig Med Dosw (Online). 2013;67:950–7.
Xu C, Yuan Q, Hu H, Wang W, Zhang Q, Li L, Wang J, Yang R. Expression of Cripto-1 predicts poor prognosis in stage I non-small cell lung cancer. J Cell Mol Med. 2020;24:9705–11.
Deng S, Hirschberg A, Worzfeld T, Penachioni JY, Korostylev A, Swiercz JM, Vodrazka P, Mauti O, Stoeckli ET, Tamagnone L, et al. Plexin-B2, but not Plexin-B1, critically modulates neuronal migration and patterning of the developing nervous system in vivo. J Neurosci. 2007;27:6333–47.
Page DJ, Miossec MJ, Williams SG, Monaghan RM, Fotiou E, Cordell HJ, Sutcliffe L, Topf A, Bourgey M, Bourque G, et al. Whole Exome Sequencing Reveals the Major Genetic Contributors to Nonsyndromic Tetralogy of Fallot. Circ Res. 2019;124:553–63.
Zhang L, Au-Yeung CL, Huang C, Yeung TL, Ferri-Borgogno S, Lawson BC, Kwan SY, Yin Z, Wong ST, Thomas V, et al. Ryanodine receptor 1-mediated Ca(2+) signaling and mitochondrial reprogramming modulate uterine serous cancer malignant phenotypes. J Exp Clin Cancer Res. 2022;41:242.
Acknowledgements
Sample collection and biobanking for this study was supported by Institutional Development Funds from the Children’s Hospital of Philadelphia (CHOP) to the Center for Applied Genomics (CAG) and CHOP´s Endowed Chair in Genomic Research (CAG). The sequencing data was provided through the Gabriella Miller Kids First Pediatric Research Program consortium (Kids First), supported by the Common Fund of the Office of the Director of the National Institutes of Health (www.commonfund.nih.gov/KidsFirst), awarded to CAG. The TOPMed acknowledgements can be found at: https://www.nhlbiwgs.org/acknowledgements. We thank the CAG staff and the participating patients and families who contributed biosamples to CAG/CHOP.
Funding
The study was supported by Institutional Development Funds from the Children’s Hospital of Philadelphia to the Center for Applied Genomics, The Children’s Hospital of Philadelphia Endowed Chair in Genomic Research to HH.
Author information
Authors and Affiliations
Contributions
Conceptualization, Y.L. and H.H; literature search, Y.L.; data preparation & analysis, Y.L., H.Q.Q., C.X., F.D.M., K.N., and H.Q.; data interpretation, Y.L., H.Q.Q., C.X., K.N., X.W., J.G., A.H.S., D.W., and H.H.; original draft writing, Y.L.; review and revision, Y.L., H.Q.Q. and H.H. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
We confirm that all methods were carried out in accordance with relevant guidelines and regulations and all experimental protocols were approved by the Children’s Hospital of Philadelphia (CHOP) Institutional Review Board (IRB). Informed consent was obtained from all subjects or, if subjects are under 18, from a parent and/or legal guardian with assent from the child if 7 years or older.
Consent for publication
Not applicable.
Competing interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., Qu, HQ., Chang, X. et al. Identification of risk variants related to malignant tumors in children with birth defects by whole genome sequencing. Biomark Res 10, 84 (2022). https://doi.org/10.1186/s40364-022-00431-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40364-022-00431-y