Abstract
Background
Polypharmacy is often prescribed for bipolar disorder, yet medication non-adherence remains a serious problem. This study investigated the regularity in the daily dosage taken of mood stabilizers and second generation antipsychotics.
Methods
Daily self-reported data on medications taken and mood were available from 241 patients with a diagnosis of bipolar disorder who received treatment as usual. Patients who took the same mood stabilizer or second generation antipsychotic for ≥ 100 days were included. Approximate entropy was used to determine serial regularity in daily dosage taken. Generalized estimating equations were used to estimate if demographic or clinical variables were associated with regularity.
Results
There were 422 analysis periods available from the 241 patients. Patients took drugs on 84.4% of days. Considerable irregularity was found, mostly due to single-day omissions and dosage changes. Drug holidays (missing 3 or more consecutive days) were found in 35.8% of the analysis periods. Irregularity was associated with an increasing total number of psychotropic drugs taken (p = 0.009), the pill burden (p = 0.026), and the percent of days depressed (p = 0.049).
Conclusion
Despite low missing percent of days, daily drug dosage may be irregular primarily due to single day omissions and dosage changes. Drug holidays are common. Physicians should expect to see partial adherence in clinical practice, especially with complex drug regimens. Daily dosage irregularity may impact the continuity of drug action, contribute to individual variation in treatment response, and needs further study.
Similar content being viewed by others
Background
Drug regimens for the treatment of bipolar disorder are increasing in complexity. Polypharmacy, defined as two or more psychotropic medications, is prescribed to the majority of inpatients and outpatients, including the elderly (Weinstock et al. 2014; Bjørklund et al. 2016; Bauer et al. 2013a; Peselow et al. 2016; Kleimann et al. 2016; Golden et al. 2017; Rej et al. 2017; Kessing et al. 2016). A minority of patients, ranging from 18 to 36% in recent studies, are prescribed four or more psychotropic medications (Bauer et al. 2013a; Weinstock et al. 2014; Golden et al. 2017; Goldberg et al. 2009). The use of evidence-based combination therapies may improve treatment response, and many drug combinations are included as first and second-line recommendations in international guidelines for the treatment of bipolar disorder (Parker et al. 2017; Fountoulakis et al. 2017). The challenges of polypharmacy include unproven combination therapies, limited available evidence, increased risks of serious adverse reactions and drug interactions, and patient costs (Kukreja et al. 2013; Sachs et al. 2014).
Less than half of patients with bipolar disorder are estimated to be adherent with prescribed treatments, with most having intermittent or partial adherence that fluctuates over time (García et al. 2016; Pompili et al. 2009; Scott and Pope 2002; Kessing et al. 2007). Medication non-adherence in bipolar disorder is associated with an increased risk of relapse, hospitalization, and suicide (Hassan and Lage 2009; Hong et al. 2011; Gonzalez-Pinto et al. 2006; Schuepbach et al. 2008). Medication adherence is difficult to measure, and all methods have strengths and weaknesses (Hawkshead and Krousel-Wood 2007; Pearson et al. 2007; Levin et al. 2015; Sajatovic et al. 2010). Clinical studies of adherence generally involve subjective scales completed by patients or physicians, which quantify missing days, doses or attitudes (Pompili et al. 2009; Baldessarini et al. 2008; Jónsdóttir et al. 2010). We previously measured the regularity in the daily dosage taken of mood stabilizers (lithium and anticonvulsants) using self-reported data (Bauer et al. 2013b). Dosage regularity measures daily changes and enhances understanding beyond the basic percent of missing days. Considerable irregularity in the daily dosage of mood stabilizers was found in patients missing less than 14% of days (Bauer et al. 2013b). Both the total number of psychotropic medications and the pill burden were associated with increased irregularity. The purpose of this study is to repeat the regularity analysis including second-generation antipsychotics as well as traditional mood stabilizers.
Methods
All data were obtained from outpatients, aged 18 years or older, who agreed to record mood, sleep, and medications taken daily using ChronoRecord software (Bauer et al. 2004, 2008). All the participants were volunteers, primarily recruited by the prescribing psychiatrist, who were informed about the study prior to providing written informed consent. The study was approved by local institutional review boards. The diagnosis was made by the prescribing psychiatrist at a clinical interview, and the patient received pharmacological treatment as usual throughout the study. Data were obtained from 666 patients, of which 480 had a diagnosis of any bipolar disorder based on DSM IV or DSM 5 criteria, and returned ≥ 30 days of data.
Patient data entry
Patents received about a half hour of training on the use of ChronoRecord software, in person or by telephone, before entering data. During the training session, a medication list was created for each patient. The medication list includes all drugs prescribed for bipolar disorder and any other prescribed or over-the-counter (OTC) drugs that the patient felt impacted their mood. The prescribed psychotropic drugs were selected from a list in the software, displayed by both brand and generic names. The patient could add a drug not included in the software list, and could modify the list of drugs taken at any time. For each selected drug, the pill strength was chosen from a list of available strengths. Every day, for each drug, the patient entered the total number of pills taken. Patients could enter partial pills (1/4, 1/2, or 3/4) for tablets but not capsules. If a drug was not taken, the patient entered 0 pills for that drug for that day. A missing day of data was also treated as if no pills were taken. Data not entered on 1 day could be entered at a later date. The software includes error checking to prevent entry for a future date, and to verify entry of a large number of pills for a drug.
In addition to medications, the patients entered mood, sleep, and significant life events daily, and weight weekly into the ChronoRecord software. ChronoRecord uses a 100-unit visual analog scale between the extremes of mania and depression to rate mood. Based upon the prior validation studies (Bauer et al. 2004, 2008), a mood entry less than 40 was considered depression, 40–60 euthymia, and greater than 60 hypomania/mania. The depression ratings varied from mild (entry of 20–39) to moderate–severe (entry of 0–19), and the mania ratings varied from hypomania (entry of 61–80) to moderate-severe (entry of 81–100).
Drugs analyzed
The drugs analyzed were traditional mood stabilizers as in the prior analysis: lithium, valproate, lamotrigine, carbamazepine, oxcarbazepine (Bauer et al. 2013b), and second generation antipsychotics: aripiprazole, olanzapine, risperidone, quetiapine, ziprasidone, paliperidone, asenapine, lurasidone, and clozapine. The analysis of the total psychotropic drugs taken and the daily pill burden also included antidepressants, benzodiazepines, typical antipsychotics, insomnia medications, other anticonvulsants (topirimate, gabapentin, pregabalin, tiagabine, levetiracetam, zonisamide), thyroid hormones and estrogens.
Regularity analysis using ApEn
Regularity in the daily medication dosage was calculated using Approximate Entropy (ApEn) as in the prior studies (Bauer et al. 2013b, c). ApEn is a family of statistics that measure serial regularity in a time series, are model independent, and can be used with datasets that are small and noisy (Pincus 1991; Pincus et al. 1991). Regularity can be thought of as the tendency that values within a time series remain the same on incremental comparisons (Pincus 1991; Pincus et al. 1991). ApEn computes a single positive value, with 0 indicating a completely regular sequence, and with increasingly larger numbers signifying greater serial irregularity. The estimated value of the ApEn (m, r, N) depends on: m the pattern length used for prediction of the subsequent value, r the level of noise filtering, and N the number of data values in the run to be compared. The ApEn noise filtering compares the difference between the data in each sequence of m days of data (Pincus et al. 1991). Conceptually, when the absolute value of the difference is greater than the noise filter level, the ApEn statistic is incremented. Otherwise, the difference is treated as noise and ignored. The level of noise filtering was calculated as a percent of the individual subjects’ standard deviation (Pincus et al. 1993). For this analysis, the parameters included were m = 1 day, r = 0.2 × SD in daily drug dosage, and N = 100 days.
The calculated value of ApEn is dependent upon the order of the data in the time series. Changing the order of the data will likely change the calculated value of ApEn. In contrast, the calculated value of the familiar mean and standard deviation will be identical for a set of data in a time series regardless of the order of the data. ApEn is a valuable measure of the daily dosage fluctuations found with partial adherence (Bauer et al. 2013b, c). For example, the ApEn would be 0 if the patient made no changes to the daily dosage or discontinued a medication, and would be largely unaffected by a prescription change if the patient keeps taking the new dosage (Bauer et al. 2013b).
Per patient regularity analysis
For every drug included in the ApEn analysis, the time span for taking the drug was determined for each patient. If the time span was ≥ 100 days, the ApEn was calculated for the first 100 days of data. Patients who took more than one drug for ≥ 100 days could have more than one ApEn analysis. Of the 480 patients with bipolar disorder, 241 patients took at least one drug for sufficient length of time for analysis. For the 241 patients, 422 ApEn sequences were calculated.
Statistics
Descriptive statistics for the demographic and clinical characteristics of the 241 patients were calculated. For each patient, for each 100-day ApEn period, the percent of days with depressed, euthymic and manic/hypomanic mood were determined. Drug holidays, defined as missing 3 or more consecutive days (Urquhart 1998), were determined for each patient during the 100-day period. The daily pill burden was defined as total number of pills for all psychotropic medications. For each patient, for each 100-day ApEn period, the mode of the daily number of psychotropic medications, daily pill burden, and daily dosage were calculated. The mode is the most frequent value in a series of numbers, and was chosen as a proxy for the prescribed daily number of medications, pill burden and daily dosage. The mean values for the entire sample were calculated using the modal values for each patient.
Since one patient could have more than one ApEn analysis, generalized estimating equations (GEE) were used to adjust model coefficients and standard errors for within-patient correlation. To estimate if demographic or clinical variables were associated with ApEn, GEE models were used with ApEn as the dependent variable and an independent working correlation structure (Pan and Connett 2002). GEE models were also used to estimate if demographic or clinical variables were associated with the percent of missing doses or with drug holidays. SPSS Version 24 was used for all analyses.
Results
422 ApEn sequences were calculated from the 241 patients. Of the 241 patients, 158 (66%) were recruited from a university mood clinic and 83 (34%) from a private practice. The demographic characteristics of the 241 patients are shown in Table 1. During the 100-day periods, the patients were euthymic 71.6% of days, depressed 20.9% of days, and hypomanic/manic 7.5% of days. The 241 patients returned a mean of 389 (SD 567) days of data.
Medications
The medications taken by the 241 patients are summarized in Table 2. The patients took a mean of 3.9 psychotropic medications, with a mean pill burden of 7.2 for these drugs. Many of the 241 patients were taking more than one mood stabilizer or antipsychotic, or changed medication, such that 121 (50%) of the patients had 1 ApEn analysis, 72 (30%) had 2 ApEn analysis, 40 (17%) had 3 ApEn analyses, and 8 (3%) had > 3 ApEn analyses.
Missing days and drug holidays
Overall, the patients took medication on a mean of 84.4% of days. Missing drug data occurred frequently within the 100-day analysis periods. There was at least one single day omission in 64.7% of the 422 analyses periods. The percent of days of missing drug data was associated with the percent of days depressed (p = 0.046), and inversely associated with the percent of days euthymic (p = 0.047).
One or more drug holidays were found in 151 (35.8%) of the 422 analysis periods. Of the 151 analysis periods containing a drug holiday, more than one drug holiday was present in 57 (37.8%). Taking a drug holiday was associated with working full time (p = 0.005), and the total number of psychotropic drugs (p = 0.043).
Regularity analysis
For the 422 100-day analyses periods, the ApEn values ranged between 0 and 0.94, with a mean of 0.21 (SD 0.18). For the 422 analyses, the ApEn was between 0 and 0.2 for 240 (56.9%), between 0.2 and 0.4 for 128 (30.3%), and > 0.4 for 54 (12.8%). The ApEn was 0 (no change to daily dosage) in 56 (13.3%) of the analyses.
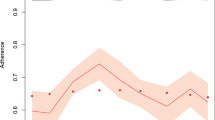
ApEn is directly related to the percent of days of missing doses (p < 0.001). However, even patients with a low percent of days missing doses may have irregular daily dosages. Figure 1 includes examples graphs of patients with irregular daily dosage, despite low missing days of data, and one example of how a patient may have both a larger number of missing days, and variable dosage.
Example ApEn, adherence and drug holiday values for 100 days of data. In a–f, patients have few missing days but irregular daily dosage (high ApEn). In g, the patient has both a large number of missing days and irregular daily dosage. a Lamotrigine. ApEn 0.3432 with 94% adherence and 0 drug holidays. b Valproate. ApEn 0.4836 with 87% adherence and 2 drug holidays. c Lithium. ApEn 0.3511 with 97% adherence and 0 drug holidays. d Risperidone. ApEn 0.6007 with 80% adherence and 4 drug holidays. e Asenapine. ApEn 0.7117 with 86% adherence and 1 drug holiday. f Lamotrigine. ApEn 0.3756 with 99% adherence and 0 drug holidays. g Lamotrigine. ApEn 0.9428 with 65% adherence and 4 drug holidays
The factors other than missing days of data that were associated with increasing irregularity are shown in Table 3. The total number of psychotropic drugs (p = 0.009), the pill burden (p = 0.026), and the percent of days depressed (p = 0.049) were all associated with irregularity. The percent of days euthymic was inversely related to irregularity (p = 0.028). No other clinical or demographic variables were associated with irregularity.
Discussion
Patients with bipolar disorder in this study were motivated to actively participate in their care, and took medication on about 84% of days. Yet, even among this group, despite the low percent of missing days, there was considerable irregularity in the daily dosage taken. Days of missing doses, primarily single day omissions, and changes to the daily dosage were the primary cause of the irregularity. Additionally, there was at least one drug holiday in 35.8% of the analysis periods. These results are consistent with our prior studies, and there are many implications of these findings (Bauer et al. 2013b, c).
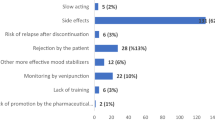
It is challenging for the physician to reliably assess patient adherence and the link between non-adherence and inadequate response. Irregularity in the daily dosage may be a contributing factor. Most psychiatrists prefer to assess adherence of patients with bipolar disorder by asking the patient (Vieta et al. 2012), but physician perceptions are often incorrect and optimistic (Velligan et al. 2009; Baldessarini et al. 2008). For example, physicians overestimated adherence with second-generation antipsychotics, primarily by patients with bipolar disorder, as compared to claims data (Stephenson et al. 2012). For 97 patients who went to an emergency room for an exacerbation of psychosis, including 26 with bipolar disorder, staff assessments of adherence and non-adherence were correct 41.5 and 75% of the time respectively, when compared to plasma antipsychotic levels (Lopez et al. 2017).
In this study, single day omissions occurred frequently. Some drugs and formulations are more forgiving about dosage omissions than others, varying with the pharmacokinetic and pharmacodynamic properties (Osterberg et al. 2010; Urquhart 1998). With a forgiving drug, the duration of action is much longer than the dosage interval, so an occasional missed dose is unlikely to interrupt therapeutic activity (Osterberg et al. 2010). Recently, the number of drug formulations that require less frequent dosing has increased, including formulations for psychotropic drugs. While a less frequent dosing regimen generally increases adherence (Saini et al. 2009; Claxton et al. 2001), it may not improve outcomes (Comté et al. 2007; Richter et al. 2003; Vrijens et al. 2014; Vrijens and Heidbuchel 2015; Harden 2017; Bialer 2007). For example, the consequences of missing one dose of a once-daily drug may be more deleterious to the continuity of therapeutic action than missing one dose of a twice-daily drug (Osterberg et al. 2010; Hughes 2006; Urquhart and Vrijens 2006). However, extended release formulations that reduce fluctuations in plasma concentration may improve the forgiveness of once-daily drugs (Pellock and Brittain 2016; Chen et al. 2013; Brittain and Wheless 2015).
The relatively large number of drug holidays reported in this study, with a dosing interruption of 3 or more days, are of considerable concern. The rapid discontinuation of a psychotropic drug may trigger immediate withdrawal symptoms or delayed rebound phenomena, related to complex factors including pharmacokinetic and pharmacodynamic properties of a drug formulation, and individual metabolism (Baldessarini et al. 1999; Cerovecki et al. 2013; Franks et al. 2008; Fava et al. 2015; Correll 2010; Osterberg et al. 2010). After a drug holiday, patients often resume taking the full-strength dosage, including of drugs that are slowly titrated upward. Re-starting a drug after a long lapse may trigger first-dose effects (Urquhart 1998). Given the frequent use of polypharmacy, drug holidays may impact the potential for drug interactions (Spina et al. 2016). There is a need for increased understanding of the clinical impacts of repeated starting and stopping of mood stabilizers and antipsychotic drugs, in various product formulations (Osterberg et al. 2010; Hughes 2008; Samtani et al. 2012). In this study, taking a drug holiday was associated with working full time, suggesting that some patients may doubt they need ongoing treatment (Clatworthy et al. 2009), or lack insight into the value of medications (Copeland et al. 2008). In prior research, employment was not associated with psychotropic medication adherence (Bulloch and Patten 2010; Razzano et al. 2005, Sajatovic et al. 2006).
In addition to dosage omissions, changes to the daily dosage contributed to the irregularity. The patients in this study took polypharmacy with a mean of 3.9 psychotropic medications for bipolar disorder, and a mean pill burden of 7.2. Both the number of psychotropic medications and the pill burden were associated with irregularity in daily dosage. Research in a wide range of chronic medical illnesses has found that medication regimen complexity decreases adherence (Ingersoll and Cohen 2008). Some patients with bipolar disorder may have trouble integrating a complex drug regimen into their daily routine (Sajatovic et al. 2009; Wagner and Ryan 2004), especially those with a disorganized lifestyle (Frank et al. 2006). Even patients intent on adhering often forget about doses, especially on days with unexpected schedule interruptions (Dunbar-Jacob and Mortimer-Stephens 2001; Bulloch and Patten 2010), which usually results in underdosing but sometimes overdosing.
Other factors contribute to irregular daily dosages. Patients may have an “as needed” approach to dosing, taking doses to treat symptoms or lessen side effects (Dunbar-Jacob and Mortimer-Stephens 2001; Marder 2003; Pound et al. 2005). Recent societal emphasis on self-management may be encouraging self-experimentation (Swan 2013). Some patients want to take as little medication as possible (Pound et al. 2005). Consistent with our prior studies, depressive symptoms were associated with increased irregularity (Bauer et al. 2013b, c). In other research, depressive symptoms were associated with non-adherence in bipolar disorder (Belzeaux et al. 2013; Johnson et al. 2007), as well chronic medical conditions (Grenard et al. 2011).
Several issues may impact the generalizability of this study. No data were available on the rate and characteristics of patients who were asked but declined to participate in the study. A large percentage of patients were recruited from university clinics, which may not reflect other settings. In the current study, more females than males were included, and patients varied in the phase of illness and disease severity. However, the demographic characteristics of the patients who use ChronoRecord are similar to those reported for other studies of bipolar disorder (Bauer et al. 2012). Since taking a mood stabilizer or antipsychotic for 100 days was required for analysis, the least adherent patients were excluded. However, even higher irregularity in daily dosage would be expected from patients who are less adherent.
There are other limitations to this study. All data were self-reported. However, review articles about the measurement of medication adherence have found moderate-to-high concordance between self-reported patient questionnaires and diaries, and electronic monitoring (Garber et al. 2004; Shi et al. 2010; Monnette et al. 2018). In a study of patients with bipolar disorder, good agreement was found between patient questionnaires and serum levels of psychotropic medications (Jónsdóttir et al. 2010). This study underestimated regimen complexity since medications taken for general medical reasons and OTC drugs were not included. Other aspects of drug regimen complexity such as administration instructions, and dosage timing were not available. Some of the dosage changes may have been prescribed by the physician. Only oral medications were included in this study. Different formulations of the same medication, such as pill size and ease of swallowing, are known to impact adherence but were not considered (Bhosle et al. 2009; Fields et al. 2015). The specific drug regimens were not investigated but are highly variable in clinical practice, including different combinations of medication classes and drugs (Bauer et al. 2013a).
It is important to put the findings of this study into context. In this sample of patients with bipolar disorder who were motivated to participate in their care, there was considerable irregularity in daily dosage. However, partial adherence is also routinely found in patients with chronic medical conditions who do not have mental illness (Osterberg and Blaschke 2005; Brown et al. 2016). Even in a monitored environment, less than 70% of over 16,000 patients with various medical conditions enrolled in 95 clinical studies were fully adherent (Vrijens and Urquhart 2014; Blaschke et al. 2012). The clinician treating patients with bipolar disorder should expect a level of nonadherence including dosage omissions, changes, and drug holidays, even among patients determined to recover. If the patient’s condition is such that exceptional adherence is required, such as approaching no missing dosages, intensive educational measures, and customization of the individual’s regimen are required. These findings also confirm the need for careful evaluation of newly appearing or worsening symptoms.
Conclusion
In conclusion, considerable irregularity in daily dosage of mood stabilizers and antipsychotic medications was found despite a low percent of missing days. The total number of psychotropic drugs, pill burden and depression were associated with increased irregularity. The irregularity in daily dosage was primarily due to single day omissions and dosage changes. Drug holidays were also present. These findings may contribute to understanding the individual variation in treatment response seen in clinical practice. Physicians should expect to see partial adherence with treatments for bipolar disorder. More understanding of the impacts of daily irregularity on specific drugs and formulations is needed.
References
Baldessarini RJ, Tondo L, Viguera AC. Discontinuing lithium maintenance treatment in bipolar disorders: risks and implications. Bipolar Disord. 1999;1:17–24.
Baldessarini RJ, Perry R, Pike J. Factors associated with treatment nonadherence among US bipolar disorder patients. Hum Psychopharmacol. 2008;23:95–105.
Bauer M, Grof P, Gyulai L, Rasgon N, Glenn T, Whybrow PC. Using technology to improve longitudinal studies: self-reporting with ChronoRecord in bipolar disorder. Bipolar Disord. 2004;2004(6):67–74.
Bauer M, Wilson T, Neuhaus K, Sasse J, Pfennig A, Lewitzka U, et al. Self-reporting software for bipolar disorder: validation of ChronoRecord by patients with mania. Psychiatry Res. 2008;159:359–66.
Bauer M, Glenn T, Keil M, Bauer R, Marsh W, Grof P, et al. Brief depressive symptoms in patients with bipolar disorder: analysis of long-term self-reported data. Aust N Z J Psychiatry. 2012;46:1068–78.
Bauer M, Glenn T, Alda M, Sagduyu K, Marsh W, Grof P, et al. Drug treatment patterns in bipolar disorder: analysis of long-term self-reported data. Int J Bipolar Disord. 2013a;1:5.
Bauer M, Glenn T, Alda M, Sagduyu K, Marsh W, Grof P, et al. Regularity in daily mood stabilizer dosage taken by patients with bipolar disorder. Pharmacopsychiatry. 2013b;46:163–8.
Bauer R, Glenn T, Alda M, Sagduyu K, Marsh W, Grof P, et al. Antidepressant dosage taken by patients with bipolar disorder: factors associated with irregularity. Int J Bipolar Disord. 2013c;1:26.
Belzeaux R, Correard N, Boyer L, Etain B, Loftus J, Bellivier F, et al. Depressive residual symptoms are associated with lower adherence to medication in bipolar patients without substance use disorder: results from the FACE-BD cohort. J Affect Disord. 2013;151:1009–15.
Bhosle M, Benner JS, Dekoven M, Shelton J. Difficult to swallow: patient preferences for alternative valproate pharmaceutical formulations. Patient Prefer Adherence. 2009;3:161–71.
Bialer M. Extended-release formulations for the treatment of epilepsy. CNS Drugs. 2007;21:765–74.
Bjørklund L, Horsdal HT, Mors O, Østergaard SD, Gasse C. Trends in the psychopharmacological treatment of bipolar disorder: a nationwide register-based study. Acta Neuropsychiatr. 2016;28:75–84.
Blaschke TF, Osterberg L, Vrijens B, Urquhart J. Adherence to medications: insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu Rev Pharmacol Toxicol. 2012;52:275–301.
Brittain ST, Wheless JW. Pharmacokinetic simulations of topiramate plasma concentrations following dosing irregularities with extended-release vs. immediate-release formulations. Epilepsy Behav. 2015;52:31–6.
Brown MT, Bussell J, Dutta S, Davis K, Strong S, Mathew S. Medication adherence: truth and consequences. Am J Med Sci. 2016;351:387–99.
Bulloch AG, Patten SB. Non-adherence with psychotropic medications in the general population. Soc Psychiatry Psychiatr Epidemiol. 2010;45:47–56.
Cerovecki A, Musil R, Klimke A, Seemüller F, Haen E, Schennach R, et al. Withdrawal symptoms and rebound syndromes associated with switching and discontinuing atypical antipsychotics: theoretical background and practical recommendations. CNS Drugs. 2013;27:545–72.
Chen C, Wright J, Gidal B, Messenheimer J. Assessing impact of real-world dosing irregularities with lamotrigine extended-release and immediate-release formulations by pharmacokinetic simulation. Ther Drug Monit. 2013;35:188–93.
Clatworthy J, Bowskill R, Parham R, Rank T, Scott J, Horne R. Understanding medication non-adherence in bipolar disorders using a necessity-concerns framework. J Affect Disord. 2009;116:51–5.
Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–310.
Comté L, Vrijens B, Tousset E, Gérard P, Urquhart J. Estimation of the comparative therapeutic superiority of QD and BID dosing regimens, based on integrated analysis of dosing history data and pharmacokinetics. J Pharmacokinet Pharmacodyn. 2007;34:549–58.
Copeland LA, Zeber JE, Salloum IM, Pincus HA, Fine MJ, Kilbourne AM. Treatment adherence and illness insight in veterans with bipolar disorder. J Nerv Ment Dis. 2008;196:16–21.
Correll CU. From receptor pharmacology to improved outcomes: individualising the selection, dosing, and switching of antipsychotics. Eur Psychiatry. 2010;25(Suppl 2):S12–21.
Dunbar-Jacob J, Mortimer-Stephens MK. Treatment adherence in chronic disease. J Clin Epidemiol. 2001;54(Suppl 1):S57–60.
Fava GA, Gatti A, Belaise C, Guidi J, Offidani E. Withdrawal symptoms after selective serotonin reuptake inhibitor discontinuation: a systematic review. Psychother Psychosom. 2015;84:72–81.
Fields J, Go JT, Schulze KS. Pill properties that cause dysphagia and treatment failure. Curr Ther Res Clin Exp. 2015;77:79–82.
Fountoulakis KN, Grunze H, Vieta E, Young A, Yatham L, Blier P, Kasper S, Moeller HJ. The International College of Neuro-Psychopharmacology (CINP) treatment guidelines for bipolar disorder in adults (CINP-BD-2017), part 3: the clinical guidelines. Int J Neuropsychopharmacol. 2017;20:180–95.
Frank E, Gonzalez JM, Fagiolini A. The importance of routine for preventing recurrence in bipolar disorder. Am J Psychiatry. 2006;163:981–5.
Franks M, Macritchie KA, Mahmood T, Young AH. Bouncing back: is the bipolar rebound phenomenon peculiar to lithium? A retrospective naturalistic study. J Psychopharmacol. 2008;22:452–6.
Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: a summary of the literature. Med Care. 2004;42:649–52.
García S, Martínez-Cengotitabengoa M, López-Zurbano S, Zorrilla I, López P, Vieta E, et al. Adherence to antipsychotic medication in bipolar disorder and schizophrenic patients: a systematic review. J Clin Psychopharmacol. 2016;36:355–71.
Goldberg JF, Brooks JO 3rd, Kurita K, Hoblyn JC, Ghaemi SN, Perlis RH, et al. Depressive illness burden associated with complex polypharmacy in patients with bipolar disorder: findings from the STEP-BD. J Clin Psychiatry. 2009;70:155–62.
Golden JC, Goethe JW, Woolley SB. Complex psychotropic polypharmacy in bipolar disorder across varying mood polarities: a prospective cohort study of 2712 inpatients. J Affect Disord. 2017;221:6–10.
Gonzalez-Pinto A, Mosquera F, Alonso M, López P, Ramírez F, Vieta E, et al. Suicidal risk in bipolar I disorder patients and adherence to long-term lithium treatment. Bipolar Disord. 2006;8:618–24.
Grenard JL, Munjas BA, Adams JL, Suttorp M, Maglione M, McGlynn EA, et al. Depression and medication adherence in the treatment of chronic diseases in the United States: a meta-analysis. J Gen Intern Med. 2011;26:1175–82.
Harden CL. Generic modified-release antiepileptic drugs: no difference within formulations, but important differences across formulations. Epilepsy Curr. 2017;17:29–31.
Hassan M, Lage MJ. Risk of rehospitalization among bipolar disorder patients who are nonadherent to antipsychotic therapy after hospital discharge. Am J Health Syst Pharm. 2009;66:358–65.
Hawkshead J, Krousel-Wood MA. Techniques for measuring medication adherence in hypertensive patients in outpatient settings. Disease Manag Health Outcomes. 2007;15:109–18.
Hong J, Reed C, Novick D, Haro JM, Aguado J. Clinical and economic consequences of medication non-adherence in the treatment of patients with a manic/mixed episode of bipolar disorder: results from the European Mania in Bipolar Longitudinal Evaluation of Medication (EMBLEM) study. Psychiatry Res. 2011;190:110–4.
Hughes D. Less is more: medicines that require less frequent administration improve adherence, but are they better? Pharmacoeconomics. 2006;24:211–3.
Hughes DA. Estimation of the impact of noncompliance on pharmacokinetics: an analysis of the influence of dosing regimens. Br J Clin Pharmacol. 2008;65:871–8.
Ingersoll KS, Cohen J. The impact of medication regimen factors on adherence to chronic treatment: a review of literature. J Behav Med. 2008;31:213–24.
Johnson FR, Ozdemir S, Manjunath R, Hauber AB, Burch SP, Thompson TR. Factors that affect adherence to bipolar disorder treatments: a stated-preference approach. Med Care. 2007;45:545–52.
Jónsdóttir H, Opjordsmoen S, Birkenaes AB, Engh JA, Ringen PA, Vaskinn A, et al. Medication adherence in outpatients with severe mental disorders: relation between self-reports and serum level. J Clin Psychopharmacol. 2010;30:169–75.
Kessing LV, Sondergard L, Kvist K, Andersen PK. Adherence to lithium in naturalistic settings: results from a nationwide pharmacoepidemiological study. Bipolar Disord. 2007;9:730–6.
Kessing LV, Vradi E, Andersen PK. Nationwide and population-based prescription patterns in bipolar disorder. Bipolar Disord. 2016;18:174–82.
Kleimann A, Schrader V, Stübner S, Greil W, Kahl KG, Bleich S, et al. Psychopharmacological treatment of 1650 in-patients with acute mania-data from the AMSP study. J Affect Disord. 2016;191:164–71.
Kukreja S, Kalra G, Shah N, Shrivastava A. Polypharmacy in psychiatry: a review. Mens Sana Monogr. 2013;11:82–99.
Levin JB, Sams J, Tatsuoka C, Cassidy KA, Sajatovic M. Use of automated medication adherence monitoring in bipolar disorder research: pitfalls, pragmatics, and possibilities. Ther Adv Psychopharmacol. 2015;5:76–87.
Lopez LV, Shaikh A, Merson J, Greenberg J, Suckow RF, Kane JM. Accuracy of clinician assessments of medication status in the emergency setting: a comparison of clinician assessment of antipsychotic usage and plasma level determination. J Clin Psychopharmacol. 2017;37:310–4.
Marder SR. Overview of partial compliance. J Clin Psychiatry. 2003;64(Suppl 16):3–9.
Monnette A, Zhang Y, Shao H, Shi L. Concordance of adherence measurement using self-reported adherence questionnaires and medication monitoring devices: an updated review. Pharmacoeconomics. 2018;36:17–27.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97.
Osterberg LG, Urquhart J, Blaschke TF. Understanding forgiveness: minding and mining the gaps between pharmacokinetics and therapeutics. Clin Pharmacol Ther. 2010;88:457–9.
Pan W, Connett JE. Selecting the working correlation structure in generalized estimating equations with application to the lung health study. Statistica Sinica. 2002;12:475–90.
Parker GB, Graham RK, Tavella G. Is there consensus across international evidence-based guidelines for the management of bipolar disorder? Acta Psychiatr Scand. 2017;135:515–26.
Pearson CR, Simoni JM, Hoff P, Kurth AE, Martin DP. Assessing antiretroviral adherence via electronic drug monitoring and self-report: an examination of key methodological issues. AIDS Behav. 2007;11:161–73.
Pellock JM, Brittain ST. Use of computer simulations to test the concept of dose forgiveness in the era of extended-release (XR) drugs. Epilepsy Behav. 2016;55:21–3.
Peselow ED, Naghdechi L, Pizano D, IsHak WW. Polypharmacy in maintenance of bipolar disorder. Clin Neuropharmacol. 2016;39:132–4.
Pincus SM. Approximate entropy as a measure of system complexity. Proc Natl Acad Sci USA. 1991;88:2297–301.
Pincus SM, Gladstone IM, Ehrenkranz RA. A regularity statistic for medical data analysis. J Clin Monit. 1991;7:335–45.
Pincus SM, Cummins TR, Haddad GG. Heart rate control in normal and aborted-SIDS infants. Am J Physiol. 1993;264:R638–46.
Pompili M, Serafini G, Del Casale A, Rigucci S, Innamorati M, Girardi P, et al. Improving adherence in mood disorders: the struggle against relapse, recurrence and suicide risk. Expert Rev Neurother. 2009;9:985–1004.
Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med. 2005;61:133–55.
Razzano LA, Cook JA, Burke-Miller JK, Mueser KT, Pickett-Schenk SA, Grey DD, et al. Clinical factors associated with employment among people with severe mental illness: findings from the employment intervention demonstration program. J Nerv Ment Dis. 2005;193:705–13.
Rej S, Herrmann N, Shulman K, Fischer HD, Fung K, Gruneir A. Current psychotropic medication prescribing patterns in late-life bipolar disorder. Int J Geriatr Psychiatry. 2017;32:1459–65.
Richter A, Anton SF, Koch P, Dennett SL. The impact of reducing dose frequency on health outcomes. Clin Ther. 2003;25:2307–35.
Sachs GS, Peters AT, Sylvia L, Grunze H. Polypharmacy and bipolar disorder: what’s personality got to do with it? Int J Neuropsychopharmacol. 2014;17:1053–61.
Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15:e22–33.
Sajatovic M, Bauer MS, Kilbourne AM, Vertrees JE, Williford W. Self-reported medication treatment adherence among veterans with bipolar disorder. Psychiatr Serv. 2006;57:56–62.
Sajatovic M, Ignacio RV, West JA, Cassidy KA, Safavi R, Kilbourne AM, et al. Predictors of nonadherence among individuals with bipolar disorder receiving treatment in a community mental health clinic. Compr Psychiatry. 2009;50:100–7.
Sajatovic M, Velligan DI, Weiden PJ, Valenstein MA, Ogedegbe G. Measurement of psychiatric treatment adherence. J Psychosom Res. 2010;69:591–9.
Samtani MN, Sheehan JJ, Fu DJ, Remmerie B, Sliwa JK, Alphs L. Management of antipsychotic treatment discontinuation and interruptions using model-based simulations. Clin Pharmacol. 2012;4:25–40.
Schuepbach D, Novick D, Haro JM, Reed C, Boeker H, Noda S, et al. Determinants of voluntary vs. involuntary admission in bipolar disorder and the impact of adherence. Pharmacopsychiatry. 2008;41:29–36.
Scott J, Pope M. Nonadherence with mood stabilizers: prevalence and predictors. J Clin Psychiatry. 2002;63:384–90.
Shi L, Liu J, Koleva Y, Fonseca V, Kalsekar A, Pawaskar M. Concordance of adherence measurement using self-reported adherence questionnaires and medication monitoring devices. Pharmacoeconomics. 2010;28:1097–107.
Spina E, Pisani F, de Leon J. Clinically significant pharmacokinetic drug interactions of antiepileptic drugs with new antidepressants and new antipsychotics. Pharmacol Res. 2016;106:72–86.
Stephenson JJ, Tunceli O, Gu T, Eisenberg D, Panish J, Crivera C, et al. Adherence to oral second-generation antipsychotic medications in patients with schizophrenia and bipolar disorder: physicians’ perceptions of adherence vs. pharmacy claims. Int J Clin Pract. 2012;66:565–73.
Swan M. The quantified self: fundamental disruption in big data science and biological discovery. Big Data. 2013;1:85–99.
Urquhart J. Pharmacodynamics of variable patient compliance: implications for pharmaceutical value. Adv Drug Deliv Rev. 1998;33:207–19.
Urquhart J, Vrijens B. ‘Hedged’ prescribing for partially compliant patients. Clin Pharmacokinet. 2006;45:105–8.
Velligan DI, Weiden PJ, Sajatovic M, Scott J, Carpenter D, Ross R, et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry. 2009;70(Suppl 4):1–46.
Vieta E, Azorin JM, Bauer M, Frangou S, Perugi G, Martinez G, et al. Psychiatrists’ perceptions of potential reasons for non- and partial adherence to medication: results of a survey in bipolar disorder from eight European countries. J Affect Disord. 2012;143:125–30.
Vrijens B, Heidbuchel H. Non-vitamin K antagonist oral anticoagulants: considerations on once- vs. twice-daily regimens and their potential impact on medication adherence. Europace. 2015;17:514–23.
Vrijens B, Urquhart J. Methods for measuring, enhancing, and accounting for medication adherence in clinical trials. Clin Pharmacol Ther. 2014;95:617–26.
Vrijens B, Claeys MJ, Legrand V, Vandendriessche E, Van de Werf F. Projected inhibition of platelet aggregation with ticagrelor twice daily vs. clopidogrel once daily based on patient adherence data (the TWICE project). Br J Clin Pharmacol. 2014;77:746–55.
Wagner GJ, Ryan GW. Relationship between routinization of daily behaviors and medication adherence in HIV-positive drug users. AIDS Patient Care STDS. 2004;18:385–93.
Weinstock LM, Gaudiano BA, Epstein-Lubow G, Tezanos K, Celis-Dehoyos CE, Miller IW. Medication burden in bipolar disorder: a chart review of patients at psychiatric hospital admission. Psychiatry Res. 2014;216:24–30.
Authors’ contributions
MP, MB, TG and PW worked on the conception and design of the study, interpreted the results and drafted the manuscript. TG performed the analyses. NR, MA, KS, PG, RM; WM, SM, ES, RB, and PR performed data collection, and interpretation of the findings. All authors read and approved the final manuscript.
Acknowledgements
We acknowledge support by the Open Access Publication Funds of the TU Dresden.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The data will not be shared or made publicly available. Informed consent for this was not sought from the study participants prior to the collection of data.
Consent for publication
Consent to publish has been obtained from the participants.
Ethics approval and consent to participate
All participating centers obtained approval from their Institutional Review Boards and all patients gave a written informed consent to participate in this naturalistic observational non-interventional study. The data used for this paper were derived from a naturalistic observational non-interventional study, which at the time of inclusion was not registered.
Funding
Open Access publication was funded by Publication Funds of the TU Dresden.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Pilhatsch, M., Glenn, T., Rasgon, N. et al. Regularity of self-reported daily dosage of mood stabilizers and antipsychotics in patients with bipolar disorder. Int J Bipolar Disord 6, 10 (2018). https://doi.org/10.1186/s40345-018-0118-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40345-018-0118-8