Abstract
Background
The prevalence of eating disorders is higher in transgender and non-binary compared to cisgender people. Gender diverse people who seek eating disorder treatment often report struggling to find affirming and inclusive treatment from healthcare clinicians. We sought to understand eating disorder care clinicians’ perceptions of facilitators of and barriers to effective eating disorder treatment for transgender and gender diverse patients.
Methods
In 2022, nineteen US-based licensed mental health clinicians who specialized in eating disorder treatment participated in semi-structured interviews. We used inductive thematic analysis to identify themes around perceptions and knowledge of facilitators and barriers to care for transgender and gender diverse patients diagnosed with eating disorders.
Results
Two broad themes were identified: (1) factors affecting access to care; and (2) factors affecting care while in treatment. Within the first theme, the following subthemes were found: stigmatization, family support, financial factors, gendered clinics, scarcity of gender-competent care, and religious communities. Within the second theme, prominent subthemes included discrimination and microaggressions, provider lived experience and education, other patients and parents, institutions of higher education, family-centered care, gendered-centered care, and traditional therapeutic techniques.
Conclusion
Many barriers and facilitators have potential to be improved upon, especially those caused by clinicians’ lack of knowledge or attitudes towards gender minority patients in treatment. Future research is needed to identify how provider-driven barriers manifest and how they can be improved upon to better patient care experiences.
Plain English summary
Eating disorders are more common among transgender and non-binary compared to cisgender people. Despite this, gender diverse people who seek eating disorder treatment often report struggling to find affirming and inclusive care. We interviewed nineteen US-based licensed mental health clinicians who specialized in eating disorder treatment to learn perceptions and knowledge of facilitators and barriers to care for transgender and gender diverse patients diagnosed with eating disorders. Factors affecting access to care included stigmatization, family support, financial factors, gendered clinics, scarcity of gender-competent care, and religious communities. Factors affecting care while in treatment included discrimination and microaggressions, provider lived experience and education, other patients and parents, institutions of higher education, family-centered care, gendered-centered care, and traditional therapeutic techniques. This research identified barriers and facilitators with the potential for improvement, especially those caused by clinician’s lack of knowledge or attitudes towards gender minority patients in treatment.
Similar content being viewed by others
Background
In the United States, 14.4 million people have had an eating disorder (ED) in their lifetime [1]. Self-reported history of EDs has been found to occur among 7.4–17.6% of transgender individuals generally [2–4] and among 4.32% of transgender individuals who have received gender affirming medical intervention [5]. Transgender and gender diverse people (gender minorities) are those whose gender identity differs from the gender they were assigned at birth. Some gender diverse people identify as neither a man nor a woman, or as a combination of male and female, and may use one or several terms (i.e., non-binary, gender fluid, demi-girl, demi-boy) to describe their gender identity [6]. The prevalence of EDs among transgender people is greater than among people whose gender identity aligns with gender assigned at birth (cisgender) [2].
Gender minority individuals often struggle to find healthcare that is both affirming and inclusive [7–10]. Some delay healthcare visits due to fear of discrimination. Depression and suicide attempts are much higher among those who delay healthcare visits out of fear of discrimination relative to those who do not [7]. Those seeking mental health care might be plagued with added stressors. A study using the 2015 United States Transgender Survey reported that nearly 25% of gender minority respondents had to educate their provider on gender identity [11]. Further, 18.8% of transgender women, 21.1% of transgender men, 72.5% of nonbinary, assigned female at birth, and 65.6% of nonbinary, assigned male at birth did not feel respected by their provider after identifying themselves as transgender [11]. Despite these challenges, more than half develop relationships with health care clinicians with whom they are very satisfied [12].
Qualitative studies reporting the narratives of gender minority patients seeking and receiving treatment for an ED are consistent with reports based on overall engagement with the health care system. Many describe instances of having received discriminatory comments and microaggressions from clinicians and other members of the care team. Patients emphasize experiencing fear and anxiety due to uncertainty about how inclusive a provider may be especially when attending appointments with specialists (e.g., nutritionist, internists, dentists) whom they were referred to by their primary ED care provider [3, 13, 14]. In response to the need to improve care provided to gender minority patients, the American Psychological Association developed provider standards of care for gender competent treatment [15]. Yet, analyses of patient narratives derived from two different projects led by FEDUp (Fighting Eating Disorders in Underrepresented Populations) reveal these standards of care may not have diffused into clinical practice [3, 13]. Transgender patients seeking and receiving eating disorder treatment felt that the clinicians with whom they engaged were generally unfamiliar with specific needs of transgender patients related to body image and the role of the body in traditionally structured ED treatment. Some clinicians were seen as blaming the ED entirely on the patients wanting to affirm their gender identity [3, 13, 14] and others accused patients of coming out as a means of attention seeking [14]. Most disturbingly, some clinicians suggested that symptoms of a transgender patient’s ED may lessen if the patient accepted the gender they were assigned at birth [3, 13].
Gender minority patients have clearly identified where clinicians may fail them throughout their ED treatment. The current analysis explores provider awareness of facilitators of and barriers to inclusive care for gender minority patients with EDs. Provider perspectives on these facilitators and barriers lend further insight into effective means to better address the unique health care needs of gender minority patients in the ED care setting. Through individual interviews with mental health clinicians caring for patients with EDs, we sought to learn more about provider perceptions of the barriers and facilitators to successful ED treatment for transgender and gender diverse patients and to elicit provider perspectives of the experiences of these vulnerable patients.
Conceptual model
We evaluated provider perceptions and perspectives using deductive analysis guided by the Social-Ecological Model [15]. This model is built on the premise that health outcomes and healthcare experiences are the result of mutual interactions between individuals, groups, and their immediate and extended social environments. This model is particularly helpful in allowing those who seek to develop effective policies and health promotion measures and provide a richer understanding of the patient-provider interactions, clinic settings, the regulatory and policy environment, and broader social structural factors they seek to change [15].
Methods
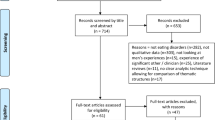
We conducted a series of individual semi-structured interviews with 19 clinicians in the United States, specializing in eating disorder treatment. Interviews addressed a range of topics related to their familiarity with transgender and gender diverse populations, perceptions of facilitators, and barriers to care, and opportunities for intervention and improvement of the delivery of ED care to transgender and gender diverse populations. The current analysis focuses on provider perceptions of gender minority patients’ experiences and challenges with eating disorder treatment.
Setting and participants
We contacted potential participants from all US states and territories using email solicitation, social media messaging, and snowball sampling. We sought to recruit professionals with experience in a range of ED treatment settings and approaches to care and to capture a diverse sample. Eligible clinicians were older than 18 years, were fluent in English, had to have access to a phone or Zoom, were licensed to provide mental health treatment, and had at least one year of experience at their current role. Providers did not have to have experience working with gender minority clients to participate.
Procedures
We identified mental health clinicians who specialized in ED treatment from the Psychology Today website (Psychology Today). All listed with a link to their website or an email address were contacted via email until sufficient representation was achieved for race, gender, and age. Additionally, clinicians were recruited via social media (Instagram) and personal academic networks (an ED interest email newsletter). Recruitment lasted 2 months. Potential participants who expressed interest in response to the recruitment messages sent via email or social media direct messaging were asked to complete a screening survey. Those who met our inclusion criteria were invited to participate and were sent the link to a background/demographic questionnaire. To improve the diversity of the pool of participants, we asked participants to identify potential respondents from their own networks who represented geographic and philosophic approaches to eating disorder care different from their own.
Web surveys and questionnaire responses for demographic and provider attitude and education data were collected and managed using REDCap electronic data capture tools [16, 17] hosted at the University of Massachusetts Chan Medical School. REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies. Participants provided consent electronically and confirmed being 18 years of age or older before completing the study background and demographics questionnaire. Questionnaires were completed before interviews; however, participants were told during the consent process that their survey responses would not be reviewed until after the interview when data analysis began. To ensure the anonymity of participants, each was assigned a participant ID. Participant names and email addresses with a matching participant ID were stored separately from participant data. All data were maintained on a secure research drive at the University of Massachusetts Chan Medical School.
Participants each met once with the interviewer (KF), via Zoom. KF is a cisgender female doctoral candidate with qualitative research experience. Semi-structured interviews were conducted using an interview protocol based on findings from Duffy et al. (2016) and Hartman-Munick et al. (2021) (See Additional file 1: Appendix A). Interviews were conducted in English and lasted 45–60 min. Elements of consent were verbally reviewed with participants prior to the start of each interview using an IRB approved Fact Sheet. Zoom audio recordings were downloaded onto secure University of Massachusetts Chan Medical School laptops connected to a secure verified network and transferred to a secure network drive for storage. Zoom video recordings and chat records were permanently deleted.
Data analysis
Interviews were transcribed from Zoom audio files using Otter.ai. Transcripts were cleaned, deidentified, and verified by KF and EM. Final transcripts were independently coded by two researchers (KF and EM), who both identify as cisgender females. Coders met weekly to review coding discrepancies and new themes as they were identified. We used NVivo [18] for coding and employed inductive thematic analysis [19] to identify themes. Interrater reliability was calculated and found 94.3% agreement between coders.
Results
Characteristics of participant
Table 1 shows the characteristics of the 19 study participants. Participants were predominantly from the South, but geographic diversity was obtained, as was diversity age, race/ethnicity, gender identify, and practice setting.
Gender identity and ED risk
Many clinicians discussed the increased risk for developing an ED among gender minority individuals (particularly youth) relative to cisgender (n = 6). Additionally, most clinicians noted that those undergoing puberty may use disordered eating behaviors to mitigate the impact of puberty on their bodies and reduce dysphoria (n = 10). Use of disordered eating for this purpose was perceived among clinicians as a risk factor for more moderate to severe ED among gender minority youth (n = 3). Higher risk was also attributed to gender dysphoria, limited accessibility of gender affirming care in the US, experiences of trauma (n = 11), physical violence (n = 5), and stigmatization (n = 8).
Factors affecting access to care
Regarding barriers to ED treatment and patients’ experience within US mental health treatment settings, clinicians cited the following factors: stigmatization, family, financial factors, gendered clinics, scarcity of gender competent care, and religious communities. Quotes supporting these findings can be found in Table 2.
Stigmatization
Most felt that gender minority patients’ fear of stigmatization or trauma triggered from prior experiences can prevent them from seeking treatment (n = 10). Clinicians recognized themselves, patient peers, as well as the family of patient peers, and patients’ own family members as having roles in shaming, silencing, or rejecting gender minority individuals. A few clinicians acknowledged their historical role as gatekeepers in accessing gender affirming care (n = 3), which they felt has contributed to gender minority patients’ distrust when seeking out psychological services, including ED treatment.
Family support
Clinicians perceived a lack of family support as negative in its impact on gender minority children seeking ED treatment (n = 19). According to several clinicians, it was not uncommon for unsupportive parents to limit their children to treatment facilities and clinicians who adhered to parental values and beliefs around gender identity (n = 10), particularly in religious communities (n = 3). Some clinicians observed that patients with unsupportive family members delayed seeking care or coming out until they were living independently as adults, to avoid familial and community conflict as youth (n = 3). They speculated that, as a result, gender related distress and ED symptomology were likely prolonged. Many families, however, were described as supportive, which allowed patients to easily access care. According to clinicians, many parents who, in one way or another, receive education around gender identity and eating disorders may be less likely to hinder their child’s ability to continue in or pursue care with affirming clinicians (n = 6).
Financial factors
It was noted that many clinicians and clinics (generally) treating EDs do not accept insurance. Cost of care was viewed as a great impediment for patients who may need to choose between costly gender affirming medical intervention or ED treatment when their safety and wellbeing may require both (n = 9). Several observed that most patients could rarely afford both types of care (n = 7).
Clinicians associated lack of financial support for ED treatment with lack of gender affirmation from family (n = 5). A few participants reflected on instances where young gender minority individuals were kicked out of their homes, having to support themselves with low-income jobs often without health insurance (n = 3). A concern was that those with insurance may find that ED care is not covered due to incongruence between gender assigned at birth and their current gender identity (n = 2).
Gendered clinics—cis female only
Clinicians highlighted that female-only residential treatment facilities, may be unappealing to gender minority patients even if they are welcomed by staff (n = 3). Patients may try to seek care elsewhere, but other mixed gender facilities may be less financially feasible to access due to 1) distance from the patient (n = 4) or 2) because facilities have staff who are discriminatory or not gender competent (n = 7).
Scarcity of gender competent care
Several clinicians noted their gender minority patients struggled to identify safe clinicians located outside of their city or state (i.e., mental health clinicians and other healthcare specialists) (n = 7). This struggle was thought to be exacerbated by a scarcity of gender-competent ED treatment professionals (n = 5). Accessing affirming or competent ED care was generally felt to be more difficult for those living (1) where care in general is scarce (patients may need to travel to access it) (n = 4) and (2) in states with more conservative political leanings (n = 5) which was believed to be a barrier as patients may be unsure of whether a provider’s political ideology facilitates discrimination towards gender minority individuals.
Religious communities
A few clinicians were familiar with the struggles of gender minority individuals living in communities with large religious populations. Clinicians who disclosed that they work or have worked in these communities (n = 4) explained that gender minority clients seeking care were often hindered by spiritual leaders and religious family members (n = 4), more so if care affirmed gender identities that were not felt to be compliant with religious doctrine (n = 2). Two of the four clinicians conveyed that it was not uncommon for gender minority patients to avoid care or struggle throughout care because they feel their identity conflicted with their religious values. Some participants felt that clinicians in religious communities are often not prepared to help patients grapple with seemingly conflicting identity and spirituality (n = 2).
Factors affecting care while in treatment
Clinicians cited the following factors affecting gender minority patients’ care while in ED treatment: discrimination and microaggressions, provider lived experience and education, other patients and parents, systems of higher education, family-centered care, gender-centered care, and traditional therapeutic techniques. Quotes supporting these findings can be found in Table 3.
Discrimination and microaggressions
Clinicians considered lack of acceptance and validation or microaggressions from other clinicians, peers in treatment, and family as barriers to successful treatment and sources of trauma for gender minority patients. Clinicians broadly associated discrimination from clinicians with being older (n = 4), having restrictive religious or political beliefs (n = 10), limited knowledge around gender identity (n = 5), and stigmas around gender identity (n = 7). Some interview participants spent time preparing gender minority patients to cope with other clinicians, usually specialists outside of their practice, whose beliefs were unknown or were known to be discriminatory but were the only option for these patients (n = 2).
Provider lived experience and education
Many clinicians perceived the mental health community broadly as well as those providing ED treatment to be poorly trained to work closely with gender minority patients (n = 17). Some clinicians discussed how patients are frequently burdened with educating clinicians about gender identity generally and as it applies to their eating disorder (n = 11). A handful of clinicians recognized that while patients are excellent first-hand resources, they should not have to take on the task of bringing clinicians up to speed on how to provide gender informed treatment (n = 5). Some clinicians discussed the benefits of programs that had staff who reflected the gender, racial, and ethnic identities of patients; stating that programs with diverse staff were more effective in their ability to provide a safe, informed, and relatable space for patients with similar identities (n = 7).
Other patients and parents
Among clinicians who offered it, group therapy was often deemed an inclusive space for gender minority patients, particularly when practices/clinics had established rules for interpersonal respect in that setting (n = 4). Use of telehealth platforms for group therapy raised some concerns about potential harm, such as inadvertently exposing patients’ personal beliefs (i.e., posters, signs, flags—in video background) or exposing identities of group members to others in a household or workplace, which otherwise may have never surfaced in an in-person clinic session (n = 2). Clinicians felt that instances such as these had reduced comfort for gender minority patients. Additionally, numerous clinicians noted that it was not uncommon for a roommate’s parents, unsatisfied with their child’s roommate’s gender identity, to either remove their child from treatment at that clinic or have them relocated to another room (n = 5). It was also mentioned that some parents of other patients had made bigoted comments about gender minority patients (n = 3).
Institutions of higher education
One provider felt that despite the counselling center at their religious university making efforts to provide safe and inclusive care, the broader university culture often counteracted much of that work. Of clinicians who acknowledged having experience working in college counseling centers (n = 5), three reported feeling that they were often a patient’s only source of affirmation, and that patients with limited support outside of the clinical setting may struggle to excel in their recovery. Additionally, two noted that gender minority patients may require several sessions before feeling safe and ready to be transparent with their provider. This may limit progress patients and clinicians can make with ED recovery, as students are typically only on campus for 2–4 years and may only be allotted a fixed number of sessions per year.
Additionally, counseling center clinicians’ efforts to make materials more inclusive were sometimes slowed by institutional procedures, policy or culture and influenced by donors, politicians, or personal beliefs of institutional leadership (n = 4). Some described pushbacks from leadership when seeking to develop and promote inclusive messaging and programming, which they felt was necessary for their clinics to promote based on the political actions of their states towards transgender individuals, in recent years (n = 2). Another clinician indicated that in addition to their institution’s religious teachings preventing them from having an LGBTQ specific group therapy program for years, once the group did receive approval, they could not title the group as being an LGBTQ support group due to the discriminatory culture on campus.
Family-centered care
Clinicians had a range of experiences with families of their gender minority patients; some with many supportive parental encounters and others reporting few to no encounters with supportive family. The role of the family is often central to ED treatment, primarily for youth. This was mentioned by most providers (n = 16). The majority of clinicians described family-centered care as most effective when parents affirmed their child’s identity (n = 15). Families who made efforts to self-educate or who were open to being educated by clinicians were viewed as great sources of support in their child’s ED recovery (n = 6). Conversely, clinicians recalled instances of unsupportive parents extracting their children from ED treatment if their child’s identity was being affirmed by clinicians (n = 5). Unsupportive parents reportedly exhibited counterproductive behaviors while their children were receiving care, having persisted in efforts to invalidate their child’s identity by using their old name (deadnaming) or misgendering them (n = 7). Several clinicians feared accidentally outing patients, while trying to affirm their identity and tiptoeing around difficult or toxic family members (n = 7).
Gender-centered care
In some female-only facilities, where transmasculine patients (female transitioning/ed to male) were receiving care, clinicians expressed concern for: (1) patients not feeling included in therapeutic programming due to their gender identity (n = 4), (2) therapeutic focus on the cisgender female body (n = 7), (3) provider unfamiliarity with working with patients identifying as male or non-binary (n = 6), and (4) a lack of neutral facilities (i.e. restrooms)—all of which may cause distress for gender minority patients in recovery (n = 3). Clinicians looked negatively upon instances where gender minority patients were placed in care wings for the gender they were assigned at birth, rather than their current gender identity (n = 4).
Traditional therapeutic techniques
A lack of knowledge around therapies that accommodate ED patients with gender dysphoria was discussed by many clinicians (n = 12). Most clinicians felt available ED treatments were not designed with transgender or gender diverse bodies in mind (n = 8); many felt unprepared to navigate providing non-triggering treatments to gender minority patients, especially to those undergoing medical transition (n = 9). Consequently, patients communicated feelings of distress to clinicians about traditional approaches to care such as observing their body in a mirror, engaging in body-positive and body acceptance talk, and exposure therapies such as residential facility field trips to practice body acceptance in retail clothing stores. Clinicians reported instances of gender minority patients feeling triggered around body-centric activities, especially in gendered settings such as fitting rooms or clinic restrooms (n = 3). Several clinicians noted that their clinic or other clinics had made changes to their facilities to provide focused programming for gender minority individuals (i.e., Intensive Outpatient Program, Partial Hospitalization Program) (n = 7). According to these clinicians, patient response was overwhelmingly positive, and programming was well utilized by members of these populations.
Discussion
Provider perceptions in the current study were in line with findings from previous studies of patient perspectives, focused on provider and systemic influences, which have hindered patients from productive and safe eating disorder treatment. Our analysis generated two overarching themes: (1) barriers to accessing care/finding provider and (2) barriers to receiving therapeutic and safe care. Many barriers to accessing care and barriers to receipt of effective and safe care were similar but had differing impacts.
In our study the role of family in eating disorder treatment and in the lives of gender minority patients was prominent. Clinicians in the current study noted the need to consider how the attitudes of their patient’s families towards their gender identity can impact success in treatment; a barrier not discussed in patient studies. The role of family in eating disorder treatment may cause unease, particularly among those who are not yet out to their families or clinicians. Many gender minority patients don’t come out at all throughout treatment to avoid mistreatment, discrimination, or other burdens imposed on them by clinicians while they are seeking help for their eating disorder [3]. Clinicians in our study noted that patients may wait to come out until they are living independently for similar reasons. Previous studies with patient participants have largely explored care experiences in those older than 18 years [3, 13, 14]; our study allowed clinicians to reflect on the experiences of patients of all ages, including the experiences of younger patients, ranging from middle school to college, who are more impacted by the role of family, and adult patients who are more independent and less impacted. Research to better understand how family centered therapeutic styles may serve as barriers to care for gender minority youth is warranted.
Clinicians in our study honed in on unique roles that patients’ social contexts and communities have on their ability to access and receive quality eating disorder care. The use of religion to justify denial of care disproportionately impacted gender minority individuals—under Conscience Clauses. The language of Conscience Clauses affords clinicians the right to refuse to provide care to transgender individuals if they feel that (1) they would need to discuss gender affirming medical intervention in any way or (2) if a condition is so much as tangentially associated with the patient’s gender identity [20]. A 2016 Center for American Progress survey found that 29% of transgender individuals were refused the ability to even see a health care provider, because of provider attitudes towards gender minority individuals [21]. Twelve percent managed to see a health care provider but the provider, because of their religious beliefs, refused to provide affirming care to the patient.
Institutions of higher learning can have direct roles in selecting what care is available to their students who use on-campus health services. According to clinicians, influence from upper leadership on campuses has resulted in an inability to use inclusive messaging to welcome gender minority patients or to provide certain types of healthcare for these individuals. Barriers to counseling center treatment were a novel finding in this study and should raise cause for concern, as gender minority individuals entering college counseling centers for care are more likely to have more severe mental health concerns than their cisgender peers [22]. Limiting or denying access to safe, affirming eating disorder care can delay a patient from entering care for their eating disorder or other treatment for other mental health conditions. Gender minority college students are 4–6 times as likely as cisgender college students to be diagnosed with an eating disorder [2]. Additionally, eating disorders increase risk for suicide and suicidal ideation, especially among gender minority individuals [23]. Risk for suicide or suicidal ideation can be exacerbated if patients are unable to access affirming care or are subjected to transphobia [24, 25]. For these reasons, the barriers that clinicians identified in these care settings serve as cause for concern. Improving access to affirming care and accommodating the needs of gender minority students on college campuses is imperative.
Clinicians in our study who worked on religious affiliated campuses and within religious communities mentioned methods of accessing care through ecclesiastical leaders as a means of getting eating disorder treatment. Despite access to care through religious pathways, transgender patients were hesitant to do so as the gender they identify as or avoided care until later in life. The religious affiliations for campus clinicians in this study did not support receipt of gender affirming care and clinicians noted that this had detrimental effects on their gender minority patients. Religiosity has been shown to be associated with negative attitudes towards gender minority individuals [26, 27]. Religiosity of a community in which a gender minority individual lives or practices their faith has been identified as a barrier for them in seeking to access health care generally [28]. However, there is a paucity of research exploring how access to care through religious pathways has impacted ED outcomes and experiences for gender minority individuals.
Study participants were particularly aware of the ways in which discrimination manifested and impacted patients. In prior studies, avoidance of treatment due to misgendering, or continued use of an old name (i.e., deadnaming), and/or clinicians using incorrect pronouns were noted as major barriers that prevented gender minority patients from receiving care for their eating disorder [29]. Twenty three percent of gender minority patients receiving any type of healthcare have reported being misgendered or deadnamed by a provider [21]. Our participants confirmed that it was not only difficult for patients to find affirming clinicians, but it was difficult for clinicians themselves to identify safe clinicians for referrals. Gender minority patients have expressed frustration with the uncertainty of safety or acceptance when seeking out a provider for eating disorder treatment—preferring that clinicians clearly identify themselves as allies of transgender and non-binary patients [13]. Although many clinicians may claim to be accepting, both patients and clinicians have found that clinicians who self-identify as allies are not always living up to that expectation [13, 14]. Clinicians and patients who identify as transgender or non-binary have expressed that those who have lived experience may be best suited to work with patients with similar gender identities; these shared experiences likely serve as a source of comfort to patients who may not wish to be so transparent with cisgender clinicians [13, 14]. Many patients have expressed greater feelings of comfort working with gender minority clinicians [14]. Patients have attributed these feelings of comfort to gender minority clinicians having a higher likelihood of affirming a patient and greater gender-competency by way of personal experience [14].
In treatment spaces, both clinicians and patients called attention to the ineffectiveness of traditional ED treatment approaches and the detrimental effects they have on gender dysphoria for many gender minority patients. Patients from prior research felt like the use of body positive approaches, such as radical body acceptance, make them feel like they are “pushing themselves to be in their body” [13]. Clinicians in our study elaborated further, noting that their gender minority ED patients have a difficult time with exposure therapies and discussions around anatomies of cisgendered bodies. Gender minority patients have expressed discomfort with gendered care settings that exclude the body experiences of transgender and non-binary individuals [3, 13, 14]. The ability to use names and pronouns to involve gender in ED treatment by clinicians is necessary, but not sufficient. Patients report that clinicians blame their ED for causing gender dysphoria and others blame the dysphoria for causing their ED [14]. Most clinicians in this study recognized that dysphoria is not always the cause of ED for every gender minority patient; their ED may result from trauma, poor body image, or anxiety. Patients have asked for care needs to be tailored to the individual such that clinicians inquire about gender identity and how it is affecting the patient individually, not as a member of a homogenous group [14].
Strengths and limitations
Complementing research including patients, this study focused on the views of clinicians, who may have a fuller picture of care experiences across multiple patients of varying ages, races and ethnicities, experiences in medical and social transition, support systems, and financial circumstances. Individual interviews allowed for extensive discussion of provider perspectives and experiences. Their views elaborate on the narratives of patient perspectives in other studies; specifically, views on provider comfort and ability to treat gender minority individuals with body-centric mental health conditions, as well as the dominant disparities in this field of care. This study provided responses from nineteen clinicians of differing ages, race/ethnicities, clinical experiences, clinical settings, and geographic locations. Our sample was representative of provider demographics in the United States [30].
Validity in qualitative research can be impacted by reactivity, researcher bias, and selection bias. We sought to include clinicians from a wide range of belief systems and attitudes towards gender minority individuals. Yet, participants may become aware of researcher preconceptions on the subject matter and feel compelled to alter responses. We made efforts to reduce participant reactivity prior to the start of each interview by having the interviewer explicitly convey that all (1) perspectives, (2) beliefs, (3) maintained knowledge and (4) lack of knowledge on the subject matter were critical and equally important to researchers in this study.
The lead author (K.F.), who served as the interviewer and as a coder, had extensive prior knowledge of barriers and facilitators to care for gender minority individuals in U.S. mental health and primary care settings. Prior content area knowledge may have biased how codes were constructed and populated. To reduce the impact of researcher bias, we employed a second coder (E.M.) with limited prior knowledge of the subject matter and population. Both K.F. and E.M. identify as cisgender females, which may have limited the scope through which data could be understood, as neither had lived experience as a gender minority individual. Both coders made concerted efforts to question whether their own beliefs and assumptions were leading them to interpret findings a particular way.
Despite these strengths, study findings must be considered with limitations in mind. We recognize that we may have missed perspectives of clinicians with radically differing attitudes toward gender minority patients given the voluntary nature of participation. Future studies should aim to focus on the perspectives and views of (1) clinicians with complete lack of knowledge/inability to make assumptions about this population’s care experiences, (2) clinicians from cultural communities that have strong beliefs about traditional gender roles, (3) clinicians who are explicitly bigoted, and (4) clinicians who feel that gender minority individuals face no difficulties in life or ED care.
Implications
Clinicians demonstrated awareness of barriers to care for gender minority ED patients but expressed great uncertainty about methods of appropriate care delivery in this population. They expressed concern regarding lack of sufficient education about effective ED care for this population. Our findings highlight a need for understanding the provider level limitations in training and potential for system change in the care space that would address needs identified by gender minority patients and their advocates.
Conclusion
Clinicians in our study were aware of a plethora of barriers to care facing gender minority patients that impair their ability to receive effective treatment for eating disorders. Improvements to eating disorder treatment spaces, provider knowledge, and treatment approaches to better serve gender minority patients are warranted. Future research should expand upon extant studies that have identified weaknesses in the education of mental health clinicians, as well as clinicians’ ability and willingness to practice gender affirming and inclusive care.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available because we did not obtain explicit consent to share these data beyond the study team. As such, we are unable to share the qualitative data collected as part of this study.
References
Deloitte Access Economics. The social and economic cost of eating disorders in the United States of America: a report for the strategic training initiative for the prevention of eating disorders and the academy for eating disorders. 2020. Available at: https://www.hsph.harvard.edu/striped/report-economic-costs-of-eating-disorders/. Accessed 18 Jan 2023.
Diemer EW, Grant JD, Munn-Chernoff MA, Patterson DA, Duncan AE. Gender identity, sexual orientation, and eating-related pathology in a national sample of college students. J Adolesc Health. 2015;57(2):144–9.
Duffy ME, Henkel KE, Earnshaw VA. Transgender clients’ experiences of eating disorder treatment. J LGBT Issues Couns. 2016;10(3):136–49.
Diemer EW, White Hughto JM, Gordon AR, Guss C, Austin SB, Reisner SL. Beyond the binary: differences in eating disorder prevalence by gender identity in a transgender sample. Transgender Health. 2018;3(1):17–23.
Ferrucci KA, Lapane KL, Jesdale BM. Prevalence of diagnosed eating disorders in US transgender adults and youth in insurance claims. Int J Eat Disord. 2022;55(6):801–9. https://doi.org/10.1002/eat.23729.
Understanding transgender people: The basics. National Center for Transgender Equality. 2016. Available from: https://transequality.org/issues/resources/understanding-transgender-people-the-basics. Accessed 18 Jan 2023.
Seelman KL, Colón-Diaz MJ, LeCroix RH, Xavier-Brier M, Kattari L. Transgender noninclusive healthcare and delaying care because of fear: connections to general health and mental health among transgender adults. Transgender Health. 2017;2(1):17–28.
Roberts TK, Fantz CR. Barriers to quality health care for the transgender population. Clin Biochem. 2014;47(10–11):983–7.
Poteat T, German D, Kerrigan D. Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc Sci Med. 2013;1(84):22–9.
Shires DA, Jaffee K. Factors associated with health care discrimination experiences among a national sample of female-to-male transgender individuals. Health Soc Work. 2015;40(2):134–41.
Kattari SK, Bakko M, Hecht HK, Kattari L. Correlations between healthcare provider interactions and mental health among transgender and nonbinary adults. SSM-Popul Health. 2020;1(10): 100525.
Ferrucci KA, Walubita T, Beccia AL, Ding EY, Jesdale BM, Lapane KL, Streed CG. Health care satisfaction in relation to gender identity: behavioral risk factor surveillance survey, 20 states (2014–2018). Med Care. 2021;59(4):312–8.
Hartman-Munick SM, Silverstein S, Guss CE, Lopez E, Calzo JP, Gordon AR. Eating disorder screening and treatment experiences in transgender and gender diverse young adults. Eat Behav. 2021;1(41): 101517.
Cusack CE, Levenson NH, Galupo MP. “Anorexia wants to kill me, dysphoria wants me to live”: centering transgender and nonbinary experiences in eating disorder treatment. J LGBTQ Issues Couns. 2022;16(3):265–84.
American Psychological Association. Guidelines for psychological practice with transgender and gender nonconforming people. Am Psychol. 2015;70(9):832–64.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN, The REDCap Consortium. Building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
QSR International Pty Ltd. (2020) NVivo (released in March 2020). https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home. Accessed 18 Jan 2023.
Braun, V. & Clarke, V. (2012) Thematic analysis. In Cooper H., Camic P. M., Long D. L., Panter A. T., Rindskopf D., & Sher K. J. (Eds), APA handbook of research methods in psychology, Vol. 2: Research designs: Quantitative, qualitative, neuropsychological, and biological (pp. 57-71). Washington, DC: American Psychological Association. (20) (PDF) Thematic analysis.
Religious refusals in health care: A prescription for disaster [Internet]. Lgbtmap.org. 2018. Available from: https://www.lgbtmap.org/file/Healthcare-Religious-Exemptions.pdf. Accessed 18 Jan 2023.
Discrimination prevents LGBTQ people from accessing health care [Internet]. Center for American Progress. 2018. Available from: https://www.americanprogress.org/article/discrimination-prevents-lgbtq-people-accessing-health-care/. Accessed 18 Jan 2023.
Platt LF. The presenting concerns of transgender and gender nonconforming clients at university counseling centers. Couns Psychol. 2020;48(3):407–31. https://doi.org/10.1177/0011000019898680.
Duffy ME, Henkel KE, Joiner TE. Prevalence of self-injurious thoughts and behaviors in transgender individuals with eating disorders: a national study. J Adolesc Health. 2019;64(4):461–6.
Turban JL, King D, Carswell JM, Keuroghlian AS. Pubertal suppression for transgender youth and risk of suicidal ideation. Pediatrics. 2020;145(2): e20191725. https://doi.org/10.1542/peds.2019-1725
Pellicane MJ, Ciesla JA. Associations between minority stress, depression, and suicidal ideation and attempts in transgender and gender diverse (TGD) individuals: systematic review and meta-analysis. Clin Psychol Rev. 2022;91: 102113.
Elischberger HB, Glazier JJ, Hill ED, Verduzco-Baker L. Attitudes toward and beliefs about transgender youth: a cross-cultural comparison between the United States and India. Sex Roles. 2018;78(1):142–60.
Norton AT, Herek GM. Heterosexuals’ attitudes toward transgender people: findings from a national probability sample of US adults. Sex Roles. 2013;68(11–12):738–53. https://doi.org/10.1007/s11199-011-0110-6.
Johnson AH, Hill I, Beach-Ferrara J, Rogers BA, Bradford A. Common barriers to healthcare for transgender people in the US Southeast. Int J Transgender Health. 2020;21(1):70–8.
Anzani A, Morris ER, Galupo MP. From absence of microaggressions to seeing authentic gender: transgender clients’ experiences with microaffirmations in therapy. J LGBT Issues Couns. 2019;13(4):258–75. https://doi.org/10.1080/15538605.2019.1662359.
Mental health professional demographics and statistics [2022]: Number of Mental Health Professionals in the US [Internet]. Zippia.com. 2022. Available from: https://www.zippia.com/mental-health-professional-jobs/demographics/. Accessed 18 Jan 2023.
Geography Division of U.S. Department of Commerce Economics and Statistics Administration U.S. Census Bureau. Census Regions and Divisions of the United States [Internet]. Available from: https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed 18 Jan 2023.
Acknowledgements
Not applicable.
Funding
Ms. Ferrucci is a recipient of a pre-doctoral slot on an institutional NIH training Grant (TL1TR001454 to Dr. Lapane).
Author information
Authors and Affiliations
Contributions
KAF developed the study protocol and study interview guide, conducted provider interviews, as well as data cleaning, coding, interpretation, analysis, and writing and editing of the manuscript through multiple drafts. She also approved the final manuscript. EM assisted with data coding, interpretation, and analysis. She also approved the final manuscript. KLL provided feedback on the study protocol and study interview guide, provided insights on the interpretation of the analysis, provided funding, provided substantial critical review, edited multiple drafts of the manuscript, and approved the final manuscript. BMJ provided feedback on the interpretation of the study findings, input on the study guide, substantial critical review, and final approval of the final manuscript. CED provided feedback on the development of the study protocol, served as a guide for the implementation of the protocol, coding of the data, analysis, and interpretation. She also provided substantial critical review and edited multiple drafts of the manuscript and approved the final manuscript. All authors read and approved the final version of the manuscript.
Author’s information
At the time of the study, authors identified as:
KAF identifies as cisgender.
EM identifies as cisgender.
KLL identifies as cisgender.
BMJ identifies as cisgender.
CED identifies as cisgender.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants gave informed consent before participating in this study. Participants were compensated for their time with a $60 electronic cash card. Ethical approval was obtained from the Institutional Review Board at the University of Massachusetts Chan Medical School (Protocol H00023851).
Consent for publication
Not applicable.
Competing interests
None of the authors have competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix A.
Interview protocol.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ferrucci, K.A., McPhillips, E., Lapane, K.L. et al. Provider perceptions of barriers and facilitators to care in eating disorder treatment for transgender and gender diverse patients: a qualitative study. J Eat Disord 11, 36 (2023). https://doi.org/10.1186/s40337-023-00760-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40337-023-00760-9