Abstract
Background
An outbreak of Plasmodium malariae infection among forest goers in Sanya City of Hainan Island, China was reported in 2015. In response to this outbreak, an innovative three-layer strategy (TLS) targeted forest goers was adapted based on the 1-3-7 approach.
Main text
Key elements of TLS are: (i) The village with five malaria cases and adjacent villages were set as the first layer. All residents including forest goers were taken as the high-risk population (HRP). Active case detection (ACD) by blood smear microscopy and PCR was selected as the primary measure, and passive case detection (PCD) as complementary measure. One case was identified under TLS implementation. (ii) The township with cases (Gaofeng Town) and the nearby towns were chosen as the second layer. Only forest goers were screened by ACD, while PCD as a routine screening method. 7831 blood smears collected by ACD and PCD and tested with negative results. (iii) The city with cases (Sanya City) and others 12 counties/county-level cities were selected as the third layer. Malaria cases were monitored passively. A total of 77,555 blood slides were screened by PCD with zero positive sample. For each layer, the malaria vector mosquitoes were monitored using light traps, cattle-baited/human-bait traps. Anopheles minimus (dominant species), An. sinensis and An. dirus were captured. Vector control measures mainly include insecticide residual spraying and long-lasting insecticide nets. The capacity of clinicians, public health practitioners and laboratory technicians has been improved through training. During 2016‒2018, TLS and chemoprophylaxis were implemented in the same areas. In the first layer, all residents were monitored by ACD, and malaria chemoprophylaxis were distributed, 89.5% of forest goers were using chemoprophylaxis against malaria. The blood smears (3126 by ACD plus 1516 by PCD) were with zero positive results. Chemoprophylaxis and ACD were offered to forest goers once a year, and PCD in residents as a complementary measure in the second and third layer, 77.8% and 95.1% of forest goers received chemoprophylaxis. In each layer, vector surveillance and control of malaria and trainings for medical staff were still in place.
Conclusions
TLS was effective in blocking the outbreak by P. malariae among forest goers in Hainan in malaria elimination stage. However, whether it could prevent the malaria resurgence in the post-elimination phase needs to be further assessed.
Graphical Abstract

Similar content being viewed by others
Background
Historically, malaria has been one of the most important infectious diseases in China. Hainan and Yunnan provinces were the main malaria transmission areas in the People's Republic of China [1, 2]. Prior to 2010, indigenous cases of falciparum malaria and vivax malaria were frequently detected in Hainan. Hainan is geographically characterized by mountains, hills, plateaus and plains, and the tropical monsoon and marine climates jointly produce a generally warm temperature not only for cultivating tropical plants (coconuts, areca nut and rubber trees, and more) but also for the breeding of Anopheles dirus and An. minimus [3]. Malaria cases in Hainan Island were mainly distributed in patches in the southwestern region of the island, and malaria infection in forest goers cannot be ignored in Hainan. Sanya City was one of malaria endemic (Plasmodium vivax and P. falciparum) cities in Hainan Island, which is located at the southern tip of Hainan Island [4, 5]. An. sinensis was considered to be a major vector in Sanya, An. minimusis was captured in mountainous regions at times.
Forest goers referred to residents and migrants who sleeping overnight in the mountains for a living by picking and planting. Forest goers were among the high-risk populations in Hainan since the 1990s [6]. In 2002, forest goers (30.9%, 95/307) were more than twice as likely to be infected than non-forest-goer residents (15.2%) [7]. In 1991, an investigation in Nanqiao of Wanning City showed that the infection rate of malaria among forest goers (49.4%, 118/239) was significantly higher than that among non-forest-goers (8%, 11/138) [8]. The factors related to malaria infection rate in forest goers including the frequency of staying in the mountains, whether to take antimalarial chemoprophylaxis, the acceptance of antimalarial propaganda, and mosquito control measures [9–11]. Hainan Island has been engaged in malaria control and elimination in forest goers since the 1990s. Been supported by the Global Fund to Fight AIDS, Tuberculosis and Malaria, the strategy for the prevention and control of malaria in forest goers including mass drug administration (MDA) that focused on patients and the surrounding population (family members or co-workers), epidemiology investigations on patients, timely surveillance of vector dynamics, and vector control measures [such as insecticide residual spraying (IRS), insecticide-treated nets (ITNs) or long-lasting insecticidal nets (LLINs)], has been intensified since 2003 [12]. Seasonal anti-malaria measures were carried out uninterruptedly in spring and autumn annually in Hainan resulting in a decline of malaria incidence [13].
In 2010, Hainan joined the National Malaria Elimination Programme (NMEP). In Hainan Island there were eight Class I counties (endemic counties of P. falciparum) and ten Class II counties (endemic counties of P. vivax) [14]. Hainan Island officially launched malaria elimination in 2011. Subsequently, the 1-3-7 approach have been applied in the disposal of foci since 2012, which refer as following: case reporting within 1 day, case investigation within 3 days, and focus investigation and action within 7 days. Under the requirement of 1-3-7 approach, every reported case was confirmed by microscopy and PCR, and every focus file was collected and reported through the Parasitic Diseases Information Reporting Management System (PDIRMS). The last indigenous malaria case of P. vivax in Hainan was reported in Sanya in 2012.
From 2013, only imported malaria cases were reported in Hainan Island, and every imported malaria focus was classified and disposed according to the guidelines of the 1-3-7 approach. In 2015, there was an outbreak reported in Sanya, which was induced by indigenous cases infected by P. malariae among forest goers [15]. Based on the 1-3-7 approach, an innovative three-layer strategy (TLS) was designed and applied in the disposal of outbreak in 2015. From 2016 to 2018, the effectiveness of TLS was evaluated and mass drug administration by chemoprophylaxis were conducted in three layers. Hainan Province has achieved the goal of elimination malaria in 2019 and acquired the WHO certification of malaria elimination by field in 2021 [16]. This article summarizes the prevention and control measures of TLS strategy which administrated during the P. malariae malaria outbreak in 2015, and further outlines the lessons learned from the generation to evaluation from process.
An outbreak of P. malariae malaria occurred in Sanya City, Hainan in 2015
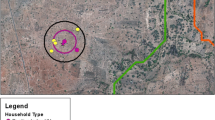
The first malaria case was reported on September 7, 2015. A total of six indigenous P. malariae cases were sequentially detected by ACD and PCD surveillance. All of them were male farmers aged from 19 to 40 years. This outbreak was reported from three villages (Baolong, Zhanan, Lixin) of Gaofeng town in Sanya City, respectively. Four cases in September, one case each in October and November, and no more cases were detected by PCD after that (Fig. 1).
Case 1 Male, 31 years, farmer, lived in Baolong village. On September 7, 2015, a male outpatient with chills, fever, headache, and limb weakness was diagnosed with P. malariae infection by blood smear microscopy in Sanya Hospital of Agricultural Reclamation (SYAR). The case subsequently confirmed by blood smear microscopy and PCR in Hainan Provincial Malaria Diagnosis Lab (HPMDL). Combined with the epidemiological history (without overnight in abroad and blood transfusion) and laboratory findings, he was determined as an indigenous case, and further classified as forest goer (Case 1). According to the information provided by Case 1, another three co-workers were confirmed as the new cases by blood smear microscopy and PCR (Case 2: Male, 19 years, farmer, lived in Lixin village; Case 3: Male, 27 years, farmer, lived in Lixin village; Case 4: Male, 31 years, farmer, lived in Lixin village). The four cases reported to stay overnight to collect bodhi fruit.
Case 5 Male, 40 years, farmer, lived in Zhanan village. On October 17, 2015, a male outpatient with chills, fever, headache, and limb weakness was diagnosed with P. malariae infection by blood smear microscopy in Nandao Township Hospital. The case subsequently confirmed by blood smear microscopy and PCR in HPMDL. Considering the epidemiological history (without overnight in abroad and blood transfusion) and laboratory findings, he was also determined as an indigenous case and classified as a forest goer.
Case 6 Male, 25 years, farmer, lived in Lixin village. On November 26, 2015, a symptomatic malaria carrier was found by PCR in HPMDL after TLS implemented. Subsequently, the case was confirmed by microscopy as P. malariae infection. However, Case 6 had no history of overnight sleeping in mountain, and classified as a victim in village.
All cases were sequentially transferred to SYAR and hospitalized to receive treatment with a standard regimen of oral chloroquine phosphate for 3 days (600 mg on 1st day, and then 300 mg once a day on the 2nd and 3rd days of therapy), plus primaquine diphosphate for 8 days (22.5 mg per day) to ensure therapeutic compliance.
Design of TLS and its application in the 2015 outbreak
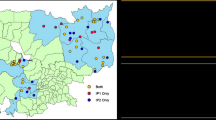
Based on the geographical distribution of five malaria cases (Case 1, 5 by PCD, and Case 2, 3, 4 by ACD), history of malaria joint defence and work urgency of elimination malaria, an innovative three-layer strategy (TLS, Fig. 2) was designed for expanded screening, PCD and ACD were optimally conducted as described in a previous study [17–19]. TLS was applied to prevent malaria transmission in the 2015 outbreak, more details showed as below, and the scope of three layers in details have showed in Additional files 1 and 3.
The skeleton map of three-layer strategy applied from 2015 to 2018 in Hainan. The red frame represents applied in the first layer only, but the blue frame represents various measures depend on different layers. IRS indoor residual spraying, TLS three-layer strategy, LLINs long lasting insecticide nets, JPCS joint prevention and control strategies, ACD active case detection, PCD passive case detection, MPD malaria parasite detection, VS vector surveillance, ACT attendees of capacity training, MC mass chemoprophylaxis
First layer
The villages with five malaria cases (Baolong, Zhanan and Lixin in Gaofeng Town, Sanya City) and adjacent villages, were regarded as the first layer. All residents who lived in the first layer were considered as the high-risk population (HRP). ACD screening was taken as primary measure in all residents by blood smear microscopy and SSU rRNA PCR assay [20], and PCD acted as complementary measure. During the implementation of ACD, a total of 1774 slides were screened by blood smear microscopy and PCR. Thirteen positive samples were found by PCR. Confirmed by experienced microscopists from HPMDL, only Case 6 were identified and determined as indigenous cases of P. malariae infection (Table 1).
Second layer
The Gaofeng Town and ten adjacent towns, which involved to Yucai in Sanya city, Daan and Zhizhong in Ledong County, Xiangshui, Maogan, Nanlin, Sandao, Xinzhen in Baoting County and Changhao in Wuzhishan city, were chosen as the second layer. ACD screening for forest goers were conducted in ten towns. While the PCD as routine screening method was reinforced in the health establishments and diagnostic assays were carried out on all febrile patients. A total of 7831 blood slides were screened by PCD and ACD, and negative results were obtained (Table 1).
Third layer
Sanya City and others 12 counties/county-level cities were selected as the third layer, refered to Ledong, Baoting, Wuzhishan, Dongfang, Lingshui, Qiongzhong, Baisha, Changjiang, Wanning, Qionghai, Tunchang and Danzhou. Febrile forest goers were screened. The forest goers who with fever at the time or had a history of fever within the past one month were defined as HRP, PCD was the primarily routine measure for screening. A total of 77,555 blood slides were screened by PCD, plus 17,795 blood slides by ACD. All tests were negative (Table 1).
Malaria vector surveillance and control measures, medical staff training
Vector surveillance and control were also implemented as described previously [21, 22]. Anopheline mosquitoes were collected using light traps, cattle-baited/human-bait traps in every month throughout the year of 2015 and for at least three consecutive nights in a month. (i) An. minimus and An. sinensis (dominant species) were trapped in the first layer. (ii) In the second layer, An. sinensis was the dominant species. An. minimus and An. dirus were captured only in Wuzhishan City. (iii) In the third layer, An. minimus was captured in 4 counties (Changjiang, Danzhou, Baisha and Tunchang); and An. dirus was captured only in Baisha County, while An. sinensis was captured in every county except for Qionghai. The dynamics of vectors indicated that there were highly effective malaria vectors around the foci in Sanya City, and mosquito surveillance was necessary.
Vector control measures mainly include IRS for An. sinensis and An. minimus, and the distribution LLINs for An. dirus and An. minimus. (i) IRS with deltamethrin was only implemented in every focus in the first layer. (ii) A total of 6783 LLINs were distributed and covered in three layers involving 11 counties or cites except for Tunchang County and Wanning City (Table 2). In addition, the capacity of clinicians, public health personnel and laboratory personnel enhanced with the regular training at different service levels (Table 3; Additional file 2).
Strengthened intervention by TLS from 2016 to 2018
From 2016 to 2018, TLS was applied to prevent malaria re-establishment, and mass chemoprophylaxis (MC) was conducted in the three layers. The scope of strengthened intervention by TLS was the same as its in 2015. The chemoprophylaxis of administration by piperaquine phosphate, and doses for children decreased by weight or age. Villagers, including forest goers, were required to sign informed consent forms before administration of the drugs.
First layer
From March to June, and September in every year from 2016 to 2018, adult residents in the first layer were given a total dose of 600 mg per month. Chemoprophylaxis and ACD were given and implemented on all residents, including forest goers. 89.5% of forest goers accepted chemoprophylaxis. A total of 4642 blood smears (3126 by ACD plus 1516 by PCD) were diagnosed by microscopy (Table 1). No positive slides were obtained.
Second layer and third layer
In the second and third layer, 77.8% of 5489 forest goers received chemoprophylaxis in the second layer. Chemoprophylaxis and ACD were used once a year seeking for forest goers in the field. In the third layer, 10,364 people were classified as forest goers, and 95.1% of them received chemoprophylaxis (Table 1).
Malaria vector surveillance and control measures, medical staff training
Vector surveillance and control were implemented as described previously. During 2016–2018, (i) An. minimus and An. sinensis were also captured in the first layer, and An. sinensis was still the dominant species. LLIN distribution was considered as an effective measure for vector control in Hainan from 2016 to 2018 because of the existence of An. dirus. (ii) In the second and third laryer, An. sinensis was the dominant species. An. minimus and An. dirus were usually captured in all years from 2016 to 2018. LLINs and training were also distributed in the two layers, except for Tunchang County and Wanning City in the third layer. Training on clinicians, public health personnel and laboratory personnel was persisted from 2016 to 2018 for maintaining alertness of the general health services to suspected malaria.
Discussion
Forest goers have the highest-risk of malaria infection in Hainan, mostly due to the abundant forest products and human behaviour. Abundant forest products, such as wood, honey, and wild animals, attracted the residents and mobile populations to work as forest goers [23]. The behaviour of staying overnight without using nets results in malaria infection. In the malaria control phase, an investigation in Nanqiao, Wanning City showed that overnight behaviour in mountains, the low usage rate of nets and the lack of malaria prevention knowledge were the key factors that affected the epidemics and control of malaria [24, 25]. In the elimination stage, the malaria outbreak in 2015 been mentioned above was caused by forest goers, and five of them had a history of staying overnight in mountains.
In the elimination phase outbreaks still happened in China, but was much less than control stage [26, 27]. The innovative TLS was adapted from 1-3-7 approach and first applied in the 2015 outbreak, and Case 6 was confirmed as an asymptomatic carrier. If 1-3-7 approach was implemented in this outbreak, only three cases associated with Case 1 and cases associated with Case 5 could be found. TLS enlarged the screening scope, improved the case detection ability and detected potential sources of infection, especially for the asymptomatic carriers and cases without treatment. In the outbreak of 2015, six cases were from different villages of the same township (Gaofeng). No malaria cases found outside Sanya City. It would alert us that different intervention measures need to tailor in different layers, which are like the prevention strategies against COVID-19 in China [28].
This outbreak was caused by P. malariae and more likely to be an imported-introduced case. The human-monkey mode of transmission is impossible because only 5 cases were found at this time. There have been no subsequent cases in the mountains, although forest goers have existed since the 1990s [6]. All of the malaria parasites in this outbreak were identified as P. malariae, not P. simium, which led to zoonosis in forest goers in Brazil[29]. Sanya is a tourist city with a large number of migrant people, including people from abroad and An. minimus, which is the main effective vector of malaria in Hainan, also exists in Sanya. The present study concluded that there was a high possibility of human-to-mosquito-to-human transmission in forest goers.
Which vector can transmit P. malariae remains a puzzle. There is no reports of P. malariae sporozoites being found in the salivary glands of vectors [30, 31]. In China, only Sanya has reported locally sequentially indigenous cases of P. malariae [32, 33]. Sporadic elderly cases of P. malaria, rather than young-to-middle aged groups in Sanya, have been reported in Guangdong and Shanghai, and no successive cases have been reported, although An. sinensis exists [30, 31]. At present, An. sinensis is widely distributed and the dominant species in China in recent years, while An. minimus is only found in Yunnan and Hainan. We presumed that An. minimus is more likely to transmit P. malaria in Sanya than An. sinensis. The transmission of P. malaria by An. minimus is currently a conjecture.
The cities or counties in the central part of Hainan Island, where An. dirus and An. minimus exists, are actively developing tourism resources for economic development [34], where the challenges in the control and prevention of imported malaria, forest goers remain as a high-risk group.
TLS was firstly applied in the 2015 outbreak, but there was no more similar scenarios in China can be used to explore scopes of the TLS for practicability after 2015. In addition, although there were at least two transmission chains in the perspective of epidemiological investigation, the relationship between two transmission chains is not certain and further investigation is urgently need.
Conclusions
The innovative TLS was effective in blocking the outbreak by P. malariae among forest goers in Hainan at malaria elimination stage. However, it still need to be tailored to apply in malaria control or elimination in similar settings for outbreak disposal. Moreover, whether it could prevent re-establishment by the potential malaria in the post-elimination phase needs to be further assessed.
Availability of data and materials
Not applicable.
Abbreviations
- CDC:
-
Center for Diseases Control and Prevention
- IRS:
-
Indoor residual spraying
- MDA:
-
Mass drug administration
- TLS:
-
Three-Layer Strategy
- LLINs:
-
Long-lasting insecticide nets
- FG:
-
Forest goer
- NMEP:
-
National Malaria Elimination Programme
- JPCS:
-
Joint prevention and control strategies
- ACD:
-
Active case detection
- PCD:
-
Passive case detection
- PDIRMS:
-
Parasitic Diseases Information Reporting Management System
- MPD:
-
Malaria parasite detection
- SYAR:
-
Sanya Hospital of Agricultural Reclamation
- HPMDL:
-
Hainan Provincial Malaria Diagnosis Lab
- HRP:
-
High-risk population
- ITNs:
-
Insecticide-treated nets
- ACT:
-
Attendees of capacity training
- MC:
-
Mass chemoprophylaxis
References
Xia ZG, Zhang L, Feng J, Li M, Feng XY, Tang LH, et al. Lessons from malaria control to elimination: case study in Hainan and Yunnan provinces. Adv Parasitol. 2014;86:47–79.
Yin JH, Zhou SS, Xia ZG, Wang RB, Qian YJ, Yang WZ, et al. Historical patterns of malaria transmission in China. Adv Parasitol. 2014;86:1–19.
Wei S, Lin S, Yang C. The 50-Year History of Health Service Development in Hainan Province from 1950 to 2000. Haikou: Nanfang Press; 2007. p. 297–311 (in Chinese).
Wang SQ. The seventy years of malaria from hyperendemicity to elimination in Hainan. Chin J Trop Med. 2019;198:707–18 (in Chinese).
Institute of Parasitic Diseases of Hainan Administrative Region. Malaria Control Research Data in Hainan Island 1950–1983. 1985, pp. 2–120 (in Chinese).
Lin M, Chen S, Deng J, Si Y, Zhong H, Huang M, et al. Investigation on malaria infection among residents of forest goers accommodation in high malaria area of Hainan Province. Hainan Med J. 1993;4:8–9 (in Chinese).
Jin Y, Wang S, Meng F, Zhuo K, Huade LC, Fu H, Huang Y. Investigation on malaria among residents and overnight people in Wuzhishan city. Chin J Trop Med. 2003;6:738–9 (in Chinese).
Lin M, Chen S, Deng J, Si Y, Zhong H, Chen W, Huang M, Chen X. Investigation on malaria infection among forest goers living in high malaria mountainous area of Hainan Province. Chin J Parasit Dis. 1994;1:71 (in Chinese).
He CH, Hu XM, Wang GZ, Zhao W, Sun DW, Li YC, et al. Eliminating Plasmodium falciparum in Hainan, China: a study on the use of behavioural change communication intervention to promote malaria prevention in mountain worker populations. Malar J. 2014;13:273.
Lan CX, Cai XZ, Zeng LH, Lin SG, Lan XH, Cai ZF, et al. Study on prevention and control of malaria infection among mountain population in Nanqiao area of Hainan Province. Hainan Med J. 1998;1:1 (in Chinese).
Lin C, Lin S, Fu Z, Ji W, Li H. Investigation and analysis of malaria control among forest goers population in malaria area of Ledong County. Chin J Trop Med. 2005;2:257–335 (in Chinese).
Lin M, Weng S. Progress on malaria control in 60 years in Nanqiao Pilot project and progress in the implementation of global fund projects against malaria. Chin J Trop Med. 2013;132:245–8 (in Chinese).
Wang SQ, Li YC, Zhang ZM, Wang GZ, Hu XM, Qualls WA, Xue RD. Prevention measures and socio-economic development result in a decrease in malaria in Hainan. China Malar J. 2014;13:362.
Fan N, Zeng W. Malaria elimination action plan launched in Hainan. Hainan Daily, 2010. http://hnrb.hinews.cn/html/2010-03/20/content_202514.htm. Accessed 20 Mar 2010 (in Chinese).
Lin C, Chen Z, Wang S, Luo P, Wu D, Zheng A, Wei J. Analysis and management of a rare malaria case of P. malariae in sanya, Hainan Province. Chin J Trop Med. 2016;165:481–4 (in Chinese).
WHO. From 30 million cases to zero: China is certified malaria-free by WHO. https://www.who.int/news/item/30-06-2021-from-30-million-cases-to-zero-china-is-certified-malaria-free-by-who. Accessed 30 Jun 2021.
Tseroni M, Georgitsou M, Baka A, Pinaka O, Pervanidou D, Tsironi M, et al. The importance of an active case detection (ACD) programme for malaria among migrants from malaria endemic countries: the greek experience in a receptive and vulnerable area. Int J Environ Res Public Health. 2020;17:4080.
Francis F, Ishengoma DS, Mmbando BP, Rutta ASM, Malecela MN, Mayala B, et al. Deployment and use of mobile phone technology for real-time reporting of fever cases and malaria treatment failure in areas of declining malaria transmission in Muheza district north-eastern Tanzania. Malar J. 2017;16:308.
Branch O, Casapia WM, Gamboa DV, Hernandez JN, Alava FF, Roncal N, et al. Clustered local transmission and asymptomatic Plasmodium falciparum and Plasmodium vivax malaria infections in a recently emerged, hypoendemic Peruvian Amazon community. Malar J. 2005;4:27.
Li YC, Wang GZ, Sun DW, Meng F, Lin SG, Hu XM, et al. A case of Plasmodium ovale wallikeri infection in a Chinese worker returning from West Africa. Korean J Parasitol. 2013;5:557–62.
Wang Y, Zhong D, Cui L, Lee MC, Yang Z, Yan G, Zhou G. Population dynamics and community structure of Anopheles mosquitoes along the China–Myanmar border. Parasit Vectors. 2015;8:445.
Tangena J-AA, Thammavong P, Hiscox A, Lindsay SW, Brey PT. The human-baited double net trap: an alternative to human landing catches for collecting outdoor biting mosquitoes in Lao PDR. PLoS One. 2015;10:e0138735.
Wu K, Chen W, Tang L, Deng D, Lin M, Cai X, et al. Study on the characteristics of lodging behavior and its relationship with malaria infection among Li and Miao ethnic groups in high malaria mountainous area of Hainan Province. Chin J Parasitol Parasit Dis. 1995;4:17–21 (in Chinese).
Wu K, Tang L, Chen W, Liu D, Lin M, Gu Z, et al. Epidemiological characteristics of malaria in mountainous areas of Hainan. Chin J Parasitol Parasit Dis. 1998;4:3–7 (in Chinese).
Chen W, Shi P, Wu K, Deng D, Tang L, Cai X, et al. Impact of socio-economic factors on malaria prevalence in Hainan province by unconditional logistic multiple regression analysis. Chin J Parasitol Parasit Dis. 1995;3:161–4 (in Chinese).
Sun YW, Yu DM, Chen J, Li X, Wang B, Wang ZJ, et al. Analysis of two cases of Plasmodium vivax malaria in Dandong city, Liaoning province. Chin J Public Health. 2017;332:314–6 (in Chinese).
Feng XY, Shi WQ, Li JL, Chen JS, Li ZX, Xia ZG. Investigation of malaria vectors in Longhui county, Hunan province. Chin J Pathog Biol. 2020;1503:317–21 (in Chinese).
Lei ZL. What is the difference between containment area, control area or prevention area. 2021. https://xw.qq.com/cmsid/20211023A04QQX00?f=newdc. Accessed 16 Sep 2021 (in Chinese).
Brasil P, Zalis MG, de Pina-Costa A, Siqueira AM, Júnior CB, Silva S, et al. Outbreak of human malaria caused by Plasmodium simium in the Atlantic forest in Rio de Janeiro: a molecular epidemiological investigation. Lancet Glob Health. 2017;510:e1038–46.
Pan B, Ruan CW, Pei FQ, Lin GQ, Cen YZ, Zhang ZX. Diagnosis and treatment analysis of a case of malariae malaria with long latent period. South China J Prev Med. 2016;421:64–7 (in Chinese).
Cao S, Wang L, Zhu M, Cai L. Traceability investigation of a P. malariae case in Shanghai. Chin J Parasitol Parasit Dis. 2016;342:150–3 (in Chinese).
Feng J, Zhang L, Zhang SS, Xia ZG, Zhou SS. Analysis of malaria epidemic in China from 2005 to 2015. Chin J Trop Med. 2017;17:325–35 (in Chinese).
Zhang L, Feng J, Zhang SS, Xia ZG, Zhou SS. Epidemiological analysis of malaria in China in 2015. Chin J Parasitol Parasit Dis. 2016;34:477–81 (in Chinese).
Shi X. Measurement and evaluation of tourism ecological coupling degree under the construction of Hainan Free Trade Port. Chin J Commer. 2021;20:40–2 (in Chinese).
Acknowledgements
We acknowledge the contributions of all the officials, professionals and people involved in controlling this outbreak. Moreover, Xiao-Nong Zhou and Jianhai Yin guided this manuscript.
Funding
This work was supported by Bill & Melinda Gates Foundation: No. INV-018913, Hainan Provincial Basic and Applied Basic Research Program (Natural Science Foundation) for High-level Talents in 2019 (2019RC394) and Natural Science Foundation of China (No. 81460520).
Author information
Authors and Affiliations
Contributions
YCL conceived the paper, analysed results, and wrote the first version of the manuscript. WZ, FM, XMH, RQC, YJH, WZH, HZX, RSY, SLH, JZ, XDW, GYW, YL, HSL, ZCZ, JW, GSW supported data collection. GZW, BY, YC supported interpretation of results and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
This study was approved by the Hainan Provincial Health and Family Planning Commission (ID: 201536, 201603, 201714, 201711). Informed consent was signed by the participants who taking piperaquine. The researchers informed medication procedure, adverse reactions, and the purpose of the medication.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Supplementary Information
Additional file 1
: The areas of three layers in details as a part of TLS in 2015
Additional file 2
: 1. Vector surveillance and control from 2015 to 2018 when implementation of the three-layer strategy. 2. Training in details in 13 counties or cities for response and intervention from 2015 to 2018
Additional file 3
: TLS applied in the disposal of the outbreak in 2015, and in strengthening epidemic measures from 2016 to 2018, respectively. (A) Bodhi fruit; (B) ACD of malaria in 2015; and (C) MDA to prevent malaria from 2016 to 2018
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Y., Huang, Y., Chen, R. et al. An innovative three-layer strategy in response to a quartan malaria outbreak among forest goers in Hainan Island, China: a retrospective study. Infect Dis Poverty 11, 97 (2022). https://doi.org/10.1186/s40249-022-01015-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-022-01015-6