Abstract
Background
The current mainstay for control/elimination of onchocerciasis and soil-transmitted helminthiasis (STH) relies on ivermectin- and mebendazole/albendazole-based preventive chemotherapies. However, children under five years of age have been excluded in both research activities and control programs, because they were believed to have insignificant infection rates. There is therefore a need for up-to-date knowledge on the prevalence and intensity of STH and onchocerciasis infections in this age group. This study aimed at assessing the rates and intensities of onchocerciasis and STH infections in children under five years of age who are excluded from ivermectin- or mebendazole/albendazole-based preventive chemotherapies.
Methods
A series of cross-sectional surveys was conducted in four Health Districts in the Centre and Littoral Regions of Cameroon between 2018 and 2019. All subjects aged 2 to 4 years, were screened for prevalence (or infection rate) and intensity [number of eggs per gram of stool (epg) or number of microfilariae per skin snip (mf/ss)] of STH and onchocerciasis infections respectively using the Kato-Katz and skin snip methodologies. Chi-square and the non-parametric tests (Mann Whitney and Kruskal Wallis) were used to compare infection rates and intensities of infections between Health Districts and genders, respectively.
Results
A total of 421 children were enrolled in this study. The overall prevalence of onchocerciasis was 6.6% [95% confidence interval (CI): 4.3‒9.9], ranging from 3.6% (in the Ntui Health District) to 12.2% (in the Bafia Health District). The intensity of infection ranged from 0.5 to 46 microfilariae per skin snip [median: 5; interquartile range (IQR): 2.25‒8.5]. The overall prevalence of STH was 9.6% (95% CI: 6.5‒13.9), with a high infection rate (29.6%) in the Akonolinga Health District. Two STH species (Ascaris lumbricoides and Trichuris trichiura) were found among infected individuals. The median intensities of STH infections were 1,992 epg (IQR: 210‒28,704) and 96 epg (IQR: 48‒168) for A. lumbricoides and T. trichiura, respectively.
Conclusions
This study reveals that children < 5 years of age are highly infected with STH and onchocerciasis, and could contribute to the spread of these diseases, perpetuating a vicious circle of transmission and hampering elimination efforts. These findings reveal the urgent need to provide (or scale) treatments (likely pediatric formulations) to these preschool-aged children, especially in areas of high transmission, to accelerate efforts to reach WHO 2030 target.
Graphical Abstract

Similar content being viewed by others
Background
In 2001, the World Health Organization (WHO) recommended annual or bi-annual administration of a single dose albendazole (ALB, 400 mg) or mebendazole (MEB, 500 mg) to STH high-risk populations. These include preschool-age children (pre-SAC), school-age children (SAC), women of childbearing age and adults who are particularly exposed to the infection in endemic areas, such as tea pickers [1]. Due to logistical constraints, only SACs were treated regularly [2], while the other groups being neglected. As the need for preventive chemotherapy (PC) for other at-risk groups became increasingly clear [1, 3], WHO reformulated guidelines and recommended new targets for STH control, including 100% of endemic countries achieving 75% coverage in the pre-SAC and SAC. Despite this new recommendation, pre-SAC phase lagged behind, because the infection rate in this age group was considered insignificant [4, 5]. Consequently, only 15% of endemic countries reported consistently administering PC to pre-SAC for more than 5 years [6], so additional epidemiological evidence of STH in these children is urgently needed to intensify control measures in this age group.
The control/elimination strategy for onchocerciasis mainly relies on ivermectin (IVM)-based PC, the so-called community-directed treatment with ivermectin (CDTI). Although IVM is distributed based on heigh or weight of individuals aged ≥ 5 years in endemic communities [7, 8]; children less than 5 years are systematically excluded from PC [9, 10], probably for practical reasons and because of the lack of epidemiological evidence in this age group. Indeed, early investigations indicated that children under five are very unlikely to harbor Onchocerca volvulus microfilariae [11, 12], and no safety and efficacy trials had been conducted for this age class [13]. As a consequence, children who are exposed to a similar risk of infection—and probably even infected—as their older peers (but not receiving PC), have an increased risk of developing nodding syndrome or onchocerciasis-associated epilepsy (OAE) as they grow older, as previously demonstrated [14,15,16,17]. Importantly, these untreated children might also constitute a human reservoir for the parasite, preventing the prospect of elimination through continued transmission. Therefore, there is a need to accumulate more evidence and update epidemiological data on onchocerciasis in children under five years of age for subsequent actions.
The WHO 2030 targets for onchocerciasis and soil-transmitted helminthiases (STH) are to interrupt the transmission in 31% of endemic countries, and to achieve and/or maintain the elimination as public health concern [6, 18, 19]. However, to reach these ambitious goals, control/elimination strategies for the helminthic diseases need to be extended to all age groups, based on appropriate evidence. We therefore conducted a series of cross-sectional studies in areas of varying endemicity for STH and onchocerciasis in Cameroon to determine the rates and intensities of onchocerciasis and STH infections in children under five years of age who are excluded from IVM- or MEB/ALB- based PC.
Methods
Study sites and population
This was a multicentric observational study conducted between 2018 and 2019 in four Health Districts (Akonolinga, Bafia, and Ntui in the Center Region, and Yabassi in the Littoral Region) in Cameroon, with varying levels of endemicity for onchocerciasis and STH.
The Akonolinga Health District, located in the Nyong-et-Mfoumou Division (Centre Region, Cameroon), is a forest zone with a plateau landscape. Its climate is of equatorial type with four seasons [20]. Estimated at 83,464 inhabitants [21], the populations are typically rural and their main activities are farming (coffee, cacao and food crops) and fishing. The area is highly endemic to STH and loiasis [22, 23], but hypo-endemic to onchocerciasis [24]. Therefore, IVM-based MDA is not implemented in the area, while school-based deworming with MEB has been introduced and implemented in the area since 2007.
The Bafia Health District, situated in the Mbam-et-Inoubou Division (Central Region, Cameroon), is a forest-savanna transition zone. The area is irrigated by many fast-flowing rivers (Sanaga, Mbam, Noun and their tributaries). The main activities of its 161,400 inhabitants are farming, fishing and sand mining [21]. Onchocerciasis is meso-endemic in the area, despite mass distribution of IVM ongoing for more than two decades [25].
The Ntui Health District is located in the Mbam-et-Kim Division (Centre Region, Cameroon), where a humid equatorial climate with four seasons prevails. In this forest-savanna transition zone, most of the tributaries of Mbam and Sanaga are surrounded by forest galleries. Due to its endemicity to onchocerciasis, CDTI was initiated in this area in 1999‒2000. In the Ntui Health District, a baseline survey conducted in the Mbangassina (one of the 11 Health Areas of the Ntui Health District), revealed high prevalence of STH (51% for Ascaris lumbricoides and 64% for Trichuris trichiura) (Kamgno et al. unpublished data).
Yabassi Health District in Nkam Division (Littoral Region, Cameroon) is a densely forested area with an equatorial climate with two seasons. The 652,683 inhabitants are mostly farmers. The area was known to be highly endemic for onchocerciasis and lymphatic filariasis, and community-based MDA with ALB and IVM has been implemented since 2000. This area was also known to be highly endemic to STH [26, 27]. School-based deworming with MEB is ongoing in the area since 2007 and a recent survey showed that STH transmission was almost interrupted, likely due to the combined effect of IVM- and MEB-based MDA [28].
Based on the availability of baseline data in the targeted settings, the Mbangassina Health Area (Ntui Health District) was surveyed for both STH and onchocerciasis, while Akonolinga Health District was screened only for STH, and Bafia and Yabassi Health Districts surveyed only for onchocerciasis.
Study design
A series of four cross-sectional studies were undertaken to determine the magnitude (prevalence and intensity) of STH and onchocerciasis infections in children aged 2‒4 years. Although the enrollees were not expected to be involved in PC (either with ALB, MEB or IVM), the surveys took place approximately 11 months after last MDA campaign (either with IVM or MEB/ALB), to limit the potential impact of the latest treatments on the transmission of targeted infections. All individuals aged 2 to 4 years and whose parents consented for their participation were included in the study; their socio-demographic data (including the age, sex village of residence, number of years spent in the village of residence, or other villages where the participant lived before arriving in the village …) were recorded and they underwent parasitological (skin snip and Kato-Katz) and clinical examinations.
Sample collection and processing
A 60 ml plastic screw-cap vial was given to all the eligible participants for stool collection. Stool samples were examined for the presence of eggs using the standard Kato-Katz technique [29]. Briefly, a single thick smear using a 41.7 mg template was prepared for each individual. The preparation was examined by qualified laboratory technicians, within one hour after slides’ preparation to ensure that all STH species present in the preparation should be identified. All STH eggs found on the slides were identified and counted, and the results expressed as eggs per gram of stool (epg). Based on the WHO criteria, STH infections were classified as light, moderate and heavy, for different parasite species, as follow: A. lumbricoides (light: 0–4,999 epg; moderate: 5000–49,999 epg; and heavy: ≥ 50,000 epg) and T. trichiura (light: 0–999 epg; moderate: 1000–9,999 epg; and heavy: ≥ 10,000 epg) [30].
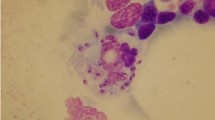
Onchocerciasis was diagnosed by the skin snip technique. Indeed, two skin biopsies were taken from each posterior iliac crest using a 2 mm corneoscleral punch (Holth-type). The skin samples were immediately placed separately into wells of microtiter plates containing a sterile normal saline solution and incubated at room temperature [31]. The skin biopsies were examined microscopically for O. volvulus microfilariae (mf). In brief, after 24 h incubation at room temperature, the fluid from each well was examined under low magnification (× 40) by trained laboratory technicians. For positive results, the microfilariae were counted and individual microfilarial densities were expressed as the arithmetic mean number of microfilariae in the two skin snips.
Statistical analyses
Microsoft Office Access was used to record field and laboratory data. The database was then exported to Microsoft Office Excel (Microsoft Co., Redmond, Washington, USA), formatted and cleaned before being definitively archived in Excel format. Statistical analyses were performed using GraphPad prism version 6 (GraphPad Software Inc., San Diego, CA, USA). Prevalence or infection rates were expressed as percentages with 95% confidence interval (CI) while intensities of infections were expressed as median of mf or eggs/larvae positive counts with interquartile range (IQR). Chi-square test was used to compare prevalence or infection rates between Health Districts and genders. The non-parametric Kruskal Wallis and Mann Whitney tests were used to compare intensities of infections between the different Health Districts and genders, respectively. The threshold for significance was set at 5% for all analyses.
Results
Socio-demographic characteristics of the study population
A total of 421 children aged 2 to 4 years (Median: 3; IQR: 2–4) were enrolled in the four Health Districts visited during this study. Most of the participants were originating from the Ntui Health District (40.1%); the sex ratio (M/F) was 0.99, with 50.4% of the participants being females (Table 1).
Prevalence and intensity of O. volvulus infection among children < 5 years
A total of 318 children were examined for onchocerciasis in the Bafia, Ntui and Yabassi Health Districts. The prevalence of O. volvulus microfilaridermia was 6.6% (95% CI: 4.3–9.9). The Bafia Health District exhibited the highest infection rate (12.2%; 95% CI: 6.8–21.2) compared to the other Health Districts (χ2: 6.79; df: 2; P-value: 0.0335) (Table 2). The infection rate was also similar between males (8.7%; 95% CI 5.1–14.1) and females (4.8%; 95% CI: 2.0–9.1) (χ2: 2.20; df: 1; P-value: 0.1362) (Table 2).
Onchocerciasis intensity of infection for microfilaremic individuals ranged from 0.5 to 46 microfilariae per skin snip (Median: 5; IQR: 2.25–8.75 mf/ss). The intensity of infection was similar between girls and boys (Mann Whitney U: 45.5; P-value: 0.8122) (Fig. 1A). However, high heterogeneity was observed in the intensity of infection between Health Districts, the mean mf counts being significantly different between the Health Districts (χ2: 9.327; P-value: 0.0045) (Fig. 1B). The Dunn’s Multiple comparison revealed that the intensity of infection was significantly higher in Bafia and Ntui Health District, compared to the Yabassi Health District (mean rank difference: − 8.633) (Fig. 1B).
Prevalence and intensity of STH infection among children < 5 years
A total of 250 children successfully provided stool samples in the two Health Districts (Akonolinga and Ntui) surveyed for STH, of whom 24 (9.6%; 95% CI: 6.5–13.9) harbored at least one of the two main STH species (A. lumbricoides and T. trichiura) (Table 3). Infected children were found only in the Akonolinga Health District; the infection rate was 29.6% (95% CI: 28.8–40.4). A. lumbricoides was the most prevalent STH species (7.6%) among infected children, and one (0.4%) child was co-infected by both STH species. No significant difference was found in the infection rate between girls (10.2%) and boys (8.9%) (χ2: 0.12; df: 1; P-value: 0.729).
The intensity of infection ranged from light to heavy infection for A. lumbricoides (192 to 50,088 epg; Median: 1,992; IQR: 210–28,704), and was light for all the infected children for T. trichiura (24 to 1,512 epg; Median: 96; IQR: 48–168). Likewise infection rate, the intensity of infection was similar between girls and boys, both for A. lumbricoides (Mann Whitney U: 1; P-value: 0.2667) (Fig. 2A) and T. trichiura (Mann Whitney U: 32; P-value: 0.3012) (Fig. 2B).
Discussion
The WHO 2030 target for onchocerciasis and STH are to interrupt the transmission in 31% of the endemic countries, and achieve and maintain the elimination as public health concern, respectively [6, 18, 19]. However, the strategies used to control/eliminate those infections generally left behind individuals aged < 5 years. To bring more evidence supporting the need of initiating or intensifying intervention in this age class, we are reporting the magnitude of onchocerciasis and STH in children aged 2–4 years in different settings with different levels of endemicity to both diseases in Cameroon, and discuss their impacts in the prospect of elimination.
In this study, although the global proportion of STH was quite low (9.6%), the proportion of infected children was 29.6% (95% CI: 28.8–40.4) in the Akonolinga Health District, with the intensity of infection ranging from light to heavy. These high rates and intensities of STH infection among pre-SAC in this area might be explained by the fact that very high infection rates have been previously found both among school-aged children and adults in the Akonolinga Health District [22], and as such the likelihood to have younger individuals (pre-SAC) infected as well is high. Additionally, the ongoing deworming activity in the area follows the school-based model, leaving somehow behind or neglected pre-SAC who are not typically reached during school-based deworming campaigns. As a consequence, those children are at high risk of developing STH-related morbidity such as malnutrition and anemia, diminished physical fitness, growth retardation and delayed intellectual development [32, 33] since the intensity of infection was found to be light or heavy for A. lumbricoides. In addition, if left untreated, those children might serve as parasites reservoir and source of re-infestation for their older counterparts who are receiving PC at schools, thus maintaining a vicious cycle of transmission and hindrance to elimination efforts. This finding adds to growing evidence that school-based deworming alone is not sufficient to interrupt STH transmission as previously demonstrated [22, 28]. This raise the need of implementation or intensification of control approaches, such as the deworming through Child Health Days (recommended by the WHO) [34], Child and Maternal Health and Nutrition Action Week (SASNIM) as it is the case in Cameroon, or the reconsideration of community-based model for an optimal coordination of STH control, at least in areas of high transmission [35, 36].
The rates and intensities of onchocerciasis infection recorded in this study are almost similar to figures recorded among individuals aged ≥ 5 years old [25, 37], suggesting that in these highly endemic areas children under 5 years have almost similar risk of infection as their older counterparts. Besides this, the prevalence of onchocerciasis was significantly lower in Mbangassina (Ntui Health District) compared to Bafia and Yabassi Health Districts. This is not surprising since the three areas exhibit different patterns of onchocerciasis transmission. Indeed, Bafia and Yabassi Health Districts are meso-endemic foci where the transmission is still unexpectedly high despite more than 20 years of MDA [25], while in the Ntui Health District, onchocerciasis prevalence has dropped from 26.3% in 2009 to 8.3% in 2020 [38, 39]. This suggests that the risk of onchocerciasis infection in children < 5 years is positively associated with the level of endemicity of onchocerciasis, and further suggest that these heavily infected children might contribute to the transmission, thus disrupting onchocerciasis elimination prospects due to continued transmission. Also, this might be one of the factors underlying the persistence of onchocerciasis in those communities, despite more than 20 years of control efforts [25]. In addition, the high intensity of infection found in these children is of great concern at a public health perspective since such high burden of O. volvulus parasites might lead to serious health and socio-economic consequences such as OAE and nodding syndrome [15,16,17]. Indeed, it was demonstrated that early childhood infection with O. volvulus is associated with an increased risk of developing either seizures or epilepsy, with a strong dose-response relationship with the intensity of infection [14]. In fact, the prepatent period of O. volvulus infection is estimated to 7 to 12 months [40]. If children are exposed to infection quite early in their life, they will already have fully reproductive parasites at 4 years; this might further explain the high prevalence of onchocerciasis associated epilepsy in the Mbam valley [15, 16, 41]. This quite high prevalence and intensity of onchocerciasis infection among children aged 2 to 4 years, and the potential health and socio-economic consequences, raise the need of intervention for this age class, and it appears worth to conduct trials investigating the IVM dose that can safely clear O. volvulus mf in this age class, or alternatively to develop a pediatric formulation of IVM.
The main limitation of this study is the small sample size at the level of Health Districts (71‒169 children aged less than 5 years of age), consecutive to the difficulty of collecting skin biopsies (painful procedure) or stool samples from this specific age class. Although this small sample size may reduce the power of statistical tests, the objective of this study was to investigate to what extent children excluded from preventive chemotherapies were infected with onchocerciasis and STH in order to prompt decisions for the control of these parasitic infections among these age groups. Further investigations with larger sample size and broader breadth of coverage across targeted age class (including children aged less than 2 years old) might be useful to better estimate the burden of onchocerciasis and STH among children excluded from IVM- or MEB/ALB- based PC, though the present study already provide important enough data for decision making.
Conclusions
Relatively high rates and intensities of STH and onchocerciasis infections have been found among children aged 2 to 4 years old in this study. Beside important health and socio-economic consequences that can arise as these children are infected quite early but left untreated, this high endemicity may also constitute a serious obstacle to the prospects of elimination of those diseases. There is therefore an urgent need to reconsider the role played by these children in the control of onchocerciasis and STH, so as to indeed end the neglect and move towards the sustainable development goals leaving no one behind.
Availability of data and materials
The data supporting the conclusions of this article are included within the article. Raw data can be obtained from corresponding authors upon reasonable request.
Change history
06 June 2022
A Correction to this paper has been published: https://doi.org/10.1186/s40249-022-00984-y
Abbreviations
- ALB:
-
Albendazole
- CDTI:
-
Community-directed treatment with IVM
- CI :
-
Confidence interval
- HD:
-
Health Districts
- IQR:
-
Interquartile range
- IVM:
-
Ivermectin
- MDA:
-
Mass drug administration
- MEB:
-
Mebendazole
- mf:
-
Microfilariae
- OAE:
-
Onchocerciasis-associated epilepsy
- PC:
-
Preventive chemotherapy
- Pre-SAC:
-
Pre-school-aged children
- SAC:
-
School-aged children
- SASNIM:
-
Semaine d'Actions de Santé et de Nutrition Infantile et Maternelle
- ss:
-
Skin snip
- STH:
-
Soil-transmitted helminthiases
- WHO:
-
World Health Organization
References
World Health Organization. Soil-transmitted helminthiases: eliminating as public health problem soil-transmitted helminthiases in children: progress report 2001–2010 and strategic plan 2011–2020. Geneva: World Health Organization; 2012.
World Health Organization. Schistosomiasis and soil-transmitted helminth infections. Fifty-fourth World Health Assembly, Resolutions and decisions WHA54.19. 2001. https://www.who.int/neglected_diseases/mediacentre/WHA_54.19_Eng.pdf. accessed 02 March 2022.
Gabrielli AF, Montresor A, Chitsulo L, Engels D, Savioli L. Preventive chemotherapy in human helminthiasis: theoretical and operational aspects. Trans R Soc Trop Med Hyg. 2011;105:683–93.
Garg R, Lee LA, Beach MJ, Wamae CN, Ramakrishnan U, Deming MS. Evaluation of the Integrated Management of Childhood Illness guidelines for treatment of intestinal helminth infections among sick children aged 2–4 years in western Kenya. Trans R Soc Trop Med Hyg. 2002;96:543–8.
Awasthi S, Pande VK. Six-monthly de-worming in infants to study effects on growth. Indian J Pediatr. 2001;68:823–7.
World Health Organization. 2030 targets for soil-transmitted helminthiases control programmes. Geneva: World Health Organization; 2020.
Tekle AH, Zouré HGM, Noma M, Boussinesq M, Coffeng LE, Stolk WA, et al. Progress towards onchocerciasis elimination in the participating countries of the African Programme for Onchocerciasis Control: epidemiological evaluation results. Infect Dis Poverty. 2016;5:66–76.
World Health Organization. Conceptual and operational framework of onchocerciasis elimination with ivermectin treatment. Geneva: African Programme for Onchocerciasis Control; 2010.
González Canga A, Sahagún Prieto AM, Diez Liébana MJ, Fernández Martínez N, Sierra Vega M, García Vieitez JJ. The pharmacokinetics and interactions of ivermectin in humans: a mini-review. AAPS J. 2008;10:42–6.
Wilkins A, Steer A, Cranswick N, Gwee A. Is it safe to use ivermectin in children less than five years of age and weighing less than 15 kg? Arch Dis Child. 2018;103:514–9.
Nelson GS. Human onchocerciasis: notes on the history, the parasite and the life cycle. Ann Trop Med Parasitol. 1991;85:83–95.
Filipe JAN, Boussinesq M, Renz A, Collins RC, Vivas-Martinez S, Grillet ME, et al. Human infection patterns and heterogeneous exposure in river blindness. Proc Natl Acad Sci USA. 2005;102:15265.
Jittamala P, Monteiro W, Smit MR, Pedrique B, Specht S, Chaccour CJ, et al. A systematic review and an individual patient data meta-analysis of ivermectin use in children weighing less than fifteen kilograms: Is it time to reconsider the current contraindication? PLoS Negl Trop Dis. 2021;15: e0009144.
Chesnais CB, Nana-Djeunga HC, Njamnshi AK, Lenou-Nanga CG, Boullé C, Bissek A-CZ-K, et al. The temporal relationship between onchocerciasis and epilepsy: a population-based cohort study. Lancet Infect Dis. 2018;18:1278–86.
Colebunders R, Nelson Siewe FJ, Hotterbeekx A. Onchocerciasis-associated epilepsy, an additional reason for strengthening onchocerciasis elimination programs. Trends Parasitol. 2018;34:208–16.
Pion SDS, Kaiser C, Boutros-Toni F, Cournil A, Taylor MM, Meredith SEO, et al. Epilepsy in onchocerciasis endemic areas: systematic review and meta-analysis of population-based surveys. PLoS Negl Trop Dis. 2009;3: e461.
Idro R, Opar B, Wamala J, Abbo C, Onzivua S, Mwaka DA, et al. Is nodding syndrome an Onchocerca volvulus-induced neuroinflammatory disorder? Uganda’s story of research in understanding the disease. Int J Infect Dis. 2016;45:112–7.
World Health Organization. Ending the neglect to attain the sustainable developmentgoals: a road map for neglected tropical diseases 2021–2030. Geneva: World Health Organization; 2021.
The World Health Organization 2030 goals for onchocerciasis: Insights and perspectives from mathematical modelling. Gates Open Res. 2019;3.
Okalla R. Le district de santé d’Akonolinga. Bulletin de l’APAD. 2001. http://journals.openedition.org/apad/33. accessed 02 Mar 2022.
World Health Organization. Health population denominators 2017-Cameroon. Geneva: World Health Organization; 2017.
Bopda J, Nana-Djeunga H, Tenaguem J, Kamtchum-Tatuene J, Gounoue-Kamkumo R, Assob-Nguedia C, et al. Prevalence and intensity of human soil transmitted helminth infections in the Akonolinga Health District (Centre Region, Cameroon): are adult hosts contributing in the persistence of the transmission? Parasite Epidemiol Control. 2016;1:199–204.
Zouré HG, Wanji S, Noma M, Amazigo UV, Diggle PJ, Tekle AH, Remme JH. The geographic distribution of Loa loa in Africa: results of large-scale implementation of the Rapid Assessment Procedure for Loiasis (RAPLOA). PLoS Negl Trop Dis. 2011;5(6): e1210.
Zouré HG, Noma M, Tekle AH, Amazigo UV, Diggle PJ, Giorgi E, Remme JH. The geographic distribution of onchocerciasis in the 20 participating countries of the African Programme for Onchocerciasis Control: (2) pre-control endemicity levels and estimated number infected. Parasit Vectors. 2014;7:326.
Kamga G-R, Dissak Delon FN, Nana Djeunga HC, Biholong B, Ghogomu S, Souopgui J, et al. Still mesoendemic onchocerciasis in two Cameroonian community-directed treatment with ivermectin projects despite more than 15 years of mass treatment. Parasit Vectors. 2016;9:12.
Ratard RC, Kouemeni LE, Bessala MME, Ndamkou CN, Sama MT, Cline BL. Ascariasis and trichuriasis in Cameroon. Trans R Soc Trop Med Hyg. 1991;85:84–8.
Ratard R, Kouemeni LE, Ekani Bessala MK, Ndamkou CN. Distribution of hookworm infection in Cameroon. Ann Trop Med Parasitol. 1992;86:413–8.
Djune-Yemeli L, Nana-Djeunga HC, Lenou-Nanga CG, Donfo-Azafack C, Domche A, Fossuo-Thotchum F, et al. Serious limitations of the current strategy to control soil-transmitted helminths and added value of ivermectin/albendazole mass administration: a population-based observational study in Cameroon. PLoS Negl Trop Dis. 2020;14: e0008794.
World Health Organization. Basic laboratory methods in medical parasitology. Geneva: World Health Organization; 1991.
World Health Organization. Cellophane faecal thick smear examination technique (Kato) for diagnosis of intestinal schistosomiasis and gastrointestinal helminth infections. PDP83.3. Geneva: World Health Organization; 1983.
Collins R, Brandling-Bennett A, Holliman R, Campbell C, Darsie R. Parasitological diagnosis of onchocerciasis: comparisons of incubation media and incubation times for skin snips. Am J Trop Med Hyg. 1980;29:35–41.
Bethony J, Brooker S, Albonico M, Geiger S, Loukas A, Diemert D, et al. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet. 2006;367:1521–32.
Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J. Helminth infections: the great neglected tropical diseases. J Clin Invest. 2008;118:1311–21.
World Health Organization. Weekly epidemiological record. World Health Org. 2016;91:585–600.
Clarke NE, Clements ACA, Amaral S, Richardson A, McCarthy JS, McGown J, et al. (S)WASH-D for Worms: a pilot study investigating the differential impact of school- versus community-based integrated control programs for soil-transmitted helminths. PLoS Negl Trop Dis. 2018;12: e0006389.
Truscott JE, Hollingsworth TD, Brooker SJ, Anderson RM. Can chemotherapy alone eliminate the transmission of soil transmitted helminths? Parasit Vectors. 2014;7:266.
Aza’ah RA, Sumo L, Ntonifor NH, Bopda J, Bamou RH, Nana-Djeunga HC. Point prevalence mapping reveals hotspot for onchocerciasis transmission in the Ndikinimeki Health District, Centre Region, Cameroon. Parasit Vectors. 2020;13(1):519.
Kuete T, Mbuagbaw J, Kollo B, Kitobo E, Same-Ekobo A. Distribution des filarioses dans une zone de transition savane-forêt du Cameroun, impact sur la prise en charge: cas de l’Aire de santé de Ntui. Département du Mbam et Kim JCAB. 2009;8:11–6.
Tsapi EM, Todjom FG, Gamago GA, Pone JW, Teukeng FFD. Prevalence of onchocerciasis after seven years of continuous community-directed treatment with ivermectin in the Ntui Health District, Centre region Cameroon. Pan Afr Med J. 2020;36:1–8.
Prost A. Latency period in onchocerciasis. Bull World Health Organ. 1980;58:923–5.
Boussinesq M, Pion SDS, Demanga-Ngangue, Kamgno J. Relationship between onchocerciasis and epilepsy: a matched case-control study in the Mbam Valley, Republic of Cameroon. Trans R Soc Trop Med Hyg. 2002;96:537–41.
Acknowledgements
The authors are thankful to the staff of the four Health Districts for their contribution, and to the participants for their cooperation.
Funding
This study is part of the EDCTP2 programme supported by European Union (Grant Agreement: EDCTP-RegNet2015-1045) through the Central Africa Network on Tuberculosis Aids/HIV, Malaria and NTDs (CANTAM2).
Author information
Authors and Affiliations
Contributions
HCND conceived the study, designed the experiments, participated to field data collection, performed the statistical analyses and prepared the first draft of the manuscript. LDY participated to field data collection, performed the statistical analyses and prepared the first draft of the manuscript. AD participated to field data collection and helped to draft the manuscript. CDA participated to field data collection and helped to draft the manuscript. AEE participated to field data collection and helped to draft the manuscript. CLN participated to study field design and data collection, and helped to draft the manuscript. NNT participated to field data collection and helped to draft the manuscript. YAB participated to field data collection and helped to draft the manuscript. JGB participated to field data collection and helped to draft the manuscript. SMT participated to field data collection and helped to draft the manuscript. TPV participated to funding acquisition and helped to draft the manuscript. VPB participated to funding acquisition and helped to draft the manuscript. FN participated to funding acquisition and helped to draft the manuscript. JK conceived and coordinated the study, designed the experiments, participated to funding acquisition and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
An ethical clearance was obtained from the Faculty of Medicine and Biomedical Sciences Institutional review board (No. 294/UY1/FMSB/VDRC/CSD) and administrative authorizations were granted by the Akonolinga, Bafia, Bangangté, Ntui and Yabassi District Medical Officers. Prior to the beginning of the surveys, the objectives and schedules of the study were explained to all the participants (their parents). Participation was entirely voluntary and any parent was free to let his child opt out without fear of retaliation from their community leaders and program personnel.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
The original online version of this article was revised: The first name is Thirumalaisamy P and the last name is Velavan for the author Tirumalaisamy P. Velavan
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nana-Djeunga, H.C., Djune-Yemeli, L., Domche, A. et al. High infection rates for onchocerciasis and soil-transmitted helminthiasis in children under five not receiving preventive chemotherapy: a bottleneck to elimination. Infect Dis Poverty 11, 47 (2022). https://doi.org/10.1186/s40249-022-00973-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-022-00973-1