Abstract
Background
New insecticides with a novel mode of action such as neonicotinoids have recently been recommended for public health by WHO. Resistance monitoring of such novel insecticides requires a robust protocol to monitor the development of resistance in natural populations. In this study, we comparatively used three different solvents to assess the susceptibility of malaria vectors to neonicotinoids across Africa.
Methods
Mosquitoes were collected from May to July 2021 from three agricultural settings in Cameroon (Njombe-Penja, Nkolondom, and Mangoum), the Democratic Republic of Congo (Ndjili-Brasserie), Ghana (Obuasi), and Uganda (Mayuge). Using the CDC bottle test, we compared the effect of three different solvents (ethanol, acetone, MERO) on the efficacy of neonicotinoids against Anopheles gambiae s.l. In addition, TaqMan assays were used to genotype key pyrethroid-resistant markers in An. gambiae and odds ratio based on Fisher exact test were used to evaluate potential cross-resistance between pyrethroids and clothianidin.
Results
Lower mortality was observed when using absolute ethanol or acetone alone as solvent for clothianidin (11.4‒51.9% mortality in Nkolondom, 31.7‒48.2% in Mangoum, 34.6‒56.1% in Mayuge, 39.4‒45.6% in Obuasi, 83.7‒89.3% in Congo and 71.1‒95.9% in Njombe pendja) compared to acetone + MERO for which 100% mortality were observed for all the populations. Similar observations were done for imidacloprid and acetamiprid. Synergist assays (PBO, DEM and DEF) with clothianidin revealed a significant increase of mortality suggesting that metabolic resistance mechanisms are contributing to the reduced susceptibility. A negative association was observed between the L1014F-kdr mutation and clothianidin resistance with a greater frequency of homozygote resistant mosquitoes among the dead than among survivors (OR = 0.5; P = 0.02). However, the I114T-GSTe2 was in contrast significantly associated with a greater ability to survive clothianidin with a higher frequency of homozygote resistant among survivors than other genotypes (OR = 2.10; P = 0.013).
Conclusions
This study revealed a contrasted susceptibility pattern depending on the solvents with ethanol/acetone resulting to lower mortality, thus possibly overestimating resistance, whereas the MERO consistently showed a greater efficacy of neonicotinoids but it could prevent to detect early resistance development. Therefore, we recommend monitoring the susceptibility using both acetone alone and acetone + MERO (4 µg/ml for clothianidin) to capture the accurate resistance profile of the mosquito populations.
Graphical Abstract

Similar content being viewed by others
Background
Malaria prevention relies extensively on mosquito control using pyrethroid-based interventions including indoor residual spraying (IRS) and long-lasting insecticidal nets (LLINs) [1, 2]. The scale-up of these tools has significantly contributed to the important reduction of malaria burden in the past decade [1, 3]. However, increasing resistance to pyrethroid in malaria vector species is a serious challenge to these vector control interventions given the heavy reliance on pyrethroid only [4]. Most African Anopheles gambiae and An. funestus populations are resistant to pyrethroid insecticides and also show varying levels of resistance to other insecticides used for vector control (carbamates, organophosphates and organochlorines). Due to the threat posed by insecticide resistance, there has been an urgent call for alternative insecticides to supplement malaria vector control [5]. Novel insecticides are gradually being introduced by manufacturers and recommended by World Health Organization (WHO) for vector control [6]. Among these, the neonicotinoids (e.g. clothianidin) and pyrole (e.g. chlorfenapyr) are the new mode of action insecticide classes for public health, recently recommended by WHO for LLINs and IRS [7].
Clothianidin is a neonicotinoid insecticide that is chemically similar to nicotine. It acts on the central nervous system of insects as an agonist of acetylcholine and stimulates nicotine acetylcholine receptors (nAChR) [8] activating post-synaptic acetylcholine receptors but does not inhibit acetyl cholinesterase (ACh). High levels overstimulate and block the receptors [9], causing paralysis and death [8]. Clothianidin is the active ingredient in SumiShield (developed by Sumitomo Chemical Company, Japan) and Fludora® Fusion (Bayer CropScience, Monheim, Germany) along with deltamethrin, an IRS formulation which was recently added to the WHO prequalification list of recommended insecticides (https://www.who.int/pq-vector-control/ prequalifed-lists/en/).
As new insecticides are developed, it is essential to monitor the development of resistance to prolong their efficacy as much as possible and avoid the level of widespread resistance now seen with pyrethroids [3]. Such resistance monitoring requires establishing diagnostic concentrations to determine baseline susceptibility of malaria vectors and to enable surveillance of insecticide resistance once the insecticides are in use.
Nowadays, WHO protocol to test the susceptibility to neonicotinoids in mosquitoes is not well established thus, making resistance monitoring to this insecticide class very challenging. Clothianidin (neonicotinoid; IRAC MoA class 4A) for example, tends to crystallize if used in straight acetone/ethanol (solvents commonly used in bioassays) and the uptake of active ingredient between the insect’s body and the crystal is very low [10,11,12]. This has made the design of standard protocols more arduous compared to other insecticide classes. In addition, because this active ingredient acts slowly, resistance profiles can be detected after bioassays only if exposed populations are rigorously monitored during a long holding period, which can last for seven days or more. Despite these difficulties, the susceptibility of wild Anopheles populations from several African countries has been evaluated using 150 µg/ml of clothianidin dissolved in either absolute ethanol or acetone [10,11,12,13]. Recently, Bayer CropScience Ltd. introduced an 81% Rapeseed oil methyl ester (0.11% MERO®) which, when added to acetone, prevents the crystallization then keeps the clothianidin for a longer period in a solved state and allows therefore the feasibility of the bottle assay. A study conducted in ivory coast, established 50 µg/ml as diagnostic dose of clothianidin [14]. However, this study did not evaluate the lower doses to see if 50 µg/ml cannot mask the detection of resistance highlighting the need of stabilising the protocol for testing of neonicotinoids. In this study, we used three different solvents to comparatively evaluate the efficacy of neonicotinoids on malaria vectors from many African countries and established the diagnostic dose of clothiandin using acetone and MERO. Furthermore, we evaluated a potential cross-resistance between pyrethroids and clothianidin.
Methods
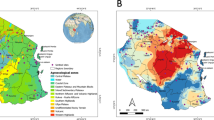
Study sites
Mosquitoes were collected from 4 regions across the continent. Mosquitoes were collected in three agricultural settings in Cameroon (Mangoum, Nkolondom, and Njombe-Penja) from May to July 2021. The climate is made up of two wet and two dry seasons typical of tropical climate around the equator. In the Democratic Republic of Congo (DRC) mosquitoes were collected at Ndjili Brasserie, a suburb of Kinshasa (4°19′39″S, 15°18′48″E), in June 2021. In Uganda, mosquitoes were collected in the Eastern region (May 2021), Mayuge (0°23′10.8′′N, 33°37′16.5′′E), and in Ghana collections were done in Obuasi (5°56′N, 1°37′W) in July 2021. In Cameroon, immature stages were collected from the breeding site using the dipping method whereas in other countries indoor resting blood fed females were collected using electric aspirators. Emerging adults (2‒5 days old) from collected larvae or F1 progeny (2‒5 days old) from indoor collected females were used for the bioassays.
Molecular identification
The genomic DNA was extracted from a subset of mosquitoes from each of the collection sites using the Livak method [25], then the members of the An. gambiae complex were identified by the PCR [26, 27].
Determination of susceptibility to neonicotinoids and establishment of the diagnostic dose of clothianidin using acetone + MERO as solvent
Clothianidin, imidacloprid and acetamiprid used were technical materials from Sigma (PESTANAL®, analytical standard, Sigma-Aldrich, Dorset, United Kingdom). These chemicals were mixed in three different solvents (acetone, absolute ethanol, or acetone with MERO). For acetone and ethanol alone, the dose of 150 µg/ml for clothianidin, 200 µg/ml for imidacloprid and 75 µg/ml for acetamiprid were used as previously described [11].
For acetone dissolved in MERO, a stock solution of an acetone/MERO® mixture was made by pipetting 0.11 ml (110 µl) MERO® to 100 ml of acetone (0.11%). 900 µg straight clothianidin was weighed and mixed with 10 ml of this stock solution of MERO plus acetone. After complete dissolution of the active ingredient, 10 ml acetone/MERO® solution containing 900 µg clothianidin was prepared. One [1] ml of this solution was applied to each test bottle to achieve a concentration of 90 µg clothianidin/250 ml bottle. This dose of insecticide was used to characterise the susceptibility of different mosquito populations. In addition, ranges of insecticide concentrations were tested (0.25, 0.50, 1, 2, 4, 40 and 90 µg/ml) using the susceptible lab strain Kisumu to evaluate the diagnostic dose of clothianidin when diluted in acetone and MERO. Approximately 24 h after coating bottles with insecticide, 25 female Kisumu (3–5 days old) were exposed to the insecticides for 1 h and the knocked down mosquitoes were recorded at the end of the 60 min (Kd-60) exposure period. After recording the Kd-60 mosquitoes were gently aspirated from the bottle into clean paper cups and provided with 10% sugar solution soaked in cotton wool during the recovery period and the final mortality was recorded 24 h post-exposure.
Synergist assay with piperonyl butoxide (PBO), di-ethyl Maleate (DEM) and s,s,s–tri-butylphosphorotrithioate (DEF)
To identify the possible enzyme systems involved in reduced susceptibility to neonicotinoids, synergist bioassays were conducted for clothianidin in Nkolondom using the emerging adult from larval collection. Two- to four-day-old F0/F1 females were first exposed to the synergist (4% PBO, 8% DEM or 0.25% DEF) for 1 h, followed by exposure to 150 µg/ml clothianidin (dissolved in acetone) for 1 h. Mortality was recorded 24 h after exposure and the differences in mortalities between synergized and non-synergized experiments were compared using a Chi-square test.
Potential cross-resistance between neonicotinoids and pyrethroids
To assess the potential cross-resistance between neonicotinoids and pyrethroids, we crossed the pyrethroid highly resistant field strain from Nkolondom (where the 1014F-Kdr is fixed) with the fully susceptible laboratory strain Kisumu (with no 1014F-Kdr). This hybrid strain was exposed to sub-lethal doses of clothianidin (dissolved in acetone only) to select the dead and alive mosquitoes. These mosquitoes were genotyped for the L1014F target-site knockdown resistance (Kdrw) and the 114 T-GSTe2 metabolic resistance marker (all associated with DDT/pyrethroid resistance in An. gambiae) using Taqman methods as previously described [15, 16]. PCR reactions (10 μl) contained 1 μl of genomic DNA, 5 μl of SensiMix DNA kit (catalog: SM2-717104), 0.125 μl of each probe and 3.875 μl of sigma water. Samples were run on a Mx3000P™ Multiplex quantitative PCR system with the temperature cycling conditions of: 10 min at 95 °C followed by 40 cycles of 95 °C for 10 s and 60 °C for 45 s.
Odds ratio and Fisher exact test were used to establish the statistical significance of any association between this DDT/pyrethroid resistance marker and the ability to survive clothianidin exposure.
Data analysis
GraphPad Prism 7.00 was used for a construction of graphs. Chi-square test was used to compare the mortality rate between different treatments whereas odds ratio and Fisher exact test were used to establish statistical significance of any association between pyrethroid resistant markers and mosquitoe's ability to survive clothianidin exposure.
Results
Molecular identification of mosquitoes tested
PCR assays revealed that all the mosquitoes tested from Mangoum (44/44), Nkolondom (50/50), and Congo (60/60) were An. gambiae. Those collected in Njombe (Cameroon) were mainly An. coluzzii (58/60). The An. gambiae s.l. population from Uganda were mix of 82% An. gambiae and 17% An. arabiensis whereas those from Ghana were 60% (39/65) An. gambiae and 40% (39/65) An. coluzzii.
Susceptibility profile to clothianidin
The Kisumu lab strain was susceptible to clothianidin whatever the solvent used (Fig. 1A and Additional file 1: Fig. S1). However, the susceptibility to this insecticide varied significantly in An. gambiae field populations depending on the solvent used. Using acetone combined with 0.11% MERO® (81% Rapeseed oil methyl ester) as solvent, induced significant higher mortality compared to acetone or ethanol alone (Fig. 1A). A full susceptibility was observed for all the An. gambiae populations with a mortality rate of 100% when exposed to clothianidin dissolved in acetone + MERO at a concentration of 90 µg/ml (Fig. 1A). However, when exposed to clothianidin dissolved in acetone alone (150 µg/ml), the mortality varied from 51.1 ± 15.2% in Nkolondom to 95.9 ± 2.6% in Njombe-Penja. On the other hand, when using ethanol as solvent, the mortality varied from 11.4 ± 4.6% in Nkolondom to 71.0 ± 6.9% and 89.3 ± 7.6% in Njombe-penja and Ndjilli (DRC) respectively (Fig. 1A). The mortality with these two solvents increased significantly from 24 h to 7 days post-exposure confirming a slow-acting effect of this insecticide (Additional file 1: Fig. S1, Additional file 2: Fig. S2 and Additional file 3: Fig. S3).
Susceptibility profile of An. gambiae s.l. to clothianidin across Africa. A Mortality rate (%) of mosquitoes from various sites 7 days post-exposure to clothianidin dissolved in different solvents compared to the susceptible lab strain Kisumu. B Effect of pre-exposure to synergist PBO, DEM and DEF against clothianidin on An. gambiae from Nkolondom. Results are average of percentage mortalities from four–five replicates each. The bars represent the standard error on the mean (SEM), linear color dots indicate the threshold for resistance (red) and susceptibility (green). CMR Cameroon, DRC Democratic Republic of Congo, GH Ghana, UG Uganda
Susceptibility profile to imidacloprid
The susceptibility to imidacloprid was evaluated on mosquitoes from Nkolondom and Mangoum (Cameroon), Obuasi (Ghana) and Mayµge (Uganda). Higher mortality with this insecticide was observed in all the localities when using acetone + MERO as solvent. In Nkolondom, a mortality rate of 83.9% was observed with acetone + MERO compared to 65.3 ± 16.6% with acetone only (χ2 = 10.9; P = 0.001) and 27.2% with ethanol (χ2 = 64.8; P < 0.0001) suggesting a likely resistance in this population (Fig. 2A). The similar pattern was observed in Mangoum where a mortality rate of 96.6% was observed with acetone + MERO compared to 27.7% with acetone only (χ2 = 100; P < 0.0001) and 40.4% with absolute ethanol (χ2 = 72.8; P < 0.0001) (Fig. 2A). In Ghana, imadacloprid dissolved in acetone + MERO induced 97.9% mortality and 57.2% when dissolved in acetone only (χ2 = 47.3; P < 0.0001). The mortality was very low when using absolute ethanol as solvent with mortality rate of 12.6% (χ2 = 146; P < 0.0001). The similar profile (96.1% mortality vs. 27.3%) was obtained in Uganda (χ2 = 99.6; P < 0.0001).
Susceptibility profile of An. gambiae s.l. to imidacloprid and acetamiprid across Africa. Mortality rate (%) of mosquitoes from different sites 7 days post-exposure to imidacloprid A and acetamiprid B dissolved in various solvents compared to the susceptible lab strain Kisumu. Results are average of percentage mortalities from four–five replicates each ± SEM. Linear colour dots indicate the threshold for resistance (red) and susceptibility (green). CMR: Cameroon; GH: Ghana; UG: Uganda
Susceptibility profile to acetamiprid
When dissolved in acetone + MERO, acetamiprid also displayed greater efficacy compared to when dissolved in acetone only (Fig. 2B). In Nkolondom, 100% mortality was obtained when using acetone and MERO compared to 73.5 ± 6.6% without MERO (χ2 = 30.4; P < 0.0001). In Obuasi, 89.0 ± 4.6% mortality was obtained when using acetone and MERO compared to 30% without MERO (χ2 = 71.8; P < 0.0001) (Fig. 2B). In Mayuge, full susceptibility was noticed with MERO compared to 60% mortality without MERO (χ2 = 49.7; P < 0.0001). These results suggest that the level of reduced susceptibility to acetamiprid is higher in Ghana compared to other locations tested.
Synergist test
Susceptibility testing using PBO, DEM, and DEF as synergists revealed a significant recovery of susceptibility to clothianidin in Nkolondom which showed a highest level of reduced susceptibility to this insecticide when diluted in ethanol or acetone alone (Fig. 1B). In Nkolondom, the mortality with clothianidin + PBO was 96.0 ± 2.6% versus 51.9 ± 8.5% for clothianidin without PBO pre-exposure (χ2 = 59.5; P < 0.0001). The same pattern was observed with DEM: DEM pre-exposure 92.1 ± 3.2% vs. 51.9 ± 8.5% for no DEM pre-exposure (χ2 = 38.6; P < 0.0001) (Fig. 1B). Synergist bioassay with DEF also revealed significant recovery of susceptibility to clothianidin (DEF pre-exposure 86.4 ± 7.1% vs. 51.9 ± 8.5% mortality without DEF pre-exposure; χ2 = 28.6; P < 0.0001) although this was slightly lower compared to PBO and DEM. All these results suggest that monooxygenases, GSTs and esterases all combined to drive the reduced susceptibility clothianidin resistance in Nkolondom.
Diagnostic dosage of clothianidin using acetone and MERO as a solvent
Because of the very high mortality consistently observed with clothianidin dissolved in acetone + MERO, we decided to establish the diagnostic concentration using the susceptible lab strain Kisumu. The mortality 24 h post-exposure to clothianidin were ranged from 66.8 ± 7.0% at 0.25 µg/ml, 60.9 ± 9.4% at 0.5 µg/ml, 82.8 ± 9.3% at 1 µg/ml to 94.2 ± 3.6% at 2 µg/ml and 100% at 4 µg/ml, 40 µg/ml and 90 µg/ml (Fig. 3). These results suggest that the concentration of 4 µg/ml (as 2 µg/ml kills more than 90% of the susceptible strain) could be used as a diagnostic dose for resistance monitoring in the field populations of malaria vectors.
Assessment of diagnostic dose of clothianidin using acetone and MERO as solvent. Percentage mortality (24 h) of the susceptible lab strain Kisumu after exposure to each of the six concentrations of clothianidin (with acetone + MERO as solvent). LC50 represents the concentration able to kill 50% of mosquitoes and LC90 the concentration able to kill 90%
Cross-resistance between clothianidin and pyrethroids
The distribution of L1014F-Kdr_w genotypes in mosquitoes alive after exposure to a sub-lethal dose of clothianidin was as follows: 24.1% (7/29) homozygous resistant (1014F/F), 27.6% (8/29) heterozygotes (L1014F-RS) and 55.17% (16/29) homozygous susceptible (L/L1014) (Fig. 4). In the dead mosquitoes, 30.0% (9/30) were homozygous resistant (1014F/F), 46.7% (14/30) were heterozygotes (L1014F-RS) whereas 23.3% (7/30) were homozygous susceptible (L/L1014). A significant difference was observed in the distribution of L1014F-Kdr_w genotypes between alive and dead mosquitoes (χ2 = 18.5; P < 0.0001) with the homozygote resistant mosquitoes less able to survive (OR = 0.5; 95% CI: 0.3–0.9; P = 0.02) compared to the susceptible genotypes (Table 1). In contrast, a significant difference was observed in the distribution of the I114T-GSTe2 genotypes between dead and alive mosquitoes and those with resistant allele had more ability to survive clothianidin exposure (χ2 = 9.78; P = 0.007) (Figs. 4 and 5). Assessing of the odds-ratio confirmed that mosquitoes with the 114T resistant allele have a significantly greater ability to survive compared to those with the I114 allele as homozygous resistant mosquitoes were significantly more likely to survive clothianidin exposure compared to both heterozygote (OR = 2.10; 95% CI: 1.11–3.97; P = 0.013) and homozygous susceptible (OR = 2.46; 95% CI: 1.15–5.26; P = 0.012) mosquitoes (Table 2). There was no difference between heterozygote and susceptible mosquitoes (OR = 1.17; P = 0.41).
Discussion
The present study compared the efficacy of neonicotinoids in the major malaria vector An. gambiae s.l. across many African countries using three different solvents. Susceptibility testing confirmed that neonicotinoids are slower-acting insecticides (when using acetone or ethanol alone) compared with neurotoxic pyrethroids [17]. While pyrethroids are characterized by rapid mortality of mosquitoes within 24 h, clothianidin/imidacloprid/acetamiprid dissolved in ethanol or acetone alone induced mortality at 24 h post-exposure was generally low (albeit highly variable) and increased over days. Final mortality was recorded seven days post-exposure when using ethanol/acetone alone as done previously [10]. The mortality was low when using ethanol and acetone alone and was the lowest in Nkolondom, an area of intense agriculture. The mortality rates of less than 20% with ethanol and less than 40% with acetone observed in this locality support a recent report of reduced susceptibility to neonicotinoids in the An. gambiae population of this location [18]. However, the addition of 0.11% MERO® (81% rapeseed oil methyl ester) increased significantly the effect of these insecticides with 100% mortality for all the populations 24 h post exposure even at a very low concentration. The low knock-down/mortality observed for all the populations when using ethanol or acetone alone as a solvent could be linked to the crystallization issue reported for neonicotinoids [19] preventing complete knockdown/mortality within 1‒2 h. The use of MERO® by preventing the crystallization, keeps the neonicotinoids for a longer period in a soluble state and increases the reliability of the bottle assay.
Despite the low mortality obtained with acetone or ethanol alone, a significant difference was observed between different populations with a mortality rate of 11.4% observed in Nkolondom, 31.1% in Mangoum, 45.6% in Ghana and Uganda compared to 71% in Njombe or 89.3% in Congo and 100% in Kisumu. This indicates that using ethanol or acetone alone might still be useful in capturing the variability between populations and even to detect those populations with reduced susceptibility and thus allow a better management of resistance. In contrast, using acetone plus MERO although more suitable in showing the full efficacy of neonicotinoids, might mask the selection of resistance in populations if not used at the right dose and could prevent detecting the emergence of resistance. Therefore, to take advantage of the strengths of both profiles it could be beneficial to monitor the susceptibility profile to neonicotinoids using acetone (or ethanol) alone and also acetone plus MERO. Because the dose of 90 µg/ml as recommended by Bayer or 50 µg as determined recently in Ivory coast is very high for monitoring of resistance, one option could be to reduce this dose to a level allowing to assess the efficacy of neonicotinoids while monitoring resistance development. In this study, we observed that the concentration of 4 µg/ml could be used for monitoring of resistance to clothianidin as 2 µg was giving more than 90% mortality with the susceptible lab strain Kisumu.
Cross resistance between pyrethroid and neonicotinoid
A negative association was observed between the 1014F-kdr allele and resistance to clothianidin. Such negative impact could be attributed to the deleterious effect of kdr or other related genes in the presence of clothianidin, for which the vgsc is not the target. Accordingly, a gradual decrease of kdr-resistant homozygotes mosquitoes was observed during the clothianidin selection process by Zoh et al. [20] and this could explain the negative correlation observed in this study between kdr and clothianidin resistance. This is the first time such negative association is observed between pyrethroid resistance mechanism and insecticides with different mode of action. However, more studies are needed to clarify the link between kdr and clothianidin resistance.
Synergist assay using PBO and DEF also revealed significant recovery of susceptibility to clothianidin showing that monoxygenases, GSTs and esterases are all involved in clothianidin resistance. Over expression of P450s monoxygenases was frequently reported in many resistant cases such as in An. gambiae recently where a strong selection signature associated with clothianidin selection was observed on a cytochrome P450 gene cluster with the gene CYP6M1 showing the highest selection signature together with a transcription profile supporting a role in clothianidin resistance. Overexpression of P450s were also mentioned in Myzus persicae [21], Bemisia tabaci [22,23,24], Trialeurodes vaporariorum [25], Nilaparvata lµgens [26], Leptinotarsa decemlineata [27] and many other pests [28].
For the first time, we observed in this study a significant correlation between GSTe2 and clothianidin resistance in An. gambiae indicating that GSTe2 could metabolise or could be involved in phase 2 conjugation of metabolite of clothianidin degradation. This can be supported by the synergist testing with DEM which helped to recover the susceptibility to clothianidin. Since GSTe2 is also pyrethroid/DDT resistance gene, its association with clothianidin resistance indicates that clothianidin-based tools could probably show reduced efficacy in areas of high GSTe2-based metabolic resistance. However, future studies are needed to establish the role of GST or specific mechanisms such as esterases and P450s in clothianidin resistance.
One limitation of the study is that we did not evaluate the susceptibility profile of field mosquitoes with 4 µg/ml which was found as a diagnostic concentration (with acetone + Mero) but this will be done in the future.
Conclusions
This study investigated the susceptibility of the major African malaria vector An. gambiae to neonicotinoids using three different solvents and evaluated potential cross resistance between pyrethroid resistance markers and clothianidin survival. The study revealed that the use of acetone or ethanol alone as a solvent for clothianidin can over-estimate the level of resistance in mosquitoes due to crystallisation issue. Furthermore, we showed that the use of clothiandin dissolved in acetone + MERO display very strong efficacy with 4 µg/ml as diagnostic dose for monitoring of resistance to clothianidin but could mask the development of resistance. We recommend therefore monitoring the susceptibility using both acetone alone and acetone + MERO to capture the accurate resistance profile of the mosquito populations.
Availability of data and materials
All the relevant datasets supporting the conclusions of this article are included within the article.
References
Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015;526(7572):207–11.
World Health Organization. World Malaria Report 2016. Geneva: World Health Organization; 2016.
Riveron JM, Tchouakui M, Mugenzi L, Menze BD, Chiang MC, Wondji CS. Insecticide resistance in malaria vectors: An update at a global scale. Towards Malaria Elimination-A Leap Forward: IntechOpen; 2018.
Hemingway J, Vontas J, Poupardin R, Raman J, Lines J, Schwabe C, et al. Country-level operational implementation of the Global Plan for Insecticide Resistance Management. Proc Natl Acad Sci U S A. 2013;110(23):9397–402.
Blaschke TF, Lumpkin M, Hartman D. The World Health Organization prequalification program and clinical pharmacology in 2030. Clin Pharmacol Ther. 2020;107(1):68–71.
Hemingway J. The way forward for vector control. Science. 2017;358(6366):998–9.
WHO. Global vector control response: progress in planning and implementation. 2020.
Krupke CH, Long EY. Intersections between neonicotinoid seed treatments and honey bees. Curr Opin Insect Sci. 2015;10:8–13.
Yamamoto I, Casida JE. Nicotinoid insecticides and the nicotinic acetylcholine receptor. Tokyo: Springer; 1999.
Oxborough RM, Seyoum A, Yihdego Y, Chabi J, Wat’senga F, Agossa FR, et al. Determination of the discriminating concentration of chlorfenapyr (pyrrole) and Anopheles gambiae sensu lato susceptibility testing in preparation for distribution of Interceptor® G2 insecticide-treated nets. Malar J. 2021;20(1):1–10.
Agumba S, Gimnig JE, Ogonda L, Ombok M, Kosgei J, Munga S, et al. Diagnostic dose determination and efficacy of chlorfenapyr and clothianidin insecticides against Anopheles malaria vector populations of western Kenya. Malar J. 2019;18(1):1–9.
Dagg K, Irish S, Wiegand RE, Shililu J, Yewhalaw D, Messenger LA. Evaluation of toxicity of clothianidin (neonicotinoid) and chlorfenapyr (pyrrole) insecticides and cross-resistance to other public health insecticides in Anopheles arabiensis from Ethiopia. Malar J. 2019;18(1):1–11.
Darriet F, Chandre F. Efficacy of six neonicotinoid insecticides alone and in combination with deltamethrin and piperonyl butoxide against pyrethroid-resistant Aedes aegypti and Anopheles gambiae (Diptera: Culicidae). Pest Manag Sci. 2013;69(8):905–10.
Mouhamadou CS, de Souza SS, Fodjo BK, Zoh MG, Bli NK, Koudou BG. Evidence of insecticide resistance selection in wild Anopheles coluzzii mosquitoes due to agricultural pesticide use. Infect Dis Poverty. 2019;8(1):1–8.
Bass C, Williamson MS, Wilding CS, Donnelly MJ, Field LM. Identification of the main malaria vectors in the Anopheles gambiae species complex using a TaqMan real-time PCR assay. Malar J. 2007;6(1):1–9.
Mitchell SN, Rigden DJ, Dowd AJ, Lu F, Wilding CS, Weetman D, et al. Metabolic and target-site mechanisms combine to confer strong DDT resistance in Anopheles gambiae. PLoS ONE. 2014;9(3):e92662.
Anto F, Asoala V, Anyorigiya T, Oduro A, Adjuik M, Owusu-Agyei S, et al. Insecticide resistance profiles for malaria vectors in the Kassena-Nankana district of Ghana. Malar J. 2009;8(1):1–8.
Fouet C, Ashu AF, Ambadiang MM, Tchapga W, Wondji CS, Kamdem C. Resistance of Anopheles gambiae to the new insecticide clothianidin associated with unrestricted use of agricultural neonicotinoids in Yaounde, Cameroon. BioRxiv. 2020. https://doi.org/10.1101/2020.08.06.239509.
Stica C, Jeffries CL, Irish SR, Barry Y, Camara D, Yansane I, et al. Characterizing the molecular and metabolic mechanisms of insecticide resistance in Anopheles gambiae in Faranah, Guinea. Malar J. 2019;18(1):1–15.
Zoh MG, Bonneville JM, Tutagana J, Laporte F, Fodjo BK, Mouhamadou CS, et al. Neonicotinoid and pyrethroid combination: A tool to manage insecticide resistance in malaria vectors? Insights from experimental evolution. BioRxiv. 2021. https://doi.org/10.1101/2021.06.09.447494.
Puinean AM, Foster SP, Oliphant L, Denholm I, Field LM, Millar NS, et al. Amplification of a cytochrome P450 gene is associated with resistance to neonicotinoid insecticides in the aphid Myzus persicae. PLoS Genet. 2010;6(6):e1000999.
Karunker I, Benting J, Lueke B, Ponge T, Nauen R, Roditakis E, et al. Over-expression of cytochrome P450 CYP6CM1 is associated with high resistance to imidacloprid in the B and Q biotypes of Bemisia tabaci (Hemiptera: Aleyrodidae). Insect Biochem Mol Biol. 2008;38(6):634–44.
Jones CM, Daniels M, Andrews M, Slater R, Lind RJ, Gorman K, et al. Age-specific expression of a P450 monooxygenase (CYP6CM1) correlates with neonicotinoid resistance in Bemisia tabaci. Pestic Biochem Physiol. 2011;101(1):53–8.
Yang N, Xie W, Jones C, Bass C, Jiao X, Yang X, et al. Transcriptome profiling of the whitefly Bemisia tabaci reveals stage-specific gene expression signatures for thiamethoxam resistance. Insect Mol Biol. 2013;22(5):485–96.
Karatolos N, Williamson MS, Denholm I, Gorman K, Ffrench-Constant RH, Bass C. Over-expression of a cytochrome P450 is associated with resistance to pyriproxyfen in the greenhouse whitefly Trialeurodes vaporariorum. PLoS ONE. 2012;7(2):e31077.
Bass C, Carvalho R, Oliphant L, Puinean A, Field L, Nauen R, et al. Overexpression of a cytochrome P450 monooxygenase, CYP6ER1, is associated with resistance to imidacloprid in the brown planthopper Nilaparvata lugens. Insect Mol Biol. 2011;20(6):763–73.
Zhao J-Z, Bishop BA, Grafius EJ. Inheritance and synergism of resistance to imidacloprid in the Colorado potato beetle (Coleoptera: Chrysomelidae). J Econ Entomol. 2000;93(5):1508–14.
Bass C, Denholm I, Williamson MS, Nauen R. The global status of insect resistance to neonicotinoid insecticides. Pestic Biochem Physiol. 2015;121:78–87.
Acknowledgements
We are very grateful to all the international partners for supporting in sample collection. We are also grateful to the Community Health Workers from all the villages
Funding
This study was funded by the BMGF Grant (INV-006003) awarded to CSW.
Author information
Authors and Affiliations
Contributions
CSW conceived and designed the study; MT, LMJM, BDM, DNN, collected the samples with the help of JK, FW, EZM, and MO; MT, TA, and WT, maintained the strain in the insectary and performed bioassays; MT and T.A performed the molecular analyses; MT, and CSW analyzed the data; MT wrote the manuscript with contributions from and CSW, JK, FW, EZM., and MO. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
This paper is published with the authority from the Executive Director of the Centre for Research in Infectious Diseases (CRID).
Competing interests
The authors declare no conflicts of interests.
Supplementary Information
Additional file 1.
Variation in mortality rate of the lab strain kisumu over 7days after exposure to clothianidin and imidacloprid with different solvents.
Additional file 2.
Variation in mortality rate of An gambiae populations across Africa over 7days after exposure to clothianidin with different solvents.
Additional file 3.
Variation in mortality rate of An gambiae populations from Ghana and Uganda over 7days after exposure to clothianidin with different solvents.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tchouakui, M., Assatse, T., Mugenzi, L.M.J. et al. Comparative study of the effect of solvents on the efficacy of neonicotinoid insecticides against malaria vector populations across Africa. Infect Dis Poverty 11, 35 (2022). https://doi.org/10.1186/s40249-022-00962-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-022-00962-4