Abstract
Background
Non-pharmaceutical interventions (NPIs) are a crucial suite of measures to prevent and control infectious disease outbreaks. Despite being particularly important for crisis-affected populations and those living in informal settlements, who typically reside in overcrowded and resource limited settings with inadequate access to healthcare, guidance on NPI implementation rarely takes the specific needs of such populations into account. We therefore conducted a systematic scoping review of the published evidence to describe the landscape of research and identify evidence gaps concerning the acceptability, feasibility, and effectiveness of NPIs among crisis-affected populations and informal settlements.
Methods
We systematically reviewed peer-reviewed articles published between 1970 and 2020 to collate available evidence on the feasibility, acceptability, and effectiveness of NPIs in crisis-affected populations and informal settlements. We performed quality assessments of each study using a standardised questionnaire. We analysed the data to produce descriptive summaries according to a number of categories: date of publication; geographical region of intervention; typology of crisis, shelter, modes of transmission, NPI, research design; study design; and study quality.
Results
Our review included 158 studies published in 85 peer-reviewed articles. Most research used low quality study designs. The acceptability, feasibility, and effectiveness of NPIs was highly context dependent. In general, simple and cost-effective interventions such as community-level environmental cleaning and provision of water, sanitation and hygiene services, and distribution of items for personal protection such as insecticide-treated nets, were both highly feasible and acceptable. Logistical, financial, and human resource constraints affected both the implementation and sustainability of measures. Community engagement emerged as a strong factor contributing to the effectiveness of NPIs. Conversely, measures that involve potential restriction on personal liberty such as case isolation and patient care and burial restrictions were found to be less acceptable, despite apparent effectiveness.
Conclusions
Overall, the evidence base was variable, with substantial knowledge gaps which varied between settings and pathogens. Based on the current landscape, robust evidence-based guidance is not possible, and a research agenda is urgently required that focusses on these specific vulnerable populations. Although implementation of NPIs presents unique practical challenges in these settings, it is critical that such an agenda is put in place, and that the lessons learned from historical and present experiences are documented to build a firm evidence base.
Graphical Abstract

Similar content being viewed by others
Background
Non-pharmaceutical interventions (NPIs), also referred to as Public Health and Social Measures, are an important suite of health interventions used to reduce transmission and mitigate impacts of infectious diseases, particularly during early phases of epidemics when effective pharmaceutical interventions (i.e. therapeutics and vaccination) are not yet available or widely accessible [1].
NPIs range from lighter-touch personal protective measures, such as hand-hygiene and mask-wearing, to more stringent restrictions applied at community or societal levels, such as quarantines and travel bans, that are specifically geared to limiting person-to-person spread no matter the mode of transmission. Recently, there has been substantial research and guidance on implementing NPIs against pandemic influenza [2,3,4,5,6] and COVID-19 [7,8,9,10,11,12,13].
Humanitarian crises are characterised by limited access to resources, chronic underfunding, and poor accessibility. Within such settings, people are subject to an exacerbation of the inverse care law, whereby socially disadvantaged people have poorer access to more effective forms of disease prevention and control, specifically therapeutics and vaccinations, for which costs are higher and/or the global stockpile limited [14]. The number and geographic origin of crisis-affected individuals has expanded in recent years, with nearly 168 million people in need of humanitarian assistance and protection in 2020, an 86% increase since 2015 [15, 16]. In addition, an estimated one billion people, or one-third of the world’s urban population, live in informal settlements (slums), which are characterised by similar constraints [17, 18], and therefore also merit special consideration when planning disease prevention and control interventions.
While research and guidance has been published exploring NPI implementation in non-emergency settings [1, 19], the evidence base remains limited [20], and little work has focussed on these millions of particularly vulnerable people. Furthermore, existing guidance does not account for context-specific risk factors that these settings present and that increase the risks of infectious disease outbreaks, including densely crowded and low-quality shelters, poor access to water, sanitation and hygiene (WASH) facilities, and nutritional stress [21, 22]. Understanding the potential use and impact of NPIs in containing the spread of infectious diseases in these settings is, therefore, critical. Despite this, there remain important gaps in the understanding of three key areas that influence the extent to which implementation of NPIs will be successful: (1) feasibility (how realistic is it to implement the proposed interventions given logistical, financial, socio-cultural, and other barriers); (2) acceptability (how do affected communities perceive the interventions); and (3) effectiveness (do the measures impact disease transmission in real-life).
Therefore, we conducted a systematic scoping review of the published literature to better understand the range and quality of evidence on the feasibility, acceptability, and effectiveness of NPIs against infectious diseases among crisis-affected populations and in informal settlements. We present and synthesise this work, identifying gaps for further research to guide infectious disease prevention and control activities among these vulnerable populations.
Materials and methods
Eligibility criteria
Articles describing research on NPIs against infectious diseases conducted in humanitarian crisis-affected settings and informal settlements, two settings typified by similarly exacerbated infectious disease risks and resource constraints for disease prevention and control, were eligible for inclusion. We defined crisis-affected settings as those in which ‘an event or series of events has resulted in a critical threat to health, safety, security or well-being of a community or other large group of people’ [12], identifying five conditions, as previously described [23]: (1) progressive loss of livelihoods and deterioration of essential services due to ever-present risk of violence; (2) mass displacement into camp-like settlements; (3) displacement into neighbouring host communities; (4) sudden loss of livelihoods and rapid environmental change due to natural disaster, and (5) food crises. The United Nations Human Settlements Programme defines informal settlements as human settlements that have the following characteristics: inadequate access to safe water; inadequate access to sanitation and other infrastructure; poor structural quality of housing; overcrowding; and insecure residential status [17, 24]. We classified NPIs according to adapted versions of available taxonomies previously developed for influenza and COVID-19, including additional measures unrelated to these diseases [2, 3, 25,26,27].
Articles written in English and published in peer-reviewed journals between 1970 and 2020 were eligible for inclusion. Both quantitative and qualitative studies were included, provided they contained relevant primary data.
These inclusion and exclusion criteria are summarised in greater detail in Additional file 1: Table S1.
Search strategy and information sources
On 24 May 2020, we searched two bibliographic databases, PubMed and Web of Science, for entries dated between 1970 and 2020. The full search terms are listed in Additional file 1. This search was repeated on 5 January 2021 to gather additional literature published after the initial search.
Studies were loaded into Covidence systematic review management software (Veritas Health Innovation) [28]. Duplicate entries were automatically detected and reduced to single entries. Review articles returned by the initial search were screened for potentially relevant references, which were added to the list of articles, with the reviews subsequently excluded. The following steps were then carried out on the deduplicated records independently by two reviewers. Irrelevant articles were excluded in two-steps; first by screening titles and abstracts and then by screening the full text of the remaining articles. Discrepancies and borderline cases were resolved through discussions between at least two reviewers.
Data charting process
The final list of included articles was divided among reviewers for data charting (extraction and summary) using a structured questionnaire. The data items extracted related to several domains: (1) study metadata: authors, publication year, the years during which the NPIs were implemented, the region (using World Bank classification scheme) and country of study, country of origin of the crisis-affected population; (2) typologies of crisis, population, shelter, disease transmission mode, and level of intervention (individual, community, environmental, surveillance and response, physical distancing, or travel); (3) study descriptions: study design and size, research type (quantitative vs qualitative), and measure (feasibility, accessibility or effectiveness); and (4) study detail: brief description of NPIs implemented and extraction of the main findings.
We charted information related to the following key outcomes and their adapted definitions [29, 30]: (1) feasibility—the viability, practicability, or workability of the intervention. How possible or practicable it is to carry it out; (2) acceptability—a multi-faceted construct that reflects the extent to which people delivering or receiving a healthcare intervention consider it to be appropriate, based on anticipated or experienced cognitive and emotional responses to the intervention; (3) effectiveness—the extent to which a specific intervention, when deployed in the usual circumstances of practice, does what it is intended to do for a specified population. Where multiple research types and/or measures were reported in a single article (e.g., a quantitative finding on effectiveness and a qualitative finding on acceptability), data were entered across multiple rows.
Critical appraisal of individual sources of evidence
The quality of the evidence of the included studies was assessed using the National Institutes of Health study quality assessment tool [31], with each rated “good”, “fair”, or “poor”. While this approach accounted for intra-design variability in quality, we also considered inter-design quality, using a rating scheme adapted from Yetley et al. (2016) [32] that ranked study designs from highest to lowest, as follows: controlled intervention study, cohort study, case–control study, pre-post evaluation, cross-sectional study, and case study. These qualitative scores were taken into consideration at the data synthesis stage to help gauge the quality and strength of the evidence.
Synthesis of results
We performed a qualitative synthesis of the findings, according to level of intervention (individual, community, environmental, surveillance and response, physical distancing, or travel), crisis type (conflict, natural disaster, complex emergency, food security crisis, and informal settlement), and shelter type (camp or camp-like, resident, hosted, and informal housing). Findings were grouped by the three key outcome measures (feasibility, acceptability, and effectiveness). We synthesised and summarised identifiable trends and commonalities in the findings and highlighted important gaps and limitations in the published research.
We report our findings according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) statement [33].
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Results
Selection of sources of evidence
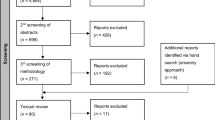
The database search initially identified 8,399 studies, with a further 31 from review articles. After removing duplicates, 4,518 (53.6%) remained, the majority of which (3,972, 87.9%) were excluded at the abstract screening stage for not fitting the inclusion criteria, leaving 546 for full text screening. Of these, 461 (84.4%) were excluded: 242 did not concern an infectious disease or were not in a crisis-affected setting or informal settlement, 129 did not include an NPI, 62 were opinion pieces, the full text was not found for 18, six studies occurred before 1970, and four were unavailable in English, leaving 85 articles for inclusion [34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118] (Fig. 1).
Characteristics of sources of evidence
Characteristics of publications and setting
The volume of research increased over time, with no studies published prior to 1987, just two (2.4%) during the 1980s, eight (9.4%) during the 1990s, approximately one quarter (20, 23.5%) during the subsequent decade, and nearly two-thirds (55, 64.7%) published from 2010 to 2020 (Table 1).
Studies were conducted in 38 countries across the seven World Bank regions, with the majority being in conflict-affected (n = 54, 63.5%) or natural disaster (n = 19, 22.4%) settings (Table 1). Nearly half (n = 39, 45.9%) of the articles were from the sub-Saharan African region. The majority of these studies were in East and Central Africa, with nine from the Democratic Republic of the Congo (DRC) [40, 53, 65, 68,69,70, 76, 109, 111], seven from Sudan/South Sudan [34, 43, 83, 84, 108, 110, 112] and four from Uganda [79, 80, 82, 103]. Almost all (N = 35, 89.7%) of the studies in this region were in conflict-affected settings, with two of the remaining four studies being the sole examples of both food crises [110] and complex emergencies [39] (Fig. 2). South Asia (n = 17, 20.0%), and East Asia and the Pacific (n = 13, 15.3%), accounted for the bulk of the remainder, with fewer than ten studies in each of the remaining regions. Of these, four studies were conducted in the Middle East and North Africa, all in conflict-affected settings; three relating to the Syria conflict [36, 45, 56, 114] and one during a cholera outbreak in Yemen [36]). There was just one study from Europe and Central Asia, during a Norovirus outbreak in a refugee camp in Germany [52]. The four studies in North America all took place in the United States of America (USA), all following natural disasters [47, 54, 62, 67].
Over half of the studies (n = 50, 58.8%) were in camp or camp-like settings (Table 1, Fig. 2), mostly (n = 29, 58.0%) among refugees but with a sizable proportion (n = 20, 40.0%) among internally displaced persons (IDPs). Most of the remaining studies were among crisis-affected resident (n = 16, 18.8%) and informally housed (i.e., slum dwelling) (n = 8, 9.4%) populations. There were just two studies among hosted IDPs [96] and refugees [45] and one study among prisoners of war [104].
Characteristics of research
Approximately one-third of studies focussed on water-borne diseases (n = 52, 32.9%) and vector-borne diseases (n = 46, 29.1%), with roughly one quarter (n = 40, 25.3%) focussed on air-borne and sexually transmitted infections (STIs; Table 2). Ten studies were on blood-borne diseases [all Ebola Virus Disease (EVD) in DRC and Uganda] [68,69,70, 76, 82, 111] and just three on vehicle-borne diseases (tetanus, norovirus, and intestinal parasites) [34, 62, 75].
Approximately one-third of the studies (n = 53, 33.5%) were of community measures, most of which (n = 32) were studies of risk communication and community engagement (RCCE), while the bulk of the remainder were assessments of WASH activities (Fig. 3). Just two studies examined each of physical distancing (both during an EVD outbreak in DRC [68, 69]) and travel-related measures (both of pre-departure screening of refugees on the Thai-Myanmar border migrating to the USA [75, 81]). One quarter of the studies examined each of surveillance and response (n = 42, 26.6%) and individual (n = 38, 24.1%) NPIs. Among the former, most studies (n = 33) investigated active case detection (ACD), while among the latter, half (n = 19) focused on vector protection and a quarter (n = 9) on hand hygiene. Of the 21 studies that explored environmental NPIs, the vast majority explored vector control, with a small number looking at cleaning, disinfection, and waste management.
Assessments of effectiveness accounted for approximately half of the studies (n = 81, 51.3%), three-quarters of which were quantitative and one-quarter qualitative. Feasibility assessments accounted for one third of the studies, while the smallest category of research type was acceptability. Acceptability studies were mostly quantitative (n = 14, 58.3%), while feasibility studies were mostly qualitative (n = 32, 60.4%).
Critical appraisal within sources of evidence
Case studies, the lowest ranking design on the quality rating scale, were the predominant study design (n = 57, 36.1%, Table 2). Cross-sectional studies and “pre-post evaluations” (studies with an ecological design comparing measures of interest before and after the introduction of an intervention but lacking a control group) each made up nearly one quarter of studies (n = 38, 24.1%), The highest-ranked study designs, namely controlled intervention, cohort, and case–control studies, accounted for just one-sixth of included studies (n = 25, 15.8%).
Most feasibility assessments used a case study design (n = 31, 58.5%), while most acceptability assessments were done by cross-sectional survey (n = 13, 54.2%), predominantly household survey or key informant interview (Additional file 1: Figure S1). Effectiveness studies had the greatest variation in study design, with sizable proportions of controlled intervention, pre-post, cross-sectional and case study designs.
Over half the studies were rated “poor” (n = 91, 57.6%), with just one-fifth (n = 29, 18.4%) rating “good” (Table 2). Approximately half of both the acceptability (n = 12, 50%) and effectiveness (n = 38, 46.9%) studies were rated as “poor”, with the remainder evenly split between “good” and “fair” ratings (Additional file 1: Table S2). Feasibility studies fared worse, with over three-quarters (n = 41, 77.4%) rated as “poor” and just 4 (7.5%) achieving a “good” rating, largely due to the reliance on lower-quality case study designs to assess this measure.
Most interventions described were of short (under one year) duration, with a maximum of 12 years (IQR: 0–1, range: 0–12). The median delay between the start of the intervention and publication was three years (but with a very long-tailed distribution of up to 22 years, IQR: 2–4, range: 0–22].
Synthesis of results
The full results of the scoping review are shown in Additional file 1: Table S2, which have been summarised in Table 3 and in the following text.
Environmental measures
Vector control
Studies indicate indoor residual spraying (IRS) is a feasible intervention in complex emergencies [86], refugee camps [38, 58, 92] and post-disaster settings [37, 100]. Important barriers included logistical problems such as absence of roads, remoteness of houses, and insecurity [86, 100]. High coverage has been achieved in refugee settlements, where structured and close settlements facilitate IRS implementation [38].
While few studies assessed the acceptability of IRS, a cross-sectional survey within Afghan refugee settlements in Pakistan reported that incomplete coverage was due to the absence of household decision-makers during implementation [38].
Substantial evidence indicates IRS can (cost-)effectively reduce malaria incidence and mortality in camp and camp-like settings, including in Sudan [43], Pakistan [38, 58, 90, 92] and Myanmar [118]. To ensure effectiveness, insecticide resistance, the timing of IRS implementation and malaria transmission, and the endophily and endophagy of the target vector must be considered [86, 92]. Case-studies suggested that the application of insecticide (IRS, larvicide or fogging) can reduce exposure to a range of mosquito species following extreme weather events [37, 100], though the impact is likely to be location-, intervention-, or vector species-specific [54].
Cleaning, disinfection & waste management
Quantitative evidence of feasibility of cleaning, disinfection and waste management was limited to a single case study of drinking water container disinfection during a shigellosis outbreak in an IDP camp in Sudan, with 88% of containers disinfected within five days [112]. Logistical issues, including stock shortages, have been qualitatively identified as a limiting factor in WASH intervention feasibility within IDP camps [78].
A cross-sectional study conducted during a cholera outbreak in post-earthquake Haiti found high acceptability of household disinfection kits (97.6% uptake) [48]. Qualitative evidence within multiple IDP camps and across various socio-cultural settings indicated concerns regarding the use of chlorine, including fears of poisoning or sterilisation and unfavourable smell which, when combined with ineffective communication, may reduce the acceptability of this NPI [78, 112].
Evidence on the effectiveness of cleaning, disinfection and waste management on infectious disease transmission is highlighted by a case–control study in Dadaab refugee camp, which found that inadequate WASH interventions were associated with increased cholera risk [49].
Community measures
Risk communication
RCCE interventions were found to be highly feasible for communicating risk of cholera [87], hepatitis E [108], malaria [113], and HIV [106]. Sex and age differences were reported, with seeking treatment at health facilities, notifying sexual partners about symptoms, and adopting protective barriers well adopted among men but less among women, highlighting the importance of population-targeted messaging [44].
Effectiveness of RCCE was contextually dependent. Educational campaigns were generally highly effective for STIs. Community sensitisation programmes were associated with increased rates of HIV testing and case detection [80, 87], while education and radio messaging campaigns improved STI risk awareness and behaviour [44, 106, 113]. However, STI education campaigns in Ngara refugee camp, Tanzania, were found to be ineffective, with no apparent impact on sexual behaviour and with STI prevalence increasing over time [72].
WASH RCCE campaigns were largely effective at improving hand-washing behaviour [77], knowledge of prevention strategies [98], and reductions in consumption of unsafe water [50] and water-borne illness morbidity and mortality [50, 63, 74, 85, 107]. Waste disposal education was also associated with reduced latrine blockages in an informal settlement in Dhaka [116]. However, awareness campaigns did not lead to a change in water purification behaviours in Kathmandu [99].
RCCE campaigns, in conjunction with insecticide-treated net (ITN) distribution, were highly effective at improving knowledge on the causes of malaria and correct use of ITNs [88, 103], and education campaigns aimed at improving awareness of dengue led to an increase in knowledge of the disease and vector [35]. Education campaigns for tetanus were found to substantially increase vaccine uptake in a refugee camp in Darfur, Sudan [34]. RCCE was implemented with success for tuberculosis (TB) treatment, reducing default [102] and increasing health seeking behaviour [97].
During an EVD outbreak, a majority of respondents to a qualitative survey believed that RCCE contributed to the response efforts [68], although one study in the same setting reported difficulties in communicating health information due to language barriers, which, once addressed, improved RCCE effectiveness [76]. Language barriers were also reported to have led to community mistrust and decreased effectiveness of cholera outbreak interventions [78].
Water, sanitation, and hygiene (WASH)
Establishing WASH services was often feasible, but financial constraints [36], sustainable maintenance [117], and implementation were important challenges reported [49]. Establishing trust between stakeholders was identified as a key determinant of successful implementation [39].
One study explored the acceptability of WASH interventions in six IDP camps in Borno State, Nigeria [78]. Overcrowding and distance from home caused lack of acceptability of communal latrines, while chlorine use required the mobilisation of trusted members of the community to enhance acceptability.
A programme that complemented WASH interventions with hygiene education led to improvements in household water quality, access to sanitation, and improved hand washing behaviour, associated with reduced diarrhoea incidence among children [77]. WASH interventions were associated with low cholera outbreak case fatality ratio [78]. In a case study post-Tsunami in Indonesia, no major outbreaks of any disease occurred, possibly linked to hygiene interventions [74].
Physical distancing
We identified just two studies exploring physical distancing NPIs, both of which were cross-sectional studies of the acceptability of these measures during an EVD outbreak response in DRC. They reported low acceptability of burial practices that excluded touching the corpse [68, 69] and a willingness to hide suspected Ebola-positive family members from health authorities [68].
Travel measures
We identified just two studies exploring travel measure NPIs, both of which were quantitative effectiveness studies of exit screening of refugees in camps on the Thai-Myanmar border [75, 81]. A case study reported that screening of 15,455 people for TB led to the detection of 272 cases [81], while a pre-post study reported that the introduction of pre-departure screening led to a substantial reduction in helminth infections and associated moderate-to-severe anemia [75].
Surveillance and response measures
Active case detection
ACD for HIV and TB was judged to be both feasible [79, 80, 110] and acceptable [80] in refugee camps in Sudan and Uganda, while ACD of diarrhoeal disease by household visitation and mobile phone surveillance was feasible, but limited by technical issues, lack of treatment follow-up and by poor information sharing and coordination [36, 42]. For case detection of human African trypanosomiasis, passive screening at health facilities was easier to implement than ACD among refugees in South Sudan [83], while widespread ACD among a rural, conflict-affected resident population in the DRC was prevented by conflict and instability [109].
Desire for knowledge of HIV status, peer encouragement, and provision of a "package" (including RCCE and bundling with tests for other diseases) were key to the high acceptability of HIV voluntary counselling and testing (VCT) observed in informal settlements [60, 87]. 'Opt-out' and community-based screening strategies increased access and uptake, particularly among high-risk groups [65, 80, 87]. In a refugee camp in Sudan, refusal of TB screening was associated with a fear of negative consequences of a positive test result, linked to the status of refugees within the host country and lack of trust [110].
ACD contributed to improved TB detection, defaulting rates, and treatment outcomes among TB patients in informal settlements and among refugees [45, 71, 81]. In IDP camps in the Central African Republic, screening for malaria by rapid diagnostic test (RDT) led to a very high percentage (98%) of positive cases receiving appropriate treatment [96]. In a refugee camp in Tanzania, a combined ACD and RCCE approach ensured that most cholera patients arrived in a stable condition, improving their chances of survival [85]. Similarly, a mixed ACD and RCCE programme resulted in more refugees screened and more HIV+ patients detected in a refugee camp in Uganda [79].
Contact tracing
Contact tracing was feasible for the detection and management of an influenza A outbreak in a post-disaster setting in the USA [67]. It was also feasible and effective for TB control among Syrian refugees in Jordan [56] and in an informal settlement in Haiti [71], leading to the identification of additional cases of latent TB.
Case isolation
In conflict-affected settings in Central Africa, isolation of EVD cases was reported to have low acceptability [69], despite reducing mortality and leading to shorter outbreak duration [82]. Case isolation, in combination with other measures including personal hygiene and mask wearing, was found to be effective at reducing the attack rate of influenza A during an outbreak in temporary shelters in Japan [61].
Quarantine
The sole study on quarantining reported that a community-imposed quarantine on household members of an uncooperative EVD case successfully prevented the spread of the disease [82]. Further details were unavailable.
Individual measures
Vector protection
Personal vector protection measures (ITN and mosquito repellent) were reported to be both highly feasible [100] and acceptable [57], with user costs being the only important barrier noted. ITNs were highly effective in reducing malaria infection risk in various settings [91, 93, 95, 118].
Hand hygiene
The feasibility of implementing hand hygiene measures was context-specific, with uptake of measures and a reduction in disease incidence seen in shelters following natural disasters [55] and among refugees displaced by conflict [108]. Conversely, substantial issues with feasibility were observed during a norovirus outbreak in a refugee camp in Germany, owing to a lack of water supply, alcohol-based sanitizer, and language barriers [52]. Acceptability issues due to cultural differences in eating habits were also reported [52]. Hand hygiene, in conjunction with other preventative measures, was found to be effective at reducing the influenza A attack rate during an outbreak in a temporary shelter following the Tōhoku earthquake in 2011 [61], and no infectious disease outbreaks were detected following the 2004 tsunami in Aceh, Indonesia where soap and hygiene kits were distributed [74]. Age-differentiated effectiveness was also reported, with handwashing effective against dysentery among children aged over 5, but not those younger, in an informal settlement in Kolkata [101].
Water purification
Bottled water distribution in a temporary shelter following an earthquake in Sichuan Province, China was feasible in the short term, but sustainability was problematic [117], while water purification and the distribution of improved water containers was highly effective at reducing the occurrence of diarrhoea among refugees in Africa [46, 50, 89].
Condom distribution
Condom distribution had mixed effectiveness, with one study finding a substantial reduction in high-risk sexual behaviours among refugees in Liberia and Sierra Leone [113], while another found no effect on sexual behaviour among Rwandan refugees, with an increase in STIs reported over the intervention period [72].
Face masks
Face mask distribution was found to be feasible, acceptable, and effective when used in conjunction with other control measures aimed at preventing and reducing the spread of Influenza A among populations living in temporary shelters following natural disasters in Japan [55, 61].
Discussion
Summary of evidence
The evidence-base for the feasibility, acceptability, and effectiveness of NPIs in crisis-affected populations and informal settlements was limited for all but a small number of communicable diseases. Most studies were of short duration (typically under 1 year) and produced low-quality evidence due to study design limitations. While this is understandable given the complexity and insecurity of humanitarian emergencies, it remains an important shortcoming of the body of evidence, limiting what can be asserted and the generalisability of the findings, and underscoring the need for more and better-quality research in different contexts.
The research was limited to a narrow range of settings, transmission modes, NPIs, and timespan. Most research was conducted in those parts of sub-Saharan Africa and Asia in which most crisis-affected people live, and the high number of studies in conflict and disaster settings reflects the predominance of these crises. Furthermore, as has been described elsewhere [21], approximately half of the studies were in camp or camp-like settings, despite most crisis-affected populations living in out-of-camp settings. There was scant evidence from informal settlements, which is concerning given the large number of affected people and lack of historical health data [17, 18].
The preponderance of research on water-borne and vector-borne diseases may reflect the types of interventions available and typically implemented by humanitarian relief agencies (e.g., WASH, ITN distribution) and the relative ease of implementing and studying them. However, air-borne diseases remain vastly under-investigated, particularly given their potential for large, highly transmissible epidemics of devastating impact. Such modes of transmission may necessitate novel and difficult-to-implement approaches such as quarantines, travel restrictions, and restrictions of (mass) gatherings of which the feasibility, acceptability, and ultimately the effectiveness are currently poorly documented in crisis-affected populations and informal settlements.
Despite the limited body of evidence, and the large extent to which the evidence was dependent on the context in which the NPIs were implemented, it was possible to identify some common themes that emerged from the scientific literature. Relatively simple and cost-effective interventions, such as community-level environmental cleaning and provision of WASH services, and those that involved the distribution of items for personal protection such as ITNs, were both highly feasible and acceptable, which aided in their effectiveness. The principal barriers with such interventions tended to be logistical, financial, or human resource constraints that impacted access and feasibility, particularly over the long term beyond the acute phase of a crisis. Conversely, resource-intensive individual-level interventions that involve potential restrictions on personal liberty, such as active detection and isolation of cases and contact tracing, were more challenging to implement, and community trust played an extremely important role in their acceptance and success.
The feasibility of implementing of each NPI is greatly affected by resource limitations. While some are difficult to implement in inaccessible and under-supported settings, others are feasible in most, if not all, settings. For example, distributions of ITNs and provision of water purification material is generally relatively feasible in any setting (Table 3). Another important consideration is the trade-off between the infeasibility of any particular intervention and the potential benefits they may bring. For example, although we found very low acceptability of physical distancing in the context of EVD patient care and burial, this is a mainstay of infection prevention and control for a variety of infectious diseases, including EVD and COVID-19. In such cases, careful consideration must be given to approaches for improving the acceptability and adherence to such measures, such as by making the necessary investments in the RCCE complement. Indeed, a general conclusion is that efforts to enhance the RCCE component of NPIs is highly recommended for all NPIs and in all settings (Table 3).
Vertical programmes imposed on communities by external actors have a mixed history of success, and many studies identified low acceptability and poor feasibility in NPI maintenance over the medium- and long-term. An alternative model is increasingly being sought, with humanitarian actors working more closely with communities to implement sustainable programmes with viability over the long-term and complementing development programmes [119]. To support this view, the evidence suggested that many NPIs benefited from incorporating an RCCE component. Regular and meaningful contact with affected communities facilitated feedback loops, which may have helped to identify potential concerns and propose community-led solutions [120]. Moreover, NPIs should be considered in the wider context in which they are implemented, which has the potential to impact all three measures of success. For example, interventions that restrict people’s ability to carry on their regular activities, including work and attending social gatherings, can have severe consequences for their mental and physical well-being. Thorough consideration should be given to mitigate such impacts, such as through providing mental health and psychosocial support and home-care packages that include essential food and non-food items [120].
Limitations
We only included articles published in peer-reviewed journals, but the nature of conducting research in crisis settings, much of which is done as operational research to inform programmes, may result in a substantial wealth of unpublished “grey” literature. The English language restriction further limited the pool of available studies.
The findings are likely to be subject to publication bias, with interventions that were found to be less feasible or effective less likely to be published. It cannot be stressed enough that negative findings should also be published, to avoid “reinventing the wheel”, with subsequent researchers repeating work that was inadequately documented.
Conclusions
The implementation of NPIs poses unique practical constraints in resource-limited settings that need to be considered when planning disease prevention and control programmes. The evidence-base in the peer-reviewed literature on this important theme is scant, occasionally contradictory, and generally low quality. The evidence found through this review revealed major limitations, and cautious interpretation is therefore needed, particularly where the quality of evidence is weakest.
Implementing rigorous, high quality studies in these complex and insecure environments is both logistically and ethically challenging [121,122,123]. However, it is important that guidance on infectious disease prevention and control is rooted in a firm evidence-base, i.e., with high-quality studies. More thought should also be given to how useful lessons can be gathered from studies among stable populations with similar profiles, such as informally housed, crisis-affected resident populations, and refugees and IDPs in protracted crisis settings. Given the substantial resources engaged in protecting populations in emergency situations, basing these on better quality evidence would be a valuable use of resources and should be increasingly considered.
New evidence is beginning to emerge from implementing NPIs in the context of COVID-19, including in crisis-affected populations and informal settings [12, 13, 124,125,126,127,128,129], which is encouraging. However, the evidence base remains limited [20], and we call for further work to be conducted and documented to help us better prepare for current and future infectious diseases outbreaks in these contexts.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- ACD:
-
Active case detection
- DRC:
-
Democratic Republic of the Congo
- EVD:
-
Ebola virus disease
- IRS:
-
Indoor residual spraying
- ITN:
-
Insecticide-treated net
- IDP:
-
Internally displaced person
- NPI:
-
Non-pharmaceutical interventions
- PRISMA-Scr:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews
- RCCE:
-
Risk communication and community engagement
- STI:
-
Sexually transmitted infection
- TB:
-
Tuberculosis
- USA:
-
United States of America
- VCT:
-
Voluntary counselling and testing
- WASH:
-
Water, sanitation and hygiene
References
Peak CM, Childs LM, Grad YH, Buckee CO. Comparing nonpharmaceutical interventions for containing emerging epidemics. Proc Natl Acad Sci USA. 2017;114:4023–8.
WHO Writing Group. Nonpharmaceutical interventions for pandemic influenza, national and community measures. Emerg Infect Dis. 2006;12:88–94.
WHO Writing Group. Nonpharmaceutical interventions for pandemic influenza, international measures. Emerg Infect Dis. 2006;12:81–7.
Fong MW, Gao H, Wong JY, Xiao J, Shiu EYC, Ryu S, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-social distancing measures. Emerg Infect Dis. 2020;26:976–84.
Xiao J, Shiu EYC, Gao H, Wong JY, Fong MW, Ryu S, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-personal protective and environmental measures. Emerg Infect Dis. 2020;26:967–75.
Saunders-Hastings P, Crispo JAG, Sikora L, Krewski D. Effectiveness of personal protective measures in reducing pandemic influenza transmission: a systematic review and meta-analysis. Epidemics. 2017;20:1–20.
Liu Y, Morgenstern C, Kelly J, Lowe R, Munday J, Villabona-Arenas CJ, et al. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC Med. 2021;19:40.
Davies NG, Kucharski AJ, Eggo RM, Gimma A, Edmunds WJ. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health. 2020;5:e375–85.
Flaxman S, Mishra S, Gandy A, Unwin HJT, Mellan TA, Coupland H, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584:257–61.
Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–70.
Hellewell J, Abbott S, Gimma A, Bosse NI, Jarvis CI, Russell TW, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8:e488–96.
Interim Guidance on Scaling-up COVID-19 Outbreak in Readiness and Response Operations in Camps and Camp-like Settings. Inter-Agency Standing Committee; [cited 2021 Mar 24]. https://interagencystandingcommittee.org/other/interim-guidance-scaling-covid-19-outbreak-readiness-and-response-operations-camps-and-camp-settings
Interim Guidance on Public Health and Social Measures for COVID-19 Preparedness and Response Operations in Low Capacity and Humanitarian Settings. Inter-Agency Standing Committee; [cited 2021 May 20]. https://interagencystandingcommittee.org/health/interim-guidance-public-health-and-social-measures-covid-19-preparedness-and-response-operations-low
Cookson R, Doran T, Asaria M, Gupta I, Mujica FP. The inverse care law re-examined: a global perspective. Lancet. 2021;397:828–38.
Global Humanitarian Overview 2020. UN Office for the Coordination of Humanitarian Affairs (OCHA); https://reliefweb.int/sites/reliefweb.int/files/resources/GHO-2020_v9.1.pdf
Garfield RM, Polonsky J, Burkle FM. Changes in size of populations and level of conflict since World War II: implications for health and health services. Disaster Med Public Health Prep. 2012;6:241–6.
Riley LW, Ko AI, Unger A, Reis MG. Slum health: diseases of neglected populations. BMC Int Health Hum Rights. 2007;7:2.
Ezeh A, Oyebode O, Satterthwaite D, Chen Y-F, Ndugwa R, Sartori J, et al. The history, geography, and sociology of slums and the health problems of people who live in slums. Lancet. 2017;389:547–58.
Cheatley J, Vuik S, Devaux M, Scarpetta S, Pearson M, Colombo F, et al. The effectiveness of non-pharmaceutical interventions in containing epidemics: a rapid review of the literature and quantitative assessment. 2020. https://doi.org/10.1101/2020.04.06.20054197.
Enria D, Feng Z, Fretheim A, Ihekweazu C, Ottersen T, Schuchat A, et al. Strengthening the evidence base for decisions on public health and social measures. Bull World Health Organ. 2021;99:610-610A.
Blanchet K, Ramesh A, Frison S, Warren E, Hossain M, Smith J, et al. Evidence on public health interventions in humanitarian crises. Lancet. 2017;390:2287–96.
Charnley GEC, Kelman I, Gaythorpe KAM, Murray KA. Traits and risk factors of post-disaster infectious disease outbreaks: a systematic review. Sci Rep. 2021;11:5616.
Checchi F, Gayer M, Grais RF, Mills EJ. Public health in crisis-affected populations. A practical guide for decision-makers. Overseas Development Institute, London; 2007 [cited 2021 Mar 24]. https://fieldresearch.msf.org/handle/10144/52753
Programme UNHS. The Challenge of Slums: Global Report on Human Settlements, 2003. Earthscan Publications; 2003.
Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza. World Health Organization; https://www.who.int/publications-detail-redirect/non-pharmaceutical-public-health-measuresfor-mitigating-the-risk-and-impact-of-epidemic-and-pandemic-influenza
Aledort JE, Lurie N, Wasserman J, Bozzette SA. Non-pharmaceutical public health interventions for pandemic influenza: an evaluation of the evidence base. BMC Publ Health. 2007;7:208.
Taxonomy and glossary of public health and social measures that may be implemented to limit the spread of COVID-19.. World Health Organization; 2020 [cited 2021 May 21]. https://cdn.who.int/media/docs/default-source/documents/phsm/phsm---taxonomy_95529eca-9133-42e5-8549-daff3b208e97.zip?sfvrsn=7b98572e_16
Covidence systematic review software. Melbourne, Australia: Veritas Health Innovation; www.covidence.org
Porta M. A dictionary of epidemiology. 6th ed. Oxford: Oxford University Press; 2014.
Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17:88.
National Institutes of Health (2014). Study Quality Assessment Tools. [cited 2021 May 21]. Available at https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
Yetley EA, MacFarlane AJ, Greene-Finestone LS, Garza C, Ard JD, Atkinson SA, et al. Options for basing Dietary Reference Intakes (DRIs) on chronic disease endpoints: report from a joint US-/Canadian-sponsored working group. Am J Clin Nutr. 2017;105:249S-285S.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–73.
Adam IF, Nakamura K, Kizuki M, Al Rifai R, Vanching U. Relationship between implementing interpersonal communication and mass education campaigns in emergency settings and use of reproductive healthcare services: evidence from Darfur, Sudan. BMJ Open. 2015;5:e008285.
AhbiRami R, Zuharah WF. School-based health education for dengue control in Kelantan, Malaysia: Impact on knowledge, attitude and practice. PLoS Negl Trop Dis. 2020;14:e0008075.
Altmann M, Suarez-Bustamante M, Soulier C, Lesavre C, Antoine C. First Wave of the 2016–17 Cholera Outbreak in Hodeidah City, Yemen - ACF Experience and Lessons Learned. PLoS Curr. 2017;9:ecurrents.outbreaks.5c338264469fa046ef013e48a71fb1c5.
Aumentado C, Cerro BR, Olobia L, Suy LL, Reyes A, Kusumawathie PHD, et al. The prevention and control of dengue after Typhoon Haiyan. West Pac Surveill Response J WPSAR. 2015;6(Suppl 1):60–5.
Bouma MJ, Parvez SD, Nesbit R, Winkler AM. Malaria control using permethrin applied to tents of nomadic Afghan refugees in northern Pakistan. Bull World Health Organ. 1996;74:413–21.
Brocklehurst C, Malik M, Sebunya K, Salama P. Engineering in the time of cholera: overcoming institutional and political challenges to rebuild Zimbabwe’s water and sanitation infrastructure in the aftermath of the 2008 cholera epidemic. J Water Sanit Hyg Dev. 2013;3:222–9.
Brooks HM, Jean Paul MK, Claude KM, Mocanu V, Hawkes MT. Use and disuse of malaria bed nets in an internally displaced persons camp in the Democratic Republic of the Congo: a mixed-methods study. PLoS ONE. 2017;12:e0185290.
Burns M, Rowland M, N’Guessan R, Carneiro I, Beeche A, Ruiz SS, et al. Insecticide-treated plastic sheeting for emergency malaria prevention and shelter among displaced populations: an observational cohort study in a refugee setting in Sierra Leone. Am J Trop Med Hyg. 2012;87:242–50.
Carstensen LS, Tamason CC, Sultana R, Tulsiani SM, Phelps MD, Gurley ES, et al. The cholera phone: diarrheal disease surveillance by mobile phone in Bangladesh. Am J Trop Med Hyg. 2019;100:510–6.
Charlwood JD, Qassim M, Elnsur EI, Donnelly M, Petrarca V, Billingsley PF, et al. The impact of indoor residual spraying with malathion on malaria in refugee camps in eastern Sudan. Acta Trop. 2001;80:1–8.
Chen MI, von Roenne A, Souare Y, von Roenne F, Ekirapa A, Howard N, et al. Reproductive health for refugees by refugees in Guinea II: sexually transmitted infections. Confl Health. 2008;2:14.
Cookson ST, Abaza H, Clarke KR, Burton A, Sabrah NA, Rumman KA, et al. Impact of and response to increased tuberculosis prevalence among Syrian refugees compared with Jordanian tuberculosis prevalence: case study of a tuberculosis public health strategy. Confl Health. 2015;9:18.
Doocy S, Burnham G. Point-of-use water treatment and diarrhoea reduction in the emergency context: an effectiveness trial in Liberia. Trop Med Int Health. 2006;11:1542–52.
Elledge BL, Boatright DT, Woodson P, Clinkenbeard RE, Brand MW. Learning from Katrina: environmental health observations from the SWCPHP response team in Houston. J Environ Health. 2007;70:22–6.
Gartley M, Valeh P, de Lange R, DiCarlo S, Viscusi A, Lenglet A, et al. Uptake of household disinfection kits as an additional measure in response to a cholera outbreak in urban areas of Haiti. J Water Health. 2013;11:623–8.
Golicha Q, Shetty S, Nasiblov O, Hussein A, Wainaina E, Obonyo M, et al. Cholera outbreak in dadaab refugee camp, Kenya — November 2015–June 2016. MMWR Morb Mortal Wkly Rep. 2018;67:958–61.
Graf J, Zebaze Togouet S, Kemka N, Niyitegeka D, Meierhofer R, Gangoue PJ. Health gains from solar water disinfection (SODIS): evaluation of a water quality intervention in Yaoundé, Cameroon. J Water Health. 2010;8:779–96.
Graham K, Mohammad N, Rehman H, Farhan M, Kamal M, Rowland M. Comparison of three pyrethroid treatments of top-sheets for malaria control in emergencies: entomological and user acceptance studies in an Afghan refugee camp in Pakistan. Med Vet Entomol. 2002;16:199–206.
Grote U, Schleenvoigt BT, Happle C, Dopfer C, Wetzke M, Ahrenstorf G, et al. Norovirus outbreaks in german refugee camps in 2015. Z Für Gastroenterol. 2017;55:997–1003.
Hamze H, Charchuk R, Jean Paul MK, Claude KM, Léon M, Hawkes MT. Lack of household clustering of malaria in a complex humanitarian emergency: implications for active case detection. Pathog Glob Health. 2016;110:223–7.
Harris JW, Richards SL, Anderson A. Emergency mosquito control on a selected area in Eastern North Carolina after hurricane Irene. Environ Health Insights. 2014;8:29–33.
Hatta M, Endo S, Tokuda K, Kunishima H, Arai K, Yano H, et al. Post-tsunami outbreaks of influenza in evacuation centers in Miyagi Prefecture. Japan Clin Infect Dis. 2012;54:e5-7.
Hosten E, Mehta M, Andre E, Abu Rumman K, Van der Linden D. Tuberculosis contact-tracing among Syrian refugee populations: lessons from Jordan. Confl Health. 2018;12:25.
Howard N, Shafi A, Jones C, Rowland M. Malaria control under the Taliban regime: insecticide-treated net purchasing, coverage, and usage among men and women in eastern Afghanistan. Malar J. 2010;9:7.
Howard N, Guinness L, Rowland M, Durrani N, Hansen KS. Cost-effectiveness of adding indoor residual spraying to case management in Afghan refugee settlements in Northwest Pakistan during a prolonged malaria epidemic. PLoS Negl Trop Dis. 2017;11:e0005935.
Husain F, Hardy C, Zekele L, Clatworthy D, Blanton C, Handzel T. A pilot study of a portable hand washing station for recently displaced refugees during an acute emergency in Benishangul-Gumuz Regional State Ethiopia. Confl Health. 2015;9:26.
Kabiru CW, Beguy D, Crichton J, Zulu EM. HIV/AIDS among youth in urban informal (slum) settlements in Kenya: what are the correlates of and motivations for HIV testing? BMC Public Health. 2011;11:685.
Kamigaki T, Seino J, Tohma K, Nukiwa-Soma N, Otani K, Oshitani H. Investigation of an Influenza A (H3N2) outbreak in evacuation centres following the Great East Japan earthquake, 2011. BMC Public Health. 2014;14:34.
Karmarkar E, Jain S, Higa J, Fontenot J, Bertolucci R, Huynh T, et al. Outbreak of Norovirus Illness Among Wildfire Evacuation Shelter Populations — Butte and Glenn Counties, California, November 2018. MMWR Morb Mortal Wkly Rep. 2020;69:613–7.
Khan R, Nguyen TH, Shisler J, Lin L-S, Jutla A, Colwell R. Evaluation of risk of cholera after a natural disaster: lessons learned from the 2015 Nepal earthquake. J Water Resour Plan Manag. 2018;144:04018044.
Kimani EW, Vulule JM, Kuria IW, Mugisha F. Use of insecticide-treated clothes for personal protection against malaria: a community trial. Malar J. 2006;5:63.
Kohli A, Makambo MT, Ramazani P, Zahiga I, Mbika B, Safari O, et al. A Congolese community-based health program for survivors of sexual violence. Confl Health. 2012;6:6.
Lantagne D, Clasen T. Effective use of household water treatment and safe storage in response to the 2010 Haiti earthquake. Am J Trop Med Hyg. 2013;89:426–33.
Liu L, Haynie A, Jin S, Zangeneh A, Bakota E, Hornstein BD, et al. Influenza A (H3) outbreak at a hurricane harvey megashelter in Harris County, Texas: successes and challenges in disease identification and control measure implementation. Disaster Med Public Health Prep. 2019;13:97–101.
Masumbuko Claude KM, Underschultz J, Hawkes MT. Ebola virus epidemic in war-torn eastern DR Congo. Lancet. 2018;392:1399–401.
Masumbuko Claude K, Underschultz J, Hawkes MT. Social resistance drives persistent transmission of Ebola virus disease in Eastern Democratic Republic of Congo: a mixed-methods study. PLoS ONE. 2019;14:e0223104.
Masumbuko Claude K, Hawkes MT. Ebola crisis in Eastern Democratic Republic of Congo: student-led community engagement. Pathog Glob Health. 2020;114:218–23.
Masur J, Koenig SP, Julma P, Ocheretina O, Durán-Mendicuti MA, Fitzgerald DW, et al. Active tuberculosis case finding in Haiti. Am J Trop Med Hyg. 2017;97:433–5.
Mayaud P. The challenge of sexually transmitted infections control for HIV prevention in refugee settings: Rwandan refugees in Tanzania. Trans R Soc Trop Med Hyg. 2001;95:121–4.
McGinn T, Allen K. Improving refugees’ reproductive health through literacy in Guinea. Glob Public Health. 2006;1:229–48.
World Health Organization. Epidemic-prone disease surveillance and response after the tsunami in Aceh Province, Indonesia. Wkly Epidemiol Rec. 2005;80:160–4.
Mitchell T, Lee D, Weinberg M, Phares C, James N, Amornpaisarnloet K, et al. Impact of enhanced health interventions for United States-bound refugees: evaluating best practices in migration health. Am J Trop Med Hyg. 2018;98:920–8.
Mobula LM, Samaha H, Yao M, Gueye AS, Diallo B, Umutoni C, et al. Recommendations for the COVID-19 response at the national level based on lessons learned from the ebola virus disease outbreak in the democratic Republic of the Congo. Am J Trop Med Hyg. 2020;103:12–7.
Moll DM, McElroy RH, Sabogal R, Corrales LF, Gelting RJ. Health impact of water and sanitation infrastructure reconstruction programmes in eight Central American communities affected by Hurricane Mitch. J Water Health. 2007;5:51–65.
Ngwa MC, Wondimagegnehu A, Okudo I, Owili C, Ugochukwu U, Clement P, et al. The multi-sectorial emergency response to a cholera outbreak in Internally Displaced Persons camps in Borno State, Nigeria, 2017. BMJ Glob Health. 2020;5:e002000.
O’Laughlin KN, Kasozi J, Walensky RP, Parker RA, Faustin ZM, Doraiswamy S, et al. Clinic-based routine voluntary HIV testing in a refugee settlement in Uganda. J Acquir Immune Defic Syndr. 1999;2014(67):409–13.
O’Laughlin KN, He W, Greenwald KE, Kasozi J, Chang Y, Mulogo E, et al. Feasibility and acceptability of home-based HIV testing among refugees: a pilot study in Nakivale refugee settlement in southwestern Uganda. BMC Infect Dis. 2018;18:332.
Oeltmann JE, Varma JK, Ortega L, Liu Y, O’Rourke T, Cano M, et al. Multidrug-resistant tuberculosis outbreak among US-bound Hmong refugees, Thailand, 2005. Emerg Infect Dis. 2008;14:1715–21.
Okware SI, Omaswa F, Talisuna A, Amandua J, Amone J, Onek P, et al. Managing Ebola from rural to urban slum settings: experiences from Uganda. Afr Health Sci. 2015;15:312–21.
Palmer JJ, Kelly AH, Surur EI, Checchi F, Jones C. Changing landscapes, changing practice: negotiating access to sleeping sickness services in a post-conflict society. Soc Sci Med. 1982;2014(120):396–404.
Phillips RM, Vujcic J, Boscoe A, Handzel T, Aninyasi M, Cookson ST, et al. Soap is not enough: handwashing practices and knowledge in refugee camps, Maban County, South Sudan. Confl Health. 2015;9:39.
Plummer M. Community health for Rwandan refugees. Can Nurse. 1995;91:45–6.
Protopopoff N, Van Herp M, Maes P, Reid T, Baza D, D’Alessandro U, et al. Vector control in a malaria epidemic occurring within a complex emergency situation in Burundi: a case study. Malar J. 2007;6:93.
Reif LK, Rivera V, Louis B, Bertrand R, Peck M, Anglade B, et al. Community-based HIV and health testing for high-risk adolescents and youth. AIDS Patient Care STDs. 2016;30:371–8.
Richards AK, Banek K, Mullany LC, Lee CI, Smith L, Oo EKS, et al. Cross-border malaria control for internally displaced persons: observational results from a pilot programme in eastern Burma/Myanmar. Trop Med Int Health. 2009;14:512–21.
Roberts L, Chartier Y, Chartier O, Malenga G, Toole M, Rodka H. Keeping clean water clean in a Malawi refugee camp: a randomized intervention trial. Bull World Health Organ. 2001;79:280–7.
Rowland M, Hewitt S, Durrani N. Prevalence of malaria in Afghan refugee villages in Pakistan sprayed with lambdacyhalothrin or malathion. Trans R Soc Trop Med Hyg. 1994;88:378–9.
Rowland M, Bouma M, Ducornez D, Durrani N, Rozendaal J, Schapira A, et al. Pyrethroid-impregnated bed nets for personal protection against malaria for Afghan refugees. Trans R Soc Trop Med Hyg. 1996;90:357–61.
Rowland M, Hewitt S, Durrani N, Bano N, Wirtz R. Transmission and control of vivax malaria in Afghan refugee settlements in Pakistan. Trans R Soc Trop Med Hyg. 1997;91:252–5.
Rowland M, Hewitt S, Durrani N, Saleh P, Bouma M, Sondorp E. Sustainability of pyrethroid-impregnated bednets for malaria control in Afghan communities. Bull World Health Organ. 1997;75:23–9.
Rowland M, Durrani N, Hewitt S, Mohammed N, Bouma M, Carneiro I, et al. Permethrin-treated chaddars and top-sheets: Appropriate technology for protection against malaria in Afghanistan and other complex emergencies. Trans R Soc Trop Med Hyg. 1999;93:465–72.
Rowland M, Downey G, Rab A, Freeman T, Mohammad N, Rehman H, et al. DEET mosquito repellent provides personal protection against malaria: a household randomized trial in an Afghan refugee camp in Pakistan. Trop Med Int Health. 2004;9:335–42.
Ruckstuhl L, Lengeler C, Moyen JM, Garro H, Allan R. Malaria case management by community health workers in the Central African Republic from 2009–2014: overcoming challenges of access and instability due to conflict. Malar J. 2017;16:388.
Samal J, Dehury RK. Impact of a structured tuberculosis awareness strategy on the knowledge and behaviour of the families in a slum area in Chhattisgarh, India. J Clin Diagn Res JCDR. 2017;11:11–5.
Scobie HM, Phares CR, Wannemuehler KA, Nyangoma E, Taylor EM, Fulton A, et al. Use of oral cholera vaccine and knowledge, attitudes, and practices regarding safe water, sanitation and hygiene in a long-standing refugee camp, Thailand, 2012–2014. PLoS Negl Trop Dis. 2016;10:e0005210.
Sekine K, Roskosky M. Emergency response in water, sanitation and hygiene to control cholera in post-earthquake Nepal in 2016. J Water Sanit Hyg Dev J Int Water Assoc. 2018;8:799–802.
Shortus M, Musto J, Bugoro H, Butafa C, Sio A, Joshua C. Vector-control response in a post-flood disaster setting, Honiara, Solomon Islands, 2014. West Pac Surveill Response J WPSAR. 2016;7:38–43.
Sircar BK, Sengupta PG, Mondal SK, Gupta DN, Saha NC, Ghosh S, et al. Effect of handwashing on the incidence of diarrhoea in a Calcutta slum. J Diarrhoeal Dis Res. 1987;5:112–4.
Soares ECC, Vollmer WM, Cavalcante SC, Pacheco AG, Saraceni V, Silva JS, et al. Tuberculosis control in a socially vulnerable area: a community intervention beyond DOT in a Brazilian favela. Int J Tuberc Lung Dis. 2013;17:1581–6.
Spencer S, Grant AD, Piola P, Tukpo K, Okia M, Garcia M, et al. Malaria in camps for internally-displaced persons in Uganda: evaluation of an insecticide-treated bednet distribution programme. Trans R Soc Trop Med Hyg. 2004;98:719–27.
Sundnes KO, Haimanot AT. Epidemic of louse-borne relapsing fever in Ethiopia. Lancet. 1993;342:1213–5.
Takahashi K, Kodama M, Kanda H. Call for action for setting up an infectious disease control action plan for disaster area activities: learning from the experience of checking suffering volunteers in the field after the Great East Japan Earthquake. Biosci Trends. 2013;7:294–5.
Tanaka Y, Kunii O, Hatano T, Wakai S. Knowledge, attitude, and practice (KAP) of HIV prevention and HIV infection risks among Congolese refugees in Tanzania. Health Place. 2008;14:434–52.
Tappero JW, Tauxe RV. Lessons learned during public health response to cholera epidemic in Haiti and the Dominican Republic. Emerg Infect Dis. 2011;17:2087–93.
Thomson K, Luis DJ, Lagu J, Laku R, Dineen B, Schilperoord M, et al. Investigation of hepatitis E outbreak among refugees—Upper Nile, South Sudan, 2012–2013. MMWR Morb Mortal Wkly Rep. 2013;62:581–6.
Tong J, Valverde O, Mahoudeau C, Yun O, Chappuis F. Challenges of controlling sleeping sickness in areas of violent conflict: experience in the Democratic Republic of Congo. Confl Health. 2011;5:7.
Toscani L, Richard M. Tuberculosis in a Refugee Camp: A campaign to reduce transmission. Disasters. 1988;12:259–73.
Vinck P, Pham PN, Bindu KK, Bedford J, Nilles EJ. Institutional trust and misinformation in the response to the 2018–19 Ebola outbreak in North Kivu, DR Congo: a population-based survey. Lancet Infect Dis. 2019;19:529–36.
Walden VM, Lamond E-A, Field SA. Container contamination as a possible source of a diarrhoea outbreak in Abou Shouk camp, Darfur province, Sudan. Disasters. 2005;29:213–21.
Woodward A, Howard N, Souare Y, Kollie S, von Roenne A, Borchert M. Reproductive health for refugees by refugees in Guinea IV: Peer education and HIV knowledge, attitudes, and reported practices. Confl Health. 2011;5:10.
HeRAMS Summary Report. Syrian Arab Republic. Quarter 1, 2015. World Health Organization; 2015. https://applications.emro.who.int/docs/COPub_SYR_1st_Q_health_centres_2015_EN_16718.pdf?ua=1&ua=1
Yamada S, Gunatilake RP, Roytman TM, Gunatilake S, Fernando T, Fernando L. The Sri Lanka tsunami experience. Disaster Manag Response. 2006;4:38–48.
Yeasmin F, Luby SP, Saxton RE, Nizame FA, Alam M-U, Dutta NC, et al. Piloting a low-cost hardware intervention to reduce improper disposal of solid waste in communal toilets in low-income settlements in Dhaka Bangladesh. BMC Public Health. 2017;17:682.
Zeng G. Investigation and recommendations concerning prevention and treatment of infectious diseases and promotion of hygiene in earthquake-stricken areas. J Evid-Based Med. 2008;1:2–8.
Zhao Y, Zeng J, Zhao Y, Liu Q, He Y, Zhang J, et al. Risk factors for asymptomatic malaria infections from seasonal cross-sectional surveys along the China-Myanmar border. Malar J. 2018;17:247.
Rass E, Lokot M, Brown FL, Fuhr DC, Asmar MK, Smith J, et al. Participation by conflict-affected and forcibly displaced communities in humanitarian healthcare responses: a systematic review. J Migr Health. 2020;12:100026.
Integrated Response Framework for Isolation and Quarantine as Non-Pharmaceutical Interventions Against COVID-19. READY: Global Readiness For Major Disease Outbreak Response; 2021 Mar. https://www.ready-initiative.org/integrated-framework/
Black R. Ethical codes in humanitarian emergencies: from practice to research? Disasters. 2003;27:95–108.
National Research Council (US) Roundtable on the Demography of Forced Migration. Research Ethics in Complex Humanitarian Emergencies: Summary of a Workshop. Washington (DC): National Academies Press (US); 2002 [cited 2021 May 21]. http://www.ncbi.nlm.nih.gov/books/NBK220907/
Bruno W, Haar RJ. A systematic literature review of the ethics of conducting research in the humanitarian setting. Confl Health. 2020;14:27.
Ramalingam B, Singh NS, Mahieu A, Blanchet K. Responding to COVID-19: Guidance for humanitarian agencies. 2020 [cited 2021 Mar 24]. https://covid19.alnap.org/help-library/responding-to-covid-19-guidance-for-humanitarian-agencies
Dahab M, van Zandvoort K, Flasche S, Warsame A, Ratnayake R, Favas C, et al. COVID-19 control in low-income settings and displaced populations: what can realistically be done? Confl Health. 2020;14:54.
Singh NS, Abrahim O, Altare C, Blanchet K, Favas C, Odlum A, et al. COVID-19 in humanitarian settings: documenting and sharing context-specific programmatic experiences. Confl Health. 2020;14:79.
Alawa J, Alawa N, Coutts A, Sullivan R, Khoshnood K, Fouad FM. Addressing COVID-19 in humanitarian settings: a call to action. Confl Health. 2020;14:64.
Carter SE, Gobat N, Pfaffmann Zambruni J, Bedford J, van Kleef E, Jombart T, et al. What questions we should be asking about COVID-19 in humanitarian settings: perspectives from the Social Sciences Analysis Cell in the Democratic Republic of the Congo. BMJ Glob Health. 2020;5:e003607.
COVID-19 Humanitarian Platform. [cited 2021 May 20]. https://www.covid19humanitarian.com/
Acknowledgements
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Funding
SB, KF, AH, JS and IJS acknowledge funding from the MRC Centre for Global Infectious Disease 514 Analysis (reference MR/R015600/1), jointly funded by the UK Medical Research Council 515 (MRC) and the UK Foreign, Commonwealth & Development Office (FCDO), under the 516 MRC/FCDO Concordat agreement and is also part of the EDCTP2 programme supported 517 by the European Union. SB acknowledges funding from the Wellcome Trust (219415). JS acknowledges funding from the Wellcome Trust (grant reference: 215163/Z/18/Z). IJS was supported by the QMEE CDT, funded by NERC grant number NE/P012345/1. The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
JAP and AH conceived of the study. JAP, AH, LK, KB and PS provided conceptual ideas and outline, and supervised the study. JAP, SB, KF, AH, JS, IS conducted the scoping review, scored the studies, and charted the data. SH, LK, CL, KB and PS provided strategic direction, technical oversight, and guidance for interpretation of the findings. JAP wrote the original draft, with support from SB, KF, AH, JS and IS. Substantial review and editing for content was provided by SB, KF, AH, JS, IS, SH, LK, CL, KB and PS. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not required.
Competing interests
The authors declare that they have no competing interests.
Supplementary Information
Additional File 1: Table S1.
Article inclusion and exclusion criteria for scoping review. Figure S1. Heatmap of study volume by measure and design. Table S2. Summary information from 158 research studies (from 85 published research articles) included for data charting.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Polonsky, J.A., Bhatia, S., Fraser, K. et al. Feasibility, acceptability, and effectiveness of non-pharmaceutical interventions against infectious diseases among crisis-affected populations: a scoping review. Infect Dis Poverty 11, 14 (2022). https://doi.org/10.1186/s40249-022-00935-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-022-00935-7