Abstract
Background
Artemisinin-based combination treatments (ACTs) are the first-line treatments of uncomplicated Plasmodium falciparum malaria in many endemic areas but there are few evaluation of their efficacy in anaemic malarious children.
Methods
Therapeutic efficacy of 3-day regimens of artesunate-amodiaquine and artemether-lumefantrine was evaluated in 437 anaemic and 909 non-anaemic malarious children following treatment during a seven-year period (2008–2014). Patterns of temporal changes in haematocrit were classified based on haematocrit values <30% and ≥30%. Kinetics of the disposition of the deficit in haematocrit from 30% following treatment were evaluated using a non-compartment model.
Results
PCR-corrected parasitological efficacy 28 days after start of treatment was significantly higher in artesunate-amodiaquine- compared to artemether-lumefantrine-treated children [97% (95%CI: 92.8–100) versus 96.4% (95%CI: 91.3–99.4), P = 0.02], but it was similar in non-anaemic and anaemic children. Fall in haematocrit/1 000 asexual parasites cleared from peripheral blood was significantly greater at lower compared to higher parasitaemias (P < 0.0001), and in non-anaemic compared to anaemic children (P = 0.007). In anaemic children at presentation, mean anaemia recovery time (AnRT) was 15.4 days (95%CI: 13.3–17.4) and it did not change over the years. Declines in haematocrit deficits from 30% were monoexponential with mean estimated half-time of 1.4 days (95%CI: 1.2–1.6). Anaemia half-time (t½anaemia) correlated positively with AnRT in the same patients (r = 0.69, P < 0.0001). Bland-Altman analysis of 10 multiples of t½anaemia and AnRT showed narrow limit of agreement with insignificant bias (P = 0.07) suggesting both can be used interchangeably in the same patients.
Conclusions
Artesunate-amodiaquine and artemether-lumefantrine remain efficacious treatments of uncomplicated P. falciparum infections in non-anaemic and anaemic Nigerian children in the last 7 years of adoption as first-line treatments. These ACTs may also conserve haematocrit at high parasitaemias and in anaemic children.
Trials registration
Pan African Clinical Trial Registry PACTR201508001188143, 3 July 2015; PACTR201510001189370, 3 July 2015; PACTR201508001191898, 7 July 2015 and PACTR201508001193368, 8 July 2015.
Similar content being viewed by others
Multilingual abstracts
Please see Additional file 1 for translations of the abstract into the six official working languages of the United Nations.
Background
Recommended as the first-line treatments of uncomplicated Plasmodium falciparum malaria globally [1], artemisinin-based combination treatments (ACTs) have remained largely efficacious globally except in the Greater Mekong subregion where artemisinin resistance in P. falciparum has recently emerged [2–7]. Not only do these drug combinations clear asexual and immature sexual parasitaemia rapidly and prevent progression of committed and non-committed asexual parasites to sexual forms, they may also prevent destruction of once-parasitized (once-infected) red blood cells through a splenic process called “pitting”. Pitting removes the dead parasites from parasitized red blood cells and returns the once-infected red blood cells into circulation [8–10]. This process prevents precipitous falls in haematocrit in the first few days following ACTs particularly when parasitaemias are high. In severe malaria, pitting is a life-saving process [10].
It has been suggested that in resource-poor endemic countries, the degree of precipitous falls in haematocrit following ACTs can be measured by estimating the fall in haematocrit per 1 000 red blood cells cleared from peripheral blood in the first two days following treatment [11]. The relatively little or no fall in baseline (pre-treatment) haematocrit in the first few days following treatment, particularly when parasitaemias are high, has been termed “haematocrit conservation” [11].
In many endemic and non-endemic areas of the world, anaemia is an inevitable consequence of untreated P. falciparum infections. Anaemia may occur in 10 – 90% of children or non-immune individuals presenting with acute infections [12–18]. Malaria-associated anaemia contributes significantly to morbidity or mortality in P. falciparum malaria [19–25]. Despite the frequent occurrence of malaria-associated anaemia in children living in endemic areas, the efficacy of artemisinin-based combination treatments and the adverse events following their use have been little evaluated in anaemic children with uncomplicated P. falciparum infections.
It has recently been reported that intravenous artesunate treatment may cause delayed haemolysis in immunologically naïve patients with severe malaria [10, 26–31]. However, it is unclear if artemisinin-based combination treatments conserve haematocrit in anaemic children following treatment of uncomplicated P. falciparum infections. It is also unclear if the conserved haematocrit is subsequently lost resulting in a late-appearing anaemia in children with uncomplicated infections.
In Nigeria, artemether-lumefantrine and artesunate-amodiaquine, in that order, were adopted as first-line treatments of uncomplicated P. falciparum malaria in 2005 [32]. Both ACTs have been evaluated, using standardised protocols, more or less continuously at one of seven sentinel sites set up by Nigeria’s Federal Ministry of Health in six geographical areas of Nigeria. These sentinel sites were set up to monitor the efficacy of antimalarial drugs. There is no reported study, in Nigerian children, of the efficacy of artemether-lumefantrine and artesunate-amodiaquine in the last seven years of their adoption as first-line treatments.
The aims of the present study during a 7-year period of adoption are: (i) to evaluate the efficacy of artesunate-amodiaquine and artemether-lumefantrine in uncomplicated P. falciparum malaria, (ii) to determine if efficacy of artesunate-amodiaquine and artemether-lumefantrine differs between malarious anaemic and malarious non-anaemic children, and if ACTs conserve haematocrit in anaemic children, (iii) to evaluate recovery from malaria-associated anaemia, and (iv) to elucidate the temporal changes in haematocrit following treatment with artesunate-amodiaquine and artemether-lumefantrine in anaemic malarious children.
Methods
Study locations
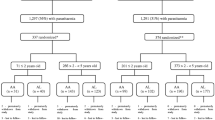
The studies were part of a programme to monitor antimalaria therapeutic efficacy at seven sentinel sites located in six geographical areas of Nigeria (Fig. 1). These sites were established by Nigeria’s Federal Ministry of Health. These studies were conducted between October 2009 and November 2010 at the following locations: Agbani, Ikot Ansa, Barkin Ladi and Damboa, in Enugu, Cross River, Plateau and Borno States, respectively (the eastern flank of the study sites), and in Ijede, and Makarfi in Lagos, and Kaduna States, respectively (the western flank). The studies were also conducted continuously in Sabo quarters of Ibadan, Oyo State (the reference centre), located on the western flank from 2008 to 2014 (Fig. 1). In virtually all study locations, malaria is endemic and transmission occurs all year round; however, it is more intense during the rainy season from April to October. P. falciparum is the predominant species, accounting for over 98% of all infections [33, 34]. Children are more affected than adults, and apparently, asymptomatic infections occur in older school children and adults [33]. The overall study profile is shown in Fig. 2.
Study profile. AA, artesunate-amodiaquine; AL, artemether-lumefantrine, * follow-up was for 42 days, ** follow-up was for 28 days, *** randomization at a ratio of 2:1 for artesunate-amodiaquine and artemether-lumefantrine, # number of children that completed follow-up period, ^ children are <5 years old.
Study procedures
Standardised procedures and protocol were used at all sentinel sites [35–40]. Briefly, patients were eligible to participate in the study if they were: aged 6 months–15 years, had symptoms compatible with acute uncomplicated malaria with P. falciparum mono-infections ≥1 000 μL−1 of blood, no history of antimalarial drug ingestion in the two weeks prior to enrolment, absence of severe malaria and written informed consent given by parents or guardians.
Enrolled patients were randomized to receive artemether-lumefantrine or artesunate-amodiaquine (co-formulated) for 3 days (days 0–2) as previously described [35, 40]. The day of presentation (day of starting treatment) was regarded as day 0. Thick and thin blood films were obtained from each child as soon as they came to the clinic and the slides were carefully labelled with the patients’ codes and air-dried before being stained. Follow-up with clinical and parasitological evaluation was done daily on days 1–3 and on days 7, 14, 21, 28 at all study sites except in Ibadan where additional follow-up was done on days 35 and 42. Parasitaemia, asexual or sexual, in thick films was estimated by counting asexual and sexual parasites relative to 500 leukocytes, or 500 asexual or sexual forms whichever occurred first. From this figure, the parasite density was calculated assuming a leukocyte count of 6 000 μL−1 of blood [41–43]. Sexual parasitaemia was estimated only in Ibadan, but their presence or absence was recorded at other sites. A slide was considered asexual parasite negative if no asexual parasite was detected after examination of 200 microscope fields.
The cure rates on days 28 and 42 were adjusted on the basis of the polymerase chain reaction (PCR) genotyping results of paired samples of patients with recurrent parasitaemia after day 7 of starting treatment using the World Health Organisation 2003 and 2009 protocols [44, 45] as previously described [35–38]. The clinical classification system consisted of the following categories of response: adequate clinical and parasitological response (ACPR), late parasitological failure (LPF), late clinical failure (LCF), early treatment failure (ETF). The primary outcomes were the 28-day uncorrected and PCR-corrected efficacy. Asexual parasite reduction ratio (PRR) [46] was defined as the ratio of day 0/day 2 parasitaemia (and for convenience, referred to as PRRD2). If there was complete clearance of parasitaemia on day 2, parasitaemia was assumed to be 1 uL−1, a level below microscopic detection. Asexual parasite reduction ratio on day 1 (PRRD1) was defined as the ratio of day 0/day 1 parasitaemia. If there was complete clearance of parasitaemia on day 1, parasitaemia was assumed to be 1 uL−1, a level below microscopic detection.
Haematological evaluation
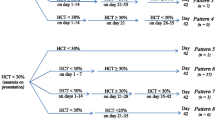
Capillary blood collected before and during follow-up was used to measure haematocrit using a microhaematocrit tube and microcentrifuge (Hawksley, Lancing, UK). Anaemia was defined as a haematocrit <30% and was classified as mild, moderate or severe if haematocrit was 21-29%, 15-20% or <15%, respectively. Anaemia recovery time (in anaemic patients) was defined as time elapsing from drug administration to attainment of a haematocrit value ≥30% and was evaluated in children with haematocrit ≤25% at presentation. In patients who had early or late monophasic declines in haematocrit which resulted in anaemia, anaemia recovery time was defined as time from appearance of, to recovery from, anaemia. Fall in haematocrit per 1 000 asexual parasites cleared from peripheral blood following treatment (FIH/1 000 asexual parasites cpb) was defined as numeric estimation of relative difference in haematocrit at baseline (pre-treatment) and the first 1 or 2 days after treatment began as numerator, and the corresponding relative difference in parasitaemia as the denominator, and expressing it per 1 000 asexual parasites cleared from peripheral blood \( \left[\frac{FIH}{1000} asexual\kern0.5em parasite\kern0.5em cpb\kern0.5em =\kern0.5em \frac{Haematocrit\kern0.5em on\kern0.5em day\kern0.5em 0- Haematocrit\kern0.5em on\kern0.5em day\kern0.5em 1\kern0.5em or\kern0.5em 2}{Parasitaemia\kern0.5em on\kern0.5em day\kern0.5em 0- Parasitaemia\kern0.5em on\kern0.5em day\kern0.5em 1\kern0.5em or\kern0.5em 2}\times 1000\right] \) [11]. Fig. 3 is the profile of investigations carried out during the study.
Profile of investigations carried out. PRRD1, parasite reduction ratio 1 day after treatment began; PRRD2, parasite reduction ratio 2 days after treatment began; PCT, parasite clearance time; FCT, fever clearance time; FIH, fall in haematocrit per 1 000 asexual parasites cleared from peripheral blood; PD, pharmacodynamic measure of recovery (anaemia recovery time); PK, pharmacokinetic measure of recovery (anaemia half-time); AA, artesunate-amodiaquine; AL, artemether-lumefantrine
Evaluation of temporal changes in haematocrit in anaemic children following treatment
Haematocrit <30% and ≥30% were the reference points in all classified patterns and was modified from a recently described patterns [47]. Temporal changes in haematocrit were classified into the following patterns.
-
1.
Haematocrit <30% before treatment followed by an increase to ≥30% after treatment (malaria-associated anaemia at presentation and recovery from anaemia).
-
2.
Haematocrit <30% followed by a rise to ≥30% by day 7, a fall to <30% between days 7 and 14 and then recovery (anaemia–early recovery–anaemia–late recovery).
-
3.
Haematocrit <30% followed by a rise to ≥30% on day 7 or 14, followed by two consecutive normal haematocrits and decline to <30% after day 14 (anaemia–early recovery–late-appearing anaemia pattern).
-
4.
Haematocrit <30% before treatment began and during the entire follow-up period (persistent, unresolved anaemia).
-
5.
Multiple falls in haematocrit below 30%, a rise to ≥30% during follow-up period and then a fall below 30% (undulating pattern of anaemia).
-
6.
Unclassifiable.
In non-anaemic patients (n = 568), evaluation of temporal changes was limited to those who had falls in haematocrit to anaemic level 3–6 weeks after commencement of treatment as previously described [47].
Kinetics of the disposition of deficit in haematocrit from 30%
The kinetics of the disposition of deficit in haematocrit from 30%, that is, of anaemia, was as previously described [35, 37, 47]. Briefly, in all anaemic patients with a haematocrit value ≤25% at enrolment, or when anaemia occurs following treatment, haematocrit values below 30% (the lower threshold of normal) and at follow-up were subtracted from 30% at each time of measurement until haematocrit rose to ≥30%, and the resulting values plotted against time. The final haematocrit when anaemia resolved was therefore zero in all patients. However, the final haematocrit at the time of resolution or recovery was assumed to be 0.01%. The areas under the curve (AUC) of deficit in haematocrit (from 30%) versus time were obtained, by trapezoidal rule using the computer program Turbo Ken (designed by Clinical Pharmacology Group, University of Southampton, United Kingdom) as previously described [35, 37]. AUC was also obtained manually by calculating the average haematocrit values between two consecutive time measurements and multiplying it by the time interval between the measurements, and summing up all the values, in a manner similar to that for the numerical estimation of area under a drug concentration-time curve [48]. The unit of quantification would be %.d, if haematocrit values were used or g/L.d if haemoglobin values were used. Haematocrit values may be converted to haemoglobin values by dividing by 3 [49]. Semilog plots of deficit in haematocrit versus time were plotted. The apparent terminal elimination rate constant (λ) was obtained by least-square regression analysis of the post-peak log-linear part of the plot of deficit in haematocrit (from 30%) versus time, and the apparent terminal half-time of anaemia (t1/2(anaemia)) was calculated from ln 2/(λ) (that is, λt = 0.693).
Statistical analysis
Data were analysed using version 6 of Epi-Info software [50] and the statistical program SPSS for Windows version 20.0 [51]. Variables considered in the analysis were related to the densities of P. falciparum asexual and sexual forms. Proportions were compared by calculating χ 2 using Yates’ correction, Fisher’s exact or Mantel Haenszel tests. Normally distributed, continuous data were compared by Student’s t test and analysis of variance (ANOVA). Data not conforming to a normal distribution were compared by the Mann–Whitney U tests and the Kruskal Wallis tests (or by Wilcoxon ranked sum test). The cumulative risk of parasite reappearance was calculated by survival analysis using Kaplan-Meier method. Correlation between anaemia recovery time and anaemia half-time in the same patients was assessed by Pearson’s correlation coefficient. Agreement between multiples of anaemia half-time (proposed pharmacokinetic method of assessing response to treatment) and anaemia recovery time (standard pharmacodynamic method of assessing response to treatment) in the same patients was assessed by Bland-Altman analysis [52]. Impacts of treatments over time were evaluated using test for trend for the following parameters: parasitological efficacy, late parasitological failure and gametocyte carriage, and by comparison of mean or median at specific time intervals for the following parameters: parasite reduction ratios 1 or 2 days after treatment began, parasite clearance time, fever clearance time, median FIH/1 000 asexual parasite cpb and anaemia recovery time. P values of <0.05 were taken to indicate significant differences. Data were double entered serially using patients’ codes and were only analysed at the end of the study.
Ethical clearance
The study protocol was approved by the Ministry of Health, Ibadan, and the National Health Research Ethics Committee, Abuja, Nigeria. The reference numbers are: Ministry of Health Ibadan - AD 13/262/56 (7 March 2006), AD 13/479/978 (December 2015); National Health Research Ethics Committee - NHREC/01/01/2007-28/10/2009d (30 October 2009), NHREC/01/01/2007-28/10/2013 (29 October 2013), NHREC/01/01/2007-22/10/2014 (30 October 2014). Written informed consents were obtained from parents/guardians of the children.
Results
Patient characteristics at enrolment
During the study period, 1 346 children of which 437 children (32%) who were anaemic at presentation were included in the present study (Fig. 3). A total of 829 and 517 children were treated with artesunate-amodiaquine and artemether-lumefantrine, respectively. Of the 437 anaemic children, anaemia was mild, moderate or severe in 395 (90.4%), 40 (9.1%) or 2 (0.5%) children, respectively. Overall, the mean age of these children was 5.3 years (95%CI: 5.1-5.5, range 0.5-15). The clinical and parasitological characteristics of these children are summarised in Table 1. Overall (see All treatments section in Table 1), children with anaemia were significantly younger, had significantly longer duration of illness and a significantly lower enrolment parasitaemia.
Therapeutic responses
Primary outcomes
Parasitological efficacy
Overall, during the 7-year period, parasitological efficacy (ACPR) on day 28 with both treatments was 96.5% (95%CI: 91.8-100) and it increased significantly with time over the study period [94.6% (95%CI: 84.1-100) versus 98.8% (95%CI: 84.0-100) P = 0.007 test for trend, in 2008–2010 and 2011–2014, respectively]. Overall, parasitological efficacy on day 28 was significantly higher in children treated with artesunate-amodiaquine compared with children treated with artemether-lumefantrine [97% (95%CI: 92.8-100) versus 96.4% (95%CI: 91.3-99.4); P = 0.02)]. The significant increase in parasitological efficacy over the years involved both artesunate-amodiaquine and artemether-lumefantrine and both anaemic and non-anaemic children (data not shown).
Overall, parasitological efficacy was similar in anaemic and non-anaemic children (97.5% (95%CI: 92.4-100) versus 96.1% (95%CI: 91.2-100), P = 0.3, respectively). In children treated with artesunate-amodiaquine, PCR-uncorrected and corrected parasitological efficacy were similar in anaemic and non-anaemic children at all study sites (Table 2). Similarly, in children treated with artemether-lumefantrine, PCR-uncorrected and corrected parasitological efficacy were similar in anaemic and non-anaemic children at all sites (Table 2).
Overall, early treatment failure (ETF) occurred in 1 child treated with artesunate-amodiaquine. Late parasitological failure (LPF) occurred in 71 children: 37 of 818 children treated with artesunate-amodiaquine and 34 of 505 children treated with artemether-lumefantrine. There was no significant difference in the proportions of children with late parasitological failure in the two treatment groups (P = 0.11). There was also no significant difference in the proportions of children with late parasitological failure in anaemic and non-anaemic groups: 28 of 429 anaemic children versus 43 of 894 non-anaemic children (P = 0.24). The proportions of children with late parasitological failure did not increase over the years: 63 of 1 105 in 2008–2010 versus 8 of 218 in 2011–2014 (P = 0.12 test for trend).
Recrudescent and new infections
Parasitaemia was detectable in 84 children before day 28–42. Of these, 17 were new infections, 57 were recrudescent infections of P. falciparum and in 10 cases, PCR results were inconclusive. Of the recrudescent infections, 27 were in children treated with artesunate-amodiaquine and 30 were in children treated with artemether-lumefantrine. The proportion of children with recrudescent infections was significantly higher in artemether-lumefantrine-treated group than in artesunate-amodiaquine-treated group (P = 0.03). However, there was no significant difference in the proportions of children with recrudescent infections in anaemic and non-anaemic children (16 of 437 versus 41 of 909, P = 0.56). Median time to recrudescent infections was similar in artesunate-amodiaquine- and artemether-lumefantrine - treated children (28 days (range 14–42) versus 28 days (range 11–42), P = 0.9). Similarly, time to recrudescent infections was similar in anaemic and non-anaemic children (28 days (range 14–42) versus 28 days (range 11–42), P = 0.94). Overall, the probabilities of reappearance of asexual parasitaemia after treatment were significantly higher with artemether-lumefantrine compared with artesunate-amodiaquine (Log-rank statistic = 7.37, P = 0.007, Fig. 4a). The probabilities of reappearance of asexual parasitaemia after treatment with the two (artesunate-amodiaquine or artemether-lumefantrine) were similar in anaemic and non-anaemic children (Log-rank statistic = 1.04, P = 0.31, Fig. 4b).
Kaplan-Meier survival estimates of asexual parasitaemia, (a) after treatment with AA (blue line) or AL (green line); [log-rank statistic = 7.37; P = 0.007], and (b) in children with (green line) or without (blue line) anaemia at presentation [log-rank statistic = 1.04; P = 0.31]. AA, artesunate-amodiaquine; AL, artemether-lumefantrine
Prevalence of asexual parasitaemia on day 1
Overall, asexual parasite prevalence 1 day after treatment began was 34% (461 of 1 346 children). The prevalence was 28% (236 of 829 children) in children treated with artesunate-amodiaquine and 44% (225 of 517 children) in those treated with artemether-lumefantrine. The difference between these two proportions was significant (P < 0.0001). Parasite prevalence 1 day after treatment began was significantly higher in anaemic compared to non-anaemic children (175 of 437 children [40%] versus 286 of 909 children [31%]; P = 0.002).
Parasite positivity on day 3
Overall, parasite positivity on day 3 was 0.7% (9 of 1 346 children and it was similar in children treated with artesunate-amodiaquine or artemether-lumefantrine (6 of 829 versus 3 of 517 children, P = 1.0). Of the 286 children who had enrolment parasitaemia ≥100 000 μL−1, 3 children (2 in artesunate-amodiaquine and 1 in artemether-lumefantrine treatment groups) had parasitaemia on day 3, suggesting there was no in-vivo evidence of any cluster of cases with slow parasite clearance after treatment. Parasite positivity on day 3 was similar in anaemic and non-anaemic children (6 of 437 versus 3 of 909; P = 0.07). All 3 children with parasite positivity on day 3 who had parasitaemia ≥100 000 μL−1 at enrolment were anaemic at presentation.
Parasite reduction ratio 1 day after treatment began (PRRD1)
Overall, geometric mean parasite reduction ratio 1 day after treatment started was 3.1 × 103 (range 1.1 × 10−1–2.1 × 106). Geometric mean parasite reduction ratio 1 day after treatment began was significantly higher in artesunate-amodiaquine- compared to artemether-lumefantrine-treated children [5.2 × 103 (range 1.1 × 10−1–1.1 × 106) versus 1.3 × 103 (range 4.1 × 10−1–2.1 × 106); P < 0.0001] (Fig. 5a). PRRD1 was significantly higher in non-anaemic compared to anaemic children [4.3 × 103 (range 3.2 × 10−1–1.1 × 106) versus 1.6 × 103 (range 1.1 × 10−1–2.1 × 106); P < 0.0001]. PRRD1 increased with year following treatment and was significantly higher in 2011–2014 than in 2008–2010 with both ACTs [1.1 × 104 (range 7.1 × 10−1–1.1 × 106) versus 2.4 × 103 (range 1.1 × 10−1–2.1 × 106), P < 0.0001] (Fig. 5b and c).
Scatter plots of day 1 parasite reduction ratios (PRRD1) in children with uncomplicated P. falciparum malaria following treatment with artesunate-amodiaquine (AA) or artemether-lumefantrine (AL): (a) all children treated with AA or AL during the period 2008–2014, (b) all children treated with AA during the period 2008–2010 and 2011–2014 and (c) all children treated with AL between 2008–2010 and 2011–2014
Parasite reduction ratio 2 days after treatment began (PRRD2)
Overall, geometric mean parasite reduction ratio 2 days after treatment began was 2.5 × 104 (range 1.6 × 101–2.1 × 106). Geometric mean parasite reduction ratio 2 days after treatment began was significantly higher in artesunate-amodiaquine- compared to artemether-lumefantrine-treated children [2.9 × 104 (range 1.6 × 101–1.1 × 106) versus 2.0 × 104 (range 1.7 × 101–2.1 × 106), P = 0.001]. PRRD2 was significantly higher in non-anaemic compared to anaemic children [2.9 × 104 (range 1.7 × 101–1.1 × 106) versus 1.9 × 104 (range 1.6 × 101–2.1 × 106); P < 0.0001]. PRRD2 increased over the years: it was significantly higher in 2011–2014 than in 2008–2010 with both ACTs [4.8 × 104 (range 2.1 × 103–1.1 × 106) versus 2.2 × 104 (range 1.6 × 101–2.1 × 106), P < 0.0001].
Secondary outcomes
Parasite and fever clearance
Overall, parasite clearance was significantly faster in artesunate-amodiaquine- compared with artemether-lumefantrine-treated children [1.3 day (95%CI: 1.3-1.4) versus 1.5 day (95%CI: 1.4-1.5), P < 0.0001]. Similarly, fever clearance was significantly faster in artesunate-amodiaquine- compared with artemether-lumefantrine-treated children [1.1 day (95%CI: 1.06 – 1.13) versus 1.2 day (95%CI: 1.13 – 1.29), P = 0.002]. The secondary outcomes in these children according to drug treatment or haematocrit status are shown in Table 3. Fever and parasite clearance times were similar in anaemic and non-anaemic children treated with artemether-lumefantrine. Fever but not parasite clearance time was similar in anaemic and non-anaemic children treated with artesunate-amodiaquine. Further exploratory analysis of the children treated with artesunate-amodiaquine when matched for age, gender, same treatment, same day of presentation and same parasitaemia, showed that, parasite and fever clearance times were similar in anaemic and non-anaemic children [1.2 day versus 1.1 day; P = 0.14 (n = 90) and 1.0 day versus 1.1 day; P = 0.18 (n = 90), respectively]. Parasite clearance time decreased significantly over the years [1.2 day (95%CI: 1.2-1.3) in 2011–2014 versus 1.4 day (95%CI: 1.4-1.5) in 2008–2010; P < 0.0001]. However, fever clearance did not change over the years [1.2 day (95%CI: 1.0-1.3) in 2011–2014 versus 1.1 day (95%CI: 1.1-1.2) in 2008–2010; P = 0.63].
Gametocyte carriage
Overall, 67 of 1 117 children (6%) had patent gametocytaemia at enrolment. Gametocyte carriage was similar in anaemic compared to non-anaemic children (19 of 295 versus 48 of 822, P = 0.71). In Ibadan where gametocyte carriage at presentation was evaluated for 7 years, gametocyte carriage did not decrease significantly over the study period (4 of 116, 15 of 255, 3 of 103, 7 of 68, 2 of 61 and 1 of 60 in 2008, 2009, 2010, 2011, 2012 and 2014, respectively, P = 0.41 test for trend). Gametocytes were not detectable in peripheral blood of all the children after day 14.
Fall in haematocrit/1 000 asexual parasites cleared from peripheral blood
Data for evaluation of fall in haematocrit (FIH)/1 000 asexual parasites cleared from peripheral blood (cpb) were available in 643 children (see Fig. 3). Overall, median FIH/1 000 asexual parasites cpb was 0.029 (range 0.0001-0.91) and it did not decrease over the years [median 0.026 (range 0.0001-0.76; n = 443) in 2008–2010 versus 0.032 (range 0.0004–0.91, n = 200) in 2011–2014, P = 0.39]. FIH/1 000 asexual parasites cleared from peripheral blood was similar in children treated with artesunate-amodiaquine and artemether-lumefantrine [median 0.028 (range 0.0001–0.91, n = 441) versus 0.031 (range 0.0003–0.87, n = 202); P = 0.65]. FIH/1 000 asexual parasites cpb was significantly greater at lower parasitaemias (<100 000 μL−1) compared to higher parasitaemias (≥100 000 μL−1) [median 0.046 (range 0.001–0.91, n = 444) versus median 0.011 (range 0.0001–0.087, n = 199), P < 0.0001], suggesting much haematocrit conservation at higher parasitaemias compared to lower parasitaemias. In non-anaemic children, FIH/1 000 asexual parasites cleared from peripheral blood was significantly greater compared to anaemic children [median 0.032 (range 0.0001–0.91, n = 502) versus median 0.022 (range 0.0004–0.62, n = 141), P = 0.007] also suggesting much haematocrit conservation in anaemic compared to non-anaemic children. Similarly, FIH was significantly greater in patients with mild compared to moderate anaemia at presentation [median 0.024 (range 0.004–0.62, n = 133) versus median 0.002 (range 0.0008–0.09, n = 8), P = 0.04]. Further exploratory analysis showed that FIH/1 000 asexual parasites cleared from peripheral blood was significantly greater in non-anaemic children with enrolment parasitaemias of 50 000 μL−1 -100 000 μL−1 compared to anaemic children with enrolment parasitaemias of 50 000–100 000 μL−1 [median 0.037 (range 0.001–0.17, n = 126) versus median 0.026 (range 0.001–0.15, n = 48), P = 0.003].
Anaemia recovery time
Anaemia recovery time was evaluated in patients who had ≥5 units fall in haematocrit from 30% and in whom haematocrit measurement was done consistently in >90% of the times of follow-up. Fifty eight of 185 anaemic children met the strict criteria for the evaluation of anaemia recovery time (see Fig. 3). Mean anaemia recovery time was 15.4 days (95%CI: 13.3–17.4). Anaemia recovery time did not change over the years (15.6 days (95%CI: 13–18.3, n = 39) in 2008 – 2010 versus 14.8 days (95%CI: 11.2–18.5, n = 19) in 2011–2014, P = 0.73). Anaemia recovery time was similar in children aged <3 and ≥3 years (18.5 days (95%CI: 13.7–23.4, n = 15) versus 14.3 days (95%CI: 12–16.5, n = 43); P = 0.07). Anaemia recovery time was also similar in anaemic children with high enrolment parasitaemias (≥100 000 μL−1) compared with those with low enrolment parasitaemias (<100 000 μL−1) [14.6 days (95%CI: 11.2–18, n = 20) versus 15.7 days (95%CI: 13–18.5, n = 38), P = 0.6]. There was no correlation between anaemia recovery time and parasite clearance time (r = 0.071, P = 0.58, n = 58) and between anaemia recovery time and FIH/1 000 asexual parasites cleared from peripheral blood (r = 0.004, P = 0.61, n = 58) in the same patients.
Temporal changes in haematocrit in anaemic children following treatment with artesunate-amodiaquine or artemether-lumefantrine
Temporal changes in haematocrit were evaluated in 123 of 185 (66%) children who were anaemic at presentation and in whom haematocrit concentration was measured in all (100%) or nearly all (90%) of the follow-up period. The temporal changes in haematocrit are as follows: 1. Haematocrit <30% before treatment, followed by an increase to ≥30% after treatment and remaining so during the entire period of follow-up (malaria-associated anaemia and recovery from anaemia, n = 98 (79.7%)). 2. Haematocrit <30% at presentation followed by a rise to ≥30% by day 7 and a fall to <30% between days 7 and 14 and then recovery (anaemia-early recovery-early anaemia-late recovery, n = 12 (9.8%)). 3. Haematocrit <30% at presentation followed by a rise to ≥30% on day 7 or 14 and two consecutive normal haematocrit values followed by a decline to <30% after day 14 (anaemia-early recovery-late-appearing anaemia pattern, n = 7 (5.7%)). 4. Haematocrit <30% at before treatment began and during the entire follow-up period (persistent, unresolved anaemia, n = 4, (3.2%). 5. Patients with multiple falls below 30%, followed by multiple rises to ≥30% during follow-up period (undulating pattern of anaemia, n = 2 (1.6%)). No patient was unclassifiable.
The characteristics of the seven children with anaemia at presentation, who recovered from their anaemia and who subsequently developed late fall in haematocrit to <30% after day 14 are shown in Table 4. The late-appearing anaemia after initial recovery from the anaemia at presentation was characterised by an age ≤5 years (5 of 7 children), relatively high enrolment parasitaemia (6 of 7 had >50 000 asexual parasitaemia μL−1), rapid clearance of asexual parasitaemia [6 of 7 cleared by day 1] and low FIH/1 000 asexual parasites (cpb). Six of these 7 children were treated with artesunate-amodiaquine. Of the children treated with artesunate-amodiaquine, 4 were given total doses of artesunate ≥ 10 mg/kg over three days.
For comparison, the characteristics of 8 of 568 non-anaemic children at presentation who subsequently developed late-appearing anaemia after day 14 are shown in Table 5. The late-appearing anaemia was characterised by an age >5 years (7 of 8 children), relatively high enrolment parasitaemia (7 of 8 had parasitaemia >50 000 asexual parasitaemia μL−1), rapid clearance of asexual parasitaemia (5 of 8 cleared by day 1) and low FIH/1 000 asexual parasites cpb. Of these children, 6 were treated with artesunate-amodiaquine. Of the children treated with artesunate-amodiaquine, 5 were given total doses of artesunate ≥10 mg/kg over three days. Apart from age, all parameters appear to be similar in children with and without anaemia at presentation who developed late-appearing anaemia after day 14.
Relationship between AUC of deficit in haematocrit from 30% versus time and FIH/1 000 asexual parasites cleared from peripheral blood
In the 7 children who were anaemic at presentation, who recovered from their anaemia and who subsequently developed anaemia 21 or more days after treatment began (see Table 4), the AUC of deficit in haematocrit from 30% versus time at presentation were similar to AUC of deficit in haematocrit from 30% versus time when anaemia developed 21 or more days after treatment began [33.9%.day (95%CI: 13.83–54.1) versus 19.9%.day (95%CI: 3.62–48.36); P = 0.09]. There was no correlation between AUC of deficit in haematocrit from 30% versus time of the late-appearing anaemia and FIH/1 000 asexual parasites cleared from peripheral blood (r = 0.45; P = 0.31).
Kinetics of the disposition of the deficit in haematocrit from 30%
The kinetics of the disposition of the deficit in haematocrit were evaluated in 58 children (n = 43 for artesunate-amodiaquine and n = 15 for artemether-lumefantrine) with the following demographic and other characteristics: mean age 5.2 years (range 1.1-13); mean duration of illness 3.5 days (range 1–7); mean body temperature 38.4°C (range 36.2-41); mean haematocrit 23.2% (range 17–25); geometric mean parasitaemia 61 752 asexual form /μL (range 2 100 – 288 461); mean fever clearance time 1.2 days (1–7); mean parasite clearance time 1.2 days (range 1–3); mean anaemia recovery time 15.4 days (range 2–28). None of the patients had late-appearing anaemia. Overall, there was monoexponential decline of the deficit in haematocrit from 30% with an estimated mean elimination half-time (t½el, t½anaemia) of 1.4 days (95%CI: 1.2-1.6) (Fig. 6). In <5 (n = 34) and ≥5 (n = 24) year olds, estimated mean elimination half-times were 1.5 days (95%CI: 1.2-1.8) and 1.3 days (95%CI: 0.9-1.6) and they were similar (P = 0.38). The estimated mean t½el values were also similar in artesunate-amodiaquine- (1.4 days, 95%CI: 1.1–1.7) and artemether-lumefantrine-treated (1.3 days, 95%CI: 0.9–1.7) children (P = 0.66) (Fig. 6). Estimated mean half-times were also similar in children with enrolment parasitaemia ≥100 000 μL−1 and those with <100 000 μL−1 [1.2 days (95%CI: 0.9–1.4, n = 20) versus 1.5 days (95%CI: 1.2–1.8, n = 38); P = 0.19], and in children with mild and moderate anaemia at presentation [1.4 days (95%CI: 1.1–1.6, n = 48) versus 1.6 days (95%CI: 1.1–2.0, n = 10); P = 0.46].
Overall, mean areas under curve of deficit in haematocrit from 30% versus time (AUCdef) value were 63.7%.day (95%CI: 51.0–76.4). Mean AUCs were similar in artesunate-amodiaquine- and artemether-lumefantrine - treated children [59.4%.day (95%CI: 46.3–72.5) versus 76.0%.day (95%CI: 41.7–110.3), P = 0.26]. Mean AUCdef values were also similar in <5 and ≥5 year olds [65.2%.day (95%CI: 49.9–80.4, n = 34) and 61.6%.day (95%CI: 38.3–84.8, n = 24), P = 0.78], and in children with enrolment parasitaemia ≥100 000 μL−1 and those with <100 000 μL−1 [65.8%.day (95%CI: 43.8–87.8; n = 20) and 62.5%.day (95%CI: 46.3–78.8; n = 38), P = 0.81].
Relationship between half - time of decline in haematocrit deficit and anaemia recovery time
The relationship between the half-time of decline in haematocrit deficit from 30% and anaemia recovery time in the same patients with anaemia at presentation was evaluated in 58 children. The mean half-time of decline in haematocrit deficit from 30% was 1.4 days (95%CI: 1.2–1.6). The mean anaemia recovery time was 15.4 days (range 2–28). There was a significantly positive correlation between half-time of decline in haematocrit deficit from 30% and anaemia recovery time in the same patients (r = 0.69, P < 0.0001). Bland-Altman plots of the anaemia recovery times and 9 or 10 multiples of anaemia half-times are shown in Fig. 7. The limit of agreement between anaemia recovery time and 9 multiples of anaemia half-time was not narrow. The bias was significantly different from 0 (P = 0.0005). However, at multiple of 10 half-times, the limit of agreement between anaemia half-time and anaemia recovery time was narrow. The bias at multiple of 10 anaemia half-times was statistically insignificant (P = 0.07).
Adverse events
Adverse events were carefully monitored in 610 non-anaemic and 185 anaemic children drawn from Ibadan centre. Overall, 186 of 795 children [23%] (150 of 548 [27%] in artesunate-amodiaquine and 36 of 247 [15%] in artemether-lumefantrine reported at least one adverse event within the first week of starting treatment. There was a significant difference in the proportions of children reporting adverse events in both treatment groups (P < 0.0001). Fever (70 of 548 [13%] versus 11 of 247 [4%], P = 0.0005), vomiting (38 of 548 (7%) versus 6 of 247 (2%), P = 0.016), headache (33 of 548 (6%) versus 4 of 247 (2%), P = 0.006), abdominal pain (46 of 548 (8%) versus 3 of 247 (1%), P = 0.00002) and anorexia (26 of 548 (5%) versus 3 of 247 (1%), P = 0.013) were significantly more common in artesunate-amodiaquine- compared with artemether-lumefantrine-treated children. Other reported adverse events (cough, weakness, puffy face, itching and drowsiness) were similar in frequency in the two treatment groups. One hundred and thirty eight of 610 children without anaemia at presentation [23%] and 48 of 185 children with anaemia at presentation [26%] reported at least one adverse event within the first week of commencement of treatment. There was no significant difference in the proportions of children reporting adverse events in anaemic and non-anaemic children (P = 0.4). The most commonly reported adverse events in non-anaemic and anaemic children were fever [65 of 610 (11%) versus 16 of 185 (9%), P = 0.62], vomiting [35 of 610 (6%) versus 9 of 185 (5%), P = 0.21], abdominal pain [31 of 610 (5%) versus 18 of 185 (10%), P = 0.03] and cough [40 of 610 (7%) versus 19 of 185 (9%), P = 0.09].
Discussion
In this study, conducted during a seven year-period of adoption of ACTs as first-line treatments of uncomplicated P. falciparum malaria in Nigeria, artesunate-amodiaquine proved a superior alternative to artemether-lumefantrine as evidenced by a significantly higher PCR-corrected 28 days parasitological efficacy or better measures of therapeutic responses. These findings were not unexpected as a previous relatively large study conducted in southwest Nigeria during the first 5 years of adoption showed similar results [36]. The PCR-corrected 28 days efficacy of over 96% with both treatments supports continuing efficacy of ACTs in P. falciparum infections in virtually all endemic areas of Nigeria since adoption as first-line treatments in 2005. It is, however, in contradistinction to the reports of declining responsiveness of P. falciparum to ACTs in Kenya or Suriname [53, 54] or resistance to artemisinin in the Greater Mekong subregion [5, 7].
It is intriguing that PRRD1, a less frequently evaluated measure of therapeutic efficacy in the area of study, was also significantly higher in children treated with artesunate-amodiaquine compared with artemether-lumefantrine. With respect to parasite prevalence 1 day after treatment began being significantly lower in children treated with artesunate-amodiaquine compared to those treated with artemether-lumefantrine, similar difference in parasite prevalence after treatment began has been reported between the two ACTs [55].
Overall, despite being significantly younger, parasitological responses in anaemic children were similar to those of non-anaemic children suggesting that in this area of full sensitivity in P. falciparum to the two ACTs, anaemia did not compromise, to any significant extent, the therapeutic responses to both treatments. The younger age of the anaemic children may be partly responsible for the slower parasite clearance and the lower parasite reduction ratios 1 and 2 days after treatment began in artesunate-amodiaquine-treated children because younger children may be considered to have relatively lower antimalarial immunity [56] and therefore slower response.
The present study showed that ACTs conserved haematocrit significantly at high parasitaemias compared to low parasitaemias, in anaemic compared to non-anaemic children, and in children with moderate compared to mild anaemia. The reasons for haematocrit conservation are unclear. It is possible the mechanisms and the kinetics of the production and disposition of the once-infected red blood cells may differ in anaemic and non-anaemic children in the first few or more days after start of artemisinin-based combination treatments. In this context, studies are needed on the production and disposition kinetics of infected and once-infected red blood cells in anaemic and non-anaemic children in this endemic area following artemisinin-based combination treatments.
Successful treatment of P. falciparum malaria with ACTs is often followed by increases in haematocrit or haemoglobin. This often led to recovery from uncomplicated malaria-associated anaemia [13, 17, 35, 40, 57]. In this relatively large series of anaemic children, anaemia recovery time in children with ≥5 units deficit in haematocrit from 30% was approximately 2 weeks. This recovery time is similar to that recently reported in very young children [58].
The monoexponential declines of the deficits in haematocrit from 30% would suggest that, using a non-compartment model, recovery from uncomplicated malaria-associated anaemia is a first-order process [47]. The anaemia recovery time : anaemia half-time of 10, and the insignificant bias between anaemia recovery time and 10 multiples of anaemia half-time by Bland-Altman analysis suggest that anaemia recovery time and 10 multiples of anaemia half-time can be used interchangeably in the evaluation of recovery from uncomplicated P. falciparum malaria-associated anaemia. This finding was expected because in a simple one-compartment pharmacokinetic model approximately 99.9% of an elimination process would have been completed in 10 half-times [48]. Thus, there is a pharmacokinetic equivalent (anaemia half-time) of a pharmacodynamic process (anaemia recovery time) in the same patients.
In children who were anaemic at presentation, the commonest temporal change in haematocrit following treatment was recovery from the associated anaemia. However, a relatively asymptomatic late-appearing anaemia occurred in 6% of anaemic children, who initially recovered from their malaria-associated anaemia following treatment. It would also appear late-appearing anaemia was significantly more frequent in anaemic compared to non-anaemic children. The relative absence of symptoms when late-appearing anaemia occurred, may make it difficult to diagnose late-appearing anaemia in children with uncomplicated infections following artemisinin-based combination treatments. The absence of overt symptoms and signs of acute haemolysis and uneventful recovery from the late-appearing anaemia would suggest that late-appearing anaemia is a previously unrecognised feature of artemisinin-based combination treatments in African children with uncomplicated infections. Studies are now under way in this endemic area of Nigeria to evaluate the risk factors associated with the relatively asymptomatic late-appearing anaemia after artemisinin-based combination treatments of uncomplicated P. falciparum malaria in children.
In general, the reported adverse events within the first week of starting treatment were indistinguishable from the symptoms of malaria. The significantly higher frequency of reported adverse events in those treated with artesunate-amodiaquine compared with artemether-lumefantrine are in keeping with previous report [59]. Pruritus has been reported in Nigeria children treated with artemether-lumefantrine [60] but in this relatively large series no child reported pruritus following artemether-lumefantrine treatment.
There are limitations of the present studies. First, although the clinical and parasitological features of children with fall in haematocrit below 30% at presentation were characterised, the nature of the anaemia was not fully characterized (that is, whether it was haemolytic or not in nature). Second, in the children with late fall in haematocrit below 30%, quantification of once-infected and infected red blood cells and the disposition of these red blood cells during the course of follow-up were not done. Third, in children with anaemia before or following treatment with ACTs, the contribution of background causes of anaemia in the area of study namely nutritional, helminthic infections, or glucose-6-phosphate dehydrogenase deficiency was not evaluated.
Conclusion
In conclusion, artesunate-amodiaquine and artemether-lumefantrine remain efficacious treatments of uncomplicated P. falciparum infections in non-anaemic and anaemic Nigerian children in the last 7 years of adoption as first-line treatments. These ACTs may also conserve haematocrit at high parasitaemias and in anaemic children.
Abbreviations
- %:
-
Percent
- °C:
-
Degree celsius
- AA:
-
Artesunate-amodiaquine
- ACPR:
-
Adequate clinical and parasitological response
- ACTs:
-
Artemisinin-based combination treatments
- AL:
-
Artemether-lumefantrine
- ANOVA:
-
Analysis of variance
- AnRT:
-
Anaemia recovery time
- AUC:
-
Area under curve
- d:
-
Day
- ETF:
-
Early treatment failure
- FCT:
-
Fever clearance time
- FIH:
-
Fall in haematocrit
- g:
-
Gram
- HCT:
-
haematocrit
- kg:
-
Kilogram
- L:
-
Litre
- LPF:
-
Late parasitological failure
- M/F:
-
Male/female
- mg:
-
Milligram
- PCR:
-
Polymerase chain reaction
- PCT:
-
Parasite clearance time
- PRR:
-
Parasite reduction ratio
- PRRD1 :
-
Parasite reduction ratio on day 1
- PRRD2 :
-
Parasite reduction ratio on day 2
- sd:
-
Standard deviation
- t½ :
-
Half-time
- μL:
-
Microliter
References
World Health Organization. Antimalarial Drug Combination Therapy. Report of a WHO Technical Consultation. Geneva: World Health Organization; 2001.
Wongsrichanalai C, Meshnick S. Declining artesunate-mefloquine efficacy against falciparum malaria on the Cambodia-Thailand border. Emerg Infect Dis. 2008;14:716–9.
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM. Evidence of artemisinin resistance in western Cambodia. N Engl J Med. 2008;359:2619–20.
Noedl H, Se Y, Sriwichai S, Schaecher K, Teja-Isavadharm P, Smith B, Rutvisuttinunt W, Bethell D, Surasri S, Fukuda MM, Socheat D, Cham TL. Artemisinin resistance in Cambodia: a clinical trial designed to address an emerging problem in Southeast Asia. Clin Infect Dis. 2010;51:e82–9.
Carrara VI, Zwang J, Ashley EA, Price RN, Stepniewka K, Marion B, Brockman A, Anderson T, McGready R, Phaiphun L, Stephane P, van Vugt M, Hutagalung R, Lwin KM, Phyo AP, Piyanuch P, Imwong M, Pukrittayakamee S, Singhasivanon P, White NJ, Nosten F. Changes in the treatment responses to artesunate-mefloquine on the northwestern border of Thailand during 13 years of continuous deployment. PLoS One. 2009;4:e511.
Lim P, Alker A, Khim N, Shah N, Incardona S, Doung S, Yi P, Bouth D, Boucher C, Mercereau P, Meshnick S, Wongsrichanalai C, Fandeur T, Bras J, Ringwald P, Ariey F. Pfmdr1 copy number and artemisinin derivatives combination therapy failure in falciparum malaria in Cambodia. Malar J. 2009;8:11.
Phyo AP, Nkhoma S, Stepniewska K, Ashley EA, Nair S, McGready R, Moo C, Al-Saai S, Dondorp AM, Lwin KM, Singhasivanon P, Day N, White NJ, Anderson TMJ, Nosten F. Emergence of arteminisin-resistant malaria on the western border of Thailand: a longitudinal study. Lancet. 2012;379:1960–6.
Chotivanich K, Udomsangpetch R, Dondorp A, Williams T, Angus B, Simpson JA, Pukrittayakamee S, Looaresuwan S, Newbold CI, White NJ. The mechanisms of parasite clearance after antimalarial treatment of Plasmodium falciparum malaria. J Infect Dis. 2000;182:629–33.
Newton PN, Chotivanich K, Chierakul W, Ruagveerayuth R, Teerapong P, Silamut K, Looareesuwan S, White NJ. A comparison of the in vivo kinetics of Plasmodium falciparum ring-infected erythrocyte surface antigen-positive and –negative erythrocytes. Blood. 2001;98:450–7.
Jauréguiberry S, Ndour PA, Roussel C, Ader F, Safeukui I, Nguyen M, Biligui S, Ciceron L, Mouri O, Kendjo E, Vray M, Angoulvant A, Mayaux J, Haldar K, Mazier D, Danis M, Caumes E, Thellier M, Buffet P. Postartesunate delayed hemolysis is a predictable event related to the lifesaving effect of artemisinins. Blood. 2014;124:167–75.
Gbotosho GO, Okuboyejo TM, Happi CT, Sowunmi A. Fall in haematocrit per 1 000 parasites cleared from peripheral blood: a simple method for estimating drug-related fall in haematocrit after treatment of malaria infections. Am J Ther. 2014;21:193–7.
Cornet M, Le Hesran J-Y, Fievet N, Cot M, Presonne P, Gounoue R, Beyeme M, Deloron P. Prevalence of and risk factors for anaemia in young children in southern Cameroon. Am J Trop Med Hyg. 1998;58:606–11.
Price R, Simpson JA, Noston F, Luxemburger C, Hkirjaroen L, ter Kuile FO, Chongsuphajasiddhi T, White NJ. Factors contributing to anaemia after uncomplicated falciparum malaria. Am J Trop Med Hyg. 2001;65:614–22.
Crawley J. Reducing the burden of anaemia in infants and young children in malaria-endemic countries of Africa. Am J Trop Med Hyg. 2004;71 Suppl 2:25–34.
Nkuo-Akenji TK, Chi PC, Cho JF, Ndamukong KK, Sumbele I. Malaria and helminth co-infection in children living in a malaria endemic setting of Mount Cameroon and predictors of anemia. J Parasitol. 2006;92:1191–5.
Ouédraogo HZ, Zeba A, Dramaix-Wilmet M, Donnen P. Moderate to severe anaemia due to afebrile Plasmodium falciparum infection in children aged 6–23 months from rural district of Kongoussi, Burkina Faso. J Trop Pediatr. 2008;54:395–400.
Sowunmi A, Gbotosho GO, Happi CT, Fateye BA. Factors contributing to anaemia after uncomplicated Plasmodium falciparum malaria in children. Acta Trop. 2010;113:155–61.
Sumbele IUN, Samje M, Nkuo-Akenji T. A longitudinal study on anaemia in children with Plasmodium falciparum infection in the Mount Cameroon region: prevalence, risk factors and perceptions by caregivers. BMC Infect Dis. 2013;13:123.
Marsh K, Forster D, Waruiru C, Mwangi I, Winstanley M, Marsh V, Newton C, Winstanley P, Warn P, Peshu M. Indicators of life-threatening malaria in African children. N Eng J Med. 1995;322:1399–404.
Kitua AY, Smith TA, Alonso PL, Urassa H, Masanja H, Kimario J, Tanner M. The role of low level Plasmodium falciparum parasitaemia in anaemia among infants living in an area of intense and perennial transmission. Trop Med Int Health. 1997;2:325–33.
Newton CRJC, Warn PA, Winstanley PA, Peshu N, Snow RW, Pasvol G, Marsh K. Severe anaemia in children living in a malaria area of Kenya. Trop Med Int Health. 1997;2:165–78.
English M. Life-threatening severe malarial anaemia. Trans R Soc Trop Med Hyg. 2000;94:585–8.
May J, Falusi AG, Mockenhaupt FP, Ademowo OG, Olumese PE, Bienzle U, Meyer CG. Impact of subpatent multi-species and multi-clonal plasmodial infections on anaemia in children from Nigeria. Trans R Soc Trop Med Hyg. 2000;94:399–403.
Murphy SC, Breman JG. Gaps in the childhood malaria burden in Africa: cerebral malaria, neurological sequelae, anaemia, respiratory distress, hypoglycemia, and complications of pregnancy. Am J Trop Med Hyg. 2001;64(1–2 Suppl):57–67.
Breman JG, Alilio MS, Mills A. Conquering the intolerable burden of malaria: what’s new, what’s needed: a summary. Am J Trop Med Hyg. 2004;71(2 Suppl):1–15.
Zoller T, Junghanss T, Kapaun A, Gjørup I, Richter J, Hugo-Persson M, Mørch K, Foroutan B, Suttorp N, Yürek S, Flick H. Intravenous artesunate for severe malaria in travellers, Europe. Emerging Inf Dis. 2011;17:771–7.
Kreeftmeijer-Vetger AR, Genderen PJ, Visser LG, Bierman WFW, Clerinx J, van Veldehuizen CKW, de Vries PJ. Treatment outcome of intravenous artesunate in patients with severe malaria in Netherlands and Belgium. Malar J. 2012;11:102.
World Health Organization. WHO Information Note on Delayed Haemolytic Anaemia Following Treatment with Artesunate. Geneva: WHO; 2013.
Medicine for Malaria Venture. Experts Group Meeting on Delayed Haemolytic Anaemia Following Treatment with Injectable Artesunate. Vienna, Austria; 2013. (http://www.mmv.org/newsroom/events/expert-group-meeting-safety-profile-injectable-artesunate).
Rolling T, Agbenyega T, Issifou S, Adegnika AA, Sylverken J, Spahlinger D, Ansong D, Löhr SJ, Burchard GD, May J, Mordmuller B, Krishna S, Kremsner PG, Cramer JP. Delayed hemolysis after treatment with parenteral artesunate in African children with severe malaria – a double-center prospective study. J Infect Dis. 2014;209:1921–8.
Burri C, Ferrari G, Ntuku HM, Kitoto AT, Duparc S, Hugo P, Mitemba DK, Lengeler C. Short report: Delayed anaemia after treatment with injectable artesunate in Demographic Republic of the Congo: a manageable issue. Am J Trop Med Hyg. 2014;91:821–3.
Federal Ministry of Health. National Antimalarial Treatment Guidelines. Abuja: Federal Ministry of Health; 2005.
Salako LA, Ajayi FO, Sowunmi A, Walker O. Malaria in Nigeria: a revisit. Ann Trop Med Parasitol. 1990;84:435–45.
World Health Organization. World Malaria Report. Geneva: World Health Organization. WHO/HTM/RBM/2014; 2014.
Gbotosho GO, Sowunmi A, Okuboyejo TM, Happi CT, Folarin OO, Michael SO, Adewoye EO. Therapeutic efficacy and effect of artemether-lumefantrine and artesunate-amodiaquine cofomulated or copackaged on malaria-associated anaemia in children in uncomplicated Plasmodium falciparum malaria in southwest Nigeria. Am J Trop Med Hyg. 2011;84:813–9.
Gbotosho GO, Sowunmi A, Happi CT, Okuboyejo TM. Therapeutic efficacies of artemisinin-based combination therapies in Nigerian children with uncomplicated falciparum malaria during five years of adoption as first-line treatments. Am J Trop Med Hyg. 2011;84:936–43.
Sowunmi A, Gbotosho GO, Happi CT, Folarin O, Okuboyejo T, Michael O, Fatunmbi B. Use of area under the curve to evaluate the effects of antimalarial drugs on malaria-associated anaemia after treatment. Am J Therap. 2011;18:1190–7.
Sowunmi A, Okuboyejo TM, Gbotosho GO, Happi CT. Early changes in Plasmodium falciparum asexual and sexual populations in children with acute infections following treatment with artemisinin-based combination drugs. Mal Chemother Ctrl Elim. 2012;1:235498. doi:10.4303/mcce/235498.
Michael OS, Gbotosho GO, Folarin OA, Okuboyejo T, Sowunmi A, Oduola AMJ, Happi CT. Early variations in Plasmodium falciparum dynamics in Nigerian children after treatment with two artemisinin-based combinations: implications on delayed parasite clearance. Malar J. 2010;9:335.
Oguche S, Okafor HU, Watila I, Meremikwu M, Agomo P, Ogala W, Agomo C, Ntadom G, Banjo O, Okuboyejo T, Ogunrinde G, Odey F, Aina O, Sofola T, Sowunmi A. Efficacy of artemisinin-based combination treatments of uncomplicated falciparum malaria in under-five year-old Nigerian children. Am J Trop Med Hyg. 2014;91:925–35.
Shaper AG, Lewis P. Genetic neutropenia in people of African origin. Lancet. 1971;2(7732):1021–3.
Ezeilo GC. Neutropenia in Africans. Trop Geogr Med. 1971;23:264–7.
Sowunmi A, Akindele JA, Balogun MA. Leukocyte counts in falciparum malaria in African children from an endemic area. Afr J Med Med Sci. 1995;24:145–9.
World Health Organization. Assessment and Monitoring of Antimalarial Drug Efficacy for the Treatment of Uncomplicated Falciparum Malaria. Geneva: WHO/HTM/RBM/2003.50; 2003.
World Health Organization. Methods for Surveillance for Antimalarial Drug Efficacy. Geneva; 2009.
White NJ. Assessment of the pharmacodynamics properties of antimalarial drugs in vivo. Antimicrob Agent Chemother. 1997;41:1413–22.
Sowunmi A, Akano K, Ayede AI, Ntadom G, Aderoyeje T, Adewoye EO, Fatunmbi B. Temporal changes in haematocrit following artemisinin-based combination treatments of uncomplicated falciparum malaria in children. BMC Inf Dis. 2015;15:454.
Rowland M, Tozer TN. Clinical pharmacokinetics: concepts and applications. Philadelphia PA Lea and Ferbiger. 1980.
Bain BJ, Bates I. Basic haematological techniques. In: Lewis SM, Bain BJ, Bates I, editors. Practical Haematology. 9th ed. Edinburgh: Churchill Living stone; 2001. p. 19–46.
Anon. Epi Info Version 6. A Word Processing Data Base and Statistics Program for Public Health on IBM-compatible Microcomputers. Atlanta: Centers for Disease Control and Prevention; 1994.
Anon. SPSS for Windows Release 20.0 (standard version). Chicago: SPSS Inc; 2011.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Borrmann S, Sasi P, Mwai L, Bashraheil M, Abdallah A, Muriithi S, Frühauf H, Schaub B, Pfeil J, Peshu J, Hanpithakpong W, Rippert A, Juma E, Tsofa B, Mosobo M, Lowe B, Oseir F, Fegan G, Lindegårdh N, Nzila A, Peshu N, Mackinnon M, Marsh K. Declining responsiveness of Plasmodium falciparum infections to artemisinin-based combination treatments on the Kenyan coast. PLoS One. 2011;6:26005.
Vreden SGS, Jitan JK, Bansie RD, Adhin MA. Evidence of an increased incidence of day 3 parasitaemia in Suriname: an indicator of the emerging resistance of Plasmodium falciparum to artemether. Mem Inst Os Cruz. 2013;108:968–73.
Das D, Price RN, Bethel D, Guerin PJ, Stepniewska K. Early parasitological response following artemisinin-containing regimens: a critical review of the literature. Malar J. 2013;12:125.
World Health Organization. Chemotherapy of Malaria and Resistance to Antimalarials. Geneva: World Health Organization; 1973.
Sowunmi A, Balogun ST, Gbotosho GO, Happi CT. Effects of amodiaquine, artesunate, and artesunate-amodiaquine of Plasmodium falciparum malaria-associated anaemia in children. Acta Trop. 2009;109:55–60.
Sowunmi A, Akano K, Ayede AI, Ntadom G, Adewoye EO, Fatunmbi B, Aderoyeje T. Therapeutic efficacy and effects of artesunate-amodiaquine and artemether-lumefantrine on malaria-associated anaemia in Nigerian children aged two years and under. Infect Dis Poverty. 2016;5:70. doi:10.1186/s40249-016-0165-2.
Schramm B, Valch P, Baudin C, Mazinda CS, Smith R, Pinoges I, Sundaygar T, Zolia YM, Jones JJ, Comte E, Bruneel A, Branger M, Jullien V, Cam G, Kiechel J-R Ashley EA, Guérin PJ. Tolerability and safety of artesunate-amodiaquine and artemether-lumefantrine fixed dose combinations for the treatment of uncomplicated Plasmodium falciparum malaria: two open-label, randomized trial in Nimba County, Liberia. Malar J. 2013;12:250.
Okafor HU, Shu EN, Oguonu T. Therapeutic efficacy and effect on gametocyte carriage of an artemisinin and a non-based combination treatment in children with uncomplicated Plasmodium. falciparum malaria, living in an area with high-level chloroquine resistance. J Trop Pediatr. 2010;56:398–406.
Acknowledgements
We are grateful to the parents/guardians and the children who participated in the study.
Funding
The efficacy studies from which the data were derived were supported by Swiss Pharma Nigeria PLC Grant to AS and by World Bank Malaria Booster Project, and Global Fund for Malaria to Federal Ministry of Health, Abuja, Nigeria through Drug Therapeutic Efficacy Testing in Nigeria. Logistic support for Drug Therapeutic Efficacy Testing was partly provided by Society for Family Health and Support for National Malaria Program (SunMap) in Nigeria.
Availability of data and materials
The dataset supporting the findings of this article is available from the corresponding author upon request.
Authors’ contributions
AS led the design, conduct, data analysis and manuscript preparation. KA, GN, AIA, TA, EOA, BF, CA and GOG participated in data collections and analysis. SO, HUO, IW, MM, PA, and WO participated in data collection. OF and CTH performed the molecular analysis of the parasite isolates and participated in the analysis. All authors read and approved the final draft of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study protocol was approved by The Ethics Committee of The Ministry of Health, Ibadan and by National Health Research Ethics Committee, Abuja, Nigeria. The reference numbers are: Ministry of Health Ibadan - AD 13/262/56 (7 March 2006), AD 13/479/978 (December 2015); National Health Research Ethics Committee - NHREC/01/01/2007-28/10/2009d (30 October 2009), NHREC/01/01/2007-28/10/2013 (29 October 2013), NHREC/01/01/2007-22/10/2014 (30 October 2014). Written informed consents were obtained from parents/guardians of the children.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Multilingual abstracts in the six official working languages of the United Nations. (PDF 808 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sowunmi, A., Akano, K., Ntadom, G. et al. Therapeutic efficacy and effects of artemisinin-based combination treatments on uncomplicated Plasmodium falciparum malaria -associated anaemia in Nigerian children during seven years of adoption as first-line treatments. Infect Dis Poverty 6, 36 (2017). https://doi.org/10.1186/s40249-016-0217-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-016-0217-7