Abstract
Background
Hepatitis C virus (HCV) infection is an important cause of chronic liver disease which has been affected 3% of world’s population. Some studies have shown that adding Sofosbuvir (SOF), an HCV polymerase inhibitor to the conventional therapy of Pegylated-interferon (PegIFN) plus Ribavirin (RBV) can increase the rate of sustained virologic response (SVR) among HCV-infected patients. This study was conducted to determine the effect of combination therapy with PegIFN and RBV plus SOF for chronic hepatitis C genotype 1 infection using systematic review with meta-analysis.
Methods
In this study, electronic databases including PubMed, Scopus, Science Direct, and Web of Science were comprehensively searched using appropriate strategies containing all related keywords of “hepatitis C”, “PegIFN”, “RBV” and “SOF”. Studies assessed the efficacy of combination therapy with PegIFN and RBV plus SOF for chronic hepatitis C genotype 1 infection were included in the meta-analysis.
Results
After screening of 757 records, we included five articles with total sample size of 411 to the meta-analysis. Based on the fixed-effect model (χ 2 = 5.29, P = 0.26 and I2 = 24.4%), pooled SVR rate for treatment regimen of PegIFN and RBV plus SOF was calculated as 88.54% (95% CI = 85.77%–91.32%).
Conclusions
Combination therapy with PegIFN and RBV plus SOF results in high treatment response in patients with HCV genotype 1 infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Hepatitis C infection is the major cause of acute and chronic hepatitis globally. Based on the World Health Organization (WHO) estimation, about 3% of world population is infected with hepatitis C virus (HCV) and the worldwide prevalence of chronic hepatitis C is more than 180 million who are at the predisposing to cirrhosis and/or liver cancer [1,2,3].
Treatment of chronic hepatitis C comprises several components including, reduction of inflammation, prevention of fibrosis, cirrhosis and hepatocellular carcinoma and virus eradication. Currently, sustained virologic response (SVR) functions as the best indicator of effective treatment [4, 5]. Although treatment decisions are influenced by the HCV genotype, combination therapy in comparison with monotherapy achieved higher response rate. Adding Ribavirin (RBV) to Pegylated-interferon (PegIFN) increased SVR rate from 15 to 20% to 40%–50% in HCV genotype 1 infection. However, to reach to more than 50% SVR, combination therapy with PegIFN and RBV lost its efficacy particularly in HCV genotype 1 infection [6,7,8].
Sofosbuvir (SOF) is a HCV NS5B polymerase inhibitor that results in suppression of HCV replication and life cycle. Sofosbuvir as a new direct-acting antiviral agent (DAA) was approved for treatment of chronic HCV genotypes 1 to 4 infections. HCV genotype 1-infected patients should receive PegIFN, RBV and SOF for 12 weeks. From the data of trials, the latter combination therapy results in SVR12 rates of 50%–90% [9, 10].
This study set out with the aim of assessing efficacy of 12-week combination of PegIFN, RBV and SOF for treatment of patients with chronic hepatitis C infection caused by HCV genotype 1.
Methods
Data resources and search strategy
In this systematic review and meta-analysis, electronic databases including PubMed, Scopus, Science Direct, and Web of Science were comprehensively searched using exact and sensitive search strategies (Additional file 1: Appendix), which concentrated on each element of HCV treatment regimen PegIFN, RBV plus SOF. On the other hand, the Google scholar was searched with appropriate keywords and after finding the last related title, we continued our search for 200 serial unrelated titles. This helped us to check the sensitivity of our search strategies. Furthermore, references of the finally included papers were investigated for retrieving any missing papers. Our last search using search strategies was performed at September 02, 2015. However, we did an updated search on April, 2016 just before analysis of data.
Inclusion and exclusion criteria
All studies reporting the rate of SVR12 after ending treatment with PegIFN, RBV plus SOF for 12 weeks in patients with HCV genotype 1 infection were included. We considered the approach of intention-to-treat in the step of data extraction. Furthermore, we excluded studies evaluating patients with history of liver transplantation, chronic hemodialysis, kidney transplantation, history of previous treatment with DAAs, HIV/HCV coinfection, and decompensated cirrhosis (Child-Pugh B and C).
Study selection and data extraction
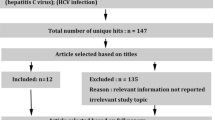
The PRISMA guideline for reporting of systematic review was used [11]. Two reviewers (FD and HKS) screened all the identified papers in three levels including title, abstract, and full-text, independently. Any disagreement between these two reviewers were discussed mutually and any remained discrepancies were resolved by the discussion with a third reviewer (SMA or HSH).
Following parameters were extracted from the included studies; author’s first name, history of previous treatment, publication year, country, sample size, mean/median age, gender, body mass index (BMI), HCV RNA level before treatment, rate of cirrhotic patients, polymorphism near IFNL3 (rs12979860), and HCV subtype 1a/1b.
Quality assessment
For evaluating risk of biases in each included clinical trial, Cochrane’s assessment tool was used [12]. These biases are random sequence generation (selection bias), allocation concealment (selection bias), blinding of participant and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition), selective reporting (reporting bias), co-interventions, intention-to-treat analysis, group similarity at baseline, compliance, timing of outcome assessments and other biases. These 12 items were scored 0 if were high risk and unclear, and scored 1 if were low risk. Then, overall score ≥6 was considered as low risk for each study.
For assessing quality of the included non-randomized studies, Newcastle-Ottawa Scale (NOS) was used [13]. This tool helps to assess methodological problems regarding selection of participants, comparability of case and control groups and also ascertain of exposure and outcomes. Any disagreement in quality assessment by two above tools were resolved by mutual discussion.
Data analysis
We used chi-square and I-squared (lies from 0 to 100%) for evaluating heterogeneity across studies’ results. P value less than 0.1 was considered statistically significant for chi-squared. We evaluated publication bias by Begg’s and Egger’s tests. Based on the presence or absence of heterogeneity, random- or fixed-effect model was employed for calculation of pooled SVR12 rate and 95% confidence interval (CI). All data analyses were performed using STATA 10.
Results
Study screening and characteristics of the included papers
A total of 757 papers were found through database searching after removing duplications. In title screening, 519 irrelevant titles and in the abstract screening, 230 irrelevant abstracts were excluded. Then, eight full-text articles were assessed for eligibility and finally five articles with total sample size of 411 were included in our quantitative synthesis (Fig. 1).
Table 1 shows important characteristics of the included papers. They were clinical trial (N = 4) and cohort (N = 1) studies. We found three eligible studies related to 2013 and two other related to 2015. Four of our finally included studies were from the United States and another one was from Germany. Furthermore, in three of them, included patients were treatment naïve and in two other studies, included both treatment naïve and treatment experienced participants.
Quality assessment
Using Cochrane’s risk of assessment tool four clinical trials were evaluated and all of them scored more than 6 (low risk). Furthermore, using NOS, one cohort study was evaluated and this study achieved 6 out of 8 possible stars. Therefore, no study categorized as low quality and also none of them were excluded based on this assessment (Table 2).
Outcome evaluation
There were no significant heterogeneity between results of studies based on the Chi-squared (Chi2 = 5.29, df = 4, P = 0.26) and I-squared (I2 = 24.4%, P = 0.26). Therefore, we used fixed-effect model and the pooled rate of SVR for HCV treatment regimen PegIFN, RBV plus SOF for 12 weeks was 88.54% (95% CI = 85.77%–91.32%) (Fig. 2).
We found no publication bias according to the Begg’s (P = 0.14), and Egger’s (P = 0.28) tests.
Discussion
This study showed that combination therapy with PegIFN, RBV plus SOF with 88.5% treatment success is an effective antiviral therapy for treatment of patients with HCV genotype 1 infection. Before 2011, the standard of care for therapy of HCV genotype 1 infection was combination regimen of PegIFN and RBV for 24–72 weeks with 40–60% success and many complications [14,15,16]. Introduction of first DAAs in 2011, was a major step in management of patients with HCV infection and eradication of hepatitis C as a major cause of liver disease in human kind [17]. In 2013, SOF was introduced as a HCV NS5B inhibitor and approved for treatment of HCV genotype 1 infection as a combination therapy with PegIFN and RBV [10].
The PegIFN, RBV plus SOF regimen was superior to PegIFN and RBV combination therapy in terms of higher efficacy, shorter treatment duration, and fewer side-effects. Furthermore, fewer host and virus parameters affect the treatment success in comparison with PegIFN and RBV regimen [10]. Among host factors, rs12979860 and cirrhosis were the factors modified treatment response in PegIFN, RBV plus SOF regimen [10, 18, 19]. Hopefully, SOF is a DAA with high-resistance barrier and none of the included studies in this meta-analysis found the resistance-associated substitutions such as NS5B Ser282Thr in the baseline or in patients with treatment failure [10, 19, 20].
It has been proved that combination of PegIFN, RBV and SOF can lead to complete elimination of HCV RNA in about 95% of HCV-infected patients at week 4 of treatment [10, 19, 20]. Furthermore, it has been reported that both 12- and 24-week treatment regimens with PegIFN, RBV and SOF can make about 89% SVR rate and therefore they have not considerable difference in term of response to therapy [19]. As a result, it can be suggested that response-guided therapy plays no role in the treatment with PegIFN, RBV plus SOF combination therapy.
Ledipasvir/Sofosbuvir is the first IFN-free treatment regimen for HCV which was approved by FDA in 2014. It provides >95% SVR rate among non-cirrhotic HCV genotype 1 patients [21,22,23]. Also, because of no existence of IFN in this regimen, it has fewer adverse-events. However, this regimen is not affordable in the most of the developing countries where the frequency of HCV infection is high. Moreover, generic SOF has been produced in many countries in domestic pharmaceutical companies and available with a reasonable price which can be afforded by most of the patients. Furthermore, the most common HCV genotype worldwide is genotype 1 and therefore the evaluated regimen in our project can be used in the low- and middle-income countries regarding its high efficacy [24]. Meanwhile, other regimens containing DAAs with high efficacy have been presented including Daclatasvir/Sofosbuvir [25], Paritaprevir-r/Ombitasvir/Dasabuvir [26], Simeprevir-containig regimens [27], Grazoprevir/Elbasvir [28], and Velpatasvir/Sofosbuvir [29].
The future treatments of HCV will be IFN-free regimens with high-resistance barrier which can be applied for treatment of special group patients and can clear the virus in nearly 100% of the HCV-infected patients. With knowing that the ultimate HCV treatment will be available, there is a great concern to clear HCV infection until 2030 globally. However, there are major steps toward eradication of HCV which should be addressed in the program of HCV eradication including development of HCV vaccine and other preventive strategies, availability and affordability of high efficacious regimens in developing countries, nation-wide screening programs for finding the patients with HCV infection, and paying special attention to special patient groups such as thalassemia, kidney- and liver-transplant patients and HIV/HCV co-infected patients [17, 30].
Conclusions
In conclusion, PegIFN, RBV plus SOF regimen is a highly effective therapy for treatment of HCV genotype 1 infection. While there are more expensive HCV antiviral treatments with higher efficacy than that of obtained by PegIFN, RBV plus SOF, the low cost of SOF and availability of this medication in many developing countries make the PegIFN, RBV plus SOF regimen as the recommended regimen for treatment of HCV genotype 1 infection especially when the patients cannot afford IFN-free regimens.
Abbreviations
- CI:
-
Confidence interval
- DAA:
-
Direct-acting antiviral agent
- HCV:
-
Hepatitis C virus
- NOS:
-
Newcastle-Ottawa Scale
- PegIFN:
-
Pegylated-interferon
- RBV:
-
Ribavirin
- SOF:
-
Sofosbuvir
- SVR:
-
Sustained virologic response
References
Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61(1 Suppl):S45–57.
Lavanchy D. The global burden of hepatitis C. Liver Int. 2009;29(s1):74–81.
Wen Y, Zheng YX, de Tan M. A comprehensive long-term prognosis of chronic hepatitis C patients with antiviral therapy: a meta-analysis of studies from 2008 to 2014. Hepat mon. 2015;15(5):e27181.
Copenhagen M. EASL international consensus conference on hepatitis C. J 01 Hepatol. 1999;30:956–61.
Lavanchy D. Global surveillance and control of hepatitis C. Report of a WHO consultation organized in collaboration with the viral hepatitis prevention board, Antwerp, Belgium. J Viral Hepat. 1999;6(1):35–47.
Bryan JP. Viral hepatitis: update on hepatitis C. Consultant. 1995;35(10):1551–4.
Health NIO. National institutes of health consensus development conference statement: management of hepatitis C: 2002--June 10-12, 2002. Hepatology. 2002;36(5 Suppl 1):S3.
Kanda T, Imazeki F, Yokosuka O. New antiviral therapies for chronic hepatitis C. Hepatol Int. 2010;4(3):548–61.
Rodriguez-Torres M, Lawitz E, Kowdley KV, Nelson DR, DeJesus E, McHutchison JG, et al. Sofosbuvir (GS-7977) plus peginterferon/ribavirin in treatment-naive patients with HCV genotype 1: a randomized, 28-day, dose-ranging trial. J Hepatol. 2013;58(4):663–8.
Lawitz E, Mangia A, Wyles D, Rodriguez-Torres M, Hassanein T, Gordon SC, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med. 2013;368(20):1878–87.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Higgins JPT, Green S, editors. eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 (updated September 2009). The Cochrane Collaboration 2008. Available http://handbook.cochrane.org/.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Haj-Sheykholeslami A, Keshvari M, Sharafi H, Pouryasin A, Hemmati K, Mohammadzadehparjikolaei F. Interferon-lambda polymorphisms and response to pegylated interferon in Iranian hepatitis C patients. World J Gastroenterol. 2015;21(29):8935–42.
Behnava B, Sharafi H, Keshvari M, Pouryasin A, Mehrnoush L, Salimi S, et al. The role of polymorphisms near the IL28B gene on response to Peg-interferon and Ribavirin in Thalassemic patients with hepatitis C. Hepat Mon. 2016;16(1):e32703.
Keshvari M, Alavian SM, Behnava B, Pouryasin A, Craig JC, Sharafi H. Impact of IFNL4 rs12979860 and rs8099917 polymorphisms on response to Peg-Interferon-alpha and Ribavirin in patients with congenital bleeding disorder and chronic hepatitis C. J Clin Lab Anal. 2016. doi:10.1002/jcla.22063. [Epub ahead of print].
Hesamizadeh K, Sharafi H, Rezaee-Zavareh MS, Behnava B, Alavian SM. Next steps toward eradication of hepatitis C in the Era of direct acting antivirals. Hepat Mon. 2016;16(4):e37089.
Steinebrunner N, Sprinzl MF, Zimmermann T, Worns MA, Zimmerer T, Galle PR, et al. Early virological response may predict treatment response in sofosbuvir-based combination therapy of chronic hepatitis c in a multi-center “real-life” cohort. BMC Gastroenterol. 2015;15:97.
Kowdley KV, Lawitz E, Crespo I, Hassanein T, Davis MN, DeMicco M, et al. Sofosbuvir with pegylated interferon alfa-2a and ribavirin for treatment-naive patients with hepatitis C genotype-1 infection (ATOMIC): an open-label, randomised, multicentre phase 2 trial. Lancet . 2013;381(9883):2100–7.
Lawitz E, Lalezari JP, Hassanein T, Kowdley KV, Poordad FF, Sheikh AM, et al. Sofosbuvir in combination with peginterferon alfa-2a and ribavirin for non-cirrhotic, treatment-naive patients with genotypes 1, 2, and 3 hepatitis C infection: a randomised, double-blind, phase 2 trial. Lancet Infect Dis. 2013;13(5):401–8.
Afdhal N, Zeuzem S, Kwo P, Chojkier M, Gitlin N, Puoti M, et al. Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N Engl J Med. 2014;370(20):1889–98.
Afdhal N, Reddy KR, Nelson DR, Lawitz E, Gordon SC, Schiff E, et al. Ledipasvir and sofosbuvir for previously treated HCV genotype 1 infection. N Engl J Med. 2014;370(16):1483–93.
Rezaee-Zavareh MS, Hesamizadeh K, Behnava B, Alavian SM, Gholami-Fesharaki M, Sharafi H. Combination of Ledipasvir and Sofosbuvir for treatment of hepatitis C virus genotype 1 infection: systematic review and meta-analysis. Ann Hepatol. 2017;16(2):188–97.
Alavian SM, Hajarizadeh B, Bagheri Lankarani K, Sharafi H, Ebrahimi Daryani N, Merat S, et al. Recommendations for the clinical management of hepatitis C in Iran: a consensus-based national guideline. Hepat Mon. 2016;16(8):e40959.
Alavian SM, Rezaee-Zavareh MS. Daclatasvir-based treatment regimens for hepatitis C virus infection: a systematic review and meta-analysis. Hepat Mon. 2016;16(9):e41077.
Flisiak R, Janczewska E, Wawrzynowicz-Syczewska M, Jaroszewicz J, Zarebska-Michaluk D, Nazzal K, et al. Real-world effectiveness and safety of ombitasvir/paritaprevir/ritonavir +/- dasabuvir +/- ribavirin in hepatitis C: AMBER study. Aliment Pharmacol Ther. 2016;44(9):946–56.
Kwo P, Gitlin N, Nahass R, Bernstein D, Etzkorn K, Rojter S, et al. Simeprevir plus sofosbuvir (12 and 8 weeks) in hepatitis C virus genotype 1-infected patients without cirrhosis: OPTIMIST-1, a phase 3, randomized study. Hepatology. 2016;64(2):370–80.
Sperl J, Horvath G, Halota W, Ruiz-Tapiador JA, Streinu-Cercel A, Jancoriene L, et al. Efficacy and safety of elbasvir/grazoprevir and sofosbuvir/pegylated interferon/ribavirin: A phase III randomized controlled trial. J Hepatol. 2016;65(6):1112–9.
Roth D, Nelson DR, Bruchfeld A, Liapakis A, Silva M, Monsour Jr H, et al. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4-5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet. 2015;386(10003):1537–45.
Alavian SM, Rezaee-Zavareh MS. The Middle East and hepatitis C virus infection: does it need special attention? Lancet Infect Dis. 2016;16(9):1006–7.
Pearlman BL, Ehleben C, Perrys M. The combination of simeprevir and sofosbuvir is more effective than that of Peginterferon, Ribavirin, and Sofosbuvir for patients with hepatitis C–related Child’s class a cirrhosis. Gastroenterology. 2015;148(4):762–70. e2.
Acknowledgements
Not applicable
Funding
There was not any financial support for this study. This manuscript is the outcome of a financially non-supported study.
Availability of data and materials
Datasets analyzed during the current study available from the corresponding author on reasonable request.
Authors’ contributions
SMA participate in design of study and supervised whole study and revised the paper critically for important intellectual content. BB completed literature bibliography and reviewed data. MSR-Z reviewed data, conducted meta-analysis, drafted and edited the paper. MG-F reviewed data and conducted meta-analysis. HK-S participated in acquisition of data. HS completed literature bibliography, reviewed all data and drafted and revised some parts of the paper. FD participated in literature bibliography, acquisition of data, drafted and revised some parts of the paper. All authors read and approved the final version of manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable
Ethics approval and consent to participate
Not applicable
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Appendix. Search strategies. (DOC 26 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dolatimehr, F., Karimi-Sari, H., Rezaee-Zavareh, M.S. et al. Combination of sofosbuvir, pegylated-interferon and ribavirin for treatment of hepatitis C virus genotype 1 infection: a systematic review and meta-analysis. DARU J Pharm Sci 25, 11 (2017). https://doi.org/10.1186/s40199-017-0177-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40199-017-0177-x