Abstract
Current debate in type 2 diabetes (T2DM) has focused on shortened leukocyte telomere length (LTL) as the result of a number of possible causes, including polymorphisms in mitochondrial uncoupling proteins (UCPs) leading to oxidative stress, telomere regulatory pathway gene polymorphisms, or as a direct result of associated cardiovascular complications inducing tissue organ inflammation and oxidative stress. There is evidence that a heritable shorter telomere trait is a risk factor for development of T2DM. This review discusses the contribution and balance of genetic regulation of UCPs and telomere pathways in the context of T2DM. We discuss genotypes that are well known to influence the shortening of LTL, in particular OBFC1 and telomerase genotypes such as TERC. Interestingly, the interaction between short telomeres and T2DM risk appears to involve mitochondrial dysfunction as an intermediate process. A hypothesis is presented that genetic heterogeneity within UCPs may directly affect oxidative stress that feeds back to influence the fine balance of telomere regulation, cell cycle regulation and diabetes risk and/or metabolic disease progression.
Similar content being viewed by others
Telomere length varies from 4–20 kb in humans and telomere shortening is thought to be key mechanistic event in cellular aging [1–3]. Shorter telomeres have been described as a risk factor for many age related chronic conditions [4], including T2DM [5–7]. A current debate concerns whether shorter telomeres are a heritable trait [8], or a consequence of an associated disease process [9, 10] or, in fact due to an age related dysfunction in telomere regulation [11, 12]. Changes in telomere length associated with type 2 diabetes (T2DM) and interactions between mitochondrial function and telomeres represent possible translational targets to treat T2DM by restoring telomere length [13–16].
Leukocyte telomere length (LTL) is associated with metabolic disease and cardiovascular risk factors
There is certainly a growing trend to report telomere length in population studies that encompass traditional metabolic and cardiovascular risk factors. The large community population Framingham heart study has demonstrated that cardiovascular risk factors such as hypertension and/or insulin resistance are associated with shorter human LTLs [17]. Shortened LTLs have been observed in patients with metabolic syndrome with impaired glycaemic control and increased waist-to-hip ratio [18]. Impaired glycaemic control in both clinical and translational studies, have been associated with increased cellular oxidative stress [19].
Oxidative stress and LTL in metabolic disease
Diabetes complicated by cardiovascular disease is associated with increased mortality and higher levels of oxidative stress and inflammation, which may accelerate telomere shortening and associated premature cell senescence [20–22]. Importantly, mitochondrial oxidative stress appears to be required to maintain cellular senescence [23]. Additionally, in cancer biology short telomere dysfunction has been associated with a tissue decrease in mitochondrial DNA copy number and, importantly, a decrease in mitochondrial bio-energetic function [24], emphasizing a close inter-relationship between oxidative stress, mitochondrial bio-energetic coupling and telomere length [25–27]. On the other hand, such associations have not been well explored in diabetes. These biological factors influencing regulatory telomere pathways would be amenable to genetic analysis, particularly in populations at risk, such as those that have developed T2DM, with and without cardiovascular risk factors.
Do short telomeres cause and/or influence progress of T2DM metabolic syndrome?
It is generally accepted that shortened telomeres may independently contribute to clinical metabolic syndrome progression via directly affecting cellular metabolic rate and influencing neighboring cell function [28–30]. For example, short telomeres may affect pancreatic β-cell metabolism directly [7]. In T2DM, studies have demonstrated a reduction in both global β-cell signaling and production of insulin in the setting of pancreatic cell senescence [7]. However, the relationship between LTL and obesity [31] and diabetes [32] has been questioned. The severity of disease complications may also interact with telomere length regulation. For example, in T2DM with complications such as a previous myocardial infarction (MI), telomere length is shorter, compared to the presence of T2DM without MI per se [18].
Is the interaction between telomere length and T2DM influenced by genetic variation?
Several studies have reported positive associations between LTL and T2DM. LTL has been shown to be shorter in patients with T2DM and also correlates with time of onset and duration of disease [19, 33, 34]. However, a Chinese population-based study found no relationship between LTL and either the time of onset or the duration of T2DM [35]. Mechanisms other than diabetes may be responsible for shorter telomeres in a Chinese population. Genetic regulation of telomeres could potentially explain telomere shortening and an increased risk for T2DM. Current conceptual thinking is that shorter telomeres may predispose to, or accelerate, biological aging-related disease by underpinning a bidirectional cause-and-effect relationship between disease and telomere length [36]. Possible mechanisms that could result in bidirectional changes in both metabolic disease progression and telomere shortening would be functional expression or activity changes in telomere length-related genes and pathways and alterations in cellular oxidative stress.
Uncoupling protein association
The three common isotypes of UCP are UCP1, mainly expressed in brown adipose tissue, UCP2, expressed widely in most cells and UCP3, expressed mainly in striated muscle [37]. UCP2 has been implicated in diabetes risk and interactions with telomere-pathways [13, 38].
UCPs are located in the inner mitochondrial membrane and mediate proton leakage, to regulate the production of ATP and reduce oxidative stress [37, 39]. The high degree of homology at the nucleotide level and the conservation of the exon/intron boundaries among the key UCP genes (UCP1, UCP2, UCP3) suggests they may have evolved from a common ancestor or are the result of gene duplication events [40]. Peroxisome proliferator-activated receptors (PPARs) are ligand-activated transcription factors involved in the regulation of glucose/lipid metabolism [41] and are pivotal in the control of transcription of the UCP family of genes [42, 43] Interestingly, pre-clinical studies in Otsuka Long-Evans Tokushima fatty (OLETF) rats, that develop T2DM, have shown that PPAR-γ is also effective at elevating telomerase activity and telomere-associated proteins [41], ameliorating the effects of T2DM on telomere shortening.
Two studies have explored the association between the UCP2 gene variant −866G < A (rs659366), T2DM and telomere length [13, 38]. One study covered a range of ethnic backgrounds [13] (Caucasian, South Asian and Afro-Caribbean) while the other focused on a Han Chinese population [38]. LTL and the −866G < A UCP2 variant were found to be independent risk factors for T2DM [38]. The −866G < A UCP2 variant was also particularly related to shorter LTL in patients [13]. These studies were some of the first to suggest a possible association between the efficiency of mitochondrial UCP regulation of reactive oxygen species [44, 45] and shorter telomere length in T2DM.
Telomerase and shelterin association
Eukaryotic chromosome stability requires telomere maintenance by the RNA-protein telomerase complex, which is responsible for reverse transcriptase activity for the maintenance of telomere ends, by adding DNA sequence repeats [46]. The telomerase holoenzyme is composed of both protein and RNA, i.e. telomeric reverse transcriptase (TERT), telomeric RNA component (TERC) and other factors, e.g. telomerase protein component 1 (TEP1). The function of telomerase relies on proper expression, maturation, trafficking and assembly of these components [47]. TERT is the catalytic subunit of the enzyme telomerase that catalyses the addition of multiple 6 bp (TTAGGG) telomere repeats, using TERC as a template [48]. TEP1 is a component that facilitates telomerase activity.
Moreover, the shelterin complex is recognized as being important for the protection of telomeres and for the regulation of telomerase activity [49]. Shelterin is comprised of six important components: telomere repeat factor 1 and 2 (TRF1 and TRF2), protection of telomere 1 (POT1), repressor/activator protein 1 (RAP1), TRF1- and TRF2- interacting nuclear protein 2 (TIN2), and tripeptidyl-peptidase 1 (TPP1) [50]. The TEL-patch of amino acids, on the oligonucleotide/oligosaccharide-binding folds of the shelterin component TPP1 is essential to recruit telomerase to telomeres [50]. While important, there is a paucity of basic biological understanding of how the shelterin complex components may interact with mitochondrial function and induce insulin resistance [51, 52], although TIN2 has been shown to be post-translationally processed in mitochondria and regulates mitochondrial oxidative phosphorylation [53].
Zee and associates explored 11 telomere pathway genes and their relationship to development of T2DM in a longitudinal cohort of 22,715 healthy middle-aged Caucasian females, free of diabetes or cardiovascular disease at baseline [54]. Gene pathways explored in this cohort were telomere maintenance genes, all selected on the basis of having had a prior association with LTL. During a follow-up period of 13 years, 1445 participants developed T2DM. Results showed that, using haplotype-block analysis, there is an association between several pre-specified haplotypes of TRF1 and TEP1 with T2DM risk. When SNPs were considered individually, SNPs (four each from TRF1 and TEP1 and one each from TPP1 and TRF2) had differential association with T2DM risk. Only one SNP–TRF2 rs4783704, remained significant after correction for repeated measures. Absolute changes in LTL were unfortunately not determined in this study.
Telomerase specifically recognizes and elongates the ends of telomeres using the RNA molecule template, TERC [55]. TERC is known to be essential for telomere homeostasis [48]. Clinical and epidemiological studies have revealed that mutations in TERC lead to premature telomere shortening and limited TERC activity result in accelerated shortening of telomere [56, 57]. Shen and associates have explored telomere pathway genes in relation to T2DM, in particular two SNPs, rs12696304 and rs16847897, located near TERC at 3q26 [58]. These SNPs were examined in 4016 Shanghai Han Chinese participants; 1936 T2DM patients and 2080 healthy controls. Both of these major alleles in regression models were associated with between 3 years (rs12696304) and 4 years (rs16847897) of advanced age-related telomere attrition adjusted for diabetes status [58]. In summary, these two TERC-related SNPs correlate with LTL of both T2DM patients and controls. Moreover, data from functional studies, where TERC is knocked down or overexpressed using exogenous mutated TERC, suggest non-telomere maintenance functions for TERC, such as cell cycle control and p53-dependant pathway activation [59, 60]. p53 pathways are of interest as they provide a mechanism linking mitochondrial damage, ROS production and DNA damage responses, and related cellular growth arrest phenotypes during cellular senescence [61–63]. Thus, it is not surprising to find that a TERC SNP related to both increased cardiovascular disease and also T2DM is characterized by cellular senescence.
Genome-wide association studies’ findings
General population studies have identified several genes through genome-wide association studies as a locus for cross-sectional individual variation in LTL [64, 65]. A novel relative telomere length locus at chromosome 16q21, an intronic variant (rs74019828) in the CSNK2A2 (Casein Kinase 2, Alpha Prime Polypeptide) gene, was found in South Asians [65]. Phosphorylation by CSNK2A2 plays an important role for regulation of telomere length homoeostasis [63]. Oligonucleotide/oligosaccharide-binding folds containing 1 (OBFC1) is involved in the initiation of DNA replication and also functions in a telomere-associated complex [66]. Several GWAS studies have associated OBFC1 with LTL [64, 67]. In the latter population study, an OBFC1 genotype (rs4387287) was found to be associated with both T2DM and LTL, where the mean difference in LTL across the homozygous genotypes approximates 400 bp in men and 180 bp in women [64]. The OBFC1 genotype (rs4387287) is associated with a defined rate of LTL shortening in the general population, circa 20–30 bp/year [68]. OBFC1 is of particular relevance since although it is unrelated to oxidative stress or mitochondrial function, it is directly engaged in telomere biology [64, 69], suggesting that OBFC1 is able to regulate telomere length and/or function [64].
The relevance of OBFC1 is supported by the finding of Maubaret et al. [70], where an OBFC1 haplotype (rs10786775G and rs11591710C) was associated with lower risk of coronary heart disease. They also found a TERC haplotype (rs12696304G, rs10936601T and rs16847897C) was associated with both a lower risk of coronary heart disease and T2DM.
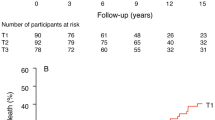
Another independent study also provides positive evidence for the association between OBFC1 and LTL. You et al. examined rs4387287 on the OBFC1 gene, which is associated with LTL, and its association with T2DM development. In addition, another nine genes, including TERT, TERC, TEP1, TRF1, TRF2, POT1, and TPP1 were exmined [71]. The study population examined was 82,069 ethnically diverse postmenopausal women who had no prior history of chronic diseases (including diabetes or cardiovascular disease), of which over 6 years of follow-up 1675 developed T2DM. Overall, You et al. concluded that LTL was found to be weakly associated with diabetes risk but was not independent from known epidemiological risk factors.
In summary, this review suggests that short LTL has been identified in a limited number of population studies as a risk factor for the development of T2DM. The shortening of LTL relates to both OBFC1 genotypes and telomerase genotypes such as TERC. Interestingly, the interaction between short telomeres and T2DM risk appears to involve mitochondrial dysfunction as an intermediate process, suggesting a mitochondrial axis where underlying gene regulation of telomerase-related pathways is important. We suggest that genetic heterogeneity within UCPs may directly affect oxidative stress that feeds back to influence the fine balance of telomere regulation and cell cycle regulation. This in turn may, in part, be related to both the development of T2DM and enhancing the rate of complications once the disease is present. The interaction of cardiovascular disease in association with the development of T2DM is important and is likely to associate with some genetic components of telomere regulation, but not with all. Overall, the accumulated data in this review illustrates the emerging influence of genetic factors on LTL and T2DM and interplay with mitochondrial function. We suggest that there is a likely need to explore the biological and pathological interactions between UCP, telomerase and shelterin regulatory pathways. These studies are required to adequately describe the precise role of mitochondria on LTL shortening with respect to both acute and chronic pathological events. A greater understanding of the genetic influences on telomere length and T2DM is likely to facilitate risk stratification amongst patients, as genomics is progressively embraced as a clinical tool in the management of this chronic illness.
References
Lesnefsky EJ, Moghaddas S, Tandler B, Kerner J, Hoppel CL (2001) Mitochondrial dysfunction in cardiac disease: ischemia-reperfusion, aging, and heart failure. J Mol Cell Cardiol 33(6):1065–1089. doi:10.1006/jmcc.2001.1378
Lemasters JJ (2005) Selective mitochondrial autophagy, or mitophagy, as a targeted defense against oxidative stress, mitochondrial dysfunction, and aging. Rejuvenation Res 8(1):3–5. doi:10.1089/rej.2005.8.3
Blasco MA (2007) Telomere length, stem cells and aging. Nat Chem Biol 3(10):640–649. doi:10.1038/nchembio.2007.38
Sanders JL, Newman AB (2013) Telomere length in epidemiology: a biomarker of aging, age-related disease, both, or neither? Epidemiol Rev 35:112–131. doi:10.1093/epirev/mxs008
Monickaraj F, Aravind S, Gokulakrishnan K, Sathishkumar C, Prabu P, Prabu D et al (2012) Accelerated aging as evidenced by increased telomere shortening and mitochondrial DNA depletion in patients with type 2 diabetes. Mol Cell Biochem 365(1–2):343–350. doi:10.1007/s11010-012-1276-0
Price LH, Kao HT, Burgers DE, Carpenter LL, Tyrka AR (2013) Telomeres and early-life stress: an overview. Biol Psychiatry 73(1):15–23. doi:10.1016/j.biopsych.2012.06.025
Guo N, Parry EM, Li LS, Kembou F, Lauder N, Hussain MA et al (2011) Short telomeres compromise beta-cell signaling and survival. PLoS One 6(3):e17858. doi:10.1371/journal.pone.0017858
Armanios M, Alder JK, Parry EM, Karim B, Strong MA, Greider CW (2009) Short telomeres are sufficient to cause the degenerative defects associated with aging. Am J Hum Genet 85(6):823–832. doi:10.1016/j.ajhg.2009.10.028
Butt HZ, Atturu G, London NJ, Sayers RD, Bown MJ (2010) Telomere length dynamics in vascular disease: a review. Eur J Vasc Endovasc Surg 40(1):17–26. doi:10.1016/j.ejvs.2010.04.012
Panossian LA, Porter VR, Valenzuela HF, Zhu X, Reback E, Masterman D et al (2003) Telomere shortening in T cells correlates with Alzheimer’s disease status. Neurobiol Aging 24(1):77–84
Armanios M (2009) Syndromes of telomere shortening. Annu Rev Genomics Hum Genet 10:45–61. doi:10.1146/annurev-genom-082908-150046
Feldser DM, Hackett JA, Greider CW (2003) Telomere dysfunction and the initiation of genome instability. Nat Rev Cancer 3(8):623–627. doi:10.1038/nrc1142
Salpea KD, Talmud PJ, Cooper JA, Maubaret CG, Stephens JW, Abelak K et al (2010) Association of telomere length with type 2 diabetes, oxidative stress and UCP2 gene variation. Atherosclerosis 209(1):42–50. doi:10.1016/j.atherosclerosis.2009.09.070
Lowell BB, Shulman GI (2005) Mitochondrial dysfunction and type 2 diabetes. Science 307(5708):384–387. doi:10.1126/science.1104343
Kelley DE, He J, Menshikova EV, Ritov VB (2002) Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 51(10):2944–2950
Mulder H (2010) Is shortening of telomeres the missing link between aging and the Type 2 Diabetes epidemic? Aging 2(10):634–636
Demissie S, Levy D, Benjamin EJ, Cupples LA, Gardner JP, Herbert A et al (2006) Insulin resistance, oxidative stress, hypertension, and leukocyte telomere length in men from the Framingham Heart Study. Aging Cell 5(4):325–330. doi:10.1111/j.1474-9726.2006.00224.x
Olivieri F, Lorenzi M, Antonicelli R, Testa R, Sirolla C, Cardelli M et al (2009) Leukocyte telomere shortening in elderly Type2DM patients with previous myocardial infarction. Atherosclerosis 206(2):588–593. doi:10.1016/j.atherosclerosis.2009.03.034
Murillo-Ortiz B, Albarran-Tamayo F, Arenas-Aranda D, Benitez-Bribiesca L, Malacara-Hernandez JM, Martinez-Garza S et al (2012) Telomere length and type 2 diabetes in males, a premature aging syndrome. Aging Male 15(1):54–58. doi:10.3109/13685538.2011.593658
Fyhrquist F, Saijonmaa O, Strandberg T (2013) The roles of senescence and telomere shortening in cardiovascular disease. Nat Rev Cardiol 10(5):274–283. doi:10.1038/nrcardio.2013.30
Mokini Z, Marcovecchio ML, Chiarelli F (2010) Molecular pathology of oxidative stress in diabetic angiopathy: role of mitochondrial and cellular pathways. Diabetes Res Clin Pract 87(3):313–321. doi:10.1016/j.diabres.2009.11.018
Polettini J, Behnia F, Taylor BD, Saade GR, Taylor RN, Menon R (2015) Telomere fragment induced amnion cell senescence: a contributor to parturition? PLoS ONE 10(9):e0137188. doi:10.1371/journal.pone.0137188
Prigione A, Fauler B, Lurz R, Lehrach H, Adjaye J (2010) The senescence-related mitochondrial/oxidative stress pathway is repressed in human induced pluripotent stem cells. Stem Cells 28(4):721–733. doi:10.1002/stem.404
Sahin E, Colla S, Liesa M, Moslehi J, Muller FL, Guo M et al (2011) Telomere dysfunction induces metabolic and mitochondrial compromise. Nature 470(7334):359–365. doi:10.1038/nature09787
Passos JF, von Zglinicki T (2005) Mitochondria, telomeres and cell senescence. Exp Gerontol 40(6):466–472. doi:10.1016/j.exger.2005.04.006
Cui H, Kong Y, Zhang H (2012) Oxidative stress, mitochondrial dysfunction, and aging. J Signal Transduct 2012:646354. doi:10.1155/2012/646354
Sahin E, DePinho RA (2012) Axis of ageing: telomeres, p53 and mitochondria. Nat Rev Mol Cell Biol 13(6):397–404. doi:10.1038/nrm3352
Higuchi Y, Maeda T, Guan JZ, Oyama J, Sugano M, Makino N (2009) Diagonal earlobe crease are associated with shorter telomere in male Japanese patients with metabolic syndrome. Circ J 73(2):274–279
Satoh M, Ishikawa Y, Takahashi Y, Itoh T, Minami Y, Nakamura M (2008) Association between oxidative DNA damage and telomere shortening in circulating endothelial progenitor cells obtained from metabolic syndrome patients with coronary artery disease. Atherosclerosis 198(2):347–353. doi:10.1016/j.atherosclerosis.2007.09.040
Epel ES, Lin J, Wilhelm FH, Wolkowitz OM, Cawthon R, Adler NE et al (2006) Cell aging in relation to stress arousal and cardiovascular disease risk factors. Psychoneuroendocrinology 31(3):277–287. doi:10.1016/j.psyneuen.2005.08.011
Hardikar S, Song X, Risques RA, Montine TJ, Duggan C, Blount PL et al (2015) Obesity and inflammation markers in relation to leukocyte telomere length in a cross-sectional study of persons with Barrett’s esophagus. BMC Obes 2:32. doi:10.1186/s40608-015-0063-3
Menke A, Casagrande S, Cowie CC (2015) Leukocyte telomere length and diabetes status, duration, and control: the 1999–2002 National Health and Nutrition Examination Survey. BMC Endocr Disord 15:52. doi:10.1186/s12902-015-0050-1
Zee RY, Castonguay AJ, Barton NS, Germer S, Martin M (2010) Mean leukocyte telomere length shortening and type 2 diabetes mellitus: a case-control study. Transl Res 155(4):166–169. doi:10.1016/j.trsl.2009.09.012
Sampson MJ, Winterbone MS, Hughes JC, Dozio N, Hughes DA (2006) Monocyte telomere shortening and oxidative DNA damage in type 2 diabetes. Diabetes Care 29(2):283–289
Shen Q, Zhao X, Yu L, Zhang Z, Zhou D, Kan M et al (2012) Association of leukocyte telomere length with type 2 diabetes in mainland Chinese populations. J Clin Endocrinol Metab 97(4):1371–1374. doi:10.1210/jc.2011-1562
Aviv A, Kark JD, Susser E (2015) Telomeres, atherosclerosis, and human longevity: a causal hypothesis. Epidemiology 26(3):295–299. doi:10.1097/EDE.0000000000000280
Rousset S, Alves-Guerra MC, Mozo J, Miroux B, Cassard-Doulcier AM, Bouillaud F et al (2004) The biology of mitochondrial uncoupling proteins. Diabetes 53(Suppl 1):S130–S135
Xiao F, Zheng X, Cui M, Shi G, Chen X, Li R et al (2011) Telomere dysfunction-related serological markers are associated with type 2 diabetes. Diabetes Care 34(10):2273–2278. doi:10.2337/dc10-2431
Jastroch M, Divakaruni AS, Mookerjee S, Treberg JR, Brand MD (2010) Mitochondrial proton and electron leaks. Essays Biochem 47:53–67. doi:10.1042/bse0470053
Lentes KU, Tu N, Chen H, Winnikes U, Reinert I, Marmann G et al (1999) Genomic organization and mutational analysis of the human UCP2 gene, a prime candidate gene for human obesity. J Recept Signal Transduct Res 19(1–4):229–244. doi:10.3109/10799899909036648
Makino N, Maeda T, Oyama J, Higuchi Y, Mimori K (2009) Improving insulin sensitivity via activation of PPAR-gamma increases telomerase activity in the heart of OLETF rats. Am J Physiol Heart Circ Physiol 297(6):H2188–H2195. doi:10.1152/ajpheart.00421.2009
Aubert J, Champigny O, Saint-Marc P, Negrel R, Collins S, Ricquier D et al (1997) Up-regulation of UCP-2 gene expression by PPAR agonists in preadipose and adipose cells. Biochem Biophys Res Commun 238(2):606–611. doi:10.1006/bbrc.1997.7348
Ito E, Ozawa S, Takahashi K, Tanaka T, Katsuta H, Yamaguchi S et al (2004) PPAR-gamma overexpression selectively suppresses insulin secretory capacity in isolated pancreatic islets through induction of UCP-2 protein. Biochem Biophys Res Commun 324(2):810–814. doi:10.1016/j.bbrc.2004.08.238
Almsherqi ZA, McLachlan CS, Slocinska MB, Sluse FE, Navet R, Kocherginsky N et al (2006) Reduced cardiac output is associated with decreased mitochondrial efficiency in the non-ischemic ventricular wall of the acute myocardial-infarcted dog. Cell Res 16(3):297–305. doi:10.1038/sj.cr.7310037
Wang CM, Almsherqi ZA, McLachlan CS, Matthews S, Ramachandran M, Tay S et al (2011) Acute starvation in C57BL/6 J mice increases myocardial UCP2 and UCP3 protein expression levels and decreases mitochondrial bio-energetic function. Stress 14(1):66–72. doi:10.3109/10253890.2010.506931
Chen JL, Greider CW (2003) Template boundary definition in mammalian telomerase. Genes Dev 17(22):2747–2752. doi:10.1101/gad.1140303
Gallardo F, Laterreur N, Wellinger RJ, Chartrand P (2012) Telomerase caught in the act: united we stand, divided we fall. RNA Biol 9(9):1139–1143. doi:10.4161/rna.21498
Njajou OT, Blackburn EH, Pawlikowska L, Mangino M, Damcott CM, Kwok PY et al (2010) A common variant in the telomerase RNA component is associated with short telomere length. PLoS One 5(9):e13048. doi:10.1371/journal.pone.0013048
Diotti R, Loayza D (2011) Shelterin complex and associated factors at human telomeres. Nucleus 2(2):119–135. doi:10.4161/nucl.2.2.15135
Schmidt JC, Dalby AB, Cech TR (2014) Identification of human TERT elements necessary for telomerase recruitment to telomeres. Elife. doi:10.7554/eLife.03563
Sullivan LB, Santos JH, Chandel NS (2012) Mitochondria and telomeres: the promiscuous roles of TIN2. Mol Cell 47(6):823–824. doi:10.1016/j.molcel.2012.09.006
Martinez P, Gomez-Lopez G, Garcia F, Mercken E, Mitchell S, Flores JM et al (2013) RAP1 protects from obesity through its extratelomeric role regulating gene expression. Cell Rep 3(6):2059–2074. doi:10.1016/j.celrep.2013.05.030
Chen LY, Zhang Y, Zhang Q, Li H, Luo Z, Fang H et al (2012) Mitochondrial localization of telomeric protein TIN2 links telomere regulation to metabolic control. Mol Cell 47(6):839–850. doi:10.1016/j.molcel.2012.07.002
Zee RY, Ridker PM, Chasman DI (2011) Genetic variants of 11 telomere-pathway gene loci and the risk of incident type 2 diabetes mellitus: the Women’s Genome Health Study. Atherosclerosis 218(1):144–146. doi:10.1016/j.atherosclerosis.2011.05.013
Blasco MA (2005) Telomeres and human disease: ageing, cancer and beyond. Nat Rev Genet 6(8):611–622. doi:10.1038/nrg1656
Du HY, Pumbo E, Ivanovich J, An P, Maziarz RT, Reiss UM et al (2009) TERC and TERT gene mutations in patients with bone marrow failure and the significance of telomere length measurements. Blood 113(2):309–316. doi:10.1182/blood-2008-07-166421
Goldman F, Bouarich R, Kulkarni S, Freeman S, Du HY, Harrington L et al (2005) The effect of TERC haploinsufficiency on the inheritance of telomere length. Proc Natl Acad Sci USA 102(47):17119–17124. doi:10.1073/pnas.0505318102
Shen Q, Zhang Z, Yu L, Cao L, Zhou D, Kan M et al (2011) Common variants near TERC are associated with leukocyte telomere length in the Chinese Han population. Eur J Hum Genet 19(6):721–723. doi:10.1038/ejhg.2011.4
Kedde M, le Sage C, Duursma A, Zlotorynski E, van Leeuwen B, Nijkamp W et al (2006) Telomerase-independent regulation of ATR by human telomerase RNA. J Biol Chem 281(52):40503–40514. doi:10.1074/jbc.M607676200
Li S, Rosenberg JE, Donjacour AA, Botchkina IL, Hom YK, Cunha GR et al (2004) Rapid inhibition of cancer cell growth induced by lentiviral delivery and expression of mutant-template telomerase RNA and anti-telomerase short-interfering RNA. Cancer Res 64(14):4833–4840. doi:10.1158/0008-5472.CAN-04-0953
Macip S, Igarashi M, Fang L, Chen A, Pan ZQ, Lee SW et al (2002) Inhibition of p21-mediated ROS accumulation can rescue p21-induced senescence. EMBO J 21(9):2180–2188. doi:10.1093/emboj/21.9.2180
da Silva GN, de Castro Marcondes JP, de Camargo EA, da Silva Passos GA Jr, Sakamoto-Hojo ET, Salvadori DM (2010) Cell cycle arrest and apoptosis in TP53 subtypes of bladder carcinoma cell lines treated with cisplatin and gemcitabine. Exp Biol Med 235(7):814–824. doi:10.1258/ebm.2010.009322
Luo H, Rankin GO, Li Z, Depriest L, Chen YC (2011) Kaempferol induces apoptosis in ovarian cancer cells through activating p53 in the intrinsic pathway. Food Chem 128(2):513–519. doi:10.1016/j.foodchem.2011.03.073
Levy D, Neuhausen SL, Hunt SC, Kimura M, Hwang SJ, Chen W et al (2010) Genome-wide association identifies OBFC1 as a locus involved in human leukocyte telomere biology. Proc Natl Acad Sci USA 107(20):9293–9298. doi:10.1073/pnas.0911494107
Saxena R, Bjonnes A, Prescott J, Dib P, Natt P, Lane J et al (2014) Genome-wide association study identifies variants in casein kinase II (CSNK2A2) to be associated with leukocyte telomere length in a Punjabi Sikh diabetic cohort. Circ Cardiovasc Genet 7(3):287–295. doi:10.1161/CIRCGENETICS.113.000412
Wan M, Qin J, Songyang Z, Liu D (2009) OB fold-containing protein 1 (OBFC1), a human homolog of yeast Stn1, associates with TPP1 and is implicated in telomere length regulation. J Biol Chem 284(39):26725–26731. doi:10.1074/jbc.M109.021105
Lee JH, Cheng R, Honig LS, Feitosa M, Kammerer CM, Kang MS et al (2013) Genome wide association and linkage analyses identified three loci-4q25, 17q23.2, and 10q11.21-associated with variation in leukocyte telomere length: the Long Life Family Study. Front Genet 4:310. doi:10.3389/fgene.2013.00310
Aviv A, Chen W, Gardner JP, Kimura M, Brimacombe M, Cao X et al (2009) Leukocyte telomere dynamics: longitudinal findings among young adults in the Bogalusa Heart Study. Am J Epidemiol 169(3):323–329. doi:10.1093/aje/kwn338
Flynn RL, Zou L (2010) Oligonucleotide/oligosaccharide-binding fold proteins: a growing family of genome guardians. Crit Rev Biochem Mol Biol 45(4):266–275. doi:10.3109/10409238.2010.488216
Maubaret CG, Salpea KD, Romanoski CE, Folkersen L, Cooper JA, Stephanou C et al (2013) Association of TERC and OBFC1 haplotypes with mean leukocyte telomere length and risk for coronary heart disease. PLoS One 8(12):e83122. doi:10.1371/journal.pone.0083122
You NC, Chen BH, Song Y, Lu X, Chen Y, Manson JE et al (2012) A prospective study of leukocyte telomere length and risk of type 2 diabetes in postmenopausal women. Diabetes 61(11):2998–3004. doi:10.2337/db12-0241
Authors’ contributions
All authors have made substantial contributions to conception and design and drafting of the manuscript; CM conceived the idea for the manuscript, and drafted the initial manuscript with ZN, YL reviewed initial drafts for technical compliance and provided review of references, YZ contributed to the final drafts with BH and expanded upon review. BH and CM made the final edits to the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zhou, Y., Ning, Z., Lee, Y. et al. Shortened leukocyte telomere length in type 2 diabetes mellitus: genetic polymorphisms in mitochondrial uncoupling proteins and telomeric pathways. Clin Trans Med 5, 8 (2016). https://doi.org/10.1186/s40169-016-0089-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40169-016-0089-2