Abstract
Background
It has been shown in laboratory experiments using human subjects that ingestion of the non-essential amino acid l-serine before bedtime enhances the advance of circadian phase induced by light exposure the next morning. In the present study, we tested the effect of ingestion of l-serine before bedtime on circadian phase in real life and whether its effect depends on the initial circadian phase.
Methods
The subjects were 33 healthy male and female university students and they were divided into an l-serine group (n = 16) and a placebo group (n = 17). This study was conducted in a double-blind manner in autumn and winter. After a baseline period for 1 week, the subjects took 3.0 g of l-serine or a placebo 30 min before bedtime for 2 weeks. Saliva was collected twice a week at home every hour under a dim light condition from 20:00 to 1 h after habitual bedtime. Dim light melatonin onset (DLMO) was used as an index of phase of the circadian rhythm.
Results
DLMO after intervention was significantly delayed compared to the baseline DLMO in the placebo group (p = 0.02) but not in the l-serine group. There was a significant difference in the amount of changes in DLMO between the two groups (p = 0.04). There were no significant changes in sleeping habits after intervention in the two groups. There were significant positive correlations between advance of DLMO and DLMO before intervention in the l-serine group (r = 0.53, p < 0.05) and the placebo group (r = 0.69, p < 0.01). There was no significant difference in the slopes of regression lines between the two groups (p = 0.71), but the intercept in the l-serine group was significantly higher than that in the placebo group (p < 0.01). The levels of light exposure were not significantly different between the two groups.
Conclusions
Our findings suggest that intake of l-serine before bedtime for multiple days might attenuate the circadian phase delay in the real world and that this effect does not depend on the initial circadian phase.
Trial registration
This study is registered with University Hospital Medical Information Network in Japan (UMIN000024435. Registered on October 17, 2016).
Similar content being viewed by others
Background
The intrinsic period of the human circadian rhythm is longer than 24 h, and morning light plays an important role in resetting the circadian rhythm to 24 h [1, 2]. On the other hand, light at night from artificial lighting causes delays in sleep timing and circadian rhythm phases through non-visual effects of light [3,4,5]. In modern society, circadian phase delays can also be caused by nighttime digital media use [6, 7] and night work [8]. Since disruption of circadian rhythms due to these factors results in various negative health outcomes including insomnia, mood disorders, obesity, and type 2 diabetes, some countermeasures are needed [8, 9].
l-Serine is a non-essential amino acid synthesized in the body. It is also a precursor for the synthesis of other amino acids including the optical isomers D-serine and glycine as well as lipids and nucleotides [10] and it plays a role in mediating the nutritional supply for neuroglial cells [11, 12]. Furthermore, recent studies have shown that l-serine is involved in improvement of depression [13], Alzheimer’s disease [14], and amyotrophic lateral sclerosis (ALS) [15]. Those studies indicate that both l-serine biosynthesis and external ingestion are important for biological functions. Moreover, a previous study in which sleep quality was evaluated by using wrist actigraphy and self-reporting questionnaires showed that l-serine administration improved the subjective feeling of sleep and tended to decrease the number of nighttime awakenings in humans [16].
The results showing improved sleep quality in that previous study might be due to a contribution of l-serine to circadian entrainment. Our previous study [17] using mice and healthy human subjects showed that light exposure after administration of l-serine affected the phase shift of circadian rhythms. In the experiments using mice, we found that light-induced wheel-running phase shifts in mice that were administrated l-serine were greater than those in mice administrated water.
In a double-blind crossover test using twenty-one human subjects, subjects with a single intake of l-serine (3.0 g) before bedtime showed a significant circadian phase advance by bright light exposure in the morning (2000 lx, 90 min) compared with that in subjects in the placebo condition. The findings in our laboratory study indicate that l-serine may have the potential to promote light-induced circadian phase advance in humans. However, it was not clear whether the same results could be obtained in real life.
Therefore, in this study, we investigated whether l-serine intake before bedtime promotes circadian phase advance in real life. Since there are large individual differences in the circadian phase in humans in real life [18, 19], we also examined whether the effect of l-serine depends on the individual initial phase of the subject.
Methods
Participants and protocol
This study was conducted in Japan (Fukuoka City) in October and December. Thirty-three healthy university students participated in this study. None of the subjects were engaged in shift work or night shifts during the experimental period. We confirmed that melatonin secretion in all subjects started before the usual bedtime. The subjects were divided into two groups: a placebo group (13 men and 4 women, 22.1 ± 2.5 years old) and an l-serine group (10 men and 6 women, 21.3 ± 1.9 years old). Table 1 shows the characteristics of subjects in each group. All of subjects were Asian living in Fukuoka City, Japan. Chronotype was determined by the Japanese version of Morningness-Eveningness Questionnaire (MEQ) [20, 21]. There was no significant difference in sex ratio, age, or chronotype between the two groups. In addition, subjects answered their sleep habits on the Japanese version of the Munich ChronoType Questionnaire (MCTQ) [22] on their school days and free days. No significant differences were found between the two groups about all parameters of sleep habits. This study was carried out with the approval of the Ethics Committee of Kyushu University. The subjects were given oral and written explanations, and written consent for participation in the study was obtained.
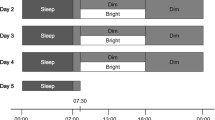
The experiment was conducted in a double-blind manner. The experiment consisted of a 1-week baseline period and a 2-week intervention period. After the start of the intervention, the subjects in each group ingested l-serine (3.0 g) or a placebo (Trehalose, 3.0 g) dissolved in 100 ml of water 30 min before bedtime every day. The intake dose was the same as that used in a previous study [16, 17]. The subjects were asked to keep their habitual sleep-wake schedule during the experiment. Excessive alcohol drinking and ingestion of sleeping pills were prohibited. The subjects were asked to record their sleep diary and wear a wrist actigraph device (MotionWatch 8, CamNtech, Cambridge, UK) for 24 h to determine their daily sleep-wake schedule and daily light exposure. The average illuminance of light exposure was log-transformed and calculated 5 h after the average wake time and 5 h before the average bedtime before and during the intervention period.
Saliva samples for melatonin assays were collected by each subject at home twice a week (on Thursday and Sunday). The subjects were forbidden from ingesting caffeine and performing strenuous exercise on the day of saliva collection. Saliva samples were collected every hour from 20:00 to each subject’s bedtime using a cotton swab (Salivatte® Sarstedt, Germany) under dim light in their home. The subjects were instructed to use an incandescent light bulb as indirect lighting from 19:30 in the room to make dim light (< 15 lx as measured by MotionWatch8). The subjects were also instructed to send a text message to the experimenter immediately after saliva collection.
Melatonin concentration in saliva was quantified by a radioimmunoassay (Buhlmann, RK-DSM2, Switzerland). Dim light melatonin onset (DLMO), a reliable marker of circadian phase [23, 24], was determined by linear interpolation between the time points before and after the melatonin concentration increased and stayed above the 3.0 pg/mL threshold [25].
Statistical analysis
One subject who showed an irregular sleep/wake schedule was excluded from the analysis. Even after exclusion, there was still no significant difference in sex ratio, age, chronotype or sleep habits between the two groups. Another subject whose wearing time of the actigraph device during the day was too short for accurate determination of light exposure was also excluded from the analysis.
In the statistical analysis, a two-sided, Welch’s t test was used for comparison of sleep habits, DLMO, amount of DLMO advance, and light exposure between the two groups. A two-sided paired t test was used for investigating changes in sleep habits and DLMO within the groups. Greenhouse–Geisser correction was performed whenever Mauchly’s test of sphericity was significant. Pearson’s correlation test was used to assess the relation between DLMO before intervention and DLMO advance in each group. Afterwards, the general linear model (GLM) was used for comparison of the slopes and intercepts of regression lines between the two groups. A p value less than 0.05 was considered statistically significant. Statistical analyses were performed using SPSS software ver. 25 (IBM, NY, USA).
Results
There were no significant differences in bedtime (p = 0.47), wake time (p = 0.55), time in bed (p = 0.98), and DLMO (p = 0.26) between the two groups before intervention (Table 2 and Fig. 1). A significant difference before and after intervention was found for DLMO in the placebo group but not in the l-serine group (Table 2). DLMO in the placebo group was significantly delayed after intervention (t = − 2.59, p < 0.05). No significant changes in sleep measurements after intervention were found in the two groups.
The magnitudes of changes after intervention were compared in the placebo group and l-serine group (Table 3). A significant difference in changes in DLMO was found between the two groups (placebo < l-serine, t = − 2.14, p = 0.04) (Table 3 and Fig. 2).
Figure 3 shows the results for mean light exposure. No significant differences were found after wake time before intervention (p = 0.89), after wake time during intervention (p = 0.84), before bedtime before intervention (p = 0.90), and before bedtime during intervention (p = 0.58).
Figure 4 shows the relationship between DLMO before intervention and DLMO advance. There were significant positive correlations between the advance of DLMO and DLMO before intervention in the l-serine group (r = 0.53, p < 0.05) and the placebo group (r = 0.69, p < 0.01).
The GLM with groups as a dependent variable and DLMO before intervention as a between-subject factor was used to test independence of DLMO before intervention. The main effect of groups was not statistically significant (p = 0.26), and independence of DLMO before intervention was thus confirmed. The GLM with DLMO advance as a dependent variable, groups as a between-subject factor and DLMO before intervention as a covariate was used to compare the slopes of regression lines. The interaction between groups and DLMO before intervention was not statistically significant (p = 0.71). Therefore, it was confirmed that there was no significant difference in slopes of regression lines. The GLM without interaction between groups and DLMO before intervention was used to test the significance of regression and to compare the intercepts of regression lines. The effect of DLMO before intervention was statistically significant (p < 0.001), and the significance of regression was therefore confirmed. Moreover, the main effect of groups was statistically significant (ηp2 = 0.30, p < 0.01). This means that the intercept of the regression line in the l-serine group was significantly greater than that in the placebo group.
Discussion
In this study, a significant delay in DLMO was confirmed in the placebo group but not in the l-serine group. Moreover, the amount of DLMO changes was significantly different between the two groups. However, given that there were no significant differences between the groups in sex, age, MEQ score, and results for DLMO and sleep habits before the intervention, it is difficult to interpret that the characteristics of the group caused the result of phase delay in the placebo group. Furthermore, the amounts of exposure to daily light just before bedtime and after wake time, which are thought to affect the results of DLMO shift, were not significantly different between the two groups.
In the present study, we showed that l-serine has a preventative effect on the delay of circadian rhythms. However, unlike in the laboratory experiments conducted in our previous study [17], no significant phase advance of the circadian rhythm was observed by l-serine intake before bedtime. One possible reason for this may be the difference in the light environment between the laboratory and field experiments. In the laboratory experiment, evening light (from 6 pm to bedtime) was dim light (< 15 lx), whereas in the field experiment, the subjects were exposed to night light by artificial lighting except on days when saliva samples for melatonin measurement were taken. It is known that artificial lighting at night in real life delays the phase of circadian rhythms [26, 27]. In other words, the lack of phase advance in this study may have been canceled out by phase delay due to exposure to light at night.
Thus, if the effects of night light cannot be avoided in daily life, increasing l-serine intake might be a possible way to induce the phase advance that was observed in the laboratory experiments [17]. However, while a dose-response relationship was observed for the effects of l-serine in a previous animal study [17], no comparison of the effects of increased intake in humans has been conducted. For example, patients with ALS were tested with l-serine at doses of up to 15 g twice daily for 6 months and no serious adverse effects were observed and the drug is generally considered safe [15]. Since l-serine is “generally recognized as safe” by the Food and Drug Administration (FDA), field studies should be conducted in the future to examine the effects of increased doses of l-serine on circadian rhythm phase advance.
In addition to eating behavior, exercise habits have a potential to impact on light-induced circadian phase shift [28]. In many studies, physical activity level was measured by using a wrist accelerometer [29, 30]. However, in the present study, wrist accelerometer data were measured to mainly determine the daily sleep-wake timing and daily light exposure of the subjects and we instructed the subjects to remove the wrist accelerometer during intense exercise to avoid damage to the device. Determination of the interactions between light exposure and physical activity including their timing and intensity in terms of circadian phase shift in daily life would be challenging but is expected to be done in a future study.
We did not expect the delay in DLMO observed in the placebo group. This result means that the phase of the circadian rhythm was delayed in the placebo group, and there could be several reasons for this. First, in the period of October to December, when this experiment was conducted, the time of sunrise is becoming later and the amount of sunshine is less than that in summer in the Northern Hemisphere. It is well known that the light and dark cycle of sunlight is the strongest zeitgeber for circadian rhythm and that morning light is important to reset the human circadian period, which is intrinsically longer than 24 h [1]. Some studies showed that circadian phase in winter was later than that in summer in countries in the Northern Hemisphere [31,32,33]. Next, the subjects in this study were healthy university students. University students generally tend to be night owls biologically and socially [34, 35] and experience relatively little light exposure in the morning and more light exposure later in the day in terms of both intensity and duration [36, 37]. It is possible that these factors affected the easiness for delay of circadian phase in daily life.
In this study, trehalose was used as a placebo. Although animal studies suggested that trehalose has effects in neurodegenerative diseases such as Huntington’s disease [38], Alzheimer’s disease [39], and ALS [40], there has been no study in which the relationship between trehalose ingestion and circadian rhythms was investigated in animals and humans. On the other hand, it has been reported that carbohydrate intake is related to sleep and circadian rhythms in humans through blood glucose levels [41, 42]. In addition, animal studies have shown that insulin directly affects the peripheral circadian clock [43, 44]. Although trehalose is converted to glucose and increases insulin concentrations [45], the dose of trehalose used as a placebo in this study (3.0 g) was very small, and its effect on glucose and insulin concentrations is likely to be limited. Therefore, the possibility that the placebo condition directly affected the delay in circadian rhythm is considered negligible. However, since we did not examine or control for the subjects’ daily diet in this experiment, we cannot exclude the possibility that differences in eating behavior between the two groups may have affected the results.
In this study, the regression coefficient by DLMO before intervention was significant for the amount of DLMO advance. A significant positive correlation between advance of DLMO and DLMO before intervention was found in both groups. This indicates that the later DLMO was, the greater was the subsequent DLMO advance. One probable cause of this is that the phase angle between the circadian phase and sleep timing affected the amount of circadian phase shift. When sleep timing is primarily tied to social factors, late circadian timing results in a short phase angle. If the phase angle is short, the phase delay zone around DLMO of the phase response curve (PRC) to light [46, 47] is masked by sleep. It is thought that the circadian phase tends to advance thereafter.
On the other hand, the effect of the group on DLMO before intervention was not significant, and there was no difference in DLMO before intervention between the two groups and DLMO before intervention did not depend on the group. Uniformity of the slopes of regression lines in the two groups was also shown. In addition, a significant difference in the intercepts of regression lines was found between the two groups. These results suggest that the DLMO advance in the l-serine group was greater than that in the placebo group in all ranges of confirmed DLMO in this study. The fact that the effect of l-serine was confirmed regardless of the subject's circadian phase means that l-serine may be useful for various chronotypes of people.
In recent years, much attention has been focused on research on the relationship between social jetlag and health [48]. In the present study, the effects of social jetlag did not be assessed because the average social jetlag of the subjects was less than 1 h (Table 1). This small social jetlag may be related to the less social constraints of weekday life for university students. However, it is known that social jet lag is greater in nocturnal chronotypes [49] and that loss of morning light exposure due to weekend recovery sleep leads to a delay of the circadian phase [50]. The effects of l-serine in populations with greater social jetlag should be examined in future studies.
The effect of l-serine was confirmed in an autumn/winter experiment, but it is necessary to consider seasonal differences in the effect of l-serine in consideration of the day length and amount of daytime sunshine in various seasons. However, considering that seasonal affective disorder [51], which is presumed to be associated with circadian rhythm disorder, is likely to develop in the period in which this study was conducted and considering the results of a study showing that l-serine enhanced the antidepressant effect of light in a mouse model of seasonal affective disorder [52], the effect of l-serine on light-induced circadian phase advance in humans that was confirmed in this study is a notable finding. This study was conducted in healthy subjects, and the effectiveness of l-serine in patients with circadian rhythm disorders as well as patients with seasonal affective disorder should also be examined.
Finally, although the mechanism by which l-serine affects the light-induced phase shift of circadian rhythms is not yet well understood, our previous study in mice (CBA/N) showed that light exposure after l-serine ingestion altered the long-term expression pattern of clock genes in the suprachiasmatic nucleus (SCN) [17]. As a possible mechanism for this, we focused on the MNDA receptor, which is believed to have a major role in light signaling in the SCN [53]. However, since the effectiveness of l-serine was not blocked by MK801, an antagonist of the NMDA receptor, we considered that this receptor was not involved [17]. On the other hand, we found that antagonists of the GABAA receptor completely blocked the effectiveness of l-serine. In other words, l-serine was thought to affect circadian rhythm phases via activation of GABAA receptors. This is consistent with the results of a previous study showing that the sedative and hypnotic effects of l-serine are mediated by GABAA receptors [54]. GABAA is also known to play an important role in circadian clock function in the SCN [55]. Therefore, the light-induced phase advance of l-serine in mice may be involved in the phase shift of circadian rhythms via the GABAergic system. Furthermore, l-serine did not affect the light-induced expression of c-fos, Per1, and Per2 in the SCN, but it altered the long-term expression of Per2 and Bmal1 [17]. These results suggest that the action of l-serine occurs in extra-SCN regions that convey information to the SCN via a post-transcriptional process. However, given that the mechanism of effects of light may differ among species [17], it is unclear whether the same mechanism of action is also true in humans. In addition, there are limitations in referring to the mechanism based on the results obtained in the present field study.
Conclusions
The results of this study showed that external intake of l-serine before bedtime for multiple days might enhance circadian phase advance by light in the morning and suppress the circadian phase delay. The results also suggested that the effect of l-serine does not depend on the initial circadian phase. l-serine intake before bedtime is expected to help prevent the delay of circadian rhythm in real word conditions in various chronotypes of people.
References
Czeisler CA, Duffy JF, Shanahan TL, Brown EN, Mitchell JF, Rimmer DW, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science. 1999;284:2177–81.
Minors DS, Waterhouse JM, Wirz-Justice A. A human phase-response curve to light. Neurosci Lett. 1991;133:36–40.
Lockley SW, Gooley JJ. Circadian photoreception: spotlight on the brain. Curr Biol. 2006;16(18):R795-7.
Lucas RJ, Peirson SN, Berson DM, Brown TM, Cooper HM, Czeisler CA, et al. Measuring and using light in the melanopsin age. Trends Neurosci. 2014;37:1.
Katsuura T, Lee S. A review of the studies on nonvisual lighting effects in the field of physiological anthropology. J Physiol Anthropol. 2019;38:1–18.
Higuchi S, Motohashi Y, Liu Y, Maeda A. Effects of playing a computer game using a bright display on presleep physiological variables, sleep latency, slow wave sleep and REM sleep. J Sleep Res. 2005;14:267–73.
LeBourgeois MK, Hale L, Chang AM, Akacem LD, Montgomery-Downs HE, Buxton OM. Digital media and sleep in childhood and adolescence. Pediatrics. 2017;140(Supplement_2):S92–6.
Lunn RM, Blask DE, Coogan AN, Figueiro MG, Gorman MR, Hall JE, et al. Health consequences of electric lighting practices in the modern world: a report on the National Toxicology Program’s workshop on shift work at night, artificial light at night, and circadian disruption. Sci Total Environ. 2017;607–608:1073–84.
Potter GDM, Skene DJ, Arendt J, Cade JE, Grant PJ, Hardie LJ. Circadian rhythm and sleep disruption: causes, metabolic consequences, and countermeasures. Endocr Rev. 2016;37:584–608.
De Koning TJ, Snell K, Duran M, Berger R, Poll-The BT, Surtees R. L-serine in disease and development. Biochem J. 2003;371(Pt 3):653.
Mitoma J, Furuya S, Hirabayashi Y. A novel metabolic communication between neurons and astrocytes: non-essential amino acid L-serine released from astrocytes is essential for developing hippocampal neurons. Neurosci Res. 1998;30:195–9.
Furuya S, Tabata T, Mitoma J, Yamada K, Yamasaki M, Makino A, et al. l-Serine and glycine serve as major astroglia-derived trophic factors for cerebellar Purkinje neurons. Proc Natl Acad Sci U S A. 2000;97:11528.
Nagasawa M, Otsuka T, Togo Y, Yamanaga M, Yoshida J, Uotsu N, et al. Single and chronic l-serine treatments exert antidepressant-like effects in rats possibly by different means. Amino Acids. 2017;49:1561–70.
Cox PA, Davis DA, Mash DC, Metcalf JS, Banack SA. Dietary exposure to an environmental toxin triggers neurofibrillary tangles and amyloid deposits in the brain. Proc Biol Sci.. 2016;283(1823):20152397.
Levine TD, Miller RG, Bradley WG, Moore DH, Saperstein DS, Flynn LE, et al. Phase I clinical trial of safety of L-serine for ALS patients. Amyotroph Lateral Scler Front Degener. 2017;18:107–11.
Ito Y, Takahashi S, Shen M, Yamaguchi K, Satoh M. Effects of L-serine ingestion on human sleep. Springerplus. 2014;3:456.
Yasuo S, Iwamoto A, Il LS, Ochiai S, Hitachi R, Shibata S, et al. L-serine enhances light-induced circadian phase resetting in mice and humans. J Nutr. 2017;147:2347–55.
Burgess HJ, Fogg LF. Individual Differences in the Amount and Timing of Salivary Melatonin Secretion. PLoS One. 2008;3:e3055.
Kantermann T, Sung H, Burgess HJ. Comparing the Morningness-Eveningness Questionnaire and Munich ChronoType Questionnaire to the Dim Light Melatonin Onset. J Biol Rhythms. 2015;30:449–53.
Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110.
Ishihara K, Miyashita A, Inugami M, Fukuda K, Yamazaki K, Miyata Y. The results of investigation by the Japanese version of Morningess-Eveningness questionnaire. Japanese J Psychol. 1986;57:87–91.
Kitamura S, Hida A, Aritake S, Higuchi S, Enomoto M, Kato M, et al. Validity of the Japanese version of the Munich ChronoType Questionnaire. Chronobiol Int. 2014;31:845–50.
Lewy AJ, Sack RL. The dim light melatonin onset as a marker for orcadian phase position. Chronobiol Int. 1989;6:93–102.
Pullman RE, Roepke SE, Duffy JF. Laboratory validation of an in-home method for assessing circadian phase using dim light melatonin onset (DLMO). Sleep Med. 2012;13:703–6.
Benloucif S, Burgess HJ, Klerman EB, Lewy AJ, Middleton B, Murphy PJ, et al. Measuring melatonin in humans. J Clin Sleep Med. 2008;4:66.
Burgess HJ, Molina TA. Home Lighting Before Usual Bedtime Impacts Circadian Timing: A Field Study. Photochem Photobiol. 2014;90:723.
Higuchi S, Il LS, Kozaki T, Harada T, Tanaka I. Late circadian phase in adults and children is correlated with use of high color temperature light at home at night. Chronobiol Int. 2016;33:448–52.
Miyazaki T, Hashimoto S, Masubuchi S, Honma S, Honma KI. Phase-advance shifts of human circadian pacemaker are accelerated by daytime physical exercise. Am J Physiol Regul Integr Comp Physiol. 2001;281(1):50–1.
Crouter SE, Flynn JI, Bassett DR. Estimating physical activity in youth using a wrist accelerometer. Med Sci Sports Exerc. 2015;47:944–51.
Lin HP, Lynk N, Moore LL, Cabral HJ, Heffernan KS, Dumas AK, et al. A pragmatic approach to the comparison of wrist-based cutpoints of physical activity intensity for the MotionWatch8 accelerometer in children. PLoS One. 2020;15(6):e0234725.
Skeldon AC, Dijk DJ. Weekly and seasonal variation in the circadian melatonin rhythm in humans: Entrained to local clock time, social time, light exposure or sun time? J Pineal Res. 2021;71:e12746.
Zerbini G, Winnebeck EC, Merrow M. Weekly, seasonal, and chronotype-dependent variation of dim-light melatonin onset. J Pineal Res. 2021;70(3):e12723.
Honma KI, Honma S, Kohsaka M, Fukuda N. Seasonal variation in the human circadian rhythm: dissociation between sleep and temperature rhythm. Am J Physiol. 1992;262(5 Pt):2.
Roenneberg T, Kuehnle T, Pramstaller PP, Ricken J, Havel M, Guth A, et al. A marker for the end of adolescence. Curr Biol. 2004;14:R1038–9.
Fukuda K, Ishihara K. Age-related changes of sleeping pattern during adolescence. Psychiatry Clin Neurosci. 2001;55:231–2.
Porcheret K, Wald L, Fritschi L, Gerkema M, Gordijn M, Merrrow M, et al. Chronotype and environmental light exposure in a student population. Chronobiol Int. 2018;35:1365–74.
Higuchi S, Lin Y, Qiu J, Zhang Y, Ohashi M, Lee SI, et al. Is the use of high correlated color temperature light at night related to delay of sleep timing in university students? A cross-country study in Japan and China. J Physiol Anthropol. 2021;40:1–8.
Tanaka M, Machida Y, Niu S, Ikeda T, Jana NR, Doi H, et al. Trehalose alleviates polyglutamine-mediated pathology in a mouse model of Huntington disease. Nat Med. 2004;10:148–54.
Tien NT, Karaca I, Tamboli IY, Walter J. Trehalose Alters Subcellular Trafficking and the Metabolism of the Alzheimer-associated Amyloid Precursor Protein. J Biol Chem. 2016;291:10528–40.
Castillo K, Nassif M, Valenzuela V, Rojas F, Matus S, Mercado G, et al. Trehalose delays the progression of amyotrophic lateral sclerosis by enhancing autophagy in motoneurons. Autophagy. 2013;9:1308–20.
Vlahoyiannis A, Giannaki CD, Sakkas GK, Aphamis G, Andreou E. A systematic review, meta-analysis and meta-regression on the effects of carbohydrates on sleep. Nutrients. 2021;13(4):1283.
Pinkhasov BB, Selyatinskaya VG, Astrakhantseva EL, Anufrienko EV. Circadian rhythms of carbohydrate metabolism in women with different types of obesity. Bull Exp Biol Med. 2016;161:323–6.
Sato M, Murakami M, Node K, Matsumura R, Akashi M. The role of the endocrine system in feeding-induced tissue-specific circadian entrainment. Cell Rep. 2014;8:393–401.
Crosby P, Hamnett R, Putker M, Hoyle NP, Reed M, Karam CJ, et al. Insulin/IGF-1 Drives PERIOD Synthesis to Entrain Circadian Rhythms with Feeding Time. Cell. 2019;177:896–909.e20.
Yoshizane C, Mizote A, Yamada M, Arai N, Arai S, Maruta K, et al. Glycemic, insulinemic and incretin responses after oral trehalose ingestion in healthy subjects. Nutr J. 2017;16:1–6.
St Hilaire MA, Gooley JJ, Khalsa SBS, Kronauer RE, Czeisler CA, Lockley SW. Human phase response curve to a 1 h pulse of bright white light. J Physiol. 2012;590:3035–45.
Khalsa SBS, Jewett ME, Cajochen C, Czeisler CA. A phase response curve to single bright light pulses in human subjects. J Physiol. 2003;549(Pt 3):945–52.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22:939–43.
Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23:497–509.
Crowley SJ, Carskadon MA. Modifications to weekend recovery sleep delay circadian phase in older adolescents. Chronobiol Int. 2010;27:1469–92.
Johansson C, Willeit M, Smedh C, Ekholm J, Paunio T, Kieseppä T, et al. Circadian clock-related polymorphisms in seasonal affective disorder and their relevance to diurnal preference. Neuropsychopharmacology. 2003;28:734–9.
Kawai M, Goda R, Otsuka T, Iwamoto A, Uotsu N, Furuse M, et al. Antidepressant-like effect of bright light is potentiated by l-serine administration in a mouse model of seasonal affective disorder. Brain Res Bull. 2015;118:25–33.
Golombek DA, Rosenstein RE. Physiology of circadian entrainment. Physiol Rev. 2010;90:1063–102.
Shigemi K, Tsuneyoshi Y, Hamasu K, Han L, Hayamizu K, Denbow DM, et al. l-Serine induces sedative and hypnotic effects acting at GABAA receptors in neonatal chicks. Eur J Pharmacol. 2008;599:86–90.
Ono D, Honma K i, Yanagawa Y, Yamanaka A, Honma S. Role of GABA in the regulation of the central circadian clock of the suprachiasmatic nucleus. J Physiol Sci. 2018;68:333–43.
Acknowledgements
We would like to thank Mr. Kota Takeoka for supporting our experiment.
Funding
This work was supported by JSPS KAKENHI Grant Number 16K21225.
Availability of data and materials
The datasets analyzed in this study are not publicly available due to a privacy policy but are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
SL, NU, CT, SM, and SH contributed to the design of the experiment. MO and SL performed the experiment. MO and SL analyzed the data. MO wrote the manuscript with advice from SL, TE, NU, CT, SM, SY, and SH. All authors participated in the discussion and preparation of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Kyushu University (Approval No. 228). Written informed consent was obtained from all participants.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ohashi, M., Lee, Si., Eto, T. et al. Intake of l-serine before bedtime prevents the delay of the circadian phase in real life. J Physiol Anthropol 41, 31 (2022). https://doi.org/10.1186/s40101-022-00306-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40101-022-00306-z