Abstract
Hearing impairment is due to various causes including ototoxicity from aminoglycosides. The susceptibility to aminoglycosides increases in the presence of certain mitochondria gene mutations. There is unrestrained use of aminoglycosides in many developing nations which may worsen the burden of hearing impairment in these countries but there is lack of data to drive required policy changes. Streptomycin (an aminoglycoside) is part of the drug regimen in re-treatment of tuberculosis. Exploring the impact of streptomycin ototoxicity in tuberculosis patients provides a unique opportunity to study aminoglycoside ototoxicity within the population thus providing data that can inform policy. Also, since streptomycin ototoxicity could adversely affect treatment adherence in tuberculosis patients this study could enable better pre-treatment counseling with subsequent better treatment adherence. Patients on tuberculosis re-treatment will be recruited longitudinally from Direct Observation Therapy-Short course centers. A baseline full audiologic assessment will be done before commencement of treatment and after completion of treatment. Early detection of ototoxicity will be determined using the American Speech and Hearing Association criteria and genetic analysis to determine relevant mitochondria gene mutations will be done. The incidence of ototoxicity in the cohort will be analyzed. Both Kaplan–Meier survival curve and Cox proportional hazards tests will be utilized to determine factors associated with development of ototoxicity and to examine association between genotype status and ototoxicity. This study will provide data on the burden and associated predictors of developing aminoglycoside induced ototoxicity. This will inform public health strategies to regulate aminoglycoside usage and optimization of treatment adherence and the management of drug-induced ototoxicity among TB patients. Furthermore the study will describe mitochondrial gene mutations associated with ototoxicity in the African population.
Similar content being viewed by others
Background
Hearing ability is one of the key human senses and it could be argued to be essential for satisfactory quality of life. Loss of hearing therefore, may be a major disability. This disability becomes more apparent in the communal cultural setting prevalent in many developing countries where hearing impaired people may suffer from social stigmatization and isolation. Hearing loss imposes significant social and economic disadvantages on both individuals and communities. Hearing impaired children often experience delayed development of speech, language, and cognitive skills, causing slowed learning and difficult progress in school (WHO 2014). Among adults, impairment of hearing makes it difficult to obtain and keep employment (WHO 2014). Hearing loss occurs via multiple pathways,—inflammatory disease of the middle ear is the commonest cause in children (Adeyemo 2012a)—but ototoxicity is an increasing cause of hearing loss in developing countries.
According to the World Health Organization (WHO) majority of hearing impaired people resides in developing countries; while a number of etiological factors have been identified as a cause of the impairment in these countries, ototoxicity from both antibiotics and antimalarial drugs feature prominently (WHO 2014) and aminoglycoside antibiotics are the commonest cause of ototoxicity (WHO 1994). Irrational prescription of aminoglycosides have been reported in many developing countries (Gwimile et al. 2012) and this unrestrained use may keep eliciting a huge burden of hearing impairment unless a significant policy change comes into effect in these countries. Unfortunately there is inadequate locally derived data to drive such a policy change.
Streptomycin, Amikacin, and Kanamycin are examples of aminoglycosides in the drug armamentarium against tuberculosis (Peloquin et al. 2004). Studying the streptomycin induced ototoxicity in tuberculosis patients provides an excellent opportunity to monitor aminoglycoside ototoxicity within a developing country population.
Aminoglycoside induced ototoxicity
Ototoxicity is an irreversible side effect of aminoglycosides (De Jager and Van Altena 2002), and could manifest as either cochlea damage with permanent hearing loss or vestibular damage with dizziness, ataxia and/or nystagmus (Duggal and Sarkar 2007). This adverse effect is dose-dependent (De Jager and Van Altena 2002) and compounded by the narrow therapeutic range of aminoglycosides and the wide inter-individual variability in the pharmacokinetics of the drug (Duggal and Sarkar 2007). Aminoglycoside ototoxicity is recognized by a distinctive pattern of hearing loss, the high frequency range (4000–8000 Hz) is affected first with lower frequencies affected subsequently (Human et al. 2010).
Aminoglycosides cause degeneration of sensory cells in the cochlea; usually involving the basal turn initially before progressing to the cochlea apex. This is the basis for the initial high frequency hearing loss subsequently followed by hearing loss in the lower frequencies. Therefore in the early stages of aminoglycoside ototoxicity conversational hearing might not be affected. Vestibular impairment occurs following damage to the vestibular sensory cells in the crista ampullaris and it manifests with ataxia and nystagmus. The subject complains of gait disturbances and oscillopsia (visual blurring with head movement) in the absence of prior existence of vertigo (Kisilevsky et al. 2004). All aminoglycosides exhibit toxicity on both the cochlea and the vestibules but often not in equal proportions though tobramycin is known to affect both the cochlea and vestibules equally (Guan 2011). Aminoglycosides such as streptomycin and gentamycin are predominantly vestibulotoxic whereas neomycin and kanamycin are more toxic on the cochlea (Guan 2011).
The incidence of ototoxicity depends on the duration and dose of the aminoglycoside; reported incidence varies widely from 28 to 37 % (Sturdy et al. 2011, Peloquin et al. 2004). However factors such as definitional criteria for hearing loss, methods of assessment, subject group and treatment parameters had influenced the reported incidence of ototoxicity (Xie et al. 2011). Therefore the use of more sensitive testing criteria will probably increase the proportion of hearing loss detected in aminoglycoside exposure (Fausti et al. 1992).
Tuberculosis control
Tuberculosis is known to man since antiquity and it is still one of the leading infectious diseases in the world with a third of the world’s population already infected (Duggal and Sarkar 2007; Jones-López et al. 2011). Nine million new cases of TB are diagnosed annually and the disease is responsible for more than two million deaths every year (Harries and Dye 2006; Adeyemo 2012b). Hopes of eradicating TB had initially brightened with the discovery of streptomycin by Waksman in 1944 (Schacht 2004) however multiple factors including resource constraints, economic crises, and recently HIV/AIDS pandemic had led to renewed surge in TB burden in many developing countries. The emergence of drug resistant TB strains are due to factors such as lack of adherence by patients to drug regimen, improper prescription, inadequate supply, and low quality drugs (Lienhardt et al. 2012). The proportion of drug resistant TB among TB cases have been increasing worldwide (Sturdy et al. 2011); since the second-line drugs advocated by WHO for the management of drug resistant TB includes aminoglycosides there has been a corresponding upsurge in the usage of aminoglycosides.
A high proportion of TB patients fail to complete their initial treatment and thus require re-treatment with streptomycin based drug regimen—category II regimen (Jones-López et al. 2011). Indeed 10–20 % of the populations with TB in developing countries are commenced on streptomycin based anti-TB drugs regimen annually (Jones-López et al. 2011) which involves daily streptomycin injection for 2 months. The key side effect of long-term administration of parenteral aminoglycosides is ototoxicity.
Single versus multiple dosing regimen
There have been previous attempts to reduce the toxicities associated with aminoglycosides by varying the frequency of dosage. Traditionally aminoglycosides have been given in Multiple Daily Doses (MDD) in either 8 or 12 hourly doses to ensure therapeutic concentrations that could guarantee clinical success as well as preventing toxicities of the kidney or inner ear.
Single daily dosing (SDD) however might lead to greater clinical efficacy. SDD produces higher peak serum concentrations which increased the rate and proportion of the microbicidal activity (Ali and Goetz 1997). Moreover, the concept of saturation of aminoglycoside uptake into the renal proximal tubule cell also encouraged SDD practice with the intention of reducing associated nephrotoxicity (Rotstein and Mandell 2004). Additional evidence which showed that laboratory animals manifest less toxicity on SDD rather than MDD (Ali and Goetz 1997) and demonstration of saturation kinetics in the entry of aminoglycosides into the ear (Tran Ba Huy et al. 1986) probably promoted adoption of SDD.
Meta-analyses of clinical trials comparing SDD and MDD showed superiority of SDD for bacteriologic eradication and a reduced incidence of nephrotoxicity (Rotstein and Mandell 2004; Turnidge 2003). However assessment of ototoxicity in the meta-analyses did not show any clear trend as some clinical trials favored SDD while others favored MDD. No statistically significant differences were seen between SDD and MDD in the data assessment of vestibular toxicity (Rotstein and Mandell 2004). The variability in techniques of evaluating ototoxicity in the trials and lack of standard definition of what constitutes “toxicity” between the trials may had accounted for the inconsistencies in the trial results (Rotstein and Mandell 2004). The simplicity of SDD (especially in out-patient set-up), cost advantages, and efficacy have made it the preferred dosage regimen in streptomycin administration in TB control programs.
Auditory assessment in ototoxicity
There is no universal consensus on the most appropriate way to monitor ototoxicity in patients receiving aminoglycoside therapy; the lack of consistent predictors of hearing loss is one of the shortcomings of research in human ototoxicity (Peloquin et al. 2004). In general, hearing loss due to ototoxicity is ascertained by comparing baseline data, ideally obtained before commencement of ototoxic drug administration, to the results obtained in subsequent monitoring tests (Duggal and Sarkar 2007). The duration of monitoring should extend for a reasonable period otherwise the onset of the ototoxicity may be missed as it may start at the end of the aminoglycoside therapy with slow progression (Xie et al. 2011).
Hotz et al. (1994) have proposed the use of Transiently Evoked Oto-Acoustic emission (TEOAE) for early monitoring of aminoglycoside induced ototoxicity, based on the relation of TEOAE characteristics reflecting the integrity of the cochlea’s outer hair cell (OHC). However the American Speech-Language-Hearing Association (ASHA) recommends otherwise; though the sensitivity of TEOAE to the status of OHC was acknowledged the lack of specific guidelines to tailor its application to ototoxicity monitoring was highlighted as its main Achilles’ heel (ASHA 1994). Moreover, the presence of abnormal middle-ear function and a baseline hearing loss of greater than 40 dB HL (decibels hearing level) may preclude effective monitoring of ototoxicity with oto-acoustic emissions (Harris et al. 2012).
Serial audiometry-including high frequencies—demonstrating change from baseline values in pure tone thresholds is probably the most effective method to prove ototoxic hearing loss (Duggal and Sarkar 2007). High frequency thresholds is required in the audiometry because this range (>8 kHz) is usually first (but sometimes solely) affected in ototoxicity. Limiting hearing monitoring to the conventional-frequency range may potentially result in missing many cases of ototoxicity therefore the ASHA and the American Academy of Audiology (AAA) guidelines recommends high-frequency audiometry as the method of choice in early detection of ototoxicity (ASHA 1994; AAA 2009). Additional measures should also be instituted to overcome other sources of errors in an ototoxicity screening program. Such measures will include: a thorough interview to identify other causes of conductive hearing loss from the medical history, full documentation of all drugs administered to subjects—even when such drugs are considered safe for hearing preservation—and a baseline audiogram to enable the subjects learn the test technique apart from providing a reference value for the hearing acuity (Duggal and Sarkar 2007). Since hearing loss due to aminoglycoside ototoxicity usually becomes manifest from the 5th day post commencement of drug treatment (De Jager and Van Altena 2002) post treatment screening should commence at least after a week of therapy. It has also been advocated that screening takes place at least weekly during the course of the treatment (Duggal and Sarkar 2007).
Other tests have also been advocated but critics have highlighted their shortcomings. Electro-cochleo-graphy (ECochG) requires an invasive technique to be very sensitive and a long time to acquire frequency-specific data thus eliminating its usefulness in routine hearing monitoring (ASHA 1994). Auditory brainstem (ABR) evoked response share similar limitations with ECochG in respect of time required for testing (ASHA 1994).
Despite perceived advantages of other monitoring methods audiometry remains the most widely accepted technique. The sturdiness of audiometry equipment and wide availability even in developing countries in addition to its other benefits makes it an attractive option to be adopted in field work in Africa.
Vestibular assessment in ototoxicity
The true incidence of vestibular ototoxicity has been underestimated. Multiple factors are responsible for the lack of clear data on the true incidence of vestibular damage following aminoglycoside exposure. A main factor is that subclinical vestibular damage is hard to document, another factor is that the initial destruction of vestibular hair cells also occurs outside the normal active and passive head movement frequency range for the vestibular system.
Vigilance and prior anticipation of symptoms are the hallmarks of effective subjective evaluation of vestibular damage. Subjective evaluation of vestibular dysfunction involves recording complaints of dizziness, imbalance and oscillopsia made by the patient. Validated survey tools are also part of the armamentarium in subjective evaluation. A good example is the Dizziness Handicap Inventory (DHI) which allows subjects to evaluate on-going well-being (Jacobson and Newman 1990).
There are multiple methods for objective evaluation of vestibular function but the main goal is to determine the normal function of the labyrinthine end-organ and the Central Nervous System (CNS) pathways via the vestibulo-ocular reflex (VOR) (Kisilevsky et al. 2004). Objective evaluations of vestibular function test the integrity of the VOR; these tests include electronystagmography (ENG), rotational chair, sacculocolic testing, vestibular evoked potentials, and computerized dynamic posturography (CDP) (Kisilevsky et al. 2004). The advantages and disadvantages of each evaluation methods are shown in Table 1.
ENG is the recording of eye movements -it is the most available and widely used test of vestibular function (Kisilevsky et al. 2004) and is based on the principle of measurement of changes in the corneo-retinal potential which occurs with eye movements with respect to electrodes placed around the eyes. There are multiple tests within the ENG test battery such as oculomotor test, measurement of spontaneous nystagmus, positional testing and caloric testing. The gold standard for objective evaluation of unilateral vestibular deficit is caloric test. The main advantage of the caloric test is that it is the only vestibular function test that allows separate stimulation of each labyrinth. This makes the test highly sensitive for unilateral peripheral vestibular lesions. The caloric test uses a thermal stimulus (water or air) to induce flow of the endolymph in the semi-circular canals (SCCs) through creation of a temperature gradient from one side of the canal to the other. The main canal tested is the horizontal SCC since it is the canal anatomically closet to the external auditory canal and thus it develops the largest temperature gradient (Kisilevsky et al. 2004).
The caloric test has handicaps which may restrict its use in aminoglycoside monitoring. Caloric testing is limited in bilateral vestibular loss which causes symmetrically depressed caloric responses (Fee 1980). By design caloric testing only allows for low-frequency stimulation. This is also limiting since the frequency of rotation obtainable with caloric stimulation is below the normal physiologic range of the vestibular system. This means a poor sensitivity and specificity of the caloric test for symmetric loss of vestibular function. Despite the handicaps the obvious advantages of the caloric test such as the ease of the test, the wide availability and portability of the equipment ensures that it remains a relevant tool in vestibular function studies. Combining this test with subjective evaluation techniques will enable a good monitoring system for aminoglycoside toxicity.
Genetic mutations associated with ototoxicity
At very high cumulative drug levels most individuals will exhibit ototoxicity to aminoglycosides; while at lower cumulative drug levels, observed aminoglycoside ototoxicity is probably a result of genetic susceptibility. Mitochondria DNA abnormality was noted by Higashi (1989) to be the likely basis of the maternal inheritance observed in familial aminoglycoside ototoxicity. This observation was buttressed when Hu et al. (1991) described maternal transmission in familial aminoglycoside ototoxicity in another set of related individuals. All these observations tended to confirm that mutation of mitochondrial genes was the likely molecular basis for aminoglycoside ototoxicity (Fischel-Ghodsian 2004). Aminoglycosides exerted their antibacterial activity by direct binding to 16S ribosomal RNA (rRNA) in the 30S subunit of the bacterial ribosome, thus causing mistranslation or premature termination of protein synthesis (Chamber and Sande 1996; Noller 1991). Accumulation of non-functional and truncated proteins thus occurred leading eventually to bacterial death (Xie et al. 2011). This effect was usually limited to bacterial ribosomes because the affinity of aminoglycosides for eukaryotic ribosomes was lowered due to structural differences hence rendering the drug safe for humans (Xie et al. 2011). However since mitochondria were evolutionarily derived from bacteria, mitochondrial ribosomes therefore shared greater similarities to bacterial ribosomes than their cytosolic counterparts (Fischel-Ghodsian 2004; Guan 2004). Thus it has been suggested that aminoglycosides exerted their ototoxic activity at the mitochondrial ribosome.
The 12S rRNA ribosomal subunit binds to aminoglycosides and it is known to confer resistance to aminoglycosides in the mitochondria of bacteria and yeast (Fischel-Ghodsian 2004). Several ototoxic mitochondria DNA (mtDNA) mutations in the 12S rRNA gene have been identified in patients with aminoglycoside ototoxicity. Current reports indicated that at least five different homoplasmic mutations in the mitochondrial gene encoding 12S rRNA (MT-RNR1) have been identified to predispose individuals to irreversible aminoglycoside induced hearing loss (Bardien et al. 2009). The homoplasmic A1555G mutation and C1494T mutation and mutations at position 961 in the 12S rRNA gene have been associated with aminoglycoside-induced hearing loss (Matthijs et al. 1996; Usami et al. 1997); other identified mutations are T1095C and A827G (Thyagarajan et al. 2000; Xing et al. 2006). The A1555G mutation was the first mutation to be described and the commonest variant seen (Bardien et al. 2009); it has been reported in different populations’ worldwide (Guan 2006). The A1555G mutation leads to increased binding of aminoglycosides to the 12S rRNA ribosomal subunit with subsequent disruption of mitochondrial protein synthesis and eventual cell death (Duggal and Sarkar 2007; Qian and Guan 2009).
Identified genetic mutations appeared to be commoner in the black population. Studies in different populations have shown the A1555G mutation to be relatively rare; a frequency of 0.48, 0.09, and 0 % were seen in studies done in the general population of New Zealand, America and Argentina respectively (Scrimshaw et al. 1999; Tang et al. 2002; Gravina et al. 2007). A recent study among the Black population in South Africa however showed prevalence as high as 0.9 % (Bardien et al. 2009). This might suggests that the mutation might be more frequent among Blacks compared to other human races. Both A1555G and C1494T mutations decrease translation accuracy in the mitochondrion. This makes the ribosomal decoding site highly susceptible to damage by aminoglycosides (Bardien et al. 2009; Hobbie et al. 2008).
Research goals
We hypothesize that the use of streptomycin based anti-TB drug regimen is associated with ototoxicity and that there is an association between genetic mutations of 12sRNA gene and development of streptomycin associated ototoxicity among West Africans.
Therefore the overall goal of this study is to determine the incidence of ototoxicity in a cohort of patients undergoing TB re-treatment and to determine any association between the genetic mutations in 12S rRNA mitochondria gene and streptomycin induced hearing loss.
Specific objectives are: (1) determine the incidence of ototoxicity in a cohort of category II TB patients; (2) determine the probability of developing ototoxicity and the median onset time of ototoxicity; (3) determine the demographic and pharmacologic parameters associated with developing ototoxicity; (4) describe the mutations in the 12S rRNA gene in the cohort.
Methods
Study design
This study was approved by the Ethics Review Board of the Ministry of Health, Oyo state, Nigeria. Subjects will be recruited at the start of TB therapy and followed in a prospective longitudinal study till conclusion of treatment.
Eligible patients must meet the following criteria:
-
1.
Diagnosis of TB and scheduled to commence TB re-treatment with streptomycin based drug regimen;
-
2.
Hearing thresholds of 60 dB or better on pure tone audiometry (PTA) before commencement of streptomycin.
Excluded individuals will be those with:
-
1.
Evidence of active infective pathology of the ear on examination;
-
2.
Evidence of conductive hearing loss with an air-bone gap exceeding 10 dB on baseline PTA;
-
3.
Asymmetric hearing exceeding 20 dB at any frequency on baseline PTA;
-
4.
Abnormal serum creatinine at baseline;
-
5.
Concomitant use of other ototoxic drugs (macrolides, diuretics, iron chelating drugs, chemotherapy drugs such as cisplatin and vinca alkaloids);
-
6.
Evidence of confirmed HIV/AIDS infection.
Study setting
Uncomplicated TB is managed in Nigeria at Directly Observed Therapy-Short course (DOTS) centers after diagnosis. These DOTs centers are located in primary health centers (PHC) within the community. PHCs are common in Nigerian towns and villages; they are sited with the goal of easy accessibility by the public. These centers are often manned by nurses, community health workers and community health extension workers. Initial diagnosis of TB (i.e. no prior treatment of TB) is designated as category I and managed with a 6 month regimen of Isoniazid, Rifampicin, Ethambutol and Pyrazinamide. However patients who default from treatment or represent with a relapse of TB are designated as category II and commenced on 8 month regimen of anti-TB medications which include daily streptomycin injection in the first 2 months. The dosage varies with weight of the patient. (See Additional file 1 for recommended streptomycin dosages by the National Tuberculosis and Leprosy Control Program of Nigeria) Study subjects will be recruited from the category II patient pool.
Subjects will be recruited consecutively as diagnosis is made and consent given at the DOTS centers. Subsequent follow-up will also take place at the DOTS centers over the course of the treatment regimen. All the relevant socio-demographic and clinical data will be recorded using an interviewer administered modified questionnaire (Katijah et al. 2009). Additional information will be retrieved from patient case notes.
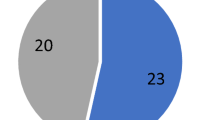
Sample size and power calculations
A recent study reported the proportion of TB patients with ototoxicity as 28 % (Sturdy et al. 2011). Assuming a 5 % level of significance, a sample size of 150 would be able to estimate a prevalence of 28 % with a precision of ±7.2 %, a prevalence of 50 % with a precision of ±8 %, and a prevalence of 5 % with a precision of ±3.5 %. The sample size will also allow the investigation of the association between ototoxicity and risk factors. For example, assuming a proportion with ototoxicity of 20 %, the study will be powered to detect an odds ratio of at least 2.5 if the prevalence of the risk factor in the population is at least 20 %. Adjustments of 10 % for loss to follow up gives a minimum sample size of 168 participants.
Study measures at baseline and follow-up visit
Baseline pre-treatment full audiologic assessment will be performed on all the patients and repeated at completion of the TB treatment. Baseline and exit audiologic tests will include both air and bone-conduction threshold measurements in all the patients. Air conduction PTA will be done weekly during the intensive phase (2 months) and monthly during the continuation phase (6 months) till completion of the TB treatment. Enquiry on subjective hearing and balance changes will be sought from the subjects at every contact. Subjects who complain of changes will undergo repeat full audiologic evaluation. The treatment guidelines of the WHO stipulate daily intramuscular streptomycin injection for category II TB patients (WHO 2010) therefore multiple dosing regimen of streptomycin will not be considered in this study.
Baseline pure tone audiograms between 250 and 16,000 Hz will be performed for all the patients using a KUDU wave audiometer (Geoaxon, Pretoria, South Africa). This is a portable device run by an eMoyo algorithm on a laptop and it obviates the need for a sound proof booth (Swanepoel et al. 2010). The audiometer uses external audio cups to attenuate environmental noise and intra-aural probe and fore head vibrator to deliver the pure tones. It also monitors ambient sound via an inbuilt microphone and the test is stopped once the environmental sound becomes loud enough to interfere with the examination. A user friendly game pad is also attached to the laptop and user is instructed to press the keys after perceiving the pure tones. This enables the software to plot the user responses directly on an audiogram. The software also prompts the examiner to position the forehead vibrator after completion of the air conduction tests; at the end of both the bone and air conduction test the pure tone average is automatically calculated and a printer friendly audiogram is generated.
The quietest place in the DOTS center will be sought to perform the PTA. The vestibular function test (Romberg Test) will be done in an examination room with an even floor and good lighting. The patient will be put at ease and the tests to be done fully explained in a language familiar to the patient. Assurances will be given that the examiner and research assistants will catch the patient and prevent a fall in case dizziness ensues in the course of the examination (see Table 2).
A panel of five homoplasmic mutations in the 12S rRNA gene previously described to predispose individuals to ototoxicity following aminoglycoside therapy will be investigated. These are: A1555G, 961delT + C(n), T1095C, C1494T and A827G (Bardien et al. 2009). All subjects will have blood samples drawn and DNA will be extracted from whole blood samples using standard protocols. The DNA will be stored at −20 °C until batch testing is done. Genetic analysis for suspected mitochondrial polymorphisms will then be done on extracted DNA using standard protocols. Magnification of the mitochondrial DNA by PCR in 24 overlapping fragments will be done according to previously described protocol (Rieder et al. 1998). Direct sequencing of the PCR products will then be done with an ABI 3700 automated DNA sequencer; the sequences will be analyzed by comparison with the reference sequences in the revised Cambridge reference sequence (rCRS) of the human mtDNA (accession no. AC_000021. 2) (Men et al. 2011).
Study outcomes
The criteria that will be used for identifying early ototoxic threshold shift from baseline audiogram are: (1) 20 dB or greater decrease at any one test frequency, (2) 10 dB or greater decrease at any two adjacent frequencies, or (3) loss of response at three consecutive frequencies where responses were previously obtained (ASHA 1994; AAA 2009). All the pure tone threshold shifts will be recorded at each frequency tested with reference to the baseline pure tone threshold at the same frequency. All the changes will be confirmed by retest on the same day. The degree of ototoxicity will be graded according to the National Cancer Institute’s Common Terminology Criteria for Adverse Events v4.3 (NCI 2010). Patients complaining of or showing audiological evidence of ototoxicity will be referred to the managing physicians for clinical review.
Statistical analysis
The data will be analyzed with Stata (Ver. 12) [Stata Corp, College Station, TX, USA]. Patient baseline characteristics will be summarized with descriptive statistics and incidence rates of ototoxicity per 1000 person-years will be computed.
Person-time will be accrued from the date of recruitment into the study until the earliest of: (1) development of ototoxicity; (2) loss to follow-up (defined as missing scheduled clinic visit and not returning during the study period); (3) transfer to another facility for any reason; or (4) completion of follow-up. For all patients, time zero will be the date of recruitment into the study.
Kaplan–Meier curves and the log-rank test will be used to compare progression to ototoxicity between groups. We will use Cox proportional hazards models to determine factors associated with development of ototoxicity and also to examine for associations between the A1555G mutation in the 12sRNA gene and development of toxicity. The following variables will be measured and considered for inclusion in regression models: socio-demographic variables like age, gender, weight, education and socio-economic status; clinical variables, BMI, total cumulative dose of strep, etc. The level of significance to be used is α = 0.05.
Discussion
This is a feasible prospective longitudinal study of streptomycin induced ototoxicity in a developing country. The protocol has not yet been fully explored before in a study setting but we believe it is robust enough to achieve the set objectives. Recruiting and following up the patients from DOTS centers will ensure that there will be minimal loss to follow up. The incidence of TB in Nigeria is 133 per 100,000 (Ibrahim et al. 2014); implying there will be a considerable population of TB patients that will progress to aminoglycoside based therapy.
Long distance to health centers have been identified as a reason for interruption of treatment of TB (Ibrahim et al. 2014) therefore this study will utilize DOTS units nested within a primary health centers for recruitment of study participants. The primary health care centers are widely distributed within communities thereby ensuring ease of access. Within these DOTS units drugs are provided free through a joint government and private donor’s initiative. The free drugs and ease of access to health care delivery point are incentives for patients to access treatment.
Despite the resurgence in incidence of TB in sub-Saharan Africa and the relatively huge numbers of people that will commence aminoglycoside based anti-TB drug regimen very little is known or being done about the ototoxicity that may arise from the aminoglycoside component of the drug regimen. It is possible that the auditory toxicities will have a negative impact on compliance with treatment. If that is true it will impair efforts to control the disease in the society. The lack of clarity in patient counseling was identified as a deterrent to treatment adherence in TB management (Ibrahim et al. 2014). Exploring the impact of aminoglycosides on the hearing and balance ability of patients will enable more accurate pre-treatment counseling sessions for patients. This will have a beneficial effect on treatment adherence. Data on genetic susceptibility will also benefit maternal relations of index participants when considering uptake of aminoglycoside based therapy.
More importantly aminoglycosides are commonly used in many developing countries. This is likely due to their cheap manufacturing costs (Xie et al. 2011) making this class of antibiotics attractive in many economically disadvantaged societies. The unrestrained use of the drugs possibly contributes to the high burden of hearing impairment in developing countries and probably a deafening of the population. Unlike in many developed societies where guidelines exists for monitoring serum concentrations when administering aminoglycosides such guidelines do not exist in many developing countries. Moreover there is lack of data to drive changes in policy regarding administration of aminoglycosides. Studying effects of streptomycin in tuberculosis patients therefore provides a unique opportunity to monitor aminoglycosides ototoxicity within the population in a developing country but the impact of the study will extend beyond tuberculosis treatment.
This study will provide insight into prevalence of ototoxicity in TB re-treatment and thus provide useful data for review of current treatment regimen and the contribution of aminoglycoside induced ototoxicity to the burden of hearing loss. It will also highlight areas requiring modification to improve treatment compliance in tuberculosis thereby providing evidence for appropriate policy formulation and resource allocation. The study will describe genetic mutations that predispose to aminoglycoside induced ototoxicity within the study cohort. There is dearth of data on these mutations in the West African population thus emphasizing further the need for this study.
Conclusion
Hearing loss remains a chronic disability in many developing societies, reducing the burden of this disability requires a multi-dimensional strategy which will include policy shifts to tackle aminoglycoside ototoxicity.
Abbreviations
- TB:
-
tuberculosis
- BCG:
-
bacillus Calmette–Guérin
- UNICEF:
-
United Nations Children’s Fund
- WHO:
-
World Health Organization
- MDR:
-
multi drug-resistant
- TEOAE:
-
Transiently Evoked Oto-Acoustic emission
- OHC:
-
outer hair cell
- ABR:
-
auditory brainstem response
- ASHA:
-
American Speech-Language-Hearing Association
- AAA:
-
American Academy of Audiology
- ECochG:
-
electro-cochleo-graphy
- DHI:
-
Dizziness Handicap Inventory
- CNS:
-
Central Nervous System
- VOR:
-
vestibulo-ocular reflex
- ENG:
-
electronystagmography
- CDP:
-
computerized dynamic posturography
- SCC:
-
semi-circular canals
- RNA:
-
ribonucleic acid
- DNA:
-
deoxyribonucleic acid
- PTA:
-
pure tone audiometry
- DOTS:
-
Directly Observed Therapy-Short course
- PHC:
-
primary health centers
- HFL:
-
high frequency loss
References
Adeyemo AA (2012a) Knowledge of caregivers on the risk factors of otitis media. Indian J Otol 18:184–188
Adeyemo AA (2012b) Metastatic cervical lymphadenopathy masquerading as extrapulmonary tuberculosis. Bangladesh J Otorhinolaryngol 18(2):234–237
Ali MZ, Goetz MB (1997) A meta-analysis of the relative efficacy and toxicity of single daily dosing versus multiple daily dosing of aminoglycosides. Clin Infect Dis 24:796–809
American Academy of Audiology (2009) Position statement and clinical practice guidelines. Ototoxicity monitoring. http://www.audiology.org/publications-resources/document-library/ototoxicity-monitoring. Accessed 1 Mar 2016
American Speech-Language Hearing Association (1994) Guidelines for the audiologic management of individuals receiving cochleotoxic drug therapy. Am Speech-Lang Hear Assoc 36:11–19
Bardien S, Human H, Harris T, Hefke G, Veikondis R, Schaaf HS, van der Merwe L, Greinwald JH, Fagan J, de Jong G (2009) A rapid method for detection of five known mutations associated with aminoglycoside-induced deafness. BMC Med Genet 10:2
Chamber HF, Sande MA (1996) The aminoglycosides. In: Hardman JG, Limbird LE, Molino PB, Ruddon RW, Gilman AG (eds) The pharmacological basis of therapeutics, 9th edn. McGraw-Hill, New York
De Jager P, Van Altena R (2002) Hearing loss and nephrotoxicity in long term aminoglycoside treatment in patients with tuberculosis. Int J Tuberc Lung Dis 6(7):622–627
Duggal P, Sarkar M (2007) Audiologic monitoring of multi-drug resistant tuberculosis patients on aminoglycoside treatment with long term follow-up. BMC Ear Nose Throat Disord. doi:10.1186/1472-6815-7-5
Fausti SA, Frey RH, Henry JA, Olson DJ, Schaffer HI (1992) Early detection of ototoxicity using high-frequency, tone burst-evoked auditory brainstem responses. J Am Acad Audiol 3:397–404
Fee WE (1980) Aminoglycoside ototoxicity in the human. Laryngoscope 90:1–19
Fischel-Ghodsian N (2004) Genetic factors in aminoglycoside ototoxicity. In: Roland PS, Rutka JA (eds) Ototoxicity. BC Decker, Hamilton
Gravina LP, Foncuberta ME, Estrada RC, Barreiro C, Chertkoff L (2007) Carrier frequency of the 35delG and A1555G deafness mutations in the Argentinean population. Impact on the newborn hearing screening. Int J Pediatr Otorhinolaryngol 71(4):639–643
Guan MX (2004) Molecular pathogenetic mechanism of maternally inherited deafness. Ann NY Acad Sci 1011:259–271
Guan MX (2006) Mitochondrial DNA mutations associated with aminoglycoside ototoxicity. Audiol Med 4(4):170–178
Guan MX (2011) Mitochondrial 12S rRNA mutations associated with aminoglycoside ototoxicity. Mitochondrion 11(2):237–245
Gwimile JJ, Shekalaghe SA, Kapanda GN, Kisanga ER (2012) Antibiotic prescribing practice in management of cough and/or diarrhoea in Moshi Municipality, Northern Tanzania: cross-sectional descriptive study. Pan Afr Med J 12:103
Harries AD, Dye C (2006) Tuberculosis. Ann Trop Med Parasitol 100(5–6):415–431
Harris T, Peer S, Fagan JJ (2012) Audiological monitoring for ototoxic tuberculosis, human immunodeficiency virus and cancer therapies in a developing world setting. J Laryngol Otol 126:548–551
Higashi K (1989) Unique inheritance of streptomycininduced deafness. Clin Genet 35:433–436
Hobbie SN, Bruell CM, Akshay S, Kalapala SK, Shcherbakov D, Böttger EC (2008) Mitochondrial deafness alleles confer misreading of the genetic code. Proc Natl Acad Sci 105(9):3244–3249
Hotz MA, Harris FP, Probst R (1994) Otoacoustic emissions: an approach for monitoring aminoglycoside-induced ototoxicity. Laryngoscope 104:1130–1134
Hu DN, Qiu WQ, Wu BT, Fang LZ, Zhou F, Gu YP, Zhang QH, Yan JH, Ding YQ, Wong H (1991) Genetic aspects of antibiotic induced deafness: mitochondrial inheritance. J Med Genet 28:79–83
Human H, Hagen CM, De Jong G, Harris T, Lombard D, Christiansen M, Bardien S (2010) Investigation of mitochondrial sequence variants associated with aminoglycoside-induced ototoxicity in South African TB patients on aminoglycosides. Biochem Biophys Res Commun 393(4):751–756
Ibrahim LM, Hadejia IS, Nguku P, Dankoli R, Waziri NE, Akhimien MO, Ogiri S, Oyemakinde A, Dalhatu I, Nwanyanwu O, Nsubuga P (2014) Factors associated with interruption of treatment among pulmonary tuberculosis patients in Plateau State, Nigeria. Pan Afr Med J 17:78
Jacobson GP, Newman CW (1990) The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg 116:424–427
Jones-López EC, Ayakaka I, Levin J, Reilly N, Mumbowa F, Dryden-Peterson S, Nyakoojo G, Fennelly K, Temple B, Nakubulwa S, Joloba ML, Okwera A, Eisenach KD, McNerney R, Elliott AM, Ellner JJ, Smith PG, Mugerwa RD (2011) Effectiveness of the standard WHO recommended retreatment regimen (category II) for tuberculosis in Kampala, Uganda: a prospective cohort study. PLoS Med 8:3. doi:10.1371/journal.pmed.1000427
Katijah KS, Anniah M, Precious MN (2009) Ototoxic effects of tuberculosis treatments: how aware are patients? Afr J Pharm Pharmacol 3(8):391–399
Kisilevsky VE, Tomlinson RD, Ranalli PJ, Prepageran N (2004) Monitoring vestibular ototoxicity. In: Roland PS, Rutka JA (eds) Ototoxicity. BC Decker, Hamilton, pp 161–169
Lienhardt C, Glaziou P, Uplekar M, Lönnroth K, Getahun H, Raviglione M (2012) Global tuberculosis control: lessons learnt and future prospects. Nat Rev Microbiol 10:407–416
Matthijs G, Claes S, Longo-Bbenza B, Cassiman J-J (1996) Non-syndromic deafness associated with a mutation and a polymorphism in the mitochondrial 12S ribosomal RNA gene in a large Zairean pedigree. Eur J Hum Genet 4:46–51
Men M, Jiang L, Wang H, Liu Y, Hu Z, He C, Feng Y (2011) Unique penetrance of hearing loss in a five-generation Chinese family with the mitochondrial 12S rRNA 1555A>G mutation. Acta Otolaryngol. 131(9):970–975
National Cancer Institute (2010) Common terminology criteria for adverse events version 4.03. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed 1 Mar 2016
Noller HF (1991) Ribosomal RNA and translation. Annu Rev Biochem 60:191–227
Peloquin CA, Berning SE, Nitta AT, Simone PM, Goble M, Huitt GA, Iseman MD, Cook JL, Curran-Everett D (2004) Aminoglycoside toxicity: daily versus thrice-weekly dosing for treatment of mycobacterial diseases. Clin Infect Dis 38:1538–1544
Qian Y, Guan MX (2009) Interaction of aminoglycosides with human mitochondrial 12S rRNA carrying the deafness-associated mutation. Antimicrob Agents Chemother 53:4612–4618
Rieder MJ, Taylor SL, Tobe VO, Nickerson DA (1998) Automating the identification of DNA variations using quality-based fluorescence re-sequencing: analysis of the human mitochondrial genome. Nucleic Acids Res 26:967–973
Rotstein C, Mandell L (2004) Clinical aminoglycoside ototoxicity. In: Roland P, Rutka J (eds) Ototoxicity. BC Decker, Hamilton, Ontario, pp 82–92
Schacht J (2004) Mechanisms for aminoglycoside ototoxicity: basic science research. In: Roland PS, Rutka JA (eds) Ototoxicity. BC Decker, Hamilton
Scrimshaw BJ, Faed JM, Tate WP, Yun K (1999) Rapid identification of an A1555G mutation in human mitochondrial DNA implicated in aminoglycoside-induced ototoxicity. J Hum Genet 44(6):388–390
Sturdy A, Goodman A, José RJ, Loyse A, O’donoghue M, Kon OM, Dedicoat MJ, Harrison TS, John L, Lipman M, Cooke GS (2011) Multidrug-resistant tuberculosis (MDR-TB) treatment in the UK: a study of injectable use and toxicity in practice. J Antimicrob Chemother 66:1815–1820
Swanepoel DW, Olusanya BO, Mars M (2010) Hearing health-care delivery in sub-Saharan Africa—a role for tele-audiology. J Telemed Telecare 16(2):53–56
Tang HY, Hutcheson E, Neill S, Drummond-Borg M, Speer M, Alford RL (2002) Genetic susceptibility to aminoglycoside ototoxicity: how many are at risk? Genet Med 4(5):336–345
Thyagarajan D, Bressman S, Bruno C, Przedborski S, Shanske S, Lynch T, Fahn S, DiMauro S (2000) A novel mitochondrial 12SrRNA point mutation in Parkinsonism, deafness, and neuropathy. Ann Neurol 48(5):730–736
Tran Ba Huy P, Bernard P, Schacht J (1986) Kinetics of gentamicin uptake and release in the rat: comparison of inner ear tissues and fluids with other organs. J Clin Invest 77:1492–1500
Turnidge J (2003) Pharmacodynamics and dosing of aminoglycosides. Infect Dis Clin North Am 17:503–528
Usami SI, Abe S, Kasai M, Shinkawa H, Moeller B, Kenyon JB, Kimberling WJ (1997) Genetic and clinical features of sensorineural hearing loss associated with the 1555 mitochondrial mutation. Laryngoscope 107:483–490
World Health Organisation (2010) Treatment of tuberculosis: guidelines 4th ed. http://whqlibdoc.who.int/publications/2010/9789241547833_eng.pdf?ua=1. Accessed 30 Jan 2015
World Health Organisation (2014) Deafness and hearing loss factsheet. http://www.who.int/mediacentre/factsheets/fs300/en/. Accessed 24 Jan 2015
World Health Organization (1994) Report of an informal consultation on strategies for prevention of hearing impairment from ototoxic drugs. World Health Organization. http://www.who.int/pbd/deafness/ototoxic_drugs.pdf. Accessed 24 Jan 2015
Xie J, Talaska AE, Schacht J (2011) New developments in aminoglycoside therapy and ototoxicity. Hear Res 281:28–37
Xing G, Chen Z, Wei Q, Tian H, Li X, Zhou A, Bu X, Cao X (2006) Maternally inherited non-syndromic hearing loss associated with mitochondrial 12S rRNA A827G mutation in a Chinese family. Biochem Biophys Res Commun 344(4):1253–1257
Authors’ contributions
AAA conceived and designed the project, and drafted the manuscript. OO and OOO made substantial contributions to the design and revised it critically for important intellectual content. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Funders
The study was supported with grants from the Consortium for Advanced Research and Training in Africa, Robert S McNamara World Bank Fellowship and the American Thoracic Society. The contents of this publication do not necessarily reflect the views or policies of the funders.
Author information
Authors and Affiliations
Corresponding author
Additional file
40064_2016_2429_MOESM1_ESM.pdf
Additional file 1. Drug tables: Table of drug regimen for Tb as advocated by the National Tuberculosis and Leprosy program of Nigeria.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Adeyemo, A.A., Oluwatosin, O. & Omotade, O.O. Study of streptomycin-induced ototoxicity: protocol for a longitudinal study. SpringerPlus 5, 758 (2016). https://doi.org/10.1186/s40064-016-2429-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2429-5