Abstract
Background
Detection and quantitation of BCR-ABL1 transcripts are crucial for managing patients with chronic myeloid leukemia (CML). Although real-time quantitative polymerase chain reaction (RT-qPCR) can be measured on an International Scale (IS), this has not become fully universal. By using a WHO international standard panel established for calibrating secondary standards based on the IS, we have previously developed an RT-qPCR kit, ODK-1201, for quantification of major BCR-ABL1.
Results
In this study, the reliability of kit-specific conversion factor 1.12 was validated by exchanging patients’ samples between three local clinical laboratories and a reference laboratory. The mean bias of the local method after IS conversion was 1.6 fold lower than the reference method. The clinically-useful sensitivity of the kit was further evaluated for monitoring patients with deep molecular response. Based on the correlation of the IS values between ODK-1201 and the reference laboratory method, the detection level of the kit was estimated as 0.0032 % BCR-ABL1 IS.
Conclusions
ODK-1201 is a highly sensitive one-step RT-qPCR system for detecting BCR-ABL1 on the IS in 2 h after RNA extraction, thus contributing to standardization of molecular monitoring in CML.
Similar content being viewed by others
Background
BCR-ABL is a constitutively active tyrosine kinase generated by the Philadelphia chromosome translocation, and is recognized as the underlying pathogenetic mechanisms of chronic myeloid leukemia (CML) (Yoshida and Melo 2004). Tyrosine kinase inhibitors (TKI) have dramatically changed the prognosis of patients with chronic phase CML, enabling high overall survival (O’Brien et al. 2003). They also allow a proportion of patients to achieve major molecular response (MMR), which is associated with a high progression-free survival, as firstly reported for the International Randomized Study of Interferon and STI571 (IRIS) trial (Hughes et al. 2003). Recent studies have indicated that achievement of early molecular response is translated into desirable long term prognosis (Hughes et al. 2014; Jabbour et al. 2014; Marin et al. 2012). Furthermore, cessation of TKI treatment has been attempted in patients who achieved deep molecular response, and has succeeded in maintaining prolonged treatment-free remission in a subset of patients (Mahon et al. 2010; Ross et al. 2013). Therefore, accuracy and standardization of molecular monitoring are essential for the management of CML patients.
Such monitoring is usually done by measuring BCR-ABL1 mRNA using real-time quantitative polymerase chain reaction (RT-qPCR) (Branford et al. 1999; Mensink et al. 1998). However, the data obtained by RT-qPCR demonstrate inter-laboratory variability, which hampers the proposal of guidelines for clinicians and the comparison of results in clinical studies (Zhang et al. 2007). For the harmonization of molecular monitoring in CML, an International Scale (IS) was proposed in 2005 and widely used in current clinical recommendations and guidelines (Baccarani et al. 2013; Hughes et al. 2006; NCCN 2016). It is based on a standardized baseline defined as 100 % BCR-ABL1 IS, and a MMR defined as 0.1 % BCR-ABL1 IS (i.e., a 3-log reduction from the standardized baseline, also referred to as MR3), as established in the IRIS trial (Hughes et al. 2006). To use this system, each laboratory needs to calibrate their data to the IS by multiplying the result of their measurement by a laboratory-specific conversion factor (CF) (Branford et al. 2008). However, it is not-straightforward to obtain the CF because it requires the exchange of clinical samples between local and reference laboratories. To solve the issue, primary BCR-ABL standard material based on the IS was developed and approved by the WHO (White et al. 2010).
We have previously reported the development of a one-step RT-qPCR kit, ODK-1201. The kit-specific CF was 1.12 determined by using the WHO standard panel. The assay performance was shown as limit of detection 0.0007 % using diluted samples containing low level of BCR-ABL1, but not using clinical samples (Nakamae et al. 2015). This is an extension of the work aimed to validate the kit-specific CF by patient’s sample exchange between local laboratories and a worldwide reference laboratory, which has been recognized as a standard method for adaptation to the IS. Furthermore, it is intended to verify accuracy, inter-laboratory reproducibility, and clinically-useful sensitivity for improved clinical utility of the kit.
Methods
Study design and data analyses
Two clinical studies (ODK-1201-01, ODK-1201-02) were carried out to identify of the performance of ODK-1201 and to get the laboratory-specific CF, sponsored by Otsuka Pharmaceutical Co. Ltd. Total 468 CML patients were recruited for these studies, and peripheral blood samples were taken after written informed consent in 24 institutions in Japan, between July 2012 and October 2013. These studies were conducted in accordance with the Declaration of Helsinki, and its design was approved by each hospital’s Institutional Review Board. The samples were firstly analyzed in three commercial laboratories, BML, Inc., SRL, and LSI Medience Corporation (previously Mitsubishi Chemical Medience Corporation) in Japan, and thereafter in SA Pathology, Adelaide, Australia, a recognized reference laboratory (Branford et al. 2008; Hughes et al. 2003). Only samples with the standard b2a2 (e13a2) and/or b3a2 (e14a2) BCR-ABL1 transcripts were included. For the validation of obtained values by ODK-1201, negative samples and samples with >10 % BCR-ABL1 IS were excluded from analysis, since the IS measurement was shown to be effective in the range of 10 % BCR-ABL1 IS or below (Branford et al. 2008). A patient bias conversion method was used to determine the CF for the IS, as previously described (Bland and Altman 1986; Branford et al. 2008). In the validation step, the bias between the kit and the reference method was calculated before and after conversion to the IS using the specific CF of each method. The estimated mean bias of the kit method after conversion was calculated as the average fold difference compared with the reference method.
Experimental design
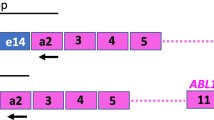
A 7-mL blood sample was taken from the patients in participating hospitals and transferred to the local laboratories. RNA extraction was carried out using the QIAamp RNA Blood Mini Kit (QIAGEN, Duesseldorf, Germany) in BML, RNeasy Mini Kit (QIAGEN) in SRL, or RNeasy Lipid Tissue Mini Kit (QIAGEN, Duesseldorf, Germany) in LSI, respectively. The study diagnostic kit in this study was coded ODK-1201. It is based on a HawkZ05 Fast One-Step RT-qPCR Kit (Roche, Indianapolis, IN, USA). In this kit, reverse transcription and quantitative PCR are performed in one tube. The analysis was carried out on an ABI™ 7500 Fast Dx system (Applied Biosystems, Foster City, California). In the quantitation with this kit, specific regions of major BCR-ABL1 mRNA and ABL1 mRNA transcripts were amplified by RT-qPCR and quantitated by using probes specific to the amplified products. The primers for ABL1 hybridize to not only ABL1 but also BCR-ABL1. In each assay with ODK-1201, 1 μg of RNA (10 μL) was added to a mixture of 13 μL of mix solution (R1) for RT-qPCR and 2 μL of Mn(OCOCH3)2 solution and applied to ABI™ 7500 Fast Dx system. The assay conditions have been described previously (Nakamae et al. 2015). Five 20-fold dilutions from a standard RNA solution included in the kit were used to create the standard curve for BCR-ABL1and ABL1. The test results were compared to the standard curve to yield the quantity of BCR-ABL1 and ABL1 mRNA. To calculate the kit-specific CF for the IS, the WHO International Standard panel was obtained from The National Institute for Biological Standards and Control (NIBSC, UK), and analyzed according to the suggested method for calibration of secondary standards (http://www.nibsc.org/documents/ifu/09-138.pdf). The panel comprises four ampoules, each containing freeze-dried BCR-ABL1-positive and -negative cells at various ratios from 0.01 to 10 % BCR-ABL1 IS. RNAs were isolated from each ampoule with a QIAamp RNA Blood Mini Kit (QIAGEN) and were subjected to the measurement of major BCR-ABL1 and ABL1 mRNAs with the ODK-1201 kit. The CF of the ODK-1201 was calculated by comparing the values of % BCR-ABL1/ABL1 obtained with the kit with those from the WHO standard panel. The RT-qPCR method carried out at the Adelaide reference laboratory has been previously detailed (Branford et al. 1999).
Results
The ODK-1201 kit-specific CF was 1.12 determined by using the WHO standard panel by following the method for calibration of secondary standards as outlined in White et al. (2010). The calculation method of the CF was presented in Fig. 1a, b, which was not detailed in our previous report (Nakamae et al. 2015).
CF calculation and validation of ODK-1201. a, Visual inspection of the data used for the CF calculation for ODK-1201 using WHO standard material. b Data bias plot using the Bland and Altman method (Bland and Altman 1986). c Visual inspection of the converted validation data of the kit-specific CF. d Validation data bias plot using the Bland and Altman method (Bland and Altman 1986)
The reliability of the kit-specific CF was next validated by analyzing the patients’ samples. A total of 106 samples were first tested with ODK-1201 in three local clinical laboratories (36, 34, and 36 samples each), and then sent to the reference laboratory. None of the samples was degraded. The BCR-ABL1 values from the reference and the local laboratories were converted to the IS by multiplying by their specific CFs. The samples with positive BCR-ABL1 values were converted to the IS using the CF 1.12 and compared (Fig. 1c, d). The mean bias of the local method after IS conversion was 1.6 fold lower than the reference method data. The upper and lower 95 % limits of agreement after IS conversion was −0.614 fold and 0.220 fold, respectively. The mean bias in the three individual local laboratories after IS conversion was 1.4-fold, 1.6-fold, and 1.8-fold lower than the reference method, respectively, indicating relatively small inter-laboratory variation of the results using the kit.
The overall concordance of the data between ODK-1201 and the reference laboratory systems was acceptable (Fig. 1c), although the bias was slightly outside the stringent criteria previously suggested (Branford et al. 2008). After conversion to the IS, 74 % of values were within twofold, 94 % within threefold, and 98 % within fivefold of the reference laboratory value. The concordance in labelling a sample as MMR (i.e., a BCR-ABL1 value of 0.10 % BCR-ABL1 IS) between the reference method and the ODK-1201was determined as 84 % (N = 43/51) of samples.
Recent improvement in CML therapy with TKI requires detection of minimal residual disease with high sensitivity, i.e., less than 0.1 % BCR-ABL1 IS. To verify the clinically-useful sensitivity of the ODK-1201 kit, we tested the correlation between the two methods in the assessment of 46 clinical samples with IS between the lowest positive value (LPV) and 0.1 % BCR-ABL1 IS. A high correlation coefficient (r = 0.89) was found (Fig. 2), suggesting that ODK-1201 can detect transcripts at the level of 0.0032 % BCR-ABL1 IS.
Discussion
The development of molecular targeted drug therapy has changed the prognosis of patients with various cancers. One of the most successful models is chronic phase CML, which has a well-documented mechanism of carcinogenesis, the constitutively active BCR-ABL kinase generated by the Philadelphia chromosome translocation (Rowley 1973). TKIs target the oncoprotein and have dramatically improved the prognosis of patients with CML (Kantarjian et al. 2010; O’Brien et al. 2003; Saglio et al. 2010). It is important to accurately evaluate the therapeutic effect and appropriately modify the treatment for achieving optimal response. However, standardization of minimal residual disease quantification has been difficult to implement even in this model neoplasia. Here, we evaluated an RT-qPCR kit, ODK-1201, which can measure BCR-ABL1 transcripts on the IS with high sensitivity, in a single tube, in two hours after the RNA extraction procedure.
The achievement of MMR has been recognized as the therapeutic goal for chronic-phase CML patients based on the results reported on the IRIS trial and subsequent ones (Baccarani et al. 2009; Hughes et al. 2003; Marin et al. 2008). Furthermore, molecular responses of less than 0.01 % BCR-ABL1 IS or deeper are becoming the next target. A few clinical trials have shown that approximately 40 % of chronic phase CML patients who achieved and sustained a deep molecular response could stop administration of TKI and maintain treatment free remission (Mahon et al. 2010; Ross et al. 2013). Thus, accurate and reproducible molecular monitoring is essential for treatment management in CML, and the lack of standardization may lead to a diagnostic misclassification. Nonetheless, it is not widely understood that the RT-qPCR technique potentially produces highly variable quantitative data which may affect the validity of results and decision on treatments (Zhang et al. 2007). Establishment of the laboratory-specific CF, which has been used for standardization based on the IS is lengthy, costly, and not realistic for many clinical laboratories, because of the limited number of reference laboratories, currently only Mannheim and Adelaide, with which to exchange samples (Cross et al. 2008). Furthermore, the CF is recommended to be revalidated on a yearly basis or in case of changing reagents for RT-qPCR at a local laboratory (Muller et al. 2010). To improve the harmonization process, a WHO international standard panel directly linked to the IS was developed in 2009 (White et al. 2010). However, the IS was initially designed to express the quantification of BCR-ABL1 transcripts in the range of MMR (as 0.10 % BCR-ABL1 IS) to standardized baseline (as 100 % BCR-ABL1 IS) established in the IRIS study, but not deeper molecular response (Hughes et al. 2006). The WHO standard panel was validated only for BCR-ABL1 detection in the range 0.01–10 % BCR-ABL1 IS (White et al. 2010). It means that validation of systems for measuring BCR-ABL1 less than 0.01 % BCR-ABL1 IS has not been formally developed. Therefore, we carried out the current study to evaluate clinical usefulness of the ODK-1201, especially at the deep molecular response, by the clinical sample exchange, and showed that the kit detects BCR-ABL1 at the level of 0.0032 % BCR-ABL1 IS, as validated by a worldwide reference laboratory. The LPV of the kit is 0.0007 % BCR-ABL1 IS (Nakamae et al. 2015), suggesting that it has the potential to detect BCR-ABL1 at the level of a 5-log reduction from the standard baseline (MR5). In contrast, when BCR-ABL1-negative samples were analyzed by the kit, BCR-ABL1 transcripts was never detected, suggesting low false positivity of the kit (data not shown). Of note, the measurement can be carried out using only 7 mL of blood, a sample which is smaller than the previously recommended volume (Baccarani et al. 2013).
The variation of results obtained by RT-qPCR is due to each stage of the procedure, including sample collection, transportation time from clinics to laboratories, RNA extraction, reverse transcription, and the actual quantitative PCR (Branford et al. 2006). The difference in internal control genes also largely affects the variation. It is imperative to consider and optimize all parameters to obtain meaningful results reported on the IS. It is recommended that samples should be stabilized immediately after collection of blood from patients, to avoid RNA degradation. More importantly, each laboratory must carry out appropriate quality controls with every batch of samples in order to monitor for shifts in the data. It is essential to ensure that samples are re-tested if the quality control results fall outside the acceptable range (Branford et al. 2006). Of note, the mean bias between the local methods in the three local laboratories after IS conversion was relatively small, indicating accuracy and inter-laboratory reproducibility of the kit. All of the three locations are major commercial clinical laboratories in Japan with strict quality control, and two of them had experience in obtaining laboratory-specific CFs using their own procedure before participation in the current study (Yoshida et al. 2012). This may have led to the relatively small mean bias shown in the three laboratories using the kit. Further studies with the participation of several laboratories worldwide are warranted for advancing the standardization of RT-qPCR measuring BCR-ABL1 using commercial kits.
Conclusions
ODK-1201 is a rapid one-step high sensitivity RT-qPCR system for detecting BCR-ABL1 based on the IS, which contributes a useful tool for evaluation of deep molecular responses and standardization of treatment in CML.
Abbreviations
- CML:
-
chronic myeloid leukemia
- RT-qPCR:
-
real-time quantitative polymerase chain reaction
- IS:
-
international scale
- TKI:
-
tyrosine kinase inhibitors
- MMR:
-
major molecular response
- IRIS:
-
International Randomized Study of Interferon and STI571
- CF:
-
conversion factor
- LPV:
-
lowest positive value
References
Baccarani M, Cortes J, Pane F, Niederwieser D, Saglio G, Apperley J, Cervantes F, Deininger M, Gratwohl A, Guilhot F, Hochhaus A, Horowitz M, Hughes T, Kantarjian H, Larson R, Radich J, Simonsson B, Silver RT, Goldman J, Hehlmann R (2009) Chronic myeloid leukemia: an update of concepts and management recommendations of European LeukemiaNet. J Clin Oncol 27:6041–6051
Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, Cervantes F, Clark RE, Cortes JE, Guilhot F, Hjorth-Hansen H, Hughes TP, Kantarjian HM, Kim DW, Larson RA, Lipton JH, Mahon FX, Martinelli G, Mayer J, Muller MC, Niederwieser D, Pane F, Radich JP, Rousselot P, Saglio G, Saussele S, Schiffer C, Silver R, Simonsson B, Steegmann JL, Goldman JM, Hehlmann R (2013) European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood 122:872–884
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Branford S, Hughes TP, Rudzki Z (1999) Monitoring chronic myeloid leukaemia therapy by real-time quantitative PCR in blood is a reliable alternative to bone marrow cytogenetics. Br J Haematol 107:587–599
Branford S, Cross NC, Hochhaus A, Radich J, Saglio G, Kaeda J, Goldman J, Hughes T (2006) Rationale for the recommendations for harmonizing current methodology for detecting BCR-ABL transcripts in patients with chronic myeloid leukaemia. Leukemia 20:1925–1930
Branford S, Fletcher L, Cross NC, Muller MC, Hochhaus A, Kim DW, Radich JP, Saglio G, Pane F, Kamel-Reid S, Wang YL, Press RD, Lynch K, Rudzki Z, Goldman JM, Hughes T (2008) Desirable performance characteristics for BCR-ABL measurement on an international reporting scale to allow consistent interpretation of individual patient response and comparison of response rates between clinical trials. Blood 112:3330–3338
Cross NC, Hughes TP, Hochhaus A, Goldman JM (2008) International standardisation of quantitative real-time RT-PCR for BCR-ABL. Leuk Res 32:505–506
Hughes TP, Kaeda J, Branford S, Rudzki Z, Hochhaus A, Hensley ML, Gathmann I, Bolton AE, van Hoomissen IC, Goldman JM, Radich JP (2003) Frequency of major molecular responses to imatinib or interferon alfa plus cytarabine in newly diagnosed chronic myeloid leukemia. N Engl J Med 349:1423–1432
Hughes T, Deininger M, Hochhaus A, Branford S, Radich J, Kaeda J, Baccarani M, Cortes J, Cross NC, Druker BJ, Gabert J, Grimwade D, Hehlmann R, Kamel-Reid S, Lipton JH, Longtine J, Martinelli G, Saglio G, Soverini S, Stock W, Goldman JM (2006) Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood 108:28–37
Hughes TP, Saglio G, Kantarjian HM, Guilhot F, Niederwieser D, Rosti G, Nakaseko C, De Souza CA, Kalaycio ME, Meier S, Fan X, Menssen HD, Larson RA, Hochhaus A (2014) Early molecular response predicts outcomes in patients with chronic myeloid leukemia in chronic phase treated with frontline nilotinib or imatinib. Blood 123:1353–1360
Jabbour E, Kantarjian HM, Saglio G, Steegmann JL, Shah NP, Boque C, Chuah C, Pavlovsky C, Mayer J, Cortes J, Baccarani M, Kim DW, Bradley-Garelik MB, Mohamed H, Wildgust M, Hochhaus A (2014) Early response with dasatinib or imatinib in chronic myeloid leukemia: 3-year follow-up from a randomized phase 3 trial (DASISION). Blood 123:494–500
Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M, Moiraghi B, Shen Z, Mayer J, Pasquini R, Nakamae H, Huguet F, Boque C, Chuah C, Bleickardt E, Bradley-Garelik MB, Zhu C, Szatrowski T, Shapiro D, Baccarani M (2010) Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 362:2260–2270
Mahon FX, Rea D, Guilhot J, Guilhot F, Huguet F, Nicolini F, Legros L, Charbonnier A, Guerci A, Varet B, Etienne G, Reiffers J, Rousselot P, Intergroupe Francais des Leucemies Myeloides Chronique (2010) Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol 11:1029–1035
Marin D, Milojkovic D, Olavarria E, Khorashad JS, de Lavallade H, Reid AG, Foroni L, Rezvani K, Bua M, Dazzi F, Pavlu J, Klammer M, Kaeda JS, Goldman JM, Apperley JF (2008) European LeukemiaNet criteria for failure or suboptimal response reliably identify patients with CML in early chronic phase treated with imatinib whose eventual outcome is poor. Blood 112:4437–4444
Marin D, Hedgley C, Clark RE, Apperley J, Foroni L, Milojkovic D, Pocock C, Goldman JM, O’Brien S (2012) Predictive value of early molecular response in patients with chronic myeloid leukemia treated with first-line dasatinib. Blood 120:291–294
Mensink E, van de Locht A, Schattenberg A, Linders E, Schaap N, Geurts van Kessel A, De Witte T (1998) Quantitation of minimal residual disease in Philadelphia chromosome positive chronic myeloid leukaemia patients using real-time quantitative RT-PCR. Br J Haematol 102:768–774
Muller MC, Munjal U, Erben P, Lion T, Mitterbauer-Hohendanner G, El Housni H, Boeckx N, Zadro R, Mayer J, Rohon P, Rulcova J, Grubach L, Raudsepp K, Kairisto V, Mahon F-X, Preudhomme C, Hayette S, Gabert J, Cayuela J-M, Thiede C, Galonska L, Pfeifer H, Hirt C, Schafhausen P, von Neuhoff N, Roskos M, Pott C, Lange T, Hess G, Schnittger S, Dufour A, Koschmieder S, Stegelmann F, Zoi K, Stamatopoulos K, Andrikovics H, Tohami T, Martinelli G, Izzo B, Gottardi E, Stoskus M, Nymoen DA, Sacha T, Diamond J, Talmaci R, Misyurin A, Dubina MV, Pajic T, Nomdedeu JF, Colomer D, Barbany-Bustinza G, Ehrencrona H, Leibundgut EO, Janssen J, Van Der Elden VHJ, Valk PJM, Ozbek U, Wang L, Gerrard G, White HE, Schenk T, Ernst T, Hehlmann R, Saglio G, Hochhaus A, Cross NCP (2010) Stability of conversion factors for BCR-ABL monitoring—implications for the frequency of validation rounds. ASH Ann Meet Abstr 116:893
Nakamae H, Yoshida C, Miyata Y, Hidaka M, Uike N, Koga D, Sogabe T, Matsumura I, Kanakura Y, Naoe T (2015) A new diagnostic kit, ODK-1201, for the quantitation of low major BCR-ABL mRNA level in chronic myeloid leukemia: correlation of quantitation with major BCR-ABL mRNA kits. Int J Hematol 102:304–311
NCCN clinical Practice Guidelines in Oncology; Chronic Myelogenous Leukemia. Version 1 (2016) http://www.nccn.org/professionals/physician_gls/pdf/cml.pdf. Accessed 17 Apr 2016
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F, Cornelissen JJ, Fischer T, Hochhaus A, Hughes T, Lechner K, Nielsen JL, Rousselot P, Reiffers J, Saglio G, Shepherd J, Simonsson B, Gratwohl A, Goldman JM, Kantarjian H, Taylor K, Verhoef G, Bolton AE, Capdeville R, Druker BJ (2003) Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 348:994–1004
Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Yeung DT, Dang P, Goyne JM, Slader C, Filshie RJ, Mills AK, Melo JV, White DL, Grigg AP, Hughes TP (2013) Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood 122:515–522
Rowley JD (1973) Letter: a new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature 243:290–293
Saglio G, Kim DW, Issaragrisil S, le Coutre P, Etienne G, Lobo C, Pasquini R, Clark RE, Hochhaus A, Hughes TP, Gallagher N, Hoenekopp A, Dong M, Haque A, Larson RA, Kantarjian HM (2010) Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med 362:2251–2259
White HE, Matejtschuk P, Rigsby P, Gabert J, Lin F, Lynn Wang Y, Branford S, Muller MC, Beaufils N, Beillard E, Colomer D, Dvorakova D, Ehrencrona H, Goh HG, El Housni H, Jones D, Kairisto V, Kamel-Reid S, Kim DW, Langabeer S, Ma ES, Press RD, Romeo G, Wang L, Zoi K, Hughes T, Saglio G, Hochhaus A, Goldman JM, Metcalfe P, Cross NC (2010) Establishment of the first World Health Organization International Genetic Reference Panel for quantitation of BCR-ABL mRNA. Blood 116:e111–e117
Yoshida C, Melo JV (2004) Biology of chronic myeloid leukemia and possible therapeutic approaches to imatinib-resistant disease. Int J Hematol 79:420–433
Yoshida C, Fletcher L, Ohashi K, Wakita H, Kumagai T, Shiseki M, Matsuei K, Inokuchi K, Hatta Y, Shirasugi Y, Yamaguchi T, Sakamoto J, Branford S, Sakamaki H (2012) Harmonization of molecular monitoring of chronic myeloid leukemia therapy in Japan. Int J Clin Oncol 17:584–589
Zhang T, Grenier S, Nwachukwu B, Wei C, Lipton JH, Kamel-Reid S, Association for Molecular Pathology Hematopathology Subdivision (2007) Inter-laboratory comparison of chronic myeloid leukemia minimal residual disease monitoring: summary and recommendations. J Mol Diagn 9:421–430
Authors’ contributions
CY investigated the study, collected the data, and wrote the manuscript. HN investigated the study, and collected the data. LF performed the analysis. SB performed the analysis and edited the manuscript. DK and TS designed the study and edited the manuscript. IM, YK and TN supervised the project. All authors read and approved the final manuscript.
Acknowledgements
The following investigators participated in this study: Takuya Komeno (National Hospital Organization Mito Medical Center), Morio Matsumoto (Nishi-Gunma Hospital), Yasuhiko Miyata (National Hospital Organization Nagoya Medical Center), Takuo Ito (National Hospital Organization Kure Medical Center), Takeshi Shimomura (National Hospital Organization Hiroshima-nishi Medical Center), Naokuni Uike (Kyushu Cancer Center), Shinichiro Yoshida (National Hospital Organization Nagasaki Medical Center), Michihiro Hidaka (National Hospital Organization Kumamoto Medical Center), Shuichi Hanada (National Hospital Organization Kagoshima Medical Center), Maeda Yasuhiro (Osaka-Minami Medical Center), Satoru Kosugi (Toyonaka Municipal Hospital), Mitsuru Tsudo (Osaka Red Cross Hospital), Masayuki Hino (Osaka City University), Yasuhito Nanya (The University of Tokyo Hospital), Yasunori Ueda (Kurashiki Central Hospital), Chikara Hirase (Kinki University Hospital), Takashi Eto (Hakata Clinic), Kenshi Suzuki (Japanese Red Cross Medical Center), Masahiro Abe (Tokushima University Hospital), Masaya Okada (Hyogo College of Medicine), Kazuma Ohyashiki (Tokyo Medical University), Kaichi Nishiwaki (Jikei University Kashiwa Hospital), Nobuyuki Aotsuka (Narita Red Cross Hospital), Takayuki Ishikawa (Kobe City Medical General Hospital). We are grateful to Prof. Junia V. Melo, University of Adelaide, for medical editing of the manuscript.
Competing interests
These results are summarized from the clinical study of ODK-1201 kit (Sponsored by Otsuka Pharmaceutical Co. Ltd.). C.Y. received grants and personal fees from Otsuka Pharmaceutical, during the conduct of the study; personal fees from Bristol-Myers Squibb, personal fees from Novartis, personal fees from Pfizer, outside the submitted work. H.N. received research funding from Otsuka during the conduct of the study and received research funding and honoraria from Otsuka outside the submitted work. L.F. has no conflict of interest. K.D. and T.S. are employee of Otsuka. I.M. and Y.K. have provided consultancy and received honoraria from Otsuka. S.B. received grants from Otsuka Pharmaceuticals, during the conduct of the study; grants from Novartis, grants from Ariad, outside the submitted work. T.N. received grants and personal fees from Otsuka Pharmaceutical Co., Ltd., during the conduct of the study; grants and personal fees from Bristol-Myers Squibb, grants and personal fees from Celgene K.K., grants and personal fees from Chugai Pharmaceutical Co., Ltd., grants and personal fees from Dainippon Sumitomo Pharma Co., Ltd., grants and personal fees from Fujifilm Corporation, grants and personal fees from Kyowa-Hakko Kirin Co., Ltd., grants and personal fees from Nippon Boehringer Ingelheim Co., Ltd., grants and personal fees from Novartis Pharma, grants and personal fees from Otsuka Pharmaceutical Co., Ltd., grants from Zenyaku Kogyo Co., Ltd., outside the submitted work.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki, and its design was approved by each hospital’s Institutional Review Board. All patients participated to this study after written informed consent.
Funding
This study is funded by Otsuka Pharmaceutical Co. Ltd.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Yoshida, C., Nakamae, H., Fletcher, L. et al. Validation of a rapid one-step high sensitivity real-time quantitative PCR system for detecting major BCR-ABL1 mRNA on an International Scale. SpringerPlus 5, 569 (2016). https://doi.org/10.1186/s40064-016-2258-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2258-6