Abstract
Background
‘Smoker’s paradox’ is a controversial phenomenon of an unexpected favourable outcome of smokers post acute myocardial infarction. There are conflicting evidences from the literature so far. We investigate for the existence of this phenomenon in our post acute myocardial infarction patients.
Methods
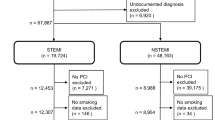
We analysed 12,442 active smokers and 10,666 never-smokers diagnosed with STEMI and NSTEMI from the Malaysian National Cardiovascular Database-Acute Coronary Syndrome (NCVD-ACS) year 2006–2013 from 18 hospitals across Malaysia. Comparisons in the baseline characteristics, clinical presentation, in-hospital treatment and short term clinical outcome were made between the two groups. To compare the clinical outcome, an extensive multivariate adjustment was made to estimate the allcause mortality risk ratios for both groups.
Results
The active smokers were younger (smokers 53.7 years vs non-smokers 62.3 years P < 0.001) and had lower cardiovascular risk burden and other co-morbidities. STEMI is more common in smokers and intravenous thrombolysis was the main reperfusion therapy in both groups. Smokers had a higher rate of in-hsopital coronary revascularisation in NSTEMI group (21.6 % smokers vs 16.7 % non-smokers P < 0.001) but similar to non-smokers in the STEMI group. Multivariate adjusted mortality risk ratios showed significantly lower mortality risks of smokers at both in-hospital (RR 0.510 [95 % CI 0.442–0.613]) and 30-day post discharge (RR 0.534 [95 % CI 0.437–0.621]).
Conclusion
Smoking seems to be associated with a favourable outcome post myocardial infarction. The phenomenon of ‘smoker’s paradox’ is in fact a reality in our patients population. The definitive explanation for this unexpected protective effect of smoking remains unclear.
Similar content being viewed by others
Background
Smoking is a well established risk factor for cardiovascular disease (Chen and Boreham 2002). ‘Smoker’s paradox’ is, however, an observational phenomenon of an unexpected favourable outcome in smokers post acute myocardial infarction (MI). There has been great interest in this controversy over the past decades. Some suggest that the paradoxical favourable outcome is due to the more ‘thrombotic’ nature of MI in smokers as oppose to atherosclerotic in non-smokers and hence better reperfusion response after thrombolyis (Grines et al. 1995; Zahger et al. 1995). Others argue that smokers were younger at the onset with better baseline prognostic factors such as lower rate of diabetes and hypertension among others (Weisz et al. 2005; Kelly et al. 1985). Nevertheless there is no universally accepted satisfactory explanation for this. Thus, we investigate for the existence of ‘smoker’s paradox’ in our post-MI population by means of anonymous patients data from the Malaysian National Cradiovascular Database registry-Acute coronary syndrome (NCVD-ACS) year 2006–2013.
Methods
Study subjects and data collection
The Malaysian National Cardiovascular Disease Database-Acute Coronary Syndrome (NCVD-ACS) registry was used to identify patients from 17 hospitals across Malaysia admitted with ST-elevation MI (STEMI) and non-ST elevation MI (NSTEMI) from the year 2006 to 2013. NVCD registry is a prospective registry sponsored by the Ministry of Health, Malaysia (MoH) and co-sponsored by the National Heart Association of Malaysia (NHAM). A total of 23,108 patients were identified for this study. Patients selected were either active smokers (n = 12,442) or non-smokers (n = 10,666). Active smokers were defined as patients having regularly smoked tobacco products/product (includes cigarettes, cigars or pipes) one or more times per day or have smoked within the 30 days prior to the admission. Non-smokers were defined as patients who have never smoked for their entire lives. Baseline characteristics, clinical presentation, in-hospital treatment, procedural details and clinical outcome at discharge and at 30 days post discharge. Record matching against the National Death Register, Malaysia was performed to verify the mortality status (alive or dead) of all study patients.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and median (IQR) if skewed. The differences between active smokers and non-smokers were analysed using t test or Wicoxon rank sum test (if skewed). Categorical variables were described as numbers (percentages), and differences were analysed using the Chi-square test or the Fisher exact test. To hinder biases in the estimates and loss of power, missing data for explanatory variables were assumed to be missing at random. A generalized linear model with a log link, binomial distribution, and a robust variance estimator was used to estimate the risk ratios. The risk ratios represent the relative risk for mortality of the patients in non-smokers compared to active smokers. Variables that were statistically significantly different (a 2-sided P value of less than 0.05) between active smokers and non-smokers, that were of clinical importance, and that had sufficient outcomes in the respective subcategories were adjusted for in the model. Statistical significance was considered if the P value was less than 0.05 and the 95 % confidence intervals of risk ratios excluded the value of 1. All analyses were conducted using SPSS statistical software (version 21, IBM SPSS Statistics, USA).
Ethics approval and consent
This NCVD registry study was approved by the Medical Review & Ethics Committee (MREC), MOH Malaysia in 2007 (Approval Code: NMRR-07-20-250). MREC waived informed consent for NCVD.
Results
Patients baseline characteristics (Table 1)
Demographics (Table 1)
Active smokers were significantly younger (53.7 vs 62.3 years P < 0.001) with higher male to female dominancy (97.9 vs 53.6 % P < 0.001) and Malay racial group (59.9 vs 45.7 % P < 0.001).
Cardiovascular risk factors and co-morbidities (Table 1)
Active smokers showed a better cardiovascular risk factor profile with significantly lower rate of diabetes mellitus (29.7 vs 52.8 % P < 0.001), hypertension (42.3 vs 69.3 % P < 0.001) and dyslipidaemia (23.6 vs 36.0 % P < 0.001). However the active smokers have higher rate of family history of premature coronary artery disease (CAD) (12.8 vs 9.9 % P < 0.001).
Other co-morbidities of previous cerebrovascular disease, congestive cardiac failure, chronic renal failure, chronic lung disease and peripheral vascular disease were also significantly lower in the active smoking group.
ACS presentation and killip class (Table 1)
There is a significantly higher rate of STEMI in active smokers compared to the non-smokers (77.2 vs 53.3 % P < 0.001). Within STEMI patients, the smokers had more patients who presented without clinical evidence of LV dysfunction (Killip 1) (66.1 vs 61.9 % P < 0.001).
In-hospital acute treatment, coronary revascularisation and evedence-based pharmacotherapy (Table 2)
Acute reperfusion therapy (Table 2)
Majority of the STEMI patients received IV thrombolysis (smokers 77.1 % vs non-smokers 69.0 %) with only a small minority had primary PCI done (smokers 9.5 % vs non-smokers 11.3 %). The median door to needle time was significantly shorter in the smokers’ group (smokers 45 min vs non smokers 50 min).
In-hospital coronary angiogram/angioplasty and pharmacotherapy (Table 2)
In the STEMI group, the smokers received similar rate of invasive coronary revascularisation (29.8 % smokers vs 29.2 % non-smokers). However in NSTEMI, the invasive revascularisatio rate is significantly higher in smokers (21.6 % smokers vs 16.7 % non-smokers). In terms of the evidence-based pharmacotherapy, more active smokers received aspirin (93.8 % smokers vs 87.9 % non-smokers) and statin (90.5 % smokers vs 86.3 % non-smokers) compared to the non-smokers. The rate of other medications were the same for both groups.
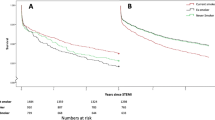
Clinical outcome (all-cause mortality) (Tables 3 and 4)
In-hospital all-cause mortality (Table 3)
The in-hospital mortality rates for STEMI, NSTEMI and overall groups were all consistently lower in active smokers compared to the non smokers. Despite extensive multi-variate adjustments of all confounding factors, the mortality risk ratios remained significantly lower in smokers across all groups. STEMI RR 0.628 [95 % CI 0.586–0.673] P < 0.001, NSTEMI RR 0.423 [95 % CI 0.369–0.575] P value <0.001, and overall RR 0.510 [95 % CI 0.442–0.613] P < 0.001.
30-day post discharge all-cause mortality (Table 4)
The mortality rate and the unadjusted mortality risk ratios remained lower in the active smokers at 30-day post discharge within all groups (STEMI, NSTEMI and overall). Again, even after extensive confounding multivariate risk adjustments, the risk ratios for active smokers were found to be significantly lower than non-smokers across all groups. STEMI RR 0.635 [95 % CI 0.592–0.681] P value <0.001, NSTEMI RR 0.489 [95 % CI 0.421–0.589] P value <0.001 and Overall RR 0.534 [95 % CI 0.437–0.621] P value <0.001.
Discussion
Our population has high prevalence of smoking. According to the National Health and Morbidity Survey (NHMS) Malaysia, the prevalence of adult male smokers in Malaysian population is 46.5 %, highest among the Malays (55.9 %), lower education group and rural areas (Lim et al. 2013). Reports from other regions regarding the unexpected favourable outcome of smokers post myocardial infarction has dated back to the pre-thrombolytic era of STEMI (Kelly et al. 1985; Helmers 1973). There have been great debates in the literature on this controversial topic and it has oftenly been disputed mainly on the confounding age and pre-morbid differences which favour smokers than the non-smokers in general (Grines et al. 1995; Barbash et al. 1995; Zuhdi et al. 2013).
Nevertheless, the main pathogenesis of acute myocardial infarction in smokers has been reported to differ from those of non-smokers. There is documented increase in haematocrit and fribrinogen levels in smokers which predispose them more to intra-coronary thrombosis (Sambola et al. 2003). It is thus suggested that the coronary flow limitation is largely due to thrombogenic obstruction with minimal underlying atherosclerotic narrowing. Where as, in non-smokers it is the atherosclerotic narrowing which is predominant (Grines et al. 1995; Zahger et al. 1995). With this came the theory of fibrin-rich thrombus in smokers which is said to be more susceptible to thrombolysis/anti-coagulation and theoretically leads to the seemingly better outcome of smokers particularly in the thrombolytic era (Aune et al. 2011). Some other hypotheses include higher case-fatality among smokers even before reaching the hospitals (Sonke et al. 1997) and the ischaemic preconditioning effect of tobacco (Gupta et al. 2014). However, these remain as theories without sufficient data for definitive proof to relate them to the favourable clinical outcome of smokers.
In one study, the response in myocardial reperfusion after thrombolytic therapy in smokers were objectively assessed and compared to non-smokers in a study using TIMI myocardial perfusion grade (TMPG) which showed better response in smokers (Kirtane et al. 2005). However more recent data in the era of primary PCI showed no significant difference betweeen smokers and non-smokers (De Luca et al. 2014; Allahwala et al. 2013) and smokers benefit equally from PCI and thrombolysis (Rasmussen et al. 2012).
Our study was done in the background of IV thrombolysis as the dominant reperfusion strategy for STEMI. Only a small minority (<10 %) of STEMIs underwent primary PCI and overall in-hospital coronary revascularisation was around 30 %. The NSTEMI patients were treated mainly with non-invasive pharmacotherapy with only around 20 % received in hospital coronary revascularisation. After extensive covariates adjustments, we observed that active smokers had a (overall) significantly lower in-hospital mortality risk compared to those who never smoked. Sub-group analysis of STEMI and NSTEMI were both consistent with a lower adjusted mortality risk compared to non-smokers. At 30-day post discharge, the trend in lower adjusted mortality risks were sustained across all groups with smokers maintaining the protective effect.
However this study only looked at the immediate clinical outcome (in-hospital and 30-day post discharge). Patients’ smoking status after the myocardial infarction was not assessed and hence the sustainability of the favourable effect of smoking in the long run for our patients remains unknown. Some recent data showed that smoking is actually related to increased long term mortality (Robertson et al. 2014; Takagi et al. 2014) and quitting smoking is associated with improved survival after acute coronary syndromes (Gerber et al. 2009; Chow et al. 2010). This comes as the suggestion that cigarette smoking may increase platelet aggregation in patients with ischemic heart disease in an aspirin nonresponsive manner (Pamukcu et al. 2011). All these data suggests that favourable smokers’ paradox effect is only limitted to short term outcome if it does exist at all.
The observed phenomenon of smokers’ paradox is thus a highly controversial one. Many other studies have refuted the existence of this phenomenon (Andrikopoulos et al. 2001; Gottlieb et al. 1996). A study showed that smokers had better early outcome but the benefit rapidly vanishes in the late phase (Takagi et al. 2014) and in the event of post coronary revascularisation (PCI or CABG), smoking is associated with adverse outcome (Zhang et al. 2015; Yi-Hwei et al. 2013).
Collectively, current data suggests that even though smoking may be associated with a favourable early outcome, the overall picture is still not in favour of smoking especially on long term outcome and post coronary revascularisation. This study did not assess the smoking status post myocardial infarction and based on the above evidence from the literature, the favourable outcome of smokers are short-lived and hence we continue to strongly advocate the importance of smoking cessation.
Conclusion
The phenomenon of ‘smoker’s paradox’ is in fact a reality among our patients and is unlikely due to just plain bias from the favourable baseline characteristics of smokers. Even after extensive covariates adjustment for all the favourable baseline characteristics in active smokers, the reduction in mortality risks persists. In conclusion, ‘smoker’s paradox’ in the immediate outcome post myocardial infarction was observed in our patients’ population. Active smokers tend to do better at both in-hospital and 30-days post discharge with significantly lower overall mortality risk compared to those patients who never smoked. The real explanation to this bizarre outcome however, remains unclear.
Nevertheless the study is limitted to only immediate outcome. Smoking status post moyocardial infarction and its effect on long term outcome was not assesed. Currently, the overall evidence from the literature is still in favour of non-smokers especially for long term outcome and post coronary revascularisations.
References
Allahwala UK, Murphy JC, Nelson GI, Bhindi R (2013) Absence of ‘smoker’s paradox’ in field triaged ST-elevation myocardial infarction patients undergoing percutaneous coronary intervention. Cardiovasc Revasc Med 14(4):213–217
Andrikopoulos GK, Richter DJ, Dilaveris PE, Pipilis A, Zaharoulis A, Gialafos JE, Toutouzas PK, Chimonas ET (2001) In-hospital mortality of habitual cigarette smokers after acute myocardial infarction. Eur Heart J 22:776–784
Aune E, Roislien J, Mathisen M, Thelle DS, Otterstad JE (2011) The ‘smoker’s paradox’ in patients with acute coronary syndrome: a systematic review. BMC Med 9:97
Barbash GI, Reiner J, White HD, Wilcox RG, Armstrong PW, Sadowsi Z et al (1995) Evaluation of paradoxic beneficial effects of smoking in patients receiving thrombolytic therapy for acute myocardial infarction: mechanism of the “smoker’s paradox” from the GUSTO-I trial, with angiographic insights. J Am Coll Cardiol 26:1222–1229
Chen Z, Boreham J (2002) Smoking and cardiovascular disease. Semin Vasc Med 2:243–252
Chow CK, Jolly S, Rao-Melacini P, Fox KA, Anand SS, Yusuf S (2010) Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation 121(6):750–758
De Luca G, Parodi G, Sciagra R, Bellandi B, Comito V, Vergara R et al (2014) Smoking and infarct size among STEMI patients undergoing primary angioplasty. Atherosclerosis 233:145–148
Gerber Y, Rosen LJ, Goldbourt U, Benyamini Y, Drory Y, for the Israel Study Group on First Acute Myocardial Infarction (2009) Smoking status and long-term survival after first acute myocardial infarction. J Am Coll Cardiol 54(25):2382–2387
Gottlieb S, Boyko V, Zahger D et al (1996) Smoking and prognosis after acute myocardial infarction in the thrombolytic era. J Am Coll Cardiol 28:1506–1513
Grines CL, Topol EJ, O’Neil WW, George BS, Kereiakes D, Phillips HR et al (1995) Effect of cigarette smoking on outcome after thrombolytic therapy for myocardial infarction. Circulation 91:298–303
Gupta T, Kolte D, Khera S, Aronow WS, Palaniswamy C, Mujib M et al (2014) Relation of smoking status to outcomes after cardiopulmonary resuscitation for in-hospital cardiac arrest. Am J Cardiol 114(2):169–174
Helmers C (1973) Short and long term prognostic indices in acute myocardial infarction. A study of 606 patients initially treated in a coronary care unit. Acta Med Scand Suppl 555:7–26
Kelly TL, Gilpin E, Ahnve S, Henning H, Ross J Jr (1985) Smoking status at the time of acute myocardial infarction and subsequent prognosis. Am Heart J 110:535–541
Kirtane AJ, Martinezclark P, Rahman AM, Ray KK, Karmpaliotis D, Murphy SA et al (2005) Association of smoking with improved myocardial perfusion and the angiographic characterization of myocardial tissue perfusion after fibrinolytic therapy for ST-segment elevation myocardial infarction. J Am Coll Cardiol 45:321–323
Lim HK, Ghazalil SM, Kee CC, Lim KK, Chan YY, Teh HC et al (2013) Epidemiology of smokinfg among Malaysian adult males: prevalence and associated factors. BMC Public Health 13:8
Pamukcu B, Oflaz H, Onur I, Cimen A, Nisanci Y (2011) Effect of cigarette smoking on platelet aggregation. Clin Appl Thromb Hemost 17(6):E175–180
Rasmussen T, Kelbaek H, Masden JK, Thayssen P, Rasmussen K, Thuesen L et al (2012) Smokers with ST-segment elevation myocardial infarction and short-time to treatment have equal effects of PCI and fibrinolysis. J Invasive Cardiol 24:401–406
Robertson JO, Ebrahimi R, Lansky AJ, Mehran R, Stone GW, Lincoff AM (2014) Impact of cigarette smoking on extent of coronary artery disease and prognosis of patients with non-st-segment elevation acute coronary syndromes. An analysis from the ACUITY trial (Acute Catheterization and Urgent Intervention Triage Strategy). J Am Coll Cardiol Intv 7(4):372–379
Sambola A, Osende J, Hathcock J, Degen M, Nemerson Y, Fuster V et al (2003) Role of risk factors in the modulation of tissue factor activity and blood thrombogenicity. Circulation 107:973–977
Sonke GS, Stewart AW, Beaglehole R, Jackson R, White HD (1997) Comparison of case fatality in smokers and non-smokers after acute cardiac event. BMJ 315:992–993
Takagi H, Umemoto T, for the ALICE (All-Literature Investigation of Cardiovascular Evidence) Group (2014) Is alice still in wonderland of the ‘smoker’s paradox’? A meta-analysis of mortality following ACS. Br J Cardiol 21:117
Weisz G, Cox DA, Garcia E, Tcheng JE, Griffin JJ, Guagliumi G et al (2005) Impact of smoking status on outcomes of primary coronary intervention for acute myocardial infarction—the smoker’s paradox revisited. Am Heart J 150:358–364
Yi-Hwei L, Gen-Min L, Cha-Po L, Chin-Lon L, Ji-Hung W (2013) The, “smoker’s paradox” in Asian versus non-Asian patients with percutaneous coronary intervention longer than 6 months follow-ip: a collaborative meta-analysis with ET-CHD registry. Int J Cardiol 168(4):4544–4548
Zahger D, Cercek B, Cannon CP, Jordan M, Davis V, Braunwald E, Shah PK (1995) How do smokers differ from non-smokers in their response to thrombolysis? (the TIMI-4 trial). Am J Cardiol 75:232–236
Zhang YJ, Iqbal J, van Klaveren D, Campos CM, Holmes DR, Kappetein AP et al (2015) Smoking is associated with adverse clinical outcomes in patients undergoing revascularization with PCI or CABG: the SYNTAX trial at 5-year follow-up. J Am Coll Cardiol 65:1107–1115
Zuhdi AS, Mariapun J, Mohd Hairi NN, Wan Ahmad WA, Abidin IZ, Undok AW et al (2013) Young coronary artery disease in patients undergoing percutaneous coronary intervention. Ann Saudi Med 33(6):572–578
Authors’ contributions
PV: manuscript write up, statistical analysis and overall structuring of manuscript; NMS: manuscript write up and statistical analysis; YZ: manuscript write up and statistical analysis; IH: manuscript write up; WAWA: site principal investigator for NCVD-ACD (Malaysia), Scientific review and preparation of manuscript; SKH: principal investigator for NCVD-ACS registry (Malaysia); ASMZ: principal research idea and scientific review of manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank the NCVD Governance Board for permission to use the data for this paper. We would also like to thank all those who have participated in the data collection of NCVD.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Venkatason, P., Salleh, N.M., Zubairi, Y. et al. The bizzare phenomenon of smokers’ paradox in the immediate outcome post acute myocardial infarction: an insight into the Malaysian National Cardiovascular Database-Acute Coronary Syndrome (NCVD-ACS) registry year 2006–2013. SpringerPlus 5, 534 (2016). https://doi.org/10.1186/s40064-016-2188-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2188-3