Abstract
Adenoidectomy, surgical removal of hypertrophic adenoids, is a common operation in children worldwide. The purpose of this study was to compare the operative effectiveness, and included total operative time, blood loss and complications, between endoscopic assisted adenoidectomy and conventional curettage adenoidectomy. EMBASE, PubMed, Cochrane Library, and China National Knowledge Infrastructure and symposiums and review articles were used to choose relevant randomized controlled trials. A meta-analysis was performed to analyze the data for total operative time, blood loss and complications. Seven studies fit the inclusion criteria, and included 331 patients treated with endoscopic assisted adenoidectomy, and 251 patients treated with conventional curettage adenoidectomy. The meta-analysis demonstrated that compared with conventional curettage adenoidectomy, endoscopic assisted adenoidectomy had a shorter operative time (SMD −1.09; 95 % CI −1.29 to −0.90; p < 0.00001), less blood loss (MD −19.74; 95 % CI −22.75 to −16.73; p < 0.00001), and fewer complications (OR 0.15; 95 % CI 0.07–0.35; p < 0.0001). Endoscopic assisted adenoidectomy has advantages over conventional curettage adenoidectomy with regard to total operative time, blood loss and complications.
Similar content being viewed by others
Background
With of approximately 250,000 cases, adenoidectomy remains one of the surgical procedures most frequently performed by otolaryngologist in the United States (Spencer and Jones 2012). The indications for adenoidectomy include children who have recrudescent or chronic otitis media, chronic rhinosinusitis, nasopharyngeal obstruction causing sleep maladjustments and consecutive mouth breathing. The objective of adenoidectomy is to remove an infected or enlarged and obstructive adenoid.
Historically recommended instrumentation for performing adenoidectomy has varied from the surgeon’s fingernail, a steel nail, cutting or biting forceps, adenotomes and adenoid curettes (Jonas et al. 2007). The conventional curettage adenoidectomy was first described in 1885 (Thornval 1969), and since then it has been considered the most commonly used surgical technique for adenoidectomy (Costantini et al. 2008). Conventional curettage for removing adenoids uses the nasopharyngeal touch method to estimate the size of the adenoid and the relationship to the surrounding structure, in order to choose the suitable adenoidectomy curette to scrape the adenoid tissue in the rhinopharynx transorally behind the nose.
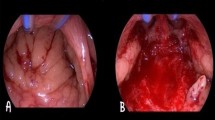
Over time, a considerable number of instruments have been employed to perform adenoidectomy, including an electronic molecular resonance tool, suction diathermy, a microdebrider, endoscopy and laser (Tarantino et al. 2004; Walker 2001; Sorin et al. 2004; Shin and Hartnick 2003; Ozkiris et al. 2013). At present, endoscopic assisted adenoidectomy involves general anesthesia, followed by the application of a microdebrider with irrigating blades of different angles (0°, 15°, 45° and 60°) or special a adenoid blade and a 0° 2.7-mm rigid telescope (4 mm for older children) to shave the adenoid (Somani et al. 2010).
Despite improvements in the surgery, the complications of adenoidectomy are often inevitable. Primary and secondary hemorrhages are the major complication for all patients undergoing adenoidectomy. Minor complication, including fever, soreness, dehydration, refractory emesis, and neck stiffness also are often seen postoperatively. In view of the large number of adenoidectomies performed, the otolaryngologist should pay close attention to the surgical method. The choice of the endoscopic assisted adenoidectomy versus conventional curettage adenoidectomy has been widely debated.
Conventional curettage adenoidectomy can be performed in any hospital, especially in those that do not possess advanced instruments. Moreover, the cost of conventional curettage adenoidectomy is very low, so the majority of patients can afford it, particularly poor families in developing countries. However the conventional curettage adenoidectomy for removing adenoids is a relatively ‘blind’ technique which risks nasopharyngeal injury and incomplete adenoid removal (Regmi et al. 2011). By measuring the volume of residual adenoid tissues, both Saxby and Chappel (2009) and Cannon et al. (1999) objectively proved that conventional curettage adenoidectomy misses a substantial amount of adenoid tissue. A prospective study involving endoscopic evaluation of cases operated by curette and microdebrider showed that conventional curettage adenoidectomy was less precise than endoscopic assisted adenoidectomy, especially in the choanal and tubaric regions (Owens et al. 2005). Compared with conventional curettage adenoidectomy, Havas and Lowinger (2002) also demonstrated that endoscopic assisted adenoidectomy had was superior to conventional curettage adenoidectomy for complete removal of adenoids in a shorter operative time. However, one study by Elnashar et al. (2014) stated that there was no difference in effectiveness between the two methods when under grade 3 adenoid enlargement on X-ray. However, Songu et al. (2010) stated that conventional adenoidectomy was better than endoscopic assisted adenoidectomy with regard to blood loss and complications.
Although many studies have compared endoscopic assisted adenoidectomy and conventional curettage adenoidectomy, there is as yet no agreement on which technique is superior. Therefore, we conducted a meta-analysis in an attempt to resolve this issue.
Methods
This study was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews) for statement (Moher et al. 2010).
Literature search
EMBASE, PubMed, Cochrane Library (CL), and China National Knowledge Infrastructure databases, and symposiums and review articles were used to identify relevant randomized controlled trials from the day they initiated until October 2014, with no limit for language types. Search keywords were as follows: “adenoidectomy”, “endoscopic assisted adenoidectomy” “conventional curettage adenoidectomy”, “classical adenoid curette”, “power assisted adenoidectomy”, “adenoid hypertrophy surgery”, “cohort study”, “prospective study”, and “randomized control trial”. If there are no original data, we contacted authors directly to obtain it. If we can not get the original data from the authors, and the study is so important for the analysis, we can use a formula to calculate according to the available data (Hozo et al. 2005).
Study selection
All studies compared endoscopic assisted adenoidectomy and conventional curettage adenoidectomy. Suitable studies are selected according to the following criteria (1) the study is reported at least one of the following outcomes: total operative time, blood loss or complications; (2)the study is obtained available data; (3) the study is irrespective of age, sex, weight and height. Reasons for study exclusion included the following (1) patients had systemic diseases; (2) the study is only reported as an abstract or with incorrect data; (3) the study is used a sample size <10; (4) the standard used to assess curative effect is not stated.
Data extraction
Two researchers (L.Y. and Y.M.) independently selected the eligible studies, and then a table was designed to extract their characteristics. If there was any disagreement between the two researchers, we sent it to a third reviewer (Z.H.) to resolve. The salient characteristics included the first author’s name, the year published, basic demographics of participants, study method and outcomes (Table 1).
Outcome measures
In this study the main outcome measures were total operative time, blood loss and complications.
Quality assessment
Because most of the relevant studies were randomized controlled trials, we chose the Jadad score for evaluation literature quality, which included randomization method, length of follow-up, and number of samples. A cumulative Jadad score ≥3 indicated high quality (Moher et al. 2000).
Statistical analysis
The data extracted were pooled to obtain estimates of overall surgery effects using Review Manager for Windows version 5.3. The mean difference (MD) or standard mean difference (SMD) with its 95 % confidence interval (CI) was used and for dichotomous data, odds risk (OR) with a 95 % CI was applied. A value of p ≤ 0.05 indicated statistical significance. The statistical heterogeneity was assessed in our study using Cochrane’s Q test and I2 statistics. Clinical heterogeneity was evaluated by study interventions and the definition of outcome measures. A fixed-effects model also could be used when the heterogeneity was (p > 0.1 or p ≤ 0.1, but was I2 ≤ 50 %) and the significant heterogeneity (p ≤ 0.1, I2 ≥ 50 %), as described in detail by Wang et al. (2014).
Results
Search results and study characteristics
With the key words, we found 2111 titles, of which 245 titles and abstracts were identified. Of these 245, 102 titles for which full texts were available were studied in detail. Unfortunately, most were retrospective non-randomized studies, case reports, or irrelevant review articles. The procedure for study selection is shown in Fig. 1. Ultimately, seven randomized controlled trials published from 2000 to 2013 matched the inclusion criteria (Songu et al. 2010; Al-Mazrou et al. 2009; Ozturk and Polat 2012; Stanislaw et al. 2000; Murray et al. 2002; Feng and Ying 2006; Zhang and Yang 2013). Five studies were published in English (Songu et al. 2010; Al-Mazrou et al. 2009; Ozturk and Polat 2012; Stanislaw et al. 2000; Murray et al. 2002) and two were published in Chinese (Feng and Ying 2006; Zhang and Yang 2013). A total of 582 patients in the studies underwent adenoidectomy, including 331 patients treated with endoscopic assisted adenoidectomy, and 251 patients with conventional curettage adenoidectomy. (For characteristics of adaptive trials refer to Table 1.)
Quality assessment
The study design, conduct and analysis were examined to assess quality. Both Songu et al. (2010) and Al-Mazrou et al. (2009) divided the children into groups using a computer-generated random numbers table and another study randomized subjects to treatment groups based on an odd or even medical number (Stanislaw et al. 2000). The remaining four studies did not clearly state the method used to randomize subjects to treatment groups. Only one study reported allocation to treatment with blinding using a worksheet (Ozturk and Polat 2012). A double-blind method was reported in three studies (Elnashar et al. 2014; Al-Mazrou et al. 2009; Feng and Ying 2006), and a single-blind method was mentioned in another study (Zhang and Yang 2013). The other three studies did not report blinding, so this was considered an undefined risk. The risks of bias for each of the seven studies are shown in Fig. 2.
Outcomes and synthesis of results
Total operative time
Total operative time was reported in six studies. According to Fig. 3, in the meta-analysis showed that it was shorter in the endoscopic assisted adenoidectomy group than in the conventional curettage adenoidectomy group (SMD −1.09; 95 % CI −1.29 to −0.90; p < 0.00001) with statistical heterogeneity; (χ2 = 133.34, I2 = 96 %; p < 0.00001).
Blood loss
As shown in Fig. 4, blood loss was compared in five studies the results of which showed that it was less in the endoscopic assisted adenoidectomy group than in the conventional curettage adenoidectomy group (MD −19.74; 95 % CI −22.75 to −16.73; p < 0.00001), with statistical heterogeneity (χ2 = 89.37, I2 = 96 %; p < 0.00001).
Complications
According to Fig. 5, complications were reported in three of seven studies. The data showed that there were fewer complications in the endoscopic assisted adenoidectomy group than the conventional curettage adenoidectomy group (OR 0.15; 95 % CI 0.07–0.35, p < 0.0001), with statistical heterogeneity: (χ2 = 4.97, I2 = 40 %; p = 0.17).
Discussion
Growing adenoid tissue is inclined to narrow the upper airway lumen to varying degrees (Papaioannou et al. 2013). Large adenoids and tonsils are diagnosed in children with mouth breathing, snoring, and sleep-disordered breathing (Niemi et al. 2015). The best way to solve the problem is adenoidectomy (Friedman et al. 2009) which must alleviate chronic nasal obstruction, mouth breathing, rhinosinusitis and eustachian tube dysfunction (Anand et al. 2014). In the clinic, the operative approaches include conventional curettage adenoidectomy and endoscopic assisted adenoidectomy. Here we report the first comprehensive meta-analysis comparing endoscopic assisted adenoidectomy and conventional curettage adenoidectomy in order to determine which method has greater benefits for children.
This meta-analysis included seven studies that all met the inclusion criteria (Songu et al. 2010; Al-Mazrou et al. 2009; Ozturk and Polat 2012; Stanislaw et al. 2000; Murray et al. 2002; Feng and Ying 2006; Zhang and Yang 2013). Five studies stated the total operative time, and the result of meta-analysis showed that endoscopic assisted adenoidectomy was better than conventional curettage adenoidectomy in this regard. The related shorter operative time could be explained by the endoscopic adenoidectomy is an operation to remove pathological tissues which clearly block the choana, and the shaver can reach them directly by using 0°, 30° endoscopy (Somani et al. 2010). Although the actual procedure time is not concerned, the total operative time the children spent is possible more important. This is specifically important in children with upper airway obstruction where the time taken to induce adequate anaesthesia and the time taken for the patient to emerge from anaesthesia was often long and unpredictable (Songu et al. 2010).
Five studies selected reported blood loss, and the meta-analysis results demonstrated that the conventional curettage adenoidectomy caused greater blood loss than endoscopic assisted adenoidectomy. This is mainly related to direct visualization, treatment of the source of bleeding, the effect of a microdebrider depended on suction efficacy and hemostasis is noticeably shortened (Vokurka 2003). This reduction of blood loss is highly suitable for children because it reduces the risk of hemorrhage (Al-Mazrou et al. 2009).
Four studies reported complications associated with endoscopic assisted adenoidectomy and conventional curettage adenoidectomy. Our meta-analysis showed that the former was superior to the latter. Concerning the intraoperative view the conventional technique gives worse visualization of the operative field which is liable to miss tissues, leading to relapse with inflammation (Regmi et al. 2011). In the clinic, conventional technique increases the risk of damaging the eustachain tube openings in the region of the rhinopharynx (Viorel 2011) and leads to mild hearing loss (Capaccio et al. 2016). Furthermore, the adenoids may only be reduced, not completely removed. If the adenoids are not completely removed, they may continue to be re-grow and cause airway obstruction (Al-Mazrou et al. 2009). By contrast, endoscopic assisted adenoidectomy removes the tissues cleanly and solves the nasopharyngeal obstruction completely.
The results of our meta-analysis suggest that the endoscopic assisted adenoidectomy is better than conventional curettage adenoidectomy in terns of total operative time, blood loss, and complications.
Our meta-analysis focused on objective outcome measurements to define surgical effectiveness. Nevertheless, dependence on subjective measurements may overestimate effectiveness. A few limitations of this meta-analysis should be considered. First, there only seven studies were included; limitations of meta-analysis based on the number of eligible studies are well known, including confounding factors and selection bias, so the results must be viewed with caution. Second, there were some differences among studies in the basic definition of effectiveness. Therefore, effectiveness differs among the studies presented, contributing to heterogeneity.
Conclusion
According to our meta-analysis, endoscopic assisted adenoidectomy has advantages over conventional curettage adenoidectomy with regard to total operative time, blood loss and complications. This result finding may be useful to otolaryngologists when choosing surgery for adenoid hypertrophy. However, current evidence is incomplete, and we hope that more high quality clinical studies will be published to enhance meta-analysis outcomes and provide a better guide for surgeons.
References
Al-Mazrou KA, Al-Qahtani A, Al-Fayez AI (2009) Effectiveness of transnasal endoscopic powered adenoidectomy in patients with choanal adenoids. Int J Pediatr Otorhinolaryngol 73(12):1650–1652
Anand V, Sarin V, Singh B (2014) Changing trends in adenoidectomy. Indian J Otolaryngol Head Neck Surg 66(4):375–380
Cannon CR, Replogle WH, Schenk MP (1999) Endoscopic-assisted adenoidectomy. Otolaryngol Head Neck Surg 121(6):740–744
Capaccio P, Torretta S, Marciante GA (2016) Endoscopic adenoidectomy in children with otitis media with effusion and mild hearing loss. Clin Exp Otorhinolaryngol 9:33
Costantini F, Salamanca F, Amaina T (2008) Videoendoscopic adenoidectomy with microdebrider. Acta Otorhinolaryngol Ital 28(1):26–29
Elnashar I, El-Anwar MW, Basha WM (2014) Objective assessment of endoscopy assisted adenoidectomy. Int J Pediatr Otorhinolaryngol 78(8):1239–1242
Feng YH, Ying SK (2006) Comparison on the effectiveness between endoscopic assisted adenoidectomy and conventional curettage adenoidectomy. J Clin Otorhinolaryngol 20(3):54–57 (in Chinese)
Friedman M, Wilson M, Lin HC (2009) Updated systematic review of tonsillectomy and adenoidectomy for treatment of pediatric obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg 140(6):800–808
Havas T, Lowinger D (2002) Obstructive adenoid tissue: an indication for powered-shaver adenoidectomy. Arch Otolaryngol Head Neck Surg 128(7):789–791
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 8:5–13
Jonas NE, Sayed R, Prescott CA (2007) Prospective, randomized, single-blind, controlled study to compare two methods of performing adenoidectomy. Int J Pediatr Otorhinolaryngol 71(10):1555–1562
Moher D, Cook DJ, Eastwood S, QUOROM Group et al (2000) Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Br J Surg 87(11):1448–1454
Moher D, Liberati A, Tetzlaff J (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341
Murray N, Fitzpatrick P, Guarisco JL (2002) Powered partial adenoidectomy. Arch Otolaryngol Head Neck Surg 128(7):792–796
Niemi P, Numminen J, Rautiainen M et al (2015) The effect of adenoidectomy on occlusal development and nasal cavity volume in children with recurrent middle ear infection. Int J Pediatr Otorhinolaryngol 12(3):142–148
Owens D, Jaramillo M, Saunders M (2005) Suction diathermy adenoid ablation. J Laryngol Otol 119(1):34–35
Ozkiris M, Karacavus S, Kapusuz Z (2013) Comparison of two different adenoidectomy techniques with special emphasize on postoperative nasal mucociliary clearance rates: coblation technique vs. cold curettage. Int J Pediatr Otorhinolaryngol 77(3):389–393
Ozturk O, Polat S (2012) Comparison of transoral power-assisted endoscopic adenoidectomy to curettage adenoidectomy. Adv Ther 29(8):708–721
Papaioannou G, Kambas I, Tsaoussoglou M et al (2013) Age-dependent changes in the size of adenotonsillar tissue in childhood: implications for sleep-disordered breathing. J Pediatr 162(2):269–274
Regmi D, Mathur NN, Bhattarai M (2011) Rigid endoscopic evaluation of conventional curettage adenoidectomy. J Laryngol Otol 125(1):53–58
Saxby AJ, Chappel CA (2009) Residual adenoid tissue post-curettage: role of nasopharyngoscopy in adenoidectomy. ANZ J Surg 79(11):809–811
Shin JJ, Hartnick CJ (2003) Pediatric endoscopic transnasal adenoid ablation. Ann Otol Rhinol Laryngol 112(6):511–514
Somani SS, Naik CS, Bangad SV (2010) Endoscopic adenoidectomy with microdebrider. Indian J Otolaryngol Head Neck Surg 62(4):427–431
Songu M, Altay C, Adibelli ZH (2010) Endoscopic-assisted versus curettage adenoidectomy: a prospective, randomized, double-blind study with objective outcome measures. Laryngoscope 120(9):1895–1899
Sorin A, Bent JP, April MM (2004) Complications of microdebrider-assisted powered intracapsular tonsillectomy and adenoidectomy. Laryngoscope 114(2):297–300
Spencer DJ, Jones JE (2012) Complications of adenotonsillectomy in patients younger than 3 years. Arch Otolaryngol Head Neck Surg 138(4):335–339
Stanislaw P Jr, Koltai PJ, Feustel PJ (2000) Comparison of power-assisted adenoidectomy vs adenoid curette adenoidectomy. Arch Otolaryngol Head Neck Surg 126(7):845–849
Tarantino V, D’Agostino R, Melagrana A et al (2004) Safety of electronic molecular resonance adenoidectomy. Int J Pediatr Otorhinolaryngol 68(12):1519–1523
Thornval A (1969) Wilhelm Meyer and the adenoids. Arch Otolaryngol 90(3):383–386
Viorel Z (2011) Conventional curettage adenoidectomy versus endoscopic assisted adenoidectomy. J Clin Med 6(4):328–329
Vokurka J (2003) Shaver (micro debridor) in otorhinolaryngology. Int Congr Ser 1240:1411–1415
Walker P (2001) Pediatric adenoidectomy under vision using suction-diathermy ablation. Laryngoscope 111(12):2173–2177
Wang J, Cai C, Wang S (2014) Merocel versus Nasopore for nasal packing: a meta-analysis of randomized controlled trials. PLoS One 9(4):93–95
Zhang YG, Yang XY (2013) Comparison of endoscopic assisted adenoidectomy versus conventional curettage. J Chin Mod Dr 51(31):25–29 (in Chinese)
Authors’ contributions
CC confirmed the theme of the manuscript, LY and YS selected the studies, HZ checked them, LY and HZ written the manuscript and YS and SW revised it. All authors read and approved the final manuscript.
Acknowledgements
This work is supported by grants from the Science and Technology Commission of Shanghai Municipality (No. 12ZR1418700).
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Yang, L., Shan, Y., Wang, S. et al. Endoscopic assisted adenoidectomy versus conventional curettage adenoidectomy: a meta-analysis of randomized controlled trials. SpringerPlus 5, 426 (2016). https://doi.org/10.1186/s40064-016-2072-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2072-1