Abstract
Introduction
Ameloblastoma is a benign odontogenic neoplasm of the jaw, rarely presenting as a malignant tumor. Although it is very important to discriminate ameloblastoma from ameloblastic carcinoma in order to decide the appropriate operative procedure, this is difficult using conventional CT and MRI.
Case descriptions
We report a case of maxillar ameloblastoma in a 78-year-old man where FDG-PET/CT was useful for making this discrimination. CT demonstrated a 31 × 43 × 46-mm mass in the left posterior maxillary sinus with destruction of its posterior and lateral wall and alveolar bone. MRI demonstrated a hypo- to isointense heterogeneous pattern on T1WI, heterogeneous hyperintensity with a prominent high-signal spot on T2WI, high signal intensity on DWI reflecting restricted diffusion, and strong heterogeneous enhancement. Because FDG-PET/CT showed mild FDG uptake (SUVmax 2.40) by the mass, ameloblastoma, rather than ameloblastic carcinoma, was considered to be the correct diagnosis.
Discussion and evaluation
It appears that ameloblastic carcinoma shows intense FDG uptake, whereas ameloblastoma shows mild or moderate FDG uptake, and only rarely intense FDG uptake. Our experience suggests that FDG-PET/CT may be effective for discriminating ameloblastoma from ameloblastic carcinoma. Especially, in cases showing mild FDG uptake, benign ameloblastoma would seem the most likely diagnosis.
Conclusions
FDG-PET/CT may be useful as an adjunctive modality for diagnosis, treatment planning and surveillance of ameloblastoma and ameloblastic carcinoma.
Similar content being viewed by others
Background
Ameloblastoma is a benign odontogenic neoplasm derived from ameloblastic epithelial tissue. It comprises only 1% of all jaw tumors and 11% of all odontogenic neoplasms (being the second most common) (Neville et al. 2002). The 2005 WHO histological classification of odontogenic tumors classified ameloblastoma into several types: solid/multicystic, extraosseous/peripheral, desmoplastic, and unicystic (Gardner et al. 2005). Although ameloblastoma is a benign neoplasm, it is locally aggressive and local recurrence is not rare (Inoue et al. 1988). Ameloblastic carcinoma is a term given to tumors that display histologically malignant features at both primary and metastatic sites with a pattern otherwise resembling ameloblastoma (Newman et al. 1995). To plan the most appropriate treatment, it is very important to determine whether a tumor is benign or malignant. However, discrimination between ameloblastoma and ameloblastic carcinoma is difficult by conventional morphological imaging modalities such as radiography, computed tomography (CT) and magnetic resonance imaging (MRI) (Devenney-Cakir et al. 2010, Dunfee et al. 2006, Matsuzaki et al. 2011, Minami et al. 1992).
Recently, assessment of glucose metabolism in cells using 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET) has been used to identify aggressive tumors and to predict their degree of malignant potential. Here we describe a case of ameloblastoma with emphasis on the imaging features revealed by FDG-PET/CT.
Case presentation
A 78-year-old male patient presented at the otolaryngology-head and neck surgery department of our hospital complaining of nasal bleeding. He had no pain, swelling or discharge. The patient gave consent to publish this case report and any accompanying images.
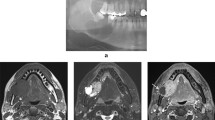
Non-contrast CT revealed a 31 × 43 × 46-mm mass in the left maxillary sinus and masticatory space, with posterior bone resorption and destruction of the maxillary sinus (Fig. 1a). The solid mass also showed partial resorption of the alveolar bone and elevation of the posterior maxillary sinus floor with destruction of the floor and lateral side wall (Fig. 1b). MRI was performed using a 1.5-T unit. MRI demonstrated hypo- to isointensity with a heterogeneous pattern on T1-weighted spin-echo images (repetition time/echo time (TR/TE) = 727/12 ms), heterogeneous hyperintensity with a prominent high-signal spot on T2-weighted fast spin-echo images (TR/TE = 4452/100 ms) (Fig. 2a), and high signal intensity on diffusion-weighted imaging (DWI) (b value = 0 and 1000 s/mm2), reflecting restricted diffusion. T1-weighted spin-echo images (TR/TE = 554/10 ms) enhanced with gadolinium-diethylene-triamine-pentaacetic acid (Gd-DTPA) (Magnevist: Bayer Schering Pharma, Osaka, Japan) showed strong and heterogeneous enhancement of the tumor (Fig. 2b). These findings of marginal bone destruction by the lesion on CT and MRI and abnormal signal intensity on DWI suggested a malignant tumor, and we first suspected ameloblastic carcinoma. The differential diagnosis included malignant peripheral nerve sheath tumor, rhabdomyosarcoma, pleomorphic adenocarcinoma or adenoid cystic carcinoma arising from the masticatory space. For initial staging, FDG-PET/CT was performed to investigate the presence of regional lymph nodes and distant metastasis. The mass showed mild FDG uptake with a maximum standardized uptake value (SUVmax) of 2.40 (Figs. 3a,b). On this basis, we considered the lesion to be a benign odontogenic tumor, probably ameloblastoma.
CT imaging findings. a Axial non-contrast CT image shows a 31 × 43 × 46-mm mass in the left maxillary sinus and masticatory space with resorption and destruction of the maxillary sinus posterior bone. b Coronal CT (bone-window) images show diffuse and partial resorption of the alveolar bone and elevation of the posterior maxillary sinus floor with destruction of the floor and lateral side wall
We performed biopsy under general anesthesia and pathological examination of the sample confirmed ameloblastoma. Later the patient underwent partial mandibulectomy. Gross pathological review revealed a shiny white solid mass (Fig. 4a). Histopathological examination revealed dense proliferation of follicular structures made up of tumor cells resembling odontogenic epithelium. Tall columnar cells resembling ameloblastoma cells formed arrays surrounding peripheral follicles, which contained a stellate reticulum-like component in the central area (Fig. 4b). The pathological diagnosis was ameloblastoma.
Histopathological findings. a Gross pathological view demonstrates a shiny white solid mass. b Microscopic view with hematoxylin and eosin staining reveals dense proliferation of follicular structures made up of tumor cells resembling odontogenic epithelium. Tall columnar cells resembling ameloblastoma cells surround peripheral follicles, which contain stellate reticulum-like central areas
At 2 years after surgery, there was no sign of tumor recurrence.
Discussion
Ameloblastoma is a benign, locally aggressive and infiltrative odontogenic neoplasm with a high rate of recurrence. Ameloblastic carcinoma tends to be aggressive and has a potential for lymph node and distant metastasis. Therefore diagnostic imaging for initial staging before treatment is very important. Resection of mandibular masses is an extensive and potentially disfiguring type of surgery; therefore preoperative understanding of the extent and malignant potential of a tumor in this area is essential for achieving a curative and cosmetically acceptable result. However, the two neoplasms are morphologically similar (Devenney-Cakir et al. 2010, Dunfee et al. 2006, Matsuzaki et al. 2011, Minami et al. 1992), and therefore an additional imaging modality to achieve adequate discrimination is desirable.
Ameloblastoma and ameloblastic carcinoma most commonly occur in the posterior mandible, typically in the region of the third molar, with associated follicular cysts or impacted teeth. The slow growth of the tumor can lead to significant expansion of the mandible. Radiographically, both lesions can appear radiolucent, being either unilocular or multilocular, exhibiting a honeycomb-like appearance with tooth root resorption. Both lesions often have distinct borders, slight marginal sclerosis without periosteal new bone formation, loss of the lamina dura, resorption of the tooth apex and tooth displacement (Devenney-Cakir et al. 2010, Dunfee et al. 2006). CT findings include cystic areas of low attenuation with scattered isoattenuating regions, representating soft tissue components. The lesion can also erode through the cortex with extension into the surrounding oral mucosa (Dunfee et al. 2006). In addition, erosion of the roots of adjacent teeth is unique to ameloblastoma and indicates the aggressive behavior of the tumor. MRI demonstrates several common findings: multilocularity, mixed solid and cystic components, irregularly thick walls, papillary projections, and marked enhancement of the walls and septa (Dunfee et al. 2006, Minami et al. 1992). MRI is superior to conventional radiography and CT in demonstrating components of the tumor, extension within the bone marrow and involvement of adjacent extraosseous structures, which is important when considering surgical resection or reconstruction planning (Devenney-Cakir et al. 2010, Dunfee et al. 2006, Matsuzaki et al. 2011, Minami et al. 1992). Ameloblastic carcinoma generally exhibits more aggressive features such as dystrophic calcifications, cortical destruction, extraosseous extension and an extensive solid component.
Few reports have described the FDG-PET/CT features of ameloblastoma and ameloblastic carcinoma (Devenney-Cakir et al. 2010, Matsuzaki et al. 2011, Nguyen 2005, Otsuru et al 2008). Matsuzaki et al. reported one case of ameloblastic carcinoma of the maxilla demonstrating intense FDG uptake with a SUVmax of 28.3 (Matsuzaki et al. 2011). Otsuru et al. reported four cases of ameloblstoma (three arising from the maxilla and one from the mandible) showing mild to moderate FDG uptake, which was correlated with glucose transporter-1 (GLUT-1) expression (Otsuru et al 2008). Two groups have demonstrated that FDG-PET/CT was also useful for detection of metastases from ameloblastic carcinoma (Devenney-Cakir et al. 2010, Nguyen 2005). From these previous reports and the present case, it appears that ameloblastic carcinoma shows intense FDG uptake, whereas ameloblastoma shows mild or moderate FDG uptake, and rarely intense FDG uptake, however further analysis in a larger patient population is necessary to confirm this speculation. Low uptake in this case may be due to weak aggressiveness and invasiveness of this tumor. Our experience suggests that FDG-PET/CT may be effective for discriminating ameloblastoma from ameloblastic carcinoma. Especially, in cases showing mild FDG uptake, benign ameloblastoma would seem the most likely diagnosis. Moreover, as FDG-PET is useful for predicting the degree of malignant potential and for identifying ameloblastoma as a locally invasive tumor, prediction and early diagnosis of recurrent ameloblastoma, and personalized treatment in individual cases, may be possible (Otsuru et al 2008).
Conclusions
We have reported the CT, MRI and FDG-PET/CT findings in a case of maxillar amelobastoma in a 78-year-old male patient. In this case, it was difficult to distinguish between amelobastoma and ameloblastic carcinoma by conventional CT and MRI. Mild FDG uptake on PET/CT was useful for diagnosis of amelobastoma. FDG-PET/CT may be useful as an adjunctive modality for diagnosis, treatment planning and surveillance of ameloblastoma and ameloblastic carcinoma.
References
Devenney-Cakir B, Dunfee B, Subramaniam R, Sundararajan D, Mehra P, Spiegel J, Sakai O (2010) Ameloblastic carcinoma of the mandible with metastasis to the skull and lung: advanced imaging appearance including computed tomography, magnetic resonance imaging and positron emission tomography computed tomography. Dentomaxillofac Radiol 39:449–453
Dunfee BL, Sakai O, Pistey R, Gohel A (2006) Radiologic and pathologic characteristics of benign and malignant lesions of the mandible. Radiographics 26:1751–1768
Gardner DG, Heikinheimo K, Shear M, Philpsen HP, Coleman H (2005) Pathology and Genetics.Head and Neck Tumours. In: Barnes L, Eveson JW, Reichart P, Sidransky D (eds) Ameloblastomas,” in World Health Organization Classification of Tumors. IARC Press, Lyon, France
Inoue N, Shimojyo M, Iwai H, Ohtsuki H, Yasumizu R, Shintaku M, Taniguchi N, Inada M, Arika T, Morita S et al (1988) Malignant ameloblastoma with pulmonary metastasis and hypercalcemia. Report of an autopsy case and review of the literature. Am J Clin Pathol 90:474–481
Matsuzaki H, Katase N, Hara M, Asaumi J, Yanagi Y, Unetsubo T, Hisatomi M, Konouchi H, Nagatsuka H (2011) Ameloblastic carcinoma: a case report with radiological features of computed tomography and magnetic resonance imaging and positron emission tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:e40–e47
Minami M, Kaneda T, Yamamoto H, Ozawa K, Itai Y, Ozawa M, Yoshikawa K, Sasaki Y (1992) Ameloblastoma in the maxillomandibular region: MR imaging. Radiology 184:389–393
Neville BW, Damm DM, Allen CM, Bouquot JE (2002) Oral and Maxillofacial Pathology 2nd edn. W.B. Saunders, Philadelphia, PA, pp 611–619
Newman L, Howells GL, Coghlan KM, DiBiase A, Williams DM (1995) Malignant ameloblastoma revisited. Br J Oral Maxillofac Surg 33:47–50
Nguyen BD (2005) Malignant ameloblastoma with thoracic vertebral metastasis: PET/CT and MR imaging. Clin Nucl Med 30:450–452
Otsuru M, Aoki T, Tsukinoki K, Ota Y, Karakida K, Yamazaki H, Yasuda M, Kaneko A (2008) Usefulness of 18F-fluorodeoxyglucose positron emission tomography for detecting ameloblastoma, with special reference to glucose transporter-1 expression. J Oral Maxillofac Surg 66:1761–1765
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SS designed this study and collected the data. SS and KK wrote the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seno, S., Kitajima, K., Inokuchi, G. et al. FDG-PET findings of Ameloblastoma: a case report. SpringerPlus 4, 250 (2015). https://doi.org/10.1186/s40064-015-0998-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-015-0998-3