Abstract
Background
Antimicrobial stewardship (AMS) strategies worldwide focus on optimising the use of antibiotics. Selective susceptibility reporting is recommended as an effective AMS tool although there is a lack of representative studies investigating the impact of selective susceptibility reporting on antibiotic use. The aim of this study was to investigate the impact of selective susceptibility reporting of Staphylococcus aureus (S. aureus) on antibiotic consumption. Enhancing the use of narrow-spectrum beta-lactam antibiotics such as flucloxacillin/cefazolin/cefalexin is one of the main goals in optimising antibiotic therapy of S. aureus infections.
Methods
This interventional study with control group was conducted at a tertiary care hospital in Germany. During the one-year interventional period susceptibility reports for all methicillin-sensitive S. aureus (MSSA) were restricted to flucloxacillin/cefazolin/cefalexin, trimethoprim-sulfamethoxazole, clindamycin, gentamicin and rifampin/fosfomycin, instead of reporting all tested antibiotics. The impact of implementing selective reporting was analysed by monitoring total monthly antibiotic consumption in our hospital and in a reference hospital (recommended daily dose/100 occupied bed days: RDD/100 BD), as well as on an individual patient level by analysing days of therapy adjusted for bed days (DOT/ 100 BD) for patients with S. aureus bacteremia (SAB) and respectively skin and soft tissue infections (SSTI).
Results
MSSA-antibiograms were acquired for 2836 patients. The total use of narrow-spectrum beta-lactams more than doubled after implementing selective reporting (from 1.2 to 2.8 RDD/100 BD, P < 0.001). The use of intravenous flucloxacillin/cefazolin for SAB rose significantly from 52 to 75 DOT/100 BD (plus 42%), just as the use of oral cefalexin for SSTI (from 1.4 to 9.4 DOT/100 BD, from 3 to 17 of 85/88 patients). Considering the overall consumption, there was no decrease in antibiotics omitted from the antibiogram. This was probably due to their wide use for other infections.
Conclusions
As narrow-spectrum beta-lactams are not widely used for other infections, their increase in the overall consumption of the entire hospital was a strong indicator that selective reporting guided clinicians to an optimised antibiotic therapy of S. aureus infections. On a patient level, this assumption was verified by a significant improved treatment of S. aureus infections in the subgroups of SAB and SSTI. As useful AMS tool, we recommend implementing selective reporting rules into the national/international standards for susceptibility reporting.
Similar content being viewed by others
Background
Significant efforts have been made to implement antimicrobial stewardship (AMS) worldwide to improve antibiotic prescribing to prevent multidrug resistance and improve patient care. There are a number of policies, strategies and tools outlined in different guidelines [1,2,3] and systematic reviews [4,5,6,7,8,9] to achieve this goal. Nevertheless, the impact of each tool is unclear.
One of the recommended tools is selective reporting of antibiotics in accordance with treatment guidelines to optimize antibiotic prescribing [1,2,3, 10,11,12]. Although this is one of the tools required there is a lack of representative studies investigating the impact of selective susceptibility reporting on antibiotic use.
S. aureus with its large number of pathogenicity factors causes severe infections that should be treated by optimal antibiotic therapy. Narrow-spectrum beta-lactam antibiotics such as flucloxacillin or cefazolin/cephalexin have better activity against S. aureus than broad-spectrum beta-lactams such as piperacillin-tazobactam, ceftriaxone or even cefuroxime [13,14,15]. In addition, third-generation cephalosporins or fluoroquinolones are associated with a number of side effects including Clostridioides difficile infections and the risk of selecting multi-resistant bacteria e.g. extended spectrum beta-lactamase-strains (ESBL) or methicillin-resistant S. aureus (MRSA). Therefore, enhancing the use of narrow-spectrum beta-lactams is one of the main goals of AMS in S. aureus infections to optimize antibiotic therapy of the individual patient and to prevent the spread of multi-resistant bacteria.
The aim of this study was to investigate the effect of switching from non-selective reporting of all tested antibiotics to selective reporting of recommended antibiotics in case of culturing S.aureus. Changes in other AMS tools were minimised during that period in order to focus on the impact of antibiotic reporting.
Methods
This interventional study was conducted at the Helios Clinics of Schwerin, a tertiary care hospital in Germany with more than 1200 beds. Helios Clinic Duisburg, a tertiary care hospital of comparable size and structure (more than 1000 beds), served as a reference without intervention. The study was approved by the Ethics Committee of the Faculty of Medicine at the University of Rostock (A 2017-0149).
Intervention
From November 01, 2017–October 31, 2018, reports on susceptibility testing (antibiogram) of all tested methicillin-sensitive S. aureus (MSSA) were modified in the following way: Only recommended therapeutically appropriate antibiotics for S. aureus infections were reported (narrow-spectrum beta-lactams: intravenous flucloxacillin/cefazolin/oral cefalexin, trimethoprim-sulfamethoxazole (TMP-SMX), clindamycin, gentamicin, rifampin/fosfomycin for combination therapy); whereas all others, especially broad-spectrum antibiotics (e.g. piperacillin-tazobactam, ceftriaxone, imipenem, meropenem, vancomycin) were excluded. The laboratory operation system (OPUS: L by OSM GmbH, Essen, Germany) was programmed to automatically omit these antimicrobials without operator intervention, in order to minimise effort and errors of the laboratory staff. The test results were still available on request. Before the intervention, all tested antibiotics were reported on the antibiogram, predetermined by industrial panels (Table 1). Additionally, the standard advice for the therapy of S. aureus infections was given in every susceptibility testing report to guide the clinician’s selection of the most appropriate antibiotic depending on the severity of the disease: "First choice for severe S. aureus infections/bacteremia: high dose intravenous flucloxacillin/cefazolin (ceftriaxone/cefotaxime/vancomycin are less effective in the treatment of MSSA); mild infection/oral follow-up: cefalexin, trimethoprim-sulfamethoxazole or clindamycin depending on the indication, side effects and allergies".
The prescribing clinicians were not informed of the ongoing study.
We did not change the reporting of susceptibility testing in methicillin-resistant S. aureus (MRSA).
Measurement of the effect of implementing selective reporting and statistical analysis
Overall antibiotic consumption of the entire hospital
To measure the effect of the intervention we monitored the recommended daily dose/100 occupied bed days (RDD/100 BD) as a standardised method for measurement of antibiotic usage. To calculate RDD/100 BD, the total monthly use of every antibiotic in the entire hospital was devided by the occupied bed days and the assumed normal daily dose (Table 2: RDD for all involved antibiotics). Antibiotic consumption was compared to Helios Clinic Duisburg as a reference hospital of comparable size, where all tested antibiotics were furthermore reported on the antibiogram (antibiotic consumption data of all Helios Clinics in Germany are available on “iNAB": intranet-based statistics of antibiotic consumption). The RDD was representative of the actual dose of different antibiotics administered in both hospitals (besides dose adjustments to kidney or liver dysfunction). There were no temporary shortages of any involved antibiotics. The number of patients in whom S. aureus was detected was recorded monthly in order to have a baseline of infections for the intervention. For overall consumption of the entire hospital, the monthly use (RDD/100 BD) of each antibiotic was analysed by linear regression using an interrupted time-series approach with group comparisons (Table 3). In this analysis the outcome variable was analysed in dependence of the time (month) since start of study, a dummy variable for the intervention, a dummy variable for the clinic (interventional or reference clinic) and all interactions terms between these variables [16]. Simultaneously, we recorded the incidence of nosocomial Clostridioides difficile infections as recommended in the IDSA guideline [2] to observe a possible secondary effect of altered prescribing habits.
Antibiotic usage on an individual patient level
Based on the manual review of electronic medical records of our hospital, we additionally obtained individual patient level antibiotic use data for one year prior to and after implementing selective reporting.
We evaluated records of all patients with skin and soft tissue infections (SSTI) caused by S. aureus based on the German invoice system 'DRG' (diagnosis-related groups, group "L"). SSTI were chosen, because there had not been any prior AMS interventions in the relevant departments.
Furthermore we analysed records of all patients with S. aureus bacteremia (SAB) selected by the statistics program of the microbiology laboratory (HyBASE® by epiNET AG, Germany).
Days of therapy (DOT) were evaluated by three independent reviewers. They were counted commencing on day 2 after the receipt of the first S. aureus positive sample in the laboratory. This specific period was chosen; because this is the period it usually takes from the detection of S. aureus to a complete antibiogram being available in the electronic patient record in our hospital. For SAB, maximum follow up was 14 days per patient (recording lost to follow-up because of death, discharge or hospital transfer), as this is the recommended minimal duration of therapy in order to limit future antibiotic usage for secondary complications. Poisson regression was used to investigate the impact of implementing selective reporting on the individual patient level. The patient bed days (BD) were used as an exposure variable. The days of therapy / 100 bed days (DOT/100 BD) were estimated for each antibiotic in the period prior to and after the implementation of selective reporting. Incidence rate ratio (IRR) and corresponding p-values were calculated to compare DOT/100 BD in regard to the two periods.
Additionally, in case of SAB the number of patients with a "reasonable" therapy adaption (defined as replacing any other antibiotic by intravenous flucloxacillin or cefazolin within day 2 to 4) was counted prior to and after intervention.
Differences in patient characteristics (sex, secondary diagnoses / age, bed days) were tested by exact Fisher-test / Mann–Whitney-U-test. All statistical tests were two-sided and the significance level was set at 0.05. For statistical analysis, Stata/IC 16.1 for Unix was used (StataCorp 4905 Lakeway Drive College Station, Texas 77845 USA).
We refrained from any other AMS interventions during the interventional period, except for restricting the use of oral cefuroxime due to its insufficient absorption rate of approximately 50%. This was implemented in both clinics at the same time. In particular, there was no additional consultative support by infectious disease specialists in S. aureus infections.
Results
The monthly number of patients with S. aureus detection in the Helios Clinics of Schwerin was not significantly different during the year prior to and after implementing selective reporting (117 vs. 99 patients per month, p = 0.844). That were approximately 0.5 patients with S. aureus infections/colonisations per 100 occupied bed days (BD), if the total occupied bed days of 549 511 during the observed two-year period is taken into account. The pre- and post-intervention antibiotic use of all available antibiotics in the Helios Clinics of Schwerin and the reference clinic is shown in Table 3.
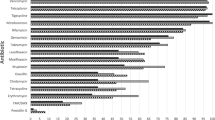
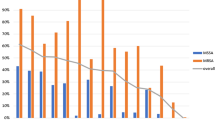
Was there any impact of selective susceptibilitiy reporting on the antibiotic consumption of the entire hospital (Table 3, Figs. 1 and 2)?
Before the start of selective reporting, no difference in the total consumption of the narrow-spectrum beta-lactams (flucloxacillin/cefazolin/cefalexin) could be found between the two hospitals (Table 3). After the implementation of selective reporting in the interventional clinic, there was a significant increase in their total use. This increased use was detected for both intravenous flucloxacillin and cefazolin as first line treatment for severe S. aureus infections (from 0.88 to 1.48 RDD/100 BD, p = 0.007), as well as use of oral cefalexin for less severe infections or follow-up therapy (from 0.29 to 1.35 RDD/100 BD, p = 0.001). Furthermore, an increase in the use of trimethoprim-sulfamethoxazole (p < 0.017) was detected after selective reporting was introduced. Overall, there was a statistically significant increase in the usage of selectively reported antibiotics in the interventional clinic (from 3.38 to 5.34 RDD/100 BD, p = 0.001).
Regarding the course of time there was a slight monthly increase of intravenous flucloxacillin/cefazolin usage in both clinics, but after implementing selective reporting in the interventional clinic the consumption rose immediately and consolidated on a higher level (Fig. 1). For oral cefalexin the interrupted time series analysis showed an immidiate and sustained higher monthly use in contrast to the reference clinic (Fig. 2).
Regarding the antibiotics omitted from the report, no significant change in the consumption was observed after intervention (Table 3). The only exception to this was a slight increase in the use of vancomycin and the very rarely used daptomycin. Compared to the reference clinic, there was a significant lower use of vancomycin and carbapenems in our clinic before the intervention, which aligned to a comparable level of use the year after. Carbapenems were analysed in sum as imipenem was replaced by meropenem during the investigation period due to its lower risk of seizures and expiring patent. For that reason, clinicians were forced to use meropenem instead of imipenem in most indications (e.g. calculated sepsis therapy).
Considering the total overall antibiotic use, there was no relevant difference between boths clinics prior to and after intervention. The incidence of nosocomial C. difficile infections was significantly lower in our clinic even before intervention, without a relevant change after intervention.
Was there any impact of selective susceptibility reporting on the antibiotic treatment of skin and soft tissue infections (SSTI) on an individual patient level (Table 4)?
Searching the DRG system for SSTI "and" S. aureus, we found 222 patients in the year before and 190 patients in the year after intervention. Excluding all patients with MRSA infection, colonization without treatment, mixed infection with other pathogens or death/discharge before susceptibility testing (day 2), the data of 85 versus 88 patients was analysed (Additional file 1: Flow chart exclusion criteria SSTI). The groups were inhomogeneous regarding age (63 versus 55 years in median), comorbidities (chronic renal failure 25 versus 10%) and length of hospital stay (6 versus 3 days in median).
Comparing days of therapy (DOT) of different antibiotics before and after implementing selective reporting (Table 4), we found more than a doubling of DOT per 100 bed days (BD) from 8.4 to 18.0 in the use of intravenous flucloxacillin/cefazolin (primarily used for severe SSTI only). However, this was not statistically significant. The use of intravenous cefazolin was established in our clinic for the first time (data not shown). There was a significant, almost sevenfold increase in the use of oral cefalexin (from 1.4 to 9.4 DOT/100 BD, p = 0.005), without a concurrent reduction in the total use of cefuroxime (13.0 vs. 10.1, p = 0.527)—despite the withdrawal of oral cefuroxime. In sum, the use of all selectively reported antibiotics nearly doubled from 20 to 38 DOT/100 BDs, reaching statistical significance. In contrast, the use of third-generation cephalosporins and carbapenemes ceased completely.
Was there any impact of selective susceptibility reporting on the antibiotic treatment of S. aureus bacteremia (SAB) on an individual patient level (Table 5)?
Searching the Hybase program we found 96 patients with SAB (MRSA excluded) in the year prior to versus 98 patients after implementing selective reporting. All pediatric patients and patients dead, discharged or transferred to another hospital before day 2 were excluded, as were all patients with missing medical records or allergy to penicillin (Additional file 2: Flow chart exclusion criteria SAB). Therefore we analysed the records of 86 versus 81 patients, including 7 versus 16 patients with additional further infections. There were no significant differences of both groups in terms of sex (71 vs. 59% male), age (72 vs. 70 years in median), comorbidities, treating specialty or rate of death within 14 days of therapy (14 vs. 15%).
We found a significant higher use of intravenous flucloxacillin/cefazolin (recommended standard therapy for SAB) after implementing selective reporting, rising from 52.4 to 74.6 DOT/100 BD (+ 42%). The sum of therapy days of all selectively reported antibiotics (except antibiotics for combination therapy only) rose in a similar way. In exchange, there was a sharp decline of the no longer reported ampicillin-sulbactam/amoxicillin-clavunate from 69 to 4 DOT/100 BD and a trend towards lower prescription of most of the other not reported antibiotics (incidence rate ratio 0.77, p = 0.087).
The number of appropriate adaptions of the antibiotic treatment of SAB significantly rose from approximately 42 to 77% of cases (solely the exchange from any other to intravenous flucloxacillin or cefazolin was considered "appropriate"). The total proportion of patients on flucloxacillin/cefazolin rose from 58 to 89%, including all patients who had initially received flucloxacillin.
As a measure of antibiotic consumption, we additionally calculated all DOT per 1000 admissions for SAB and SSTI—without any additional information.
Discussion
Is it possible to guide clinicians to prescribe the optimal antibiotic therapy for S. aureus infections by solely reporting the most effective antibiotics on the antibiogram? A consulting infectious disease specialist (ID)/clinical microbiologist has a huge impact on the optimized therapy of S. aureus infections, but this is costly and often not possible [2, 3, 6, 17, 18]. Guiding the clinician using the antibiogram as an AMS tool could be a very cost-effective alternative, even if it cannot fully replace an ID consultation. Selective antibiotic reporting is recommended by most AMS guidelines [1,2,3, 12, 19, 20], although the evidence is very scant: very few studies have proved a significant effect on antibiotic consumption for urinary tract infections or infections due to gram-negative pathogens [21,22,23,24,25] or for the use of rifampicin [26]. To our knowledge, there are no studies on frequently occurring and often severe S. aureus infections. To date, selective reporting is poorly implemented in Europe (only in about one third of European countries), predominantly for urine cultures; only in Ireland, Turkey, the UK and Sweden is it endorsed as a standard of care by the health care authorities [19, 20, 27,28,29].
Which antibiotics are the most effective in S. aureus infections to be reported on the "selective" antibiogram?
There is broad consensus that narrow-spectrum beta-lactams such as intravenous flucloxacillin or first generation cephalosporins (cefazolin/cefalexin) have better activity against MSSA than broad-spectrum beta-lactams. The treatment of bacteremia caused by S. aureus with high dose intravenous flucloxacillin or cefazolin is associated with lower mortality rates compared to the treatment with broad-spectrum beta-lactams or vancomycin [13,14,15, 30,31,32,33,34,35]. There is a minimum consensus amongst publications to report oxacillin/flucloxacillin, clindamycin and trimethoprim/ trimethoprim-sulfamethoxazole (the latter for oral treatment) on a selective antibiogram for S. aureus, as well as to omit vancomycin, linezolid or broad-spectrum beta-lactams [19, 20, 36].
How can we measure the effect of the intervention?
We monitored the monthly consumption of different antibiotics using RDD/100 BD, a standardised method for measuring antibiotic use, which is not influenced by fluctuating patient numbers. We compared consumption in the year prior to and after implementing selective susceptibility reporting in our clinic to the reference clinic. We used RDD instead of the frequently used defined daily dose (DDD) [2, 37] as the RDD is based on higher daily doses. This represents the doses used in our investigation more closely (Table 2).
Additionally, we analysed antibiotic use on an individual patient level using “Days of therapy” (DOT), favoured by IDSA guideline 2016 [2], as this is not impacted by individual dose adjustments. As our electronic patient file system does not allow an automatic assessment of DOT, patient records were analysed manually by three independent reviewers. Thus, we focussed on two patient groups: SSTI and SAB. We chose SSTI because—in contrast to other specialties—there had not been any previous AMS interventions in the involved departments.
What was the impact of the intervention on the use of selectively reported antibiotics?
Regarding the overall consumption of the hospital there was a significant increase of antibiotics recommended for S. aureus infections (from 3.38 to 5.34 RDD/100 BD, p = 0.001; Table 3) after selectively reporting commenced. This increase was particularly remarkable when put into proportion to the overall low rate of S. aureus infections (less than 0.5 newly detected S. aureus infections/colonisations/100 BD).
Especially the use of narrow-spectrum beta-lactams (flucloxacillin/cefazolin/cefalexin) rose significantly after selective reporting.
Intravenous flucloxacillin and cefazolin—used in SAB and the initial therapy of severe S. aureus infections—were analysed as an entity because they were assessed to be equally effective and replaced each other depending on side effects [30, 31, 38]. Their consumption rose from 0.9 to 1.5 RDD/100 BD throughout the hospital. Although a slight increase in the overall use of narrow spectrum beta-lactams could be seen in both hospitals over the course of time (probably due to general AMS interventions in Germany), the changing of antibiograms in our clinic had an immediate and sustained effect on the treatment of SAB in contrast to the reference clinic (Fig. 1).
There was also an immediate striking increase in the consumption of oral cefalexin used in milder infections or follow-up therapy (from 0.3 to 1.4 RDD/100 BD, p = 0.001) (Table3, Fig. 2). This increase exceeds a possible regulatory effect due to a restriction of oral cefuroxime, preauthorised by the pharmacy (simultaneously in both clinics; plus 1.01 oral cefalexin versus minus 0.53 RDD/100 BDD total cefuroxime in the interventional clinic).
As the use of narrow-spectrum beta-lactams was restricted to targeted treatment of S.aureus infections in both hospitals, the overall consumption data indicates that the selective antibiogram significantly increased their use for those infections.
This assumption was confirmed by our individual patient level data. Days of therapy (DOT) of all selectively reported antibiotics rose significantly from 20 to 38 DOT/100 BD (p = 0.020) in SSTI (Table 4) and from 58 to 79 DOT/100 BD (p = 0.002) in SAB (Table 5). In SSTI, we recorded a striking rise of oral cefalexin usage (predominantly used for mild infections without bacteremia) from 1.4 to 9.4 DOT/100 BD (p = 0.005; from 3 to 17 patients), whereas in SAB there was a significant increase in the use of intravenous flucloxacillin/cefazolin from 52 to 75 DOT/100 BD (p = 0.001; from 50 to 72 patients). Selective reporting obviously strongly supported clinicians to optimize the treatment of S. aureus infections after receiving the report. In 77% of cases with SAB, the therapy was converted to a flucloxacillin/cefazolin regime on day 2–4. This is in contrast to 42% conversion rate before the introduction of selective reporting. If you include cases where treatment had initially been started on a flucloxacillin/cefazolin regime, 72 of 81 (89%) of the patients with SAB received appropriate treatment (50 of 86 before intervention). This number could hardly be further increased, since amongst the SAB group there were patients requiring broader therapy spectrum due to further infections (7 vs. 16 patients, mainly aspiration pneumonias or urinary tract infections). We did not exclude these patients because they were difficult to determine (proven versus suspected infections).
Tan et al.[21] showed a similar significant increase in the consumption of selectively reported antibiotics such as nitrofurantoin for targeted therapy and even for calculated therapy of urinary tract infections. Also, for urinary tract infections McNulty et al. [23]. demonstrated "that prescribing reverted to pre-intervention levels once the change in antibiotic reporting had stopped". We decided not to revert the antibiograms to the pre-interventional stage due to ethical reasons, and the goal to enhance the use of more effective narrow-spectrum antibiotics, along with lowering side-effects was reached.
What was the impact of selective reporting on the use of omitted antibiotics?
Considering the overall consumption of the hospital (RRD/100 BD, Table 3), there was no decrease in the use of wide-spectrum antibiotics after selectively not-reporting for S. aureus (42.4 vs. 44.5 RDD/100 BD, p = 0.249). Neither was there an impact on the number of C. difficile infections. We didn´t expect this anyways due to the wide use of these broader spectrum antibiotics for other infections, e.g. sepsis, pneumonia or meningitis. There was even a slight (partly significant) rise in the usage of broad-spectrum antibiotics such as carbapenems and vancomycin in our clinic. In effect this led to an aligning with the significantly higher baseline level of piperacillin-tazobactam, carbapenems, fluorochinolons and vancomycin usage reported by the reference clinic for the pre-interventional period (see also limitations of RDD/100 BD).
Due to the overall low proportion of S.aureus infections, the reduction in the use of omitted antibiotics might be concealed due to their higher usage for other infections. We therefore evaluated individual patient records for two specific indications additionally. In the SAB group (Table 5), there was a significant decline in the use of aminopenicillin-beta-lactamase-inhibitors (from 7.3 to 0.4 DOT/100 BD, from 18 to 2 patients), in favour of intravenous flucloxacillin/cefazolin. A trend towards lower prescription rates of all no longer reported antibiotics (from 54 to 41 DOT/100 BD, p = 0.087) did not reach statistical significance however. This was probably due to low case numbers (86 vs. 81) and polymicrobial infections (see above). In the SSTI group (Table 4), clinicians waived third-generation cephalosporins and carbapenems (6 vs. 0 cases). Due to the heterogeneity of this group, containing a mixture of SSTI diagnoses, its statistical power was limited.
Limitations
Some limitations to this study need to be mentioned. We evaluated main data by overall antibiotic use by RDD/100 BD, because our electronic patient records did not support statistical evaluations by DOT. However, a general trend towards higher RDD/100 BD is seen throughout many German hospitals caused by a progressive reduction of the average amount of time patient spent in hospital. This is due to the German reimbursement system (DRG) and led to a higher consumption per BD (concentrating intravenous antibiotic therapies using maximal doses during the short stay in the hospital). Additionally average age and number of comorbidities increased. More patients with sepsis needed more wide-spectrum antibiotics [39].
Furthermore, a rise of AMS counselling and interventions within the last decade has already had a significant impact on the treatment of S. aureus infections such as SAB. This is certainly true for our hospital. Therefore, it´s likely that the advantage of implementing selective reporting might have been shown more clearly in clinics without prior AMS activities.
Conclusions
This interventional study is, to our knowledge, the first prospective study to prove the impact of selective reporting for S. aureus on antibiotic use. There is a strong indication that selective antibiotic reporting improves the therapy of S. aureus infections by enhancing the use of narrow-spectrum antibiotics.
Thus, selective reporting of recommended antibiotics is a useful AMS tool, which can be easily implemented with few personnel and technical efforts. We recommend implementing selective reporting rules in the national and international standards for susceptibility reporting.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BD:
-
Bed days
- DOT:
-
Days of therapy
- MSSA:
-
Methicillin-sensitive S. aureus
- MRSA:
-
Methicillin-resistant S. aureus
- RDD:
-
Recommended daily dose
- RDD/100 BD:
-
Recommended daily dose / 100 bed days
- SAB:
-
S. aureus Bacteremia
- SSTI:
-
Skin and soft tissue infections
References
European Centre for Disease Prevention and Control. Proposals for EU guidelines on the prudent use of antimicrobials in humans. Stockholm: ECDC; 2017.
Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al. Implementing an antibiotic stewardship program: guidelines by the infectious diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Inf Dis. 2016;62:e51–77.
de With K, Wilke K, Kern WV, Strauß R, Kramme E, Friedrichs A, et al. S3- Leitlinie Strategien zur Sicherung rationaler Antibiotika-Anwendung im Krankenhaus. AWMF-Registernummer 092/001—update 2018
Allerberger F, Lechner A, Wechsler-Fördös A, Gareis R on behalf of ABS International. Optimization of antibiotic use in hospitals—Antimicrobial Stewardship and the EU Project ABS International. Chemotherapy. 2008;54:260–267.
Howard P, Pulcini C, Levy Hara G, West RM, Gould IM, Harbarth S, Nathwani D; ESCMID Study Group for Antimicrobial Policies (ESGAP); ISC Group on Antimicrobial Stewardship. An international cross-sectional survey of antimicrobial stewardship programmes in hospitals. J Antimicrob Chemother. 2015;70:1245–55.
Schuts EC, Hulscher MEJL, Mouton JW, Verduin CM, Stuart JWTC, Overdiek HWPM, et al. Current evidence on hospital antimicrobial stewardship objectives: a systematic review and meta-analysis. Lancet Infect Dis. 2016;16:847–56.
Osthoff M, Bielicki J, Widmer AF, For Swissnoso. Evaluation of existing and desired antimicrobial stewardship activities and strategies in Swiss hospitals. Swiss Med Wkly. 2017; 147:w14512.
Cunney RJ, Smyth EG. The impact of laboratory reporting practice on antibiotic utilization. Int J Antimicrob Agents. 2000;14:13–9.
Kaki R, Elligsen M, Walker S, Simor A, Palmay L, Daneman N. Impact of antimicrobial stewardship in critical care: a systematic review. J Antimicrob Chemother. 2011;66:1223–30.
Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for Developing an Institutional Program to Enhance Antimicrobial Stewardship. Clin Inf Dis. 2007;44:159–77.
Morency-Potvin P, Schwartz DN, Weinstein RA. Antimicrobial Stewardship: how the microbiology laboratory can right the ship. Clin Microbiol Rev. 2017;30:381–407.
Duguid M, Cruickshank, M. Antimicrobial stewardship in Australian hospitals 2011. Available from https://www.savetyandqualitiy.gov.au/wp-content/uplouds/2011/01/Antimicrobioal-stewardship-in-Australian-hospitals-2011.pdf
Nissen JL, Skov R, Knudsen JD, Ostergaard C, Schønheyder HC, Frimodt-Møller N, Benfield T. Effectiveness of penicillin, dicloxacillin and cefuroxime for penicillin-susceptible Staphylococcus aureus bacteremia: a retrospective, propensity-score-adjusted case-control and cohort analysis. J Antimicrob Chemother. 2013;68:1894–900.
Paul M, Zemer-Wassercug N, Talker O, Lishtzinsky Y, Lev B, Samra Z, Leibovici L, Bishara J. Are all beta-lactams similarly effective in the treatment of methicillin-sensitive Staphylococcus aureus bacteremia? Clin Microbiol Infect. 2011;17:1581–6.
Weis S, Kimmig A, Hagel S, Pletz MW. Antibiotic Stewardship am Beispiel der Staphylococcus aureus Bakteriämie. Med Klin Intensivmed Notfmed. 2017;112:192–8.
Linden A. Conducting interrupted time-series analysis for single- and multiple group comparisons. Stata J. 2015;15:480–500.
Jump RL, Olds DM, Seifi N, Kypriotakis G, Jury LA, Peron EP, et al. Effective antimicrobial stewardship in a long-term care facility through an infectious disease consultation service: keeping a LID on antibiotic use. Infect Control Hops Epidemiol. 2012;33:1185–92.
Rieg S1, Peyerl-Hoffmann G, de With K, Theilacker C, Wagner D, Hübner J, et al. Mortality of S. aureus bacteremia and infectious diseases specialist consultation: a study of 521 patients in Germany. J Infect. 2009;59:232–9.
[PDF] Guidelines for Antimicrobial Stewardship in Hospitals in Irelandwww.hpsc.ie › infectioncontrolandhai › guidelines › File,4116,enSARI Hospital Antimicrobial Stewardship Working Group. December 2009. Published on behalf of SARI by HSE Health Protection Surveillance Centre.
Svenska Läkaresällskapet. Refrensgruppen för antibiotikafragor. Available from: http://www.sls.se/RAF/. Accessed 06 Sept 2016.
Tan TY, McNulty C, Charlett A, Nessa N, Kelly C, Beswick T. Laboratory antibiotic susceptibility reporting and antibiotic prescribing in general practice. J Antimicrob Chemoth. 2003;51:379–84.
Langdale P, Millar ML. Influence of laboratory sensitivity reporting on antibiotic prescribing preferences of genereal practitioners in the Leeds area. J Clin Pathol. 1986;39:233–4.
McNulty CA, Lasseter GM, Charlett A, Lovering A, Howell-Jones R, Macgowan A, Thomas M. Does laboratory antibiotic susceptibility reporting influence primary care prescribing in urinary tract infection and other infections? J Antimicrob Chemother. 2011;66:1396–404.
Coupat C, Pradier C, Degand N, Hofliger P, Pulcini C. Selective reporting of antibiotic susceptibility data improves the appropriateness of intended antibiotic prescriptions in urinary tract infections: a case-vignette randomised study. Eur J Clin Microbiol Infect Dis. 2013;32:627–36.
Langford BJ, Seah J, Chan A, Downing M, Johnstone J, Matukas LM. Antimicrobial stewardship in the microbiology laboratory: Impact of selective susceptibility reporting on ciprofloxacin utilization and susceptibility of gram-negative isolates to ciprofloxacin in a hospital setting. J Clin Microbiol. 2016;54:2343–7.
Steffee CH, Morrell RM, Wasilauskas BL. Clinical use of rifampicin during routine reporting of rifampicin susceptibilities: a lesson in selective reporting of antimicrobial susceptibility data. J Antimicrob Chemother. 1997;40:595–8.
Pulcini C, Tebano G, Mutters NT, Tacconelli E, Cambau E, Kahlmeter G, Jarlier V. On behalf of the EUCIC-ESGAP-EUCAST Selective reporting Working Group. Selective reporting of antibiotic susceptibility test results in European countries: an ESCMID cross-sectional survey. Int J Antimicrob Agents 2017; 49: 162–6.
Nathwani D. Antimicrobial prescribing policy and practice in Scotland: recommendation for good antimicrobial practice in acute hospitals. J Antimicrob Chemother. 2006;57:1189–96.
MacKenzie FM, Gould IM, Bruce J, Mollison J, Monnet DL, Krcmery V, et al. The role of microbiology and pharmacy departments in the stewardship of antibiotic prescribing in European hospitals. J Hosp Infect. 2007;65(Suppl 2):73–81.
Paul M, Kariv G, Goldberg E, Raskin M, Shaked H, Hazzan R, et al. Importance of appropriate empirical antibiotic therapy for methicillin-resistant Staphylococcus aureus bacteremia. J Antimicrob Chemother. 2010;65:2658–65.
Schweizer ML, Furuno JP, Harris AD, Johnson JK, Shardell MD, McGregor JC, et al. Comparative effectiveness of nafcillin or cefazolin versus vancomycin in methicillin-susceptible Staphylococcus aureus bacteremia. BMC Infect Dis. 2011;11:279.
Weber Z, Ariano R, Lgace-Wiens P, Zelenitzky S. Multifaced antibiotic treatment analysis of methicillin-sensitive Staphylococcus aureus bloodstrean infections. J Antimicrob Agents. 2016;48:674–9.
Kim SH, Kim KH, Kim HB, Kim NJ, Kim EC, Oh MD, Choe KW. Outcome of vancomycin treatment in patients with methicillin-susceptible Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2008;52:192–7.
Stryjewski ME, Szczech LA, Benjamin DK Jr, Inrig JK, Kanafani ZA, Engemann JJ, et al. Use of vancomycin or first-generation cephalosporins for the treatment of hemodialysis-dependent patients with methicillin-susceptible Staphylococcus aureus bacteremia. Clin Infect Dis. 2007;44:190–6.
Chang FY, Peacock JE Jr, Musher DM, Triplett P, MacDonald BB, Mylotte JM, et al. Staphylococcus aureus bacteremia: recurrence and the impact of antibiotic treatment in a prospective multicenter study. Medicine (Baltimore). 2003;82:333–9.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; 23rd informational supplement. CLSI document M100-S24. Wayne, PA: CLSI 2014.
Akpan MR, Ahmad R, Shebl NA, Ashiru-Oredope D. A review of quality measures for assessing the impact of antimicrobial stewardship programs in hospitals. Antibiotics (Basel). 2016;5:5.
Bai AD, Showler A, Burry L, Steinberg M, Ricciuto DR, Fernandes T, et al. Comparative effectiveness of cefazolin versus cloxacillin as definitive antibiotic therapy for MSSA bacteremia: results from a large multicentre cohort study. J Antimicrob Chemother. 2015;70:1539–46.
Fleischmann-Struzek C, Mikolajetz A, Schwarzkopf D, Cohen J, Hartog CS, Pletz M, et al. Challenges in assessing the burden of sepsis and understanding the inequalities of sepsis outcomes between National Health Systems: secular trends in sepsis and infection incidence and mortality in Germany. Intensive Care Med. 2018;44(11):1826–35.
Acknowledgements
We thank Hiltrud Niggemann of www.p-wert.de for her help conducting the statistical analysis and Robin Harris for proofreading the manuscript.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
FLB devised the study, analysed overall consumption and individual patient data and wrote the manuscript. RH and IS aided in devising the study, collected and analysed overall antibiotic use and individual patient data and reviewed the manuscript. All other authors supported the implementation of the intervention in the hospital and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Faculty of Medicine at the University of Rostock (A 2017-0149) and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The manuscript does not contain clinical studies or patient data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Flow chart - exclusion criteria of skin and soft tissue infections SSTI.
Additional file 2
. Flow chart - exclusion criteria S. aureus bacteremia (SAB).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lestin-Bernstein, F., Harberg, R., Schumacher, I. et al. Staphylococcus aureus - selective reporting of antibiogram results and its impact on antibiotic use: Interventional study with a reference group on the effect of switching from non-selective to selective antibiotic reporting. Antimicrob Resist Infect Control 10, 157 (2021). https://doi.org/10.1186/s13756-021-01021-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-021-01021-7