Abstract
Background
Antimicrobial resistance has been named as one of the top ten threats to public health in the world. Hospital-based antimicrobial stewardship programs (ASPs) can help reduce antimicrobial resistance. The purpose of this study was to determine perceived barriers to the development and implementation of ASPs in tertiary care centers in three low- and middle-income countries (LMICs).
Methods
Interviews were conducted with 45 physicians at tertiary care hospitals in Sri Lanka (n = 22), Kenya (12), and Tanzania (11). Interviews assessed knowledge of antimicrobial resistance and ASPs, current antimicrobial prescribing practices, access to diagnostics that inform antimicrobial use, receptiveness to ASPs, and perceived barriers to implementing ASPs. Two independent reviewers coded the interviews using principles of applied thematic analysis, and comparisons of themes were made across the three sites.
Results
Barriers to improving antimicrobial prescribing included prohibitively expensive antimicrobials, limited antimicrobial availability, resistance to changing current practices regarding antimicrobial prescribing, and limited diagnostic capabilities. The most frequent of these barriers in all three locations was limited drug availability. Many physicians in all three sites had not heard of ASPs before the interviews. Improved education was a suggested component of ASPs at all three sites. The creation of guidelines was also recommended, without prompting, by interviewees at all three sites. Although most participants felt microbiological results were helpful in tailoring antibiotic courses, some expressed distrust of laboratory culture results. Biomarkers like erythrocyte sedimentation rate and c-reactive protein were not felt to be specific enough to guide antimicrobial therapy. Despite limited or no prior knowledge of ASPs, most interviewees were receptive to implementing protocols that would include documentation and consultation with ASPs regarding antimicrobial prescribing.
Conclusions
Our study highlighted several important barriers to implementing ASPs that were shared between three tertiary care centers in LMICs. Improving drug availability, enhancing availability of and trust in microbiologic data, creating local guidelines, and providing education to physicians regarding antimicrobial prescribing are important steps that could be taken by ASPs in these facilities.
Similar content being viewed by others

Background
It is predicted that by 2050, there will be about 10 million deaths due to antimicrobial-resistant organisms every year if strategies are not implemented to curb the rise of resistant organisms globally [1]. Antimicrobial resistance (AMR) is driven in part by the use, and frequently misuse, of antimicrobials in humans and animals [2]. Antimicrobial courses that are either too short or too long in duration, or too broad in spectrum, can lead to the emergence of resistance.
Antimicrobial stewardship is a set of actions at global, national, and individual levels to promote the rational use of antimicrobials in humans, animals, and the environment [3]. Antimicrobial stewardship programs (ASPs) are programs that allow healthcare systems to strategize use of antimicrobials through the implementation of evidence-based interventions. Implementation of ASPs is one of the recommended strategies to decrease the continued rise of AMR. These programs set forth strict guidelines and restrictions for appropriate use [4]. The Centers for Disease Control and Prevention (CDC) published the guidance document “The Core Elements of Hospital Antibiotic Stewardship” to help hospitals develop these programs. The seven core elements of ASPs laid out in this document include hospital leadership commitment, accountability, pharmacy expertise, action, tracking, reporting, and education. While 85% of hospitals in the United States had ASPs that were compliant with the CDC’s seven core elements by 2018, widespread adoption of hospital-based ASPs in low- and middle- income countries (LMICs) has not been accomplished [5].
The World Health Organization (WHO) developed a practical toolkit for ASPs in LMICs [6]. This document provides guidance on how to implement ASPs in LMICs. However, to implement ASPs at a specific site, it is important to comprehend the local context. In some LMICs, antimicrobials are available in pharmacies, or even in markets, without prescriptions. Quality of antimicrobials is often variable in LMICs as well. In a review of generalized challenges facing LMICs in the implementation of ASPs, the main challenges in many resource-limited settings were access to diagnostics, access to quality antimicrobials, knowledge among practitioners, and healthcare facility infrastructure [7].
Our team has been working to support the implementation of ASPs in a context-sensitive manner in Sri Lanka, Kenya, and Tanzania. Our US academic medical center has strong research relationships with tertiary care hospitals in each of these countries. As these are the centers where we are actively working, we felt it would be appropriate to evaluate barriers that are either shared between or unique to these three sites. All three hospitals are at the tertiary care level, allowing for comparison between the countries. In this study, we conducted a qualitative assessment of medical doctors at different levels of training in medical wards in hospitals in each of the three countries to assess receptiveness to ASPs and to elicit opinions on the design of these programs within their health systems. The goal of this study was to identify perceived barriers to the development and implementation of ASPs.
Methods
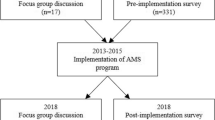
This was a qualitative study of physicians to understand their perceptions of current antimicrobial use and receptiveness to ASPs. Individual in-depth interviews were conducted with 45 physicians in 2018 at three tertiary care hospitals in Sri Lanka, Kenya and Tanzania.
Setting and participants
The hospital in Sri Lanka is a public tertiary care center with 1,800 beds and 10 adult medical wards. This hospital has a microbiology laboratory and radiology services, and provides all medications, testing, and care free of charge to patients. The hospital has a microbiology specialty service consisting of an attending-level microbiologist, microbiology physicians in training, and infection prevention nurses, and can be consulted by other physicians in the hospital for advice regarding antimicrobial prescribing. Pharmacists dispense medications but otherwise are not involved in clinical care and do not provide advice on therapy.
The hospital in Kenya is a public hospital with 990 beds and two adult medical wards. Patients pay for all medications, diagnostic testing, and care but some have national insurance which covers all of their health expenses. This hospital does not have an infectious diseases or a clinical microbiology specialty service. Clinical pharmacists participate in ward rounds with the clinicians and provide advice on therapy.
The hospital in Tanzania is a referral hospital with 630 beds and four adult medical wards. Patients pay for all medications, diagnostic testing, and care but some have national insurance, which covers all of their health expenses. If the patients cannot afford care, they can receive financial support from the hospital. This hospital has an infectious diseases specialty service that is staffed by one physician with infectious diseases and antimicrobial stewardship training. Pharmacists dispense medications but do not generally provide advice on therapy.
In each of the three study hospitals, physicians were eligible to participate if they were working on the adult medical wards, regardless of medical specialty and level of experience. Physicians were selected for enrollment in the study based on convenience sampling.
Procedures
The interview guide was developed through collaboration between study team members from Sri Lanka, Kenya, Tanzania and the United States. The interview guide explored current antimicrobial prescribing practices at the participant’s hospital, knowledge regarding antimicrobial resistance and stewardship, and receptiveness to ASP interventions. The first section of the interview guide covered current clinical practices with regards to treating infections; clinical examples were also elicited from the interviewees. The second section covered education regarding antimicrobial resistance and stewardship and current understanding of ASPs. The purpose of this section was to build an understanding of current understanding and beliefs around antimicrobial resistance and ASPs. The third section was dedicated to developing an understanding of local providers’ receptiveness to ASPs.
Interviews were conducted by trained, local research assistants (nurses or doctors) at each site. Interviews were conducted in English, which is the working language by physicians at each hospital, and lasted approximately 45 min. The interviewer followed the interview guide and used open-ended questions with follow-up probes to elicit more detailed information. Each interview was audio-recorded and subsequently transcribed.
Data analysis
We used applied thematic analysis to analyze the textual data [8]. Two physician researchers initially coded the interviews independently using a set of deductive codes informed by the interview guide. Emergent themes in the interviews were then identified by noting common patterns across the interviews. These were discussed between the two researchers, resulting in a detailed codebook that included both deductive and inductive codes. After completion of independent coding of all interviews by both physician researchers, consensus coding was developed that resolved disagreements between the two physicians. After the initial coding was completed, each deductive code was further categorized—for example, the deductive code of “distrust of diagnostics” was a category created under “use of diagnostics in clinical practice.” The codes were compared between sites based on the number of interviewees at each site who reported similar opinions. NVivo (Version 12) was used to code the interviews.
Ethical procedures
All interviewed physicians provided written informed consent prior to participation in this study. Ethical approval was obtained from the Duke University Institutional Review Board in the United States, the Ethical Review Committee of the Faculty of Medicine at the University of Ruhuna in Sri Lanka, AMPATH and the Institutional Research and Ethics Committee of Moi University/ Moi Teaching and Referral Hospital in Kenya, the Kilimanjaro Christian Medical College Research Ethics and Review Committee, and the National Institute for Medical Research in Tanzania.
Results
In total, 45 physicians were interviewed during this study. Table 1 includes details about the study participants.
Several themes emerged that were either shared or different across the domains of current practices, barriers to implementation of ASPs, and approach to ASP implementation. Table 2 provides a sample of representative quotations from the interviews for each theme.
Current practices
Discrepancies between desired and actual antimicrobial treatment
Respondents noted a discrepancy between the treatment they desired to prescribe and the one they actually administered. At all three sites, high cost and limited availability were the major drivers of discrepancy between desired and actual antimicrobial treatment. Some physicians described situations in which they were stuck between the decision of treating with an antimicrobial that may not work given an organism’s susceptibility pattern versus not treating at all due to lack of access to antimicrobials to which the organism appeared susceptible.
“Sometimes the culture report is sensitive for antimicrobials which are not available in the hospital at the moment. So we have to go with some antibiotics available at that time. And we are usually not asking the patient to buy from outside. So like if the patient is sensitive to meropenem and if it is not available, we are using third-generation cephalosporin.” I-11
Similar statements regarding cost as a barrier to prescribing desired antimicrobial agents was shared by 4/22 physicians in Sri Lanka, 4/12 in Kenya, and 5/11 in Tanzania. In interviews at all study sites, prohibitive cost of antimicrobials both during admission and after discharge were discussed. Even in the hospital in the public hospital in Sri Lanka, when antimicrobials were not available in the hospital, patients were asked to purchase them from the private sector.
“Most of the time they are not available in the hospital setting, freely available. Sometimes the patient cannot afford for a private sector. We ask the patient but they cannot afford. In that case we are going to shift to another drug which is similar or same class of antibiotic” I-10
Limited availability was mentioned by 9/22 physicians in Sri Lanka, 9/12 in Kenya, and 4/11 in Tanzania. Prior exposure to antimicrobials from either local pharmacies or clinics had an impact on the choice of antimicrobials used after patients were admitted, per one interview each in Kenya and Tanzania. Poor drug quality of meropenem was listed as a reason for discrepancy between desired and actual treatment in 2/22 of the interviews in Sri Lanka but was not mentioned in either Kenya or Tanzania.
The role of consultants, pharmacists, and other staff in antimicrobial prescribing
Overall, many physicians sought specialist advice, when available, from the microbiology or infectious diseases services for the management of complicated cases. The recommendations from specialists regarding antimicrobial prescription was followed by the clinicians who requested the advice at all study sites. Only 2/22 participants in Sri Lanka expressed concern over specialist input as they felt the consultants did not have as much clinical context as they did. “Sometimes they are not clinically relevant in my personal opinion.” I-3. This concern was not raised in Kenya or Tanzania.
Opinions regarding the role of clinical pharmacists in antimicrobial prescribing varied among the three sites. In the hospital in Kenya, clinical pharmacists rounded with the ward teams. As the pharmacists were in frequent contact with physicians, pharmacists’ opinions on prescribing seemed to be more respected than in other locations. “A very big role. I must congratulate the hospital has set up clinical pharmacy here so that at least every team, most teams have a pharmacist and it plays a big role and it really assists in patient management.” – I-23.
In the hospital in Sri Lanka, where there is no contact between pharmacists and physicians during daily clinical work, the value of pharmacists’ input was not as apparent to the physicians. “[Pharmacists] don’t come to the wards. From them we only get to know whether the drugs are available.” -I-22.
The importance of nursing staff in antimicrobial prescribing varied among the sites as well, but physicians from all three sites recognized the important role that nurses have in monitoring patients’ clinical status and in the delivery of antimicrobials. The value of nurses in monitoring patients and delivering antimicrobials was mentioned in 4/22 interviews in Sri Lanka, 9/12 in Kenya, and 5/11 in Tanzania.
The impact of the clinical microbiology laboratory and laboratory diagnostics in the prescription of antimicrobials
Results from microbiological cultures were felt to be very helpful for tailoring antibiotic courses. However, some physicians were concerned with the reliability of the culture results from their microbiology laboratories. There was concern that cultures may be contaminated when they were obtained, resulting in mixed bacterial growth that was difficult to interpret. Also, others mentioned distrust in the microbiology laboratory when cultures were negative, even when infections were highly suspected. Some remarked that most clinical decisions were made before culture results were available. These concerns may impact the ability of providers to narrow the spectrum of antimicrobial treatment.
“So maybe I don’t know if there are other modalities of doing culture or maybe the way people are taking the cultures may be the sterility is not perfect or the growing of the organisms… Because sometimes you might find that your patient has fever or other signs of infection, but the culture comes out negative… You take another culture but it comes out negative also. Sometimes you are not really sure. There is human error or lab error which can happen.” -I-36.
In addition to discussing bacterial cultures, the use of biomarkers in clinical decision-making was considered. Erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP), two biomarkers which are sometimes used to identify the presence of infection, were generally thought to not provide much additional evidence for physicians to start antimicrobials as they were markers of inflammation and too non-specific to have an impact on antimicrobial use. “Chronic diseases, inflammatory diseases, auto-immune diseases, almost anything can raise the ESR, so it’s not anything that I would use to start antibiotics based on ESR” -I-43.
Procalcitonin, a newer biomarker that is sometimes used to differentiate between bacterial and viral infection, was not available at any of the three sites. While most physicians felt procalcitonin would be helpful if available, 9/22 participants in SL, 5/12 in Kenya, and 5/11 in Tanzania were uncertain if procalcitonin would be helpful mostly given limited (or no) experience with its use clinically. Four participants felt procalcitonin would not be helpful in determining if antibiotics were needed (2 Sri Lanka, 1 Kenya, 1 Tanzania). Reasons cited included that procalcitonin is not specific for bacterial infection, is a prognostic not diagnostic marker, and is too expensive.
Education on antimicrobial resistance and ASPs
Most participants at all three sites stated that their training in antimicrobial resistance occurred in medical school. “Obviously antimicrobial resistance is something you learn in school… It is just book knowledge what you were taught in medical school. Now on practice point when you are seeing patients you suspect antimicrobial resistance because, maybe your patient is not responding to the therapy you are giving.” - I-29.
Many physicians stressed the important role of clinical training or work experience. “Clinical experience is mostly important, for example I have seen most of the junior doctors, and they used antibiotics unnecessarily. But with their experience you can learn most of the infections are due to viral infection which does not need antibiotics.” -I-13.
One participant mentioned reading articles online and on Up-To-Date to learn more about antimicrobial prescribing practices. “Well, mostly is my own readings from Up-To-Date, and do I had any, maybe once, not a recent though, CME; mostly from my own readings, from Up-To-Date and CMEs.” -I-32.
In total, 19/22 respondents in Sri Lanka, 8/12 in Kenya, and 7/11 in Tanzania had not heard of ASPs before these interviews.
Barriers to implementation of ASPs
Diagnostic uncertainty and limited awareness of local antimicrobial resistance patterns
Most participants at all three sites were not aware of the antimicrobial resistance patterns at their hospitals or of resources available to find this information.
“I don't think we get as much data back. So it's mostly anecdotal, certainly there've been resistant gram negatives. They are certainly concerned about MRSA, but I've never actually seen a positive culture for it. It's really unfortunately hard to even approach this from an institutional perspective given the lack of data.”-I-34
However, one respondent in Sri Lanka was able to discuss different antimicrobial-resistant infections that were felt to be more prevalent in certain wards. “In orthopedic wards, MRSA is a common problem. In the ICU, resistant Acinetobacter ventilator-associated pneumonia is difficult to control with antibiotics because of the resistance. In the medical ward ESBL UTIs… Those are the resistant bacteria I’ve heard of in our hospital.”- I-17.
Local clinical practice customs regarding antimicrobial prescribing
Local traditions regarding antimicrobial prescribing practices and workflow were cited as a potential barrier to the future implementation of ASPs by 12/22 in Sri Lanka, 4/12 in Kenya, and 3/11 in Tanzania. Some cited concerns about the extra time that documentation would take given the busy clinical services. Others felt that many would resist the changes or recommendations from ASPs as these would often require physicians to change their normal practices. “But I think the biggest thing is to break the traditions and to teach the people on which antibiotics are best and not just to prescribe one type of antibiotic to everyone you see.” – I-43.
Unrestricted access to antimicrobials
As discussed in ‘Current Practices’ above, drug availability was mentioned as a potential barrier to ASPs by participants in all three countries. Over-the-counter use or use in private facilities was also felt to be an impediment to rational use of antimicrobials.
“Mainly in the private sector... Because in Sri Lanka we don’t have the general practitioners who are established. So, a lot of the MBBS doctors will be doing the private practice at different places and there what the people want is some quick response to the symptoms they have. So generally, the practice there is of giving high-power antibiotics at the initial stage of disease. That of course conflicts very badly with our antimicrobial practices through Sri Lanka.” - I-21
Approach to ASP implementation
Creation of guisdelines
The creation of guidelines was a recommendation raised by interviewees, without prompting, at all three sites (13/22 in Sri Lanka, 7/12 in Kenya, 5/12 in Tanzania) as a strategy to improve the use of antimicrobials in the hospital setting. “I think we should prepare our own guidelines for our hospital with the help of the microbiologist and whole medical team. All the consultant physicians, MOs (medical officers) in pediatrics and medicine and we should make our own guidelines and these guidelines should be evaluated at least in 3 months, 6 months at least annually and change our prescription pattern.”-I-13.
Improving clinical documentation
Documentation of the reasons for prescribing antibiotics can improve communication between physicians and other staff. Documenting the justification will also give physicians another opportunity to think through their reasoning for using a given antimicrobial. Most participants at all three sites were receptive to documenting reasons for prescribing antibiotics in the chart. “The benefits will be many. Because you know this unnecessary prescribing will make doctors more aware that if I do this, someone will ask me… Why did I do this? So even the thought process will increase that instead of just giving an antibiotic, you know, you’re thinking… Where, why these antibiotics will cover this area… And it will also help us know which antibiotics are right, you know, in collaboration with the stewardship program. So the advantages are many.”—I-43.
However, some noted the high clinical volume as a potential impediment to thorough documentation.
“It is important but impractical, given the conditions we work here, we usually encounter around 50 to 70 patients in a casualty (on call) night. So, it is not practical to document everything though it’s ideal.”- I-14
Structure of ASP leadership
Views on who should be involved in ASP leadership mirrored views on current practices regarding advice from consultants, pharmacists, and other staff. In all three countries, participants valued recommendations from specialists and stated they would take advice from physicians involved in ASP leadership. However, there were mixed views on the opinions of clinical or hospital-based pharmacists. All of the participants in Kenya were receptive to pharmacist input (12/12), all but one in Tanzania were receptive 10/11, but 12/22 in Sri Lanka opposed.
Improving education on antimicrobial resistance and stewardship
Improving education regarding antimicrobial prescribing and resistance patterns was a non-elicited strategy mentioned in all three countries in the development of ASPs (7/22 in Sri Lanka, 6/12 in Kenya, 6/12 in Tanzania). Many interviewees did not limit the education only to physicians, but also included pharmacists and nurses. “It is mainly about knowledge and information that should be provided to all the medical personnel, so even the nurses, doctors, the pharmacists… these should be also involved in the prescribing of antibiotics and not just writing unnecessarily.”-I-37.
Discussion
We conducted a multi-site qualitiative study in tertiary medical centers in three LMIC to determine the barriers to and feasibility of ASPs in a context-sensitive manner to inform our implementation of ASPs in these centers. The interviews shared many similarities between sites. A common theme was the lack of prior knowledge of ASPs accompanied by the willingness to participate if programs were developed locally. Additionally, the interviews highlighted a lack of adequate diagnostic capabilities, availability of specific antimicrobials and frustration over costs of medications.
Our study identified the need for improved access to a variety of antimicrobials, as physicians were frequently forced to treat infections with antimicrobials on hand, even when the organisms causing infections were resistant to the antimicrobials. Lack of access to antimicrobials is an issue shared in other LMICs as well. One study of Nigerian physicians suggested similar concerns in lack of access to antimicrobials when developing ASPs locally [9]. Ensuring quality antimicrobials is important as well. A meta-analysis peformed in 2018 indicated a prevalence of 13.6% in substandard or falsified antimicrobials in LMICs [10]. The low quality of meropenem available through the public healthcare system was discussed by multiple physicians in Sri Lanka. Counterfeit or substandard medications that have lower levels of active drug than labeled pose a risk for future antimicrobial resistance [11]. In a 2020 review of the 2013 Lancet Commission on antimicrobial resistance, little progress in the surveillance for counterfeit or sub-standard antibiotics had occurred in the interim [12].
Empiric antimicrobial use was frequently attributed to long turnaround times from the microbiology lab. Lack of diagnostic capabilities and distrust in microbiological culture results was a common theme raised by physicians. When discussed with members of our team to clarify reasons for distrust in microbiology results, team members stated that many patients at their centers were transferred from other hospitals, having already had long hospitalizations, antibiotics, and limited to no microbiologic testing. In these situations, providers often feel there is little utility to collecting blood cultures and empirically place patients on broad-spectrum antibiotics. In other studies, physicians have attributed the overuse of antimicrobials to lack of diagnostic capability [13]. In a qualitative study performed in a secondary level hospital in India where physicians and clinical pharmacists were interviewed, unreliable antibiograms were described as a challenge in implementing stewardship programs. As many of the physicians used empiric antibiotics, and cultures were only drawn when patients were not responding to therapy, the sensitivities from cultures were likely skewed toward higher resistance than was truly present within the hospital [14]. Improved laboratory capacity and structured surveillance techniques to create an antibiogram is a critical need in many LMICs to improve antimicrobial prescribing. In 2018, the WHO published a list of essential diagnostic tests, which included microbiologic cultures and antimicrobial susceptibilitiy testing [15]. However, improvement in diagnostic capabilities needs to be accompanied by “building trust” between the diagnostic laboratories and physicians. In a study of physicians’ perceptions regarding the utility of laboratory diagnostics in Ghana, despite high laboratory capacity, local providers remained reliant on clinical judgement and empiric therapy [16]. Improving the trust of clinical providers in the results provided by the microbiology laboratory could help improve prescribing behaviors. Representation of clinical microbiology varies greatly in ASP leadership. However, their inclusion would enhance the communication between the laboratory and clinical care [17]. Improving communication could help increase trust in microbiology among clinicians. Summary data on commonly identified bacteria and their antimicrobial resistance patterns within each hospital could be used to guide the choice of empiric antimicrobials. In addition, local susceptibility and culture data could inform the development of antimicrobial guidelines. The development of a local antibiogram and local guidelines could be key actions targeted by ASPs at these LMIC hospitals.
Widespread (or easily accessible) hospital-level antimicrobial treatment guidelines are not available for physicians in either Tanzania or Kenya. The providers in these countries occasionally would look to other resources or guidelines to determine the appropriate antimicrobial therapy. As resistance rates differ between countries, this could lead to inappropriate use of antimicrobials in different clinical situations. The Infectious Diseases Society of America (IDSA) recommends the creation of guidelines based on local resistance patterns to improve the utilization of antimicrobials [18].
Education would also be essential in the introduction of ASPs in these hospitals. The majority of participants at all three sites had never heard of ASPs previously and routine practices recommended by ASPs did not seem to be a part of their daily prescribing habits. Most participants cited medical school as the last time they had received formal training regarding antimicrobial resistance and antimicrobial prescribing practices. Strategies for improving education regarding antimicrobial resistance and stewardship practices range widely from short didactic sessions to bedside stewardship rounds to dedicated continuing medical education sessions on antimicrobial resistance and stewardship [19]. Education for pharmacists would also be an important component of ASPs. A study assessing the knowledge of Australian pharmacy students compared to Sri Lankan pharmacy students showed a lower level of knowledge about antimicrobial resistance among the students from Sri Lanka [20].
Another important factor for the implementation of ASPs in these hospitals woud be determining the leadership structure for such programs. In the site in Kenya, a team comprised of both pharmacists and physicians would likely be effective based on opinions expressed in the Kenyan interviews, as pharmacists are frequently involved in clinical care. However, in both Tanzania and Sri Lanka, physicians did not feel the pharmacists should play a large role in antimicrobial prescribing decisions. These opinions seemed to correlate with the amount of contact the physicians had with pharmacists on the unit floors or in daily practice. Based on our interviews, we believe that leadership of ASPs in the sites in Tanzania and Sri Lanka would both benefit from strong physician leadership. However, further education of physicians regarding the diverse roles of other staff in antimicrobial prescribing, as well as encouraging pharmacists to engage more closely in clinical care, may also be beneficial. Ultimately, we believe that ASPs should be multidisciplinary teams.
There were several limitations in this study. First, this study was limited to a small number of participants at three hospitals in three LMICs. Extrapolation to national trends even within these countries would not be possible nor would extrapolation to all LMICs. The participants of the interviews were all physicians in medicine or medicine subspecialties. Opinions of surgeons, pharmacists, or other hospital staff were not elicited and may have differed significantly from the opinions expressed in these interviews. These interviews were all performed in tertiary care centers, and themes relevant to other levels of care are likely not highlighted in these interviews. For example, many physicians in our study discussed the widespread availability of antibiotics in community pharmacies. However, perspectives from community pharmacy and primary care providers are notably missing in this analysis; such perspectives may have raised themes such as poor access to licensed physicians being a driver of antibiotic use in the community [21].
Conclusion
In conclusion, views shared between the three sites on current barriers to appropriate antimicrobial prescribing included lack of availability or prohibitive cost of antimicrobials, distrust in results from the microbiology lab, and resistance to change from established, or traditional, practices. Next steps for the implementation of ASPs in these hospitals should include widespread educational programs for physicians and staff, the creation of hospital-specific guidelines for appropriate antimicrobial use, and the development of multidisciplinary ASP teams that eventually include representatives for physicians, pharmacists, and microbiologists.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASPs:
-
Antimicrobial Stewardship Programs
- CDC:
-
Centers for Disease Control and Prevention
- LMICs:
-
Low- and middle- income countries
- MBBS:
-
Bachelor of Medicine, Bachelor of Surgery
- MO:
-
Medical Officer
- WHO:
-
World Health Organization
References
No Time To Wait: Securing the future from drug-resistant infections: Interagency Coordination Group on Antimicrobial Resistance World Health Organization; 2019 [Available from: https://www.who.int/antimicrobial-resistance/interagency-coordination-group/IACG_final_report_EN.pdf?ua=1.
Huttner A, Harbarth S, Carlet J, Cosgrove S, Goossens H, Holmes A, et al. Antimicrobial resistance: a global view from the 2013 World Healthcare-Associated Infections Forum. Antimicrob Resist Infect Control. 2013;2:31.
Dyar OJ, Huttner B, Schouten J, Pulcini C, Esgap. What is antimicrobial stewardship? Clin Microbiol Infect. 2017;23(11):793–8.
Core Elements of Hospital Antibiotic Stewardship Programs: Centers for Disease Control and Prevention; 2020 [Available from: https://www.cdc.gov/antibiotic-use/core-elements/hospital.html.
de Oliveira TC, Rodrigues PT, Menezes MJ, Goncalves-Lopes RM, Bastos MS, Lima NF, et al. Genome-wide diversity and differentiation in New World populations of the human malaria parasite Plasmodium vivax. PLoS Negl Trop Dis. 2017;11(7):e0005824.
. World Health Organization. Antimicrobial stewardship programs in health-care facilities in low- and middle-income countries: a WHO practical toolkit. World Health Organization. https://apps.who.int/iris/handle/10665/329404. License: CC BY-NC-SA 3.0 IGO (2019).
Cox JA, Vlieghe E, Mendelson M, Wertheim H, Ndegwa L, Villegas MV, et al. Antibiotic stewardship in low- and middle-income countries: the same but different? Clin Microbiol Infect. 2017;23(11):812–8.
Guest G, MacQueen KM, Namey EE. Applied thematic analysis. Los Angeles: Sage Publications; 2012. xx, 295 p.
Kpokiri EE, Taylor DG, Smith FJ. Development of Antimicrobial Stewardship programmes in low and middle-income countries: a mixed-methods study in Nigerian Hospitals. Antibiotics (Basel). 2020;9(4).
Ozawa S, Evans DR, Bessias S, Haynie DG, Yemeke TT, Laing SK, et al. Prevalence and estimated economic burden of substandard and falsified medicines in low- and middle-income countries: a systematic review and meta-analysis. JAMA Netw Open. 2018;1(4):e181662.
Kelesidis T, Falagas ME. Substandard/counterfeit antimicrobial drugs. Clin Microbiol Rev. 2015;28(2):443–64.
Laxminarayan R, Van Boeckel T, Frost I, Kariuki S, Khan EA, Limmathurotsakul D, et al. The lancet infectious diseases commission on antimicrobial resistance: 6 years later. Lancet Infect Dis. 2020;20(4):e51–60.
Gebretekle GB, Haile Mariam D, Abebe W, Amogne W, Tenna A, Fenta TG, et al. Opportunities and barriers to implementing antibiotic stewardship in low and middle-income countries: Lessons from a mixed-methods study in a tertiary care hospital in Ethiopia. PLoS ONE. 2018;13(12):e0208447.
Mathew P, Ranjalkar J, Chandy SJ. Challenges in implementing Antimicrobial stewardship programmes at secondary level hospitals in India: An exploratory study. Front Public Health. 2020;8:493904.
. World Health Organization. World Health Organization model list of essential in vitro diagnostics. First edition (2018). WHO, Geneva (2018). URL: http://www.who.int/medical_devices/diagnostics/WHO_EDL_2018.pdf, Accessed 1 Aug 2020.
Polage CR, Bedu-Addo G, Owusu-Ofori A, Frimpong E, Lloyd W, Zurcher E, et al. Laboratory use in Ghana: physician perception and practice. Am J Trop Med Hyg. 2006;75(3):526–31.
Morency-Potvin P, Schwartz DN, Weinstein RA. Antimicrobial Stewardship: How the microbiology laboratory can right the ship. Clin Microbiol Rev. 2017;30(1):381–407.
Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159–77.
Kakkar AK, Shafiq N, Singh G, Ray P, Gautam V, Agarwal R, et al. Antimicrobial Stewardship programs in resource constrained environments: understanding and addressing the need of the systems. Front Public Health. 2020;8:140.
Sakeena MHF, Bennett AA, Carter SJ, McLachlan AJ. A comparative study regarding antibiotic consumption and knowledge of antimicrobial resistance among pharmacy students in Australia and Sri Lanka. PLoS ONE. 2019;14(3):e0213520.
Barker AK, Brown K, Ahsan M, Sengupta S, Safdar N. What drives inappropriate antibiotic dispensing? A mixed-methods study of pharmacy employee perspectives in Haryana, India. BMJ Open. 2017;7(3):e013190.
Acknowledgements
We would like to thank all the participants, research assistants, and administrative staff who were involved in this study.
Funding
This study was supported by funding from the Duke Global Health Institute. LGT is supported by a Grant from the National Institute of Allergy and Infectious Diseases (K23AI125677). Robert Rolfe received funding from the Hubert Yeargan Center and the Duke Global Health Institute.
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the participating sites. All interviewed physicians provided written informed consent prior to participation in this study. Ethical approval was obtained from the Duke University Institutional Review Board in the United States, the Ethical Review Committee of the Faculty of Medicine at the University of Ruhuna in Sri Lanka, AMPATH and the Institutional Research and Ethics Committee of Moi University/Moi Teaching and Referral Hospital in Kenya, the Kilimanjaro Christian Medical College Research Ethics and Review Committee, and the National Institute for Medical Research in Tanzania.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rolfe, R., Kwobah, C., Muro, F. et al. Barriers to implementing antimicrobial stewardship programs in three low- and middle-income country tertiary care settings: findings from a multi-site qualitative study. Antimicrob Resist Infect Control 10, 60 (2021). https://doi.org/10.1186/s13756-021-00929-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-021-00929-4