Abstract
Background
Staphylococcus aureus is the most common and most important pathogen following knee and hip arthroplasty procedures. Understanding the epidemiology of invasive S. aureus infections is important to quantify this serious complication.
Methods
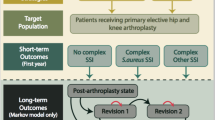
This nested retrospective cohort analysis included adult patients who had undergone insertion of knee or hip prostheses with clean or clean-contaminated wound class at 11 hospitals between 2003–2006. Invasive S. aureus infections, non-superficial incisional surgical site infections (SSIs) and blood stream infections (BSIs), were prospectively identified following each procedure. Prevalence rates, per 100 procedures, were estimated.
Results
13,719 prosthetic knee (62%) and hip (38%) insertion procedures were performed. Of 92 invasive S. aureus infections identified, SSIs were more common (80%) than SSI and BSI (10%) or BSI alone (10%). The rate of invasive S. aureus infection/100 procedures was 0.57 [95% CI: 0.43-0.73] for knee insertion and 0.83 [95% CI: 0.61-1.08] for hip insertion. More than half (53%) were methicillin-resistant. Median time-to-onset of infection was 34 and 26 days for knee and hip insertion, respectively. Infection was associated with higher National Healthcare Safety Network risk index (p ≤ 0.0001).
Conclusions
Post-operative invasive S. aureus infections were rare, but difficult-to-treat methicillin-resistant infections were relatively common. Optimizing preventative efforts may greatly reduce the healthcare burden associated with S. aureus infections.
Similar content being viewed by others
Introduction
The impact of surgical site infections (SSIs) following prosthesis procedures is devastating, often leading to higher mortality, prolonged hospitalizations, frequent readmissions, and increased costs and overall healthcare burden [1,2]. According to the United States (US) National Healthcare Safety Network (NHSN), SSI rates following total knee or hip arthroplasty procedures performed from January 1, 2006 through December 31, 2008 ranged from 0.60 to 1.60 and 0.7 to 2.4 per 100 procedures, respectively, depending on patient risk level [3]. Common factors between knee and hip procedures found to be associated with increased risk for deep incisional or organ/space SSIs include younger age, revision procedures, longer procedure duration, severity of underlying illness, hospital affiliation with a medical school, bed size >200, and trauma [4].
Staphylococcus aureus is the most common and most important pathogen following these and other orthopedic procedures. S. aureus accounts for approximately half of the deep incisional or organ/space SSIs following knee or hip joint arthroplasty reported to NHSN, with methicillin-resistant S. aureus accounting for 19% of these infections [5]. At a single-center [6], the reported rate of SSI was 1.1 per 100 procedures following total joint arthroplasty between 2003 to 2005, with S. aureus accounting for more than 50% of the infections; in addition, methicillin-resistant S. aureus (MRSA) accounted for 21% of SSIs following total knee arthroplasty and 31% of SSIs following total hip arthroplasty.
Using data from over 96,000 orthopedic, neurosurgical, cardiothoracic, and plastic surgical procedures performed in adults, we recently showed that S. aureus was the causative pathogen for about 50% of all invasive post-operative infections [7]. Of these S. aureus infections, SSI were diagnosed more often (70%) versus bloodstream infections (BSI) alone (30%). The overall rate of invasive S. aureus infections was 0.47 infections per 100 procedures (95% CI, 0.43-0.52) [7]. The rate of invasive S. aureus infections in the orthopedic surgery subgroup (insertion of prosthetic implants [ie, insertion of knee, hip, or other prosthesis], open reduction and internal fixation of a fracture, other musculoskeletal procedures, or amputation) in the preceding study was 0.37 infections per 100 procedures [95% CI, 0.32-0.42]. These infections were associated with three variables included in the NHSN risk index score: 1) American Society of Anesthesiologists (ASA) score; 2) wound class; and 3) length of procedure and patient age. In addition, orthopedic procedures involving prosthetic implants had a higher incidence of invasive S. aureus infections, 0.68 infections per 100 procedures (95% CI, 0.56-0.81), than the overall orthopedic subgroup. In the current report, we describe the incidence of invasive S. aureus SSI and BSI in the subset of 13,791 surgical procedures involving knee or hip prosthetic devices from the preceding cohort of 96,455 major surgical procedures. We also assessed potential risk factors for S. aureus infection in this group.
Methods
Study design and population
The study design has been previously described in detail [7]. Briefly, we previously performed a multicenter, retrospective cohort study using validated, prospectively collected surgical surveillance data for SSI and microbiologic data for BSI from nine community hospitals and two tertiary hospitals in North Carolina and Virginia from 2003 to 2006. Two surgical surveillance databases were used: the Duke Infection Control Outreach Network (DICON) surgical database and the Duke University Medical Center (DUMC) surgical database. These databases included operative variables such as patient age, date of surgical procedure, type of procedure, and NHSN risk index variables (i.e., wound class, ASA score, and length of procedure). At each hospital, all SSIs were prospectively identified by trained infection-control practitioners (ICPs) using standard definitions and methods [8]. ICPs used culture results from the clinical microbiology laboratory, readmission flags, and surgeon surveys to identify patients with potential SSIs. BSI data were identified by querying microbiological databases from each participating hospital. The Duke University Health System Institutional Review Board for Clinical Investigations (DUHS IRB) was the review board overseeing the study, and served as the IRB of record for the participating hospitals.
The study population comprised patients at least 18 years of age who underwent a major surgical procedure between January 1, 2003 through December 31, 2006 (N = 81,267 patients undergoing 96,455 surgical procedures). The nested retrospective analysis was limited to prosthetic surgical procedures (knee or hip insertion) with clean or clean-contaminated wound class (N = 13,719 procedures).
Outcome measures
The primary outcome was invasive SSI and/or BSI due to S. aureus. Invasive SSIs were defined as deep incisional and organ/space SSIs diagnosed within one year following surgery, consistent with Centers for Disease Control and Prevention (CDC) defintions [8]. BSIs were defined using modified CDC criteria: at least one positive blood culture within 90 days after the procedure for all pathogens except coagulase-negative staphylococci, micrococci, Propionibacteria, diphtheroids, enterococci, viridans group streptococci, and bacilli, for which at least two positive results for cultures of blood collected during a 48-hour period were required [9]. Other outcomes of interest included methicillin susceptibility of S. aureus isolates and time to infection.
Statistical analysis
This analysis was restricted to surgical procedures in patients preoperatively classified as having clean or clean-contaminated wounds. Patients could have had more than one surgery during the study period, although procedures performed after documentation of a patient's first S. aureus infection were excluded. Infections were attributed to the most recently performed procedure. Procedures associated with a superficial incisional S. aureus SSI or SSI of unknown type were also excluded.
All statistical analyses were performed using SAS software, version 9.1 (SAS Institute, Cary, NC). All statistical tests were 2-tailed, and a P-value of less than 0.05 was considered significant. Incidence rates were calculated as the number of infections per 100 surgical procedures. Nonparametric bootstrapping was used to generate 95% confidence intervals (CIs) for the rates. The proportions of patients with infections due to MRSA were also calculated. Kaplan-Meier analyses were performed to compute the median time between the date of the surgical procedure and the date of onset of infection.
To identify characteristics potentially associated with the development of invasive S. aureus infection, bivariable comparisons were performed between patients who developed an invasive S. aureus infection and those who did not. P-values were calculated using Pearson chi-square tests for categorical variables and the Student’s t-test for continuous variables. This analysis was hypothesis-generating; no adjustment was made for multiple statistical tests, and the results should be interpreted accordingly.
Results
Study population
A total of 13,719 prosthetic knee or hip insertion procedures were performed during the study period; 8,446 (62%) involved the knee and 5,273 (38%) involved the hip. Compared with patients who underwent prosthetic knee insertions, patients who underwent prosthetic hip insertions were more likely to be 60 years of age or older (66% versus 60%, p < 0.0001); to be at community hospitals (60% versus 53%, p < 0.0001); to have clean-contaminated wound class (5% versus 4%, p = 0.0028); and to have more severe disease, ASA scores of 3 or greater (56% versus 50%, p < 0.0001) (Table 1).
Rates and characteristics of invasive S. aureus infection
S. aureus caused 92 (55%) of the 167 post-operative invasive infections. Among the invasive S. aureus infections, SSIs were more common (80%) than SSI and BSI (10%) or BSI alone (10%). Of the 85 post-operative infections in patients undergoing prosthetic knee insertion, 48 (56%) were invasive S. aureus infections, of which 43 were SSIs, 4 were BSIs, and 1 was a combined SSI and BSI. Of 82 total post-operative infections in patients undergoing prosthetic hip insertion, 44 (54%) were invasive S. aureus infections, of which 31 were SSIs, 5 were BSIs, and 8 were combined SSI and BSI (Table 2). The overall rate of invasive S. aureus infection/100 procedures was 0.57 [95% CI: 0.43-0.73] following prosthetic knee insertion and 0.83 [95% CI: 0.61-1.08] following prosthetic hip insertion (p = 0.06). The distribution of S. aureus infection types in prosthetic knee insertion procedures (SSI 90%, BSI 8%, and SSI + BSI 2%) varied significantly from the distribution in prosthetic hip insertion procedures (SSI 70%, BSI 11%, and SSI + BSI 18%), p = 0.02.
MRSA accounted for 53% of S. aureus infections following all procedures, 45% following prosthetic knee insertion and 61% following prosthetic hip insertion (p = 0.11). The median time to onset of invasive S. aureus infection was 28 days for all procedures (interquartile range (IQR): 17–54 days), 34 days (IQR: 18–65 days) for prosthetic knee insertion, and 26 days (IQR: 16–40 days) for prosthetic hip insertion. Using a year surveillance period for SSIs, 18% (8/44) of invasive S. aureus SSIs occurred more than 90 days after prosthetic knee insertions, while all invasive S. aureus SSIs occurred within 90 days after prosthetic hip insertions.
Patients who developed invasive S. aureus infections had higher NHSN risk index scores than did uninfected surgical patients following prosthetic knee insertion (p < 0.0001) and prosthetic hip insertion (p = 0.0001) (Table 3). Patients who developed invasive S. aureus infections also had higher ASA scores and significantly longer surgical procedure durations compared to uninfected patients. Age was not associated with the risk of developing an invasive S. aureus infection.
Discussion
Approximately 1 million primary knee and hip arthroplasty procedures are performed annually in the US. In 2010, for example, 719,000 total knee replacements and 332,000 total hip replacements were performed [10]. The volume of joint arthroplasty procedures is projected to increase substantially in the United States in the coming decades [11]. An important complication of joint arthroplasty procedures is post-surgical infection [12], which is often caused by S. aureus.
The purpose of this analysis was to determine the epidemiology of invasive S. aureus infections following prosthetic knee or hip insertion procedures. We found a slightly higher rate of invasive S. aureus infections in patients receiving prosthetic hip insertions compared to those receiving prosthetic knee insertions (0.83 vs 0.57 per 100 procedures), although the difference was not statistically significant. NHSN risk index score, ASA score, and procedure duration all significantly affected the rates of postoperative staphylococcal infections for both types of prosthetic insertion procedures. In addition, more than half of the S. aureus infections were MRSA infections.
Our results are similar to previously published reports. Rao and colleagues found that the overall SSI rate after total joint arthroplasty at a single institution was 1.1 per 100 procedures, with S. aureus accounting for 53% of SSIs following total knee arthroplasty and 65% of SSIs following total hip arthroplasty [6]. Our results are also consistent with national surveillance rates, in which the deep incisional or organ/space SSI infection rates are reported to range between 0.60 to 2.40 per 100 procedures for prosthetic knee and hip insertions [3], with approximately 50% of these infections attributable to S. aureus and 40% of the S. aureus infections caused by MRSA [5].
The CDC updated the NHSN surveillance definitions for SSIs in January 2013. Prior to 2013, post-operative surveillance for an SSI continued for a year for prosthetic knee or hip insertion procedures [9]. In the new 2013 SSI definitions, the surveillance period for these procedures has been reduced to 90 days [13]. Changing the SSI surveillance definition from 1 year to 90 days results in an 18% decrease in the number of SSI following prosthetic knee insertion procedures in this study. The surveillance definitions used in estimating rates, whether pre- or post-January 2013, will need to be accounted for when interpreting time-trends in SSI rates [14].
Our study has several limitations. First, as with the primary analysis [7], true incidence rates of post-operative S. aureus infections were likely underestimated for the following reasons: superficial incisional SSIs and other invasive infections such as pneumonia were excluded; patients who died before diagnosis of invasive infection were not identified; and infections occurring post-discharge from the hospital may have been under-reported [15]. To minimize the likelihood of missed SSIs, surveillance methods for SSIs at study hospitals included flagging patients for re-admission and surgeon surveys to identify potential SSIs. Since BSIs were identified from the study hospitals’ microbiology databases, only patients with post-discharge BSIs re-admitted to the same study hospital performing the surgical procedure would be detected. In addition, we were unable to determine the source of BSI (e.g., “primary” versus “secondary”). The classification of surgery as elective or emergency was not captured in the surveillance database. We used clean and clean-contaminated wound class as a proxy for elective surgery. Further, patient-level data on antimicrobial prophylaxis prior to surgery were not available. Finally, the generalizability of these findings is limited since (1) all the participating hospitals are located in the southeastern U.S., and (2) the data were collected from 2003–2006, prior to improvements in infection control practices that have resulted in a reduction in MRSA infections nationally since 2006 [16].
Our study has several strengths. The data were from a large, multicenter study using pre-existing, prospectively collected surgical surveillance data for SSI and microbiology data for BSI. The study utilized well-defined methods for classification of SSI according to Centers for Disease Control and Prevention. Finally, we included data from both community and tertiary care hospitals, thereby increasing the generalizability of our results.
The healthcare and economic burden associated with prosthetic joint infections are substantial. Healthcare resource use and cost of care are significantly increased due to longer hospital stays, re-hospitalizations, lengthy antibiotic treatment, further surgery (e.g., debridement, exchange or resection arthroplasty, and amputation), rehabilitation, outpatient and emergency visits. Treatment costs for an infected knee or hip arthroplasty are more than 3 times higher than the costs for primary arthroplasty [17-20]. Assuming an infection rate of 1.0% and a cost of $130,000 per patient, the annual cost to the US healthcare system for the management of SSI after total knee arthroplasty has been estimated at ~ $2 billion [21]. Methicillin-resistant infections result in significantly higher costs of care compared to methicillin-susceptible infections, due to more hospital visits and longer hospital stays [22]. Infectious complications of arthroplasty also negatively impact the patients’ physical functioning and health-related quality of life, which potentially contribute to lost work productivity [2].
Conclusions
We found that patients undergoing hip and knee prosthetic joint surgery are at relatively high risk for S aureus infections. The rates of these infections following joint arthroplasty surgery were similar to the rates following cardiac procedures (0.79 per 100 [95% CI: 0.61-0.97]) and neurosurgical procedures (0.62 per 100 [95% CI: 0.53-0.72]), assessed in the same study population [7]. Moreover, approximately 50% of the infections observed after joint arthroplasty were due to MRSA. Given the poor outcomes and high costs associated with these infections, this patient population represents a good target for interventions to mitigate risk for invasive postoperative S. aureus infections.
References
Poultsides L, Ma Y, Gonzalez Della Valle A, Chiu YL, Sculco TP, Memtsoudis SG. In-hospital surgical site infections after primary hip and knee arthroplasty – incidence and risk factors. J Arthroplasty. 2013;28:385–9.
Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002;23:183–9.
Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, et al. National Healthcare Safety Network (NHSN) report: Data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37:783–805.
Mu Y, Edwards JR, Horan TC, Berrios-Torres SI, Fridkin SK. Improving risk-adjusted measures of surgical site infection for the national healthcare safety network. Infect Control Hosp Epidemiol. 2011;32(10):970–86.
Berrios-Torres SI, Yi SH, Bratzler DW, Ma A, Mu Y, Zhu L, et al. Activity of commonly used antimicrobial prophylaxis regimens against pathogens causing coronary artery bypass graft and arthroplasty surgical site infections in the United States 2006–2009. Infect Control Hosp Epidemiol. 2014;35(3):231–9.
Rao N, Cannella B, Crossett LS, Yates Jr AJ, McGough III R. A preoperative decolonization protocol for staphylococcus aureus prevents orthopaedic infections. Clin Orthop Relat Res. 2008;466:1343–8.
Anderson DJ, Arduino JM, Reed SD, Sexton DJ, Kaye KS, Grussemeyer CA, et al. Variation in the type and frequency of postoperative invasive Staphylococcus aureus infections according to type of surgical procedure. Infect Control Hosp Epidemiol. 2010;31:701–9.
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13:606–8.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32.
FastStats. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/fastats/inpatient-surgery.htm. Accessed June 11, 2014
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5.
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27:61–5.
Centers for Disease Control and Prevention (CDC). Surgical Site Infection (SSI) Event. Atlanta: CDC; 2014. http://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf. Accessed October 2014.
Dicks KV, Lewis SS, Durkin MJ, Baker AW, Moehring RW, Chen LF, et al. Surveying the Surveillance: Surgical Site Infections Excluded by the January 2013 Updated Surveillance Definitions. Infect Control Hosp Epidemiol. 2014;35:570–3.
Yokoe DS, Avery TR, Platt R, Huang SS. Reporting surgical site infections following total hip and knee arthroplasty: impact of limiting surveillance to the operative hospital. Clin Infect Dis. 2013;57:1282–8.
Dantes R, Mu Y, Belflower R, Aragon D, Dumyati G, Harrison LH, et al. National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med. 2013;173:1970–8.
Hebert CK, Williams RE, Levy RS, Barrack RL. Cost of treating an infected total knee replacement. Clin Orthop Relat Res. 1996;331:140–5.
Bozic KJ, Ries MD. The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg. 2005;87A:1746–51.
Klouche S, Sariali E, Mamoudy P. Total hip arthroplasty revision due to infection: a cost analysis approach. Orthop Trauma Surg Res. 2010;96:124–32.
Peel TN, Dowsey MM, Buising IL, Liew D, Choong PFM. Cost analysis of debridement and retention for management of prosthetic joint infection. Clin Microbiol Infect. 2013;19:181–6.
Kapadia BH, Johnson AJ, Issa K, Mont MA. Economic evaluation of chlorhexidine cloths on healthcare costs due to surgical site infections following total knee arthroplasty. J Arthroplasty. 2013;28:1061–5.
Parvizi J, Pawasarat IM, Azzam KA, Joshi A, Hansen EN, Bozic KJ. Periprosthetic joint infection: the economic impact of methicillin-resistant infections. J Arthroplasty. 2010;25(6 Suppl):103–7.
Acknowledgements
We thank Joelle Y. Friedman and Chelsea Grussemeyer (formerly of Duke Clinical Research Institute) and Yong Il Choi (Duke University Medical Center) for their contributions to the primary study and the secondary analysis. Medical writing and editorial assistance were provided by Jennifer Pawlowski and Kim Strohmaier (Merck Sharp & Dohme Corp.).
Funding
The primary analysis and the present secondary analysis were supported by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ.
Dr. Anderson receives research support from NIH/NIAID K23 AI095357 and has received research support from the Robert Wood Johnson Foundation Physician Faculty Scholars program. Dr. Fowler was supported by NIH K24-AI093969.
Dr. Tong was supported by an Australian-American Fulbright Scholarship, a Royal Australian College of Physicians Bayer Australia Medical Research Fellowship, and is an Australian National Health and Medical Research Council Career Development Fellow (1065736).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
D. Anderson has received research support from the AHRQCDC, and the Robert Wood Johnson Foundation.
S. Reed provides full disclosure of current and past funding sources at https://www.dcri.org/about-us/conflict-of-interest.
L. Chen has served as a speaker for Cubist and Optimer and has received research support from Merck.
V. Fowler has served as Chair of V710 Scientific Advisory Committee (Merck), has received grant support from Cerexa, Pfizer, Advanced Liquid Logic, MedImmune, has been a paid consultant for Merck, Astellas, Affinium, Theravance, Cubist, Cerexa, Durata, Pfizer, NovaDigm, Novartis, Medicines Company, Biosynexus, MedImmune, and Inimex, and has received honoraria from Merck, Astellas, Cubist, Pfizer, Theravance, and Novartis.
S. Peter, S. Smugar, and J. Arduino are current or former employees of Merck and may own stock and/or stock options in the company.
D. Sexton, K. Kaye, N. C. Hardy, and S. Tong report no conflicts of interest relevant to this article.
Authors’ contributions
Each author has made substantial contributions to the conception and design, or the acquisition of the data, or the analysis and interpretation of the data; has been involved in drafting the manuscript or revising it critically for important intellectual content; and has given final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Arduino, J.M., Kaye, K.S., Reed, S.D. et al. Staphylococcus aureus infections following knee and hip prosthesis insertion procedures. Antimicrob Resist Infect Control 4, 13 (2015). https://doi.org/10.1186/s13756-015-0057-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-015-0057-4