Abstract
Background
Both preoperative cardiopulmonary exercise test (CPET)-derived measures of fitness and postoperative C-reactive protein (CRP) concentrations are associated with complications following surgery for colorectal cancer. The aim of the present pilot study was to examine the relationship between CPET and postoperative CRP concentrations in this patient group.
Methods
Patients who had undergone CPET prior to elective surgery for histologically confirmed colorectal cancer in a single centre between September 2008 and April 2017 were included. Preoperative VO2 at the anaerobic threshold (AT) and peak exercise were recorded, along with preoperative modified Glasgow Prognostic Score (mGPS) and CRP on each postoperative day.
Results
Thirty-eight patients were included. The majority were male (30, 79%), over 65 years old (30, 79%), with colonic cancer (23, 61%) and node-negative disease (24, 63%). Fourteen patients (37%) had open surgery and 24 (63%) had a laparoscopic resection. A progressive reduction in VO2 at peak exercise was significantly associated with both increasing American Society of Anesthesiology (ASA) grade (median, ml/kg/min: ASA 1 = 22, ASA 2 = 19, ASA 3 = 15, ASA 4 = 12, p = 0.014) and increasing mGPS (median, ml/kg/min: mGPS 0 = 18, mGPS 1 = 16, mGPS 2 = 14, p = 0.039) There was no significant association between either VO2 at the AT or peak exercise and postoperative CRP.
Conclusions
The present pilot study reports a possible association between preoperative CPET-derived measures of exercise tolerance, and the preoperative systemic inflammatory response, but not postoperative CRP in patients undergoing surgery for colorectal cancer.
Similar content being viewed by others
Background
Colorectal cancer is a leading cause of death in the developed world (Cancer Research UK, 2016). Surgery continues to form the mainstay of treatment in the majority of cases; however, there is a significant associated degree of morbidity and mortality (Ghaferi et al., 2011). Long-term survival is primarily dictated by tumour differentiation and stage at presentation; however, it is increasingly recognised that postoperative complications have a significant impact on long-term oncologic outcomes (McSorley et al., 2016a).
Cardiopulmonary exercise testing (CPET/CPX) has been developed as a method of assessing a patient’s ability to meet the increased oxygen demand of major surgery (Older et al., 1993). It represents a dynamic, non-invasive assessment of a patient’s cardiovascular and pulmonary reserve (Smith et al., 2009). Two key measurements relating to oxygen delivery can be derived via CPET; oxygen consumption at the anaerobic threshold (VO2 at AT) which represents the point at which anaerobic metabolism is required in addition to aerobic metabolism to meet tissue energy demand, and oxygen consumption at peak exercise (VO2 at peak). Patients with VO2 at AT < 11 ml/min/kg or VO2 at peak < 19 ml/min/kg are at significant risk of postoperative cardiovascular death and also of surgical complications following major abdominal surgery (Older et al., 1999). Very similar thresholds have also been found to predict the development of postoperative complications in surgery for oesophagogastric cancer (Moyes et al., 2013), in surgery for rectal cancer and colon cancer (West et al., 2014a; West et al., 2014b).
The magnitude of the postoperative systemic inflammatory response is associated with the development of, and severity of, complications following surgery for colorectal cancer (Platt et al., 2012; McSorley et al., 2015). The acute phase reactant C-reactive protein (CRP) has been shown to be a reliable marker of the magnitude of the postoperative systemic inflammatory response (Watt et al., 2015). Indeed, threshold values have been established in the postoperative period which are associated with the development of postoperative complications and the need for investigation (McDermott et al., 2015). The exact mechanism by which poor VO2 at AT and VO2 at peak are linked to the development of postoperative complications is incompletely understood. It may be that poor cardiopulmonary exercise tolerance leads to the development of postoperative complications due to an exaggerated postoperative systemic inflammatory response.
Therefore, the aim of the present pilot study was to investigate the relationship between CPET measurements, the preoperative systemic inflammatory response as measured by the modified Glasgow Prognostic Score (mGPS), the postoperative systemic inflammatory response as evidenced by CRP, and complications following surgery for colorectal cancer.
Methods
Patients
This observational pilot study included patients who had undergone CPET prior to elective surgery for histologically confirmed colorectal cancer in a single centre between September 2008 and April 2017.
All patients received prophylactic antibiotics and venous thromboprophylaxis prior to the induction of anaesthesia as per hospital policy. Further postoperative investigation and intervention was at the discretion of the patient’s surgical team.
Methods
Clinicopathological data was collected prospectively in a database and anonymised. Recorded information included patient demographics, American Society of Anesthesiology (ASA) grade, body mass index (BMI), smoking status, tumour site, TNM stage (TNM, AJCC), surgical approach, preoperative and postoperative serum CRP and albumin measurements. Data regarding the nature, severity and management of complications was retrospectively categorised using the Clavien Dindo scale (Dindo et al., 2004). Any uncertainties were addressed by review of electronic and/or physical case notes. The study was approved by the West of Scotland Research Ethics Committee, Glasgow.
Serum concentrations of CRP (mg/l) were measured using an autoanalyser (Architect; Abbot Diagnostics, Maidenhead, UK) with a lower detectable limit of 0.2 mg/l as was serum albumin (normal range 35-50 g/l). The preoperative modified Glasgow Prognostic Score (mGPS) was calculated from preoperative serum CRP and albumin (McMillan, 2013).
Cardiopulmonary exercise testing was performed in a single respiratory function laboratory using a ZAN 600 (nSpire Health, Hertford, UK) and Ergoselect bicycle ergometer (Ergoline, Bitz, Germany). A doctor and resuscitation equipment were present during all tests. Several variables were recorded including electrocardiography, blood pressure, oxygen uptake and carbon dioxide output from analysis of inspiratory and expiratory gases. Patients were exposed to an incremental physical exercise protocol to their maximally tolerated level which was determined by exhaustion, symptomatic breathlessness or pain. The measured variables along with the exercise protocol allowed VO2 at AT and at peak exercise to be quantified.
Statistical analysis
In addition to being analysed as continuous variables, patients were grouped according to the previously described thresholds of VO2 at AT (< 11 or > 11 ml/min/kg) and at peak exercise (< 19 or > 19 ml/min/kg). Categorical data were compared using the chi-square test or Fisher’s exact test where appropriate. Continuous data are presented as median and range and were compared using the Mann-Whitney U test or Kruskal-Wallis test in multiple groups. Postoperative CRP concentrations were displayed graphically by postoperative day as median and 95% confidence interval. Correlation between VO2 at AT and VO2 at peak exercise and the peak postoperative CRP concentration was assessed using Spearman’s correlation coefficients. Statistical analyses were performed using IBM SPSS version 22 for Windows (Chicago, IL, USA).
Results
Patients
Thirty-eight patients completed CPET prior to elective surgery for colorectal cancer at Glasgow Royal Infirmary between 2008 and 2017 (Table 1). The majority were male (30, 79%), over 65 years old (30, 79%), with colonic cancer (23, 61%) and node-negative disease (24, 63%). Fourteen patients (37%) had open surgery and 24 (63%) had a laparoscopic resection. Prior to surgery, 3 patients with locally advanced or margin threatening rectal cancer underwent neoadjuvant chemoradiotherapy (nCRT); there were no cases of pathological complete response.
Complications
Of the 38 patients, 15 (39%) experienced complications (Table 1). No patients died within 30 days of surgery or during the same admission. Of the patients with complications, 10 (26% of all patients) were infective and 5 (13%) were non-infective. When classified using the Clavien Dindo scale, 12 (32% of all patients) were grade 1 to 2 (i.e. required minor intervention) and 3 (8%) were grade 3 to 4 (i.e. necessitated major intervention).
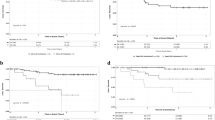
Associations between CPET variables, co-morbidity and mGPS
There was a significant positive correlation (rs = 0.628, p < 0.001) between VO2 at anaerobic threshold (AT) and VO2 at peak exercise. An increasing burden of co-morbidity as measured by ASA grade (Fig. 1) was significantly associated with progressively lower median VO2 at peak exercise (ml/kg/min: ASA 1 = 22, ASA 2 = 19, ASA 3 = 15, ASA 4 = 12, p = 0.014), but not VO2 at AT (p = 0.058).
When VO2 at AT was compared as a continuous variable amongst patients grouped by preoperative mGPS 0, 1 and 2 (Fig. 2), there was no significant association (p = 0.147). When VO2 at peak exercise was compared as a continuous variable amongst patients groups by mGPS 0, 1 and 2 (Fig. 2), higher mGPS was significantly associated with progressively lower median VO2 at peak exercise (ml/kg/min: mGPS 0 = 18, mGPS 1 = 16, mGPS 2 = 14, p = 0.039).
There was a non-significant linear trend toward greater preoperative systemic inflammation in patients with higher ASA grade (p = 0.058).
VO2 at anaerobic threshold and the postoperative SIR
Fourteen patients (37%) had VO2 at AT > 11 ml/min/kg and 24 patients (63%) had VO2 at AT < 11 ml/min/kg (Table 1). When the two groups were compared, there was a significant association between VO2 at AT and ASA grade (p = 0.041). There was no significant association between VO2 at AT and other preoperative characteristics including patient age, sex, BMI, smoking status, tumour site, TNM stage, preoperative mGPS or neoadjuvant treatment (Table 1).
There were no significant associations between VO2 at AT and postoperative complications, established CRP thresholds on postoperative days 3 or 4 (Table 1), or the postoperative CRP trend (Fig. 3). When both VO2 at AT and peak postoperative CRP (day 4) concentrations were compared as continuous variables, there was no significant correlation (p = 0.885).
VO2 at peak exercise and the postoperative SIR
Thirteen patients (34%) had VO2 at peak exercise > 19 ml/min/kg and 25 patients (66%) had VO2 at peak exercise < 19 ml/min/kg (Table 1). When the two groups were compared (Table 1), there was a significant association between VO2 at peak exercise and ASA (p = 0.004). A significantly higher proportion of patients with VO2 at peak exercise < 19 ml/min/kg had an mGPS of 1–2 (41 vs. 8%, p = 0.036). A significantly lower proportion of patients with VO2 at peak exercise < 19 ml/min/kg underwent nCRT (0 vs. 23%, p = 0.034). With regard to intraoperative variables (Table 1), a significantly higher proportion of patients with VO2 at peak exercise < 19 ml/min/kg underwent laparoscopic surgery (84 vs. 23%, p < 0.001).
There was no significant association between VO2 at peak exercise and postoperative complications, established CRP thresholds on postoperative days 3 or 4 (Table 1), or the postoperative CRP trend (Fig. 3). When VO2 at peak exercise and peak postoperative CRP (day 3) concentrations were compared as continuous variables, there was no significant correlation (p = 0.898).
Discussion
The present pilot study confirms the relationship between CPET-derived measures of exercise tolerance and co-morbidity as measures by ASA grade in patients prior to surgery for colorectal cancer. Moreover, the present results show for the first time an inverse relationship between the VO2 at peak exercise and the preoperative systemic inflammatory response. There was no significant association with the magnitude of the postoperative systemic inflammatory response. However, given the small numbers of patients examined, these relationships warrant further investigation.
The neuroendocrine, metabolic and immune responses to surgical trauma lead to an increase in oxygen requirement from baseline usually supplied by increasing tissue oxygen extraction and cardiac output in the postoperative period, with the aim of increasing oxygen delivery (Shoemaker & Czer, 1979). However, not all patients are able to utilise these mechanisms sufficiently to prevent the accrual of an “oxygen debt”, when oxygen delivery is outstripped by tissue oxygen requirement (Waxman et al., 1981). The degree of oxidative stress placed on the patient has been found to be associated with the production of pro-inflammatory cytokines (Rixen & Siegel, 2000). It has been postulated that oxidative stress and resultant tissue hypoxia, especially in the gut, drives a significant proportion of the postoperative systemic inflammatory response (Mainous et al., 1995). Indeed, it is well recognised that tissue hypoxia can lead to activation and augmentation of the innate immune system via hypoxia-inducible factor 1α (HIF-1α) (Peyssonnaux et al., 2005; Nizet & Johnson, 2009). CPET thus uses graded exercise to quantify a given patients’ anaerobic threshold and other measures including VO2 at peak exercise and METs. These CPET variables are associated with postoperative outcomes following abdominal and colorectal surgery (Older et al., 1999; West et al., 2014a; West et al., 2014b).
It was of interest that a significant association was found between VO2 at peak exercise and the preoperative mGPS at the univariate level. It remains unclear whether this relationship is explained by the association between preoperative systemic inflammation and co-morbid state or other effects. Indeed, the preoperative systemic inflammatory response has previously been shown to be directly associated with preoperative co-morbidity in patients undergoing surgery for colorectal cancer (Richards et al., 2010), and it may be this which links mGPS to reduced peak exercise tolerance. This finding was not confirmed by the results of the present study. However, the trend to association between mGPS and ASA was likely non-significant due to patient numbers. Alternatively, systemic inflammation has a key causal role in the development of the cancer cachexia syndrome, with loss of skeletal muscle quantity and quality, and resultant loss of physical function in patients with cancer (McSorley et al., 2017a). It may be that systemic inflammation exerts its influence on exercise tolerance through this mechanism.
Although previous studies in colorectal surgery have reported an association between patients with VO2 at AT < 11 ml/min/kg and VO2 at peak exercise < 19 ml/min/kg and the development of postoperative complications (West et al., 2014a; West et al., 2014b), this was not confirmed in the present study. This is most likely due to the small number of patients in the present study. The magnitude of the postoperative systemic inflammatory response, as evidenced by CRP, is increasingly understood to be associated with the development of postoperative complications following surgery for colorectal cancer (Watt et al., 2017a). These postoperative complications, whether categorised by their type or severity, are associated with poorer long-term oncologic outcomes following surgery for colorectal cancer (McSorley et al., 2016a). Furthermore, studies in surgery for oesophageal, gastric and colorectal cancer suggest that the magnitude of the postoperative systemic inflammatory response is itself a prognostic factor (Matsuda et al., 2015; Saito et al., 2015; McSorley et al., 2016b). Such findings have prompted the investigation of patient and operative factors which influence the postoperative systemic inflammatory response, along with potential methods which might be used to attenuate it, with the aim of reducing postoperative complication rates (Watt et al., 2017b; McSorley et al., 2016c; McSorley et al., 2017b). Indeed, it might be hoped that ongoing studies examining prehabilitation as an intervention to reduce postoperative complication rates may also find an impact on the postoperative systemic inflammatory response.
The main limitation of the present study is the small number of included patients. Preoperative CPET is not routinely used as an evaluation of fitness for colorectal surgery in our unit at present. These small numbers lead to limited ability to make confident statements about the association between CPET, postoperative CRP and complications, and prevented subgroup analysis. Furthermore, the multiple comparisons used in analysis, in the context of the small number of patients, also reduce the confidence in the observed associations or lack thereof.
Conclusions
In conclusion, the present pilot study reports a possible association between preoperative CPET-derived measures of exercise tolerance, and the preoperative systemic inflammatory response in patients undergoing surgery for colorectal cancer. The mGPS may be a surrogate for overall “fitness” in these patients; however, systemic inflammation may well be a causal factor in poor exercise tolerance in this group of patients. No association was found between CPET-derived measures and the magnitude of the postoperative systemic inflammatory response; however, small numbers and the presence of important confounders mean that further work in a larger cohort of patients is warranted.
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- ASA:
-
American Society of Anesthesiology
- AT:
-
Anaerobic threshold
- BMI:
-
Body mass index
- CPET/CPX/CPEX:
-
Cardiopulmonary exercise testing
- CRP:
-
C-reactive protein
- HIF:
-
Hypoxia inducible factor
- MET:
-
Metabolic equivalent
- mGPS:
-
Modified Glasgow Prognostic Score
- nCRT:
-
Neoadjuvant chemoradiotherapy
- TNM:
-
Tumour nodes metastasis staging
- VO2 :
-
Volume of oxygen consumed
References
Cancer Research UK. Bowel cancer statistics. http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer. Accessed Aug 2016.
Dindo D, Demartines N, Clavien P. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Ghaferi LG, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49:1076–81.
Mainous MR, Ertel W, Chaudry IH, et al. The gut: a cytokine-generating organ in systemic inflammation. Shock. 1995;4:193–9.
Matsuda S, Takeuchi H, Kawakubo H, et al. Correlation between intense postoperative inflammatory response and survival of esophageal cancer patients who underwent transthoracic esophagectomy. Ann Surg Oncol. 2015;22(13):4453–60.
McDermott FD, Heeney A, Kelly ME, et al. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg. 2015;102:462–79.
McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–40.
McSorley ST, Black DH, Horgan PG, et al. The relationship between tumour stage, systemic inflammation, body composition and survival in patients with colorectal cancer. Clin Nutr. 2017a. https://doi.org/10.1016/j.clnu.2017.05.017. [Epub ahead of print]
McSorley ST, Horgan PG, McMillan DC. The impact of the type and severity of postoperative complications on long-term outcomes following surgery for colorectal cancer: a systematic review and meta-analysis. Cit Rev Oncol Hematol. 2016a;97:168–77.
McSorley ST, Horgan PG, McMillan DC. The impact of preoperative corticosteroids on the systemic inflammatory response and postoperative complications following surgery for gastrointestinal cancer: a systematic review and meta-analysis. 2016c;101:139–150.
McSorley ST, Ramanathan ML, Horgan PG, et al. Postoperative C-reactive protein measurement predicts the severity of complications following surgery for colorectal cancer. Int J Color Dis. 2015;30(7):913–7.
McSorley ST, Roxburgh CSD, Horgan PG, et al. The impact of preoperative dexamethasone on the magnitude of the postoperative systemic inflammatory response and complications following surgery for colorectal cancer. Ann Surg Oncol. 2017b;24(8):2104–12.
McSorley ST, Watt DG, Horgan PG, et al. Postoperative systemic inflammatory response, complication severity, and survival following surgery for colorectal cancer. Ann Surg Oncol. 2016b;23(9):2832–40.
Moyes LH, McCaffer CJ, Carter RC, et al. Cardiopulmonary exercise testing as a predictor of complications in oesophagogastric cancer surgery. Ann R Coll Surg Engl. 2013;95:125–30.
Nizet V, Johnson RS. Interdependence of hypoxic and innate immune responses. Nat Rev Immunol. 2009;9:609–17.
Older P, Hall A, Hader R. Cardiopulmonary exercise testing as a screening test for perioperative management of major surgery in the elderly. Chest. 1999;116:355–62.
Older P, Smith R, Courtney P, et al. Preoperative evaluation of cardiac failure and ischaemia in elderly patients by cardiopulmonary exercise testing. Chest. 1993;104(3):701–4.
Peyssonnaux C, Datta V, Cramer T. HIF-1 alpha expression regulates the bactericidal activity of phagocytes. J Clin Invest. 2005;115:1806–15.
Platt JJ, Ramanathan ML, Crosbie RA, et al. C-reactive protein as a predictor of postoperative infective complications after curative resection in patients with colorectal cancer. Ann Surg Oncol. 2012;19:4168–77.
Richards CH, Leitch EF, Horgan PG, et al. The relationship between patient physiology, the systemic inflammatory response and survival in patients undergoing curative resection of colorectal cancer. Br J Cancer. 2010;103(9):1356–61.
Rixen D, Siegel JH. Metabolic correlates of oxygen debt predict posttrauma early acute respiratory distress syndrome and the related cytokine response. J Trauma. 2000;49:392–402.
Saito T, Kurokawa Y, Miyazaki Y, et al. Which is a more reliable indicator of survival after gastric cancer surgery: postoperative complication occurrence or C-reactive protein elevation? J Surg Oncol. 2015;112(8):894–9.
Shoemaker WC, Czer LS. Evaluation of the biologic importance of various haemodynamic and oxygen transport variables: which variables should be monitored in postoperative shock? Crit Care Med. 1979;7:424–31.
Smith TB, Stonell C, Purkayastha S, et al. Cardiopulmonary exercise testing as a risk assessment method in non cardiopulmonary surgery: a systematic review. Anaesthesia. 2009;64:883–89365.
Watt DG, Horgan PG, McMillan DC. Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery. 2015;157(2):362–80.
Watt DG, McSorley ST, Park JH, et al. A postoperative systemic inflammatory score predicts short- and long-term outcomes in patients undergoing surgery for colorectal cancer. Ann Surg Oncol. 2017a;24(4):1100–9.
Watt DG, Ramanathan ML, McSorley ST, et al. Clinicopathological determinants of an elevated systemic inflammatory response following elective potentially curative resection for colorectal cancer. Ann Surg Oncol. 2017b;24(9):2588–94.
Waxman K, Lazrove S, Shoemaker WC. Physiologic responses to operation in high risk surgical patients. Surg Gynecol Obstet. 1981;152:633–8.
West MA, Lythgoe D, Barben CP, et al. Cardiopulmonary exercise variables are associated with postoperative morbidity after major colonic surgery: a prospective blinded observational study. Br J Anaesthesia. 2014b;112(4):665–71.
West MA, Parry MG, Lythgoe D, et al. Cardiopulmonary exercise testing for the prediction of complications after rectal cancer surgery. Br J Surg. 2014a;101:1166–72.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to the small number of patients included and therefore the possibility that a patient may be identified even from otherwise anonymised data. Limited data are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
STM, CSDR, PGH and DCM are responsible for the study conception and design. STM, CSDR are responsible for the acquisition of data. STM and DCM are responsible for the analysis and interpretation of data. STM, PGH and DCM contributed to the drafting of the manuscript. STM, CSDR, PGH and DCM contributed to the critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved with the need for individual patient consent waived by the West of Scotland research ethics committee due to its retrospective observational nature.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
McSorley, S.T., Roxburgh, C.S.D., Horgan, P.G. et al. The relationship between cardiopulmonary exercise test variables, the systemic inflammatory response, and complications following surgery for colorectal cancer. Perioper Med 7, 11 (2018). https://doi.org/10.1186/s13741-018-0093-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13741-018-0093-8