Abstract
Background
Enhanced recovery may be viewed as a comprehensive approach to improving meaningful outcomes in patients undergoing major surgery. Evidence to support enhanced recovery pathways (ERPs) is strong in patients undergoing colorectal surgery. There is some controversy about the adoption of specific elements in enhanced recovery “bundles” because the relative importance of different components of ERPs is hard to discern (a consequence of multiple simultaneous changes in clinical practice when ERPs are initiated). There is evidence that specific approaches to fluid management are better than alternatives in patients undergoing colorectal surgery; however, several specific questions remain.
Methods
In the “Perioperative Quality Initiative (POQI) Fluids” workgroup, we developed a framework broadly applicable to the perioperative management of intravenous fluid therapy in patients undergoing elective colorectal surgery within an ERP.
Discussion
We discussed aspects of ERPs that impact fluid management and made recommendations or suggestions on topics such as bowel preparation; preoperative oral hydration; intraoperative fluid therapy with and without devices for goal-directed fluid therapy; and type of fluid.
Similar content being viewed by others
Consensus statements
Prior to surgery
-
1.
We recommend unrestricted access to clear fluids for oral intake up to 2 h before the induction of anesthesia to maintain hydration while minimizing the risk of aspiration.
-
2.
We recommend that the clear fluid used to maintain oral hydration contain at least 45 g of carbohydrate to improve insulin sensitivity (except in type I diabetics due to their insulin deficiency state). We suggest that complex carbohydrate (e.g., maltodextrin) be used when available.
-
3.
We recommend that clinicians avoid administration of intravenous fluids to replace preoperative “fluid losses” in patients who received iso-osmotic bowel preparation provided there was unrestricted intake of clear fluids for up to 2 h before the induction of anesthesia. There is no evidence that iso-osmotic mechanical bowel preparation leads to adverse effects on preoperative volume status.
-
4.
We recommend against the use of hyper-osmotic or hypo-osmotic bowel preparations prior to surgery since there is no benefit relative to iso-osmotic bowel preparation and there may be adverse effects on preoperative volume status.
During and after surgery
-
5.
We recommend the application of a hemodynamic framework to guide clinical decision-making during surgery. We have developed such a framework and suggest that the use of intraoperative goal-directed fluid therapy (GDFT) is likely to be safe in the majority of patients undergoing major colorectal surgery. GDFT has little risk, and the use of advanced hemodynamic monitoring equipment may enhance clinical decision-making when compared with the use of conventional monitors.
-
6.
We suggest that the advanced hemodynamic monitoring equipment used to guide clinical decision-making intraoperatively be selected based on a combination of surgical patient and institutional factors since such monitoring can minimize both hypovolemia (by promoting therapy in volume responders) and hypervolemia (by restricting therapy in non-responders).
-
7.
We recommend that in isolation, intraoperative oliguria should not trigger fluid therapy, as low urine output is a normal physiologic response during surgery and anesthesia. We also recommend that intraoperative oliguria be investigated and that absolute (as opposed to relative) hypovolemia be ruled out.
-
8.
We recommend that intraoperative and postoperative anuria warrant immediate attention since anuria is pathological.
-
9.
We recommend that fluid management strategies focus on the following: first, identifying if there is a clinical problem that can be solved by fluid therapy and then identifying what fluid and how much is appropriate. Rather than treating every instance of abnormal hemodynamic values (displayed by conventional or advanced monitors), clinicians must establish causation based on available information about the patient and clinical context.
-
10.
We recommend that therapy attempt to reverse the most likely cause of a hemodynamic derangement. Absolute hypovolemia may or may not be responsible for observed hemodynamic abnormalities. For instance, stroke volume variation above 13% soon after the induction of anesthesia and with the institution of mechanical ventilation should prompt consideration of vasodilation (relative hypovolemia) rather than as the cause of fluid responsiveness. The patient may hence require vasoconstrictors rather than bolus fluid therapy provided clear fluids have been consumed preoperatively and iso-osmotic bowel preparation has been used.
-
11.
We recommend the use of buffered isotonic crystalloids for the treatment of hypovolemia in patients undergoing colorectal surgical procedures. We acknowledge that the restrictions on the use of starch solutions are based on extrapolations from the critical care literature.
-
12.
We suggest that patients tolerating fluids orally after surgery be given unrestricted access to such fluids as this increases patient satisfaction and as it is likely that intravenous fluid administration offer no added benefit.
-
13.
We suggest that the hemodynamic framework utilized intraoperatively be extended into the postoperative period to the extent possible, in situations where patients might benefit from such postoperative monitoring (high-risk patients or those with significant blood loss or complications during surgery).
Background
Outcomes such as complication rates, readmissions, and length of stay may be highly variable across different centers conducting colorectal surgery (Cohen et al. 2009). Enhanced recovery pathways (ERPs), initially led in Europe (by the surgeon Henrik Kehlet), were developed in the 1990s in an effort to reduce such variability (Kehlet 1997). ERPs generally share certain core features but also have subtle differences across and even within sites (reflecting unique institutional needs, capabilities, and resource availability). Most ERPs focus on setting patient expectations and involving the patient in their own care pathway for fast recovery, avoiding prolonged preoperative restriction of fluid intake, avoidance of empirical intravenous fluid loading, minimization of systemic opioid use, and early postoperative ambulation. In several studies examining effects of ERP implementation (versus data prior to implementation), an average reduction in length of stay of 3 days appeared to result in over 3000 subjects across several institutions and in a variety of surgical procedures (Thiele et al. 2015a). Meta-analyses on ERPs in colorectal surgical procedures found similar reductions in length of stay (~2.5 days) without an increase in readmission rates (Zhuang et al. 2013; Varadhan et al. 2010).
Retrospective and prospective studies of ERPs in colorectal surgery have typically examined “bundled” interventions making it difficult to estimate the relative value of specific elements related to perioperative fluid management. Outside the context of an ERP, investigators have defined outcomes following “liberal” and “restrictive” fluid strategies during colorectal surgery. However, there is no shared definition of what amount constitutes either (Chappell et al. 2008). Calculations of intraoperative fluid deficits during colorectal surgery have, prior to ERP, included so-called “third space” losses and perioperative fluid therapy was guided by static indicators of volume status. A recent comprehensive review summarized this as follows: “Research suffers from a lack of standardization…Investigators have normally named their traditional regimen the standard group and compared it with their own restrictive ideas… A restrictive regimen in one study is often designated as liberal in another setup…This shortcoming prevents even promising results from impacting daily clinical routine and makes any pooling of the data impossible.” (Chappell et al. 2008) Thus, several specific questions, related to fluid therapy, remain. The “fluids” subgroup within the first Perioperative Quality Initiative (POQI) sought to define and answer important questions related to perioperative fluid management in patients undergoing colorectal surgery within the context of an ERP.
Methods/design
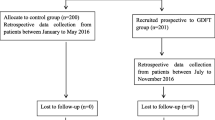
Applying a modified Delphi method, designed to use the collective expertise of a diverse group of experts to answer clinical questions, we achieved consensus on several topics related to perioperative fluid management in patients undergoing colorectal surgery within the context of an ERP.
Expert group
An international group of authorities, with specific content area expertise (based on the conduct of research and education in this area), was invited to participate. In total, 32 experts from around North America and Europe met in Durham, NC, on March 4–5, 2016, to iteratively discuss the evidence supporting enhanced recovery paradigms and develop consensus statements with practical recommendations for clinicians.
Process
A list of relevant questions was collectively developed and circulated electronically prior to the meeting. Based on literature searches performed by members, questions were formulated. In the first plenary session, the POQI perioperative fluid management subgroup presented these questions to the entire POQI workgroup, to receive feedback and assistance in refining the questions. The subgroup then worked together to formulate answers to these questions, supported by evidence when available and by expert opinion when no clear evidence was available. These were presented in the second plenary session. After receiving feedback, the subgroup refined a series of consensus statements, which was then reviewed with and modified by the entire POQI group in the final plenary session. This manuscript is based on these multiple rounds of feedback from all the experts present at the first POQI meeting.
Results
Based on both discussions (held prior to the conference) and the literature (identified by the participants), the following questions were considered most relevant to perioperative fluid management before, during, and after colorectal surgery within an ERP:
Prior to surgery
-
(i)
What are the effects of preoperative oral intake of clear solutions (containing complex versus simple carbohydrates) up to 2 h prior to the induction of anesthesia?
-
(ii)
Does mechanical bowel preparation contribute to preoperative hypovolemia?
During and after surgery
-
(iii)
Is urine output a valid indicator of perioperative fluid needs?
-
(iv)
Is there a rational approach to intraoperative fluid management based on the current evidence?
-
(v)
Which types of fluids should be used intraoperatively?
-
(vi)
How do variations in surgical and anesthesia technique affect intraoperative fluid management?
-
(vii)
How should fluid therapy be managed postoperatively?
(i) What are the effects of preoperative oral intake of clear solutions (containing complex versus simple carbohydrates) up to 2 h prior to the induction of anesthesia?
It has known that both simple (e.g., glucose) and complex (e.g., maltodextrin) carbohydrate-containing solutions prevent protein catabolism following exercise (Borsheim et al. 2004; Roy et al. 1997). Whether this is true in the perioperative period has not, until recently, been known. In animals, oral maltodextrin solution prior to sham surgery reduces protein catabolism versus fasting (with ad libitum water) (Luttikhold et al. 2013). A trial comparing a high to low maltodextrin beverages before surgery found stable post-surgical protein balance in the high but negative whole-body protein balance in the low group (Svanfeldt et al. 2007). Such data suggest that preoperative oral intake of clear solutions containing certain carbohydrates may prevent perioperative protein catabolism. Larger studies are needed to better examine impact on meaningful clinical outcomes such as length of stay or surgical complications. In a recent Cochrane Review including 1976 participants in 27 trials comparing preoperative carbohydrate loading with placebo, where preoperative carbohydrate loading was defined as the intake of at least 45 g of carbohydrates within 4 h prior to surgery, a trend towards improved postoperative insulin resistance was demonstrated (as measured by the Homeostatic Model Assessment of Insulin Resistance (HOMA-IR)) (Smith et al. 2014). On the other hand, a different meta-analysis showed that although there was a tendency toward reduction of postoperative insulin resistance, preoperative carbohydrate loading made no difference to the rates of postoperative complications (Awad et al. 2013).
In non-diabetic colectomy patients, it appears that upwards of 25% are at risk for postoperative hyperglycemia with associated risks of SSI and mortality, presumably from acute insulin resistance (Kwon et al. 2013). Measuring insulin sensitivity with the hyperinsulinemic euglycemic clamp method, carbohydrate loading (as compared with placebo or fasting) demonstrated a trend towards increased postoperative insulin sensitivity (sensitivity difference 0.24 to 1.29, p = 0.0046) (Smith et al. 2014). Additionally, Cochrane analysis identified a reduction in length of stay of 0.30 days with carbohydrate loading versus fasting but not versus placebo (−0.12 days, 95% confidence interval −0.38 to 0.12 days) (Smith et al. 2014). Much (but not all) of the data on preoperative carbohydrate loading was based on the use of maltodextrin-containing solutions. Direct comparisons with more readily available simple sugar containing solutions (e.g., glucose) have not been made. However, there are significant data suggesting the negative impact of a high versus low glycemic index meal on the response of glucose, insulin, and glucagon (Harbis et al. 2004).
Overall, based on the low risk of harm, potentially improved nitrogen balance, and better insulin sensitivity following colorectal surgery, we recommend the oral intake of carbohydrate-containing solutions prior to surgery and suggest that solutions containing complex carbohydrates be used when available. We acknowledge that cost and convenience may be barriers to the use of such solutions. It is worth noting that in patients with type I diabetes, provision of such solutions may offer no benefit over electrolyte-containing water with the possible exception of improved nitrogen balance. Lastly, in order to minimize potential risks of aspiration, as detailed in the guidelines issued by the American Society of Anesthesiologists (ASA), the oral intake of clear liquids should occur more than 2 h prior to the induction of anesthesia. ASA guidelines recommend modification of preoperative fasting on an individual basis in the presence of “gastroesophageal reflux disease, dysphagia symptoms, or other gastrointestinal motility disorders.” (American Society of Anesthesiologists C 2011)
(ii) Does mechanical bowel preparation contribute to preoperative hypovolemia?
The traditional view, that mechanical bowel preparation (MBP) may lead to hypovolemia due to gastrointestinal losses prior to colorectal surgery, was supported by a study comparing ten subjects randomized to Picolax (magnesium citrate (a hyper-osmotic laxative) and sodium picosulfate (a stimulant)) versus not. There was significantly more orthostasis and tachycardia in the group that received the hyper-osmotic bowel preparation (Barker et al. 1992). In a subsequent trial comparing 41 patients receiving Picolax randomized to oral intake and protocoled intravenous fluid administration versus oral intake alone, there was more weight loss, hemoconcentration, and orthostasis (a highly specific, but relatively insensitive marker for hypovolemia and fluid responsiveness) in the group receiving no intravenous fluid (Sanders et al. 2001). Similar investigations on hyper-osmotic MBP with bisacodyl, sodium phosphate, and metoclopramide, followed by prespecified fluid intake over 3 days (in 12 healthy volunteers) revealed a median weight loss of 1.2 kg, decrease in exercise tolerance (median 9% reduction in watts), but no changes in orthostasis (Holte et al. 2004). The small sizes of these studies, relative health of the volunteers, and the lack of surgery make it challenging to interpret these data, although weight loss (presumably due to fluid losses from the gastrointestinal tract) is incontrovertible.
In a clinical study of 19 patients undergoing laparoscopic colonic surgery after MBP (bisacodyl, polyethylene glycol 24 h preoperatively), the mean cardiac index was 2.66 L/m2 (normal range 3.5–5) based on transpulmonary thermodilution, after induction of anesthesia. The authors concluded that hypovolemia was likely to be present (Junghans et al. 2006). Unfortunately, the lack of control comparators makes attribution of changes in cardiac index to MBP difficult. The effects of induction of general anesthesia cannot be controlled for. In a meta-analysis of prospective trials studying MBP for colorectal surgery examining the risk of “cardiac events,” MBP was associated with an increased incidence of such events (2.9 versus 4.6% among 2472 patients included in the meta-analysis) (Gravante et al. 2008).
Modern MBP techniques typically utilize iso-osmotic agents, which in theory do not produce dehydration (no osmotic shift in fluids toward the bowel lumen). When combined with the emphasis on intake of clear fluids up to 2 h before surgery (see question i) in compliance with the ASA Fasting Guidelines, concerns related to the impact of MBP on volume status are minimal. There is no need for fluid therapy to treat presumed fluid losses from iso-osmotic MBP and starvation. The shift in practice away from empiric administration of fluid therapy toward therapy based on the detection of “fluid responsiveness” (defined as a specified increase in cardiac output following fluid administration, typically at least by 10%) has further diminished arbitrary preoperative intravenous hydration. If clinicians are able to rapidly identify hypovolemia intraoperatively, excessive preoperative fluid losses can be detected and managed objectively. Since it has not been established that iso-osmotic MBP predisposes patients to hypovolemia, and since clinicians can identify patients in whom MBP might have produced excessive fluid losses promptly (utilizing methods such as respiratory variation in the plethysmography preoperatively (Tsuchiya et al. 2010), we recommend against empiric pre-emptive intravenous fluid therapy to correct MBP-induced hypovolemia. In summary, while some data have previously suggested that hyper-osmotic MBP leads to dehydration before surgery (with increased risk of perioperative adverse cardiac events), there is no evidence that iso-osmotic MBP leads to any hemodynamic perturbations or increased cardiac risk among patients allowed unrestricted access to clear fluids for oral intake prior to surgery.
(iii) Is urine output a valid indicator of perioperative fluid needs?
Traditionally, urine output has been viewed as an indicator of the adequacy of kidney perfusion. Anuria is abnormal and should always be a cause for concern warranting prompt investigation. However, oliguria, defined as urine output less than 0.5 mL/kg/h by the Kidney Disease: Improving Global Outcomes (KDIGO) group, is more challenging to interpret as abnormal, especially when other indicators of overall tissue perfusion are normal (Section 2: AKI Definition. Kidney Int Suppl 2012).
For instance, it is now understood that the release of vasopressin (antidiuretic hormone) is a natural response to anesthesia and surgery. The resorptive actions of vasopressin on the collecting duct in nephrons lead to the retention of water with accompanying oliguria—this may not indicate organ dysfunction (Cochrane et al. 1981). In 1984, a study from the Cleveland Clinic cast doubt on the utility of perioperative oliguria as an indicator of tissue hypoperfusion requiring fluid therapy. Among 137 patients undergoing aortic reconstruction surgery, mean intraoperative urine output or lowest intraoperative urine output had no relationship to changes in postoperative BUN or creatinine levels (Alpert et al. 1984). More recently, in a meta-analysis (of 1594 patients across 15 studies) examining whether intraoperative fluid restriction leads to perioperative acute kidney injury (AKI), there was a trend towards oliguria (OR 2.07, 95% CI 0.97 to 4.44) but there was no difference in the incidence of AKI (OR 1.07, 95% CI 0.60 to 1.92) (Egal et al. 2016a). Further support for the insensitivity of oliguria is provided by analysis of 1444 cases where the administration of less than or equal to 3 mL/kg/h of crystalloid during surgery was not associated with the development of AKI (Ahn et al. 2016). This study also found no difference in rates of oliguria and intraoperative urine output among patients that developed AKI versus those that did not (Ahn et al. 2016).
In contrast, there are data suggesting that high volumes of postoperative urine may indicate recovery and predict early readiness for discharge among patients undergoing colorectal surgery (Johnson et al. 2015). In order to study the effect of forced diuresis, Egal et al. analyzed the impact of oliguria reversal (i.e., targeting a specific urine output) on outcomes in a heterogenous population of 4825 patients in 28 studies undergoing GDFT. They found that while GDFT algorithms with a specific urine target did not reduce AKI compared to conventional fluid management (CFM) but that GDFT algorithms that ignored urine output did (Egal et al. 2016b). Additionally, there is some evidence in cardiac surgical patients that the administration of furosemide (presumably to reverse oliguria) leads to increased serum creatinine (Lassnigg et al. 2000). Such data suggest that while anuria is abnormal, oliguria is a normal “stress” response to surgery even conferring some clinical benefit. There are also data suggesting that the reversal of oliguria either attenuates the potential benefits of protocolized hemodynamic management strategies or even causes harm (Egal et al. 2016b). While much of this data—on urine output and renal function—comes from patients undergoing non-colorectal procedures (and in some cases, non-surgical patients), there are no prospective, randomized controlled trials comparing oliguria reversal (forced diuresis) to more conventional management in patients undergoing colorectal surgery. There is no evidence that urine output is a valid indicator of a need for fluid therapy in patients undergoing colorectal surgery. We recommend that low urine output, as an isolated abnormality, should not trigger fluid therapy and should trigger diagnostic efforts.
(iv) Is there a rational approach to intraoperative fluid management based on the current evidence?
Minimally invasive devices, that reflect cardiac output in real time without pulmonary artery catheterization, have allowed the perioperative measurement of global blood flow. Fluid therapy guided by such devices may thus be based on “fluid responsiveness” where repeated administration of fluid boluses occurs when patients “respond” to fluids (by objectively increasing global blood flow). Minimally invasive cardiac output monitoring-guided fluid management has been studied in multiple randomized controlled trials in patients undergoing diverse procedures (Sinclair et al. 1997; Gan et al. 2002; Venn et al. 2002; Wakeling et al. 2005; Noblett et al. 2006; Chytra et al. 2007; Pillai et al. 2011; Jones et al. 2013; Ni et al. 2013), including abdominal surgery. The sum of these studies suggest that application of minimally invasive cardiac output monitoring can reduce the length of stay (Sinclair et al. 1997; Gan et al. 2002; Venn et al. 2002; Wakeling et al. 2005; Noblett et al. 2006; Chytra et al. 2007; Pillai et al. 2011; Jones et al. 2013; Ni et al. 2013).
Brandstrup et al. offered an alternative to perioperative minimally invasive cardiac output monitoring, by demonstrating that a “zero-fluid balance” approach was as effective in terms of length of stay as well as incident complications (Brandstrup et al. 2003). How could it be that the initial GDFT studies, as conducted by Gan et al., suggested significant benefit with minimally invasive cardiac output monitoring (reduced length of stay), but that more recent studies show that similar benefits can be accrued by paying meticulous attention to avoiding fluid overload and maintaining “zero balance” (without the use of additional devices) (Gan et al. 2002; Brandstrup et al. 2003)? These apparently “conflicting” results may be reconciled by understanding that clinical trials examine outcomes relative to a comparator group. Depending on the fluid management strategies in this control group, achieving near-maximal stroke volume with a GDFT approach either offers an advantage (when the alternative is empirically “liberal” therapy) or is equivalent (when the alternative is “restrictive”) (Chappell et al. 2008). Thus, a rational interpretation of evidence is that there is potential benefit from GDFT using minimally invasive cardiac output monitoring devices by both avoiding unnecessary fluid therapy in volume non-responders and avoiding inadequate fluid therapy and hypoperfusion in volume responders (Bellamy’s conceptual model for keeping patients “optimized”) (Bellamy 2006).
There is little evidence that GDFT poses significant risk. The concern regarding widespread implementation is cost(s). Several investigators have examined device-guided GDFT in the modern era of ERPs. Three such groups independently tested a “zero balance” or “restrictive” strategy against conventional minimally invasive cardiac output monitoring -guided GDFT within the context of colorectal ERPs, and all found no difference in the length of stay or incident complications (335 total subjects studied) (Brandstrup et al. 2012; Srinivasa et al. 2013; Phan et al. 2014). None of these studies showed harm from GDFT. Analyzing the economic impact of esophageal Doppler-based GDFT in major abdominal surgery, but the National Institute for Health and Care Excellence (NICE) Group said that there is “cost saving per patient … when compared with the use of a central venous catheter in the perioperative period” (Excellence NIfHaC 2011). Since minimally invasive cardiac output monitoring devices are not universally used in the perioperative period, we developed a generalizable framework for perioperative fluid management incorporating such devices (Fig. 1) (Cannesson et al. 2011). Our framework does not suggest use of an algorithmic protocol (based on measures of cardiac output or surrogates) for all patients undergoing colorectal surgery; rather, we suggest that device-derived measures be placed in clinical context. For instance, fluid responsiveness rather than prompting a fluid bolus at all times may only prompt a fluid bolus when coupled with evidence of absolute hypovolemia. Abnormal physiologic values may be warning signs (not endpoints for fluid therapy), and clinical decision-making can be supplemented not replaced by the use of advanced hemodynamic monitoring devices (details are beyond the scope of this review but are discussed elsewhere) (Thiele et al. 2015b). Since intraoperative GDFT data suggests either a reduction in length of stay and complications or equipoise (albeit at higher overall cost) and also because most devices used for GDFT present minimal risk to the patient, we recommend the use of GDFT when available. We acknowledge that within ERPs for colorectal surgery, a “zero balance” approach appears to be an acceptable alternative; we do not recommend a simple “recipe book” fluid restriction (e.g., X ml/kg/hr) (Brandstrup et al. 2012; Srinivasa et al. 2013; Phan et al. 2014). This statement is supported by meta-analysis on GDFT within ER protocols (Rollins and Lobo 2016). The most benefit from GDFT is likely in certain subsets of patients rather than all patients undergoing colorectal surgery with ERPs. Depending on patient- and procedure-specific risks, clinicians may utilize conventional monitors or minimally invasive cardiac output monitoring devices (Fig. 2). Frameworks for three different risk categories are presented in Fig. 3.
(v) Which fluids should be used intraoperatively?
Most intraoperative GDFT studies used colloids as the fluid of choice for volume expansion. However, colloids were also administered in the control arms of such trials thereby making it impossible to tease out the impact of colloid solutions alone (Egal et al. 2016a). It is reasonable to conclude that if colloids are going to be used, then a GDFT approach offers benefits. On the other hand, it is unclear that colloids are necessary. In a trial randomizing patients undergoing laparoscopic segmental colectomy within the context of an established ERP to three groups (with all groups receiving lactated Ringer’s at 5 mL/kg/h during the surgical procedure and anesthesia): standard fluid therapy (22 patients) versus intraoperative GDFT with lactated Ringer’s (21 patients) versus intraoperative GDFT with hetastarch (21 patients), the length of stay was longer in the GDFT groups. Furthermore, the group randomized to GDFT with lactated Ringer’s solution received the highest amount of intraoperative fluids while the group randomized to GDFT with hetastarch received the highest amount of fluids during hospitalization (Senagore et al. 2009). Yates et al. randomized 202 medium to high-risk patients undergoing colorectal surgery to receipt of a background infusion of crystalloid during the surgical procedure (1.5 mL/kg/h of Hartmann’s solution) and hemodynamic optimization (GDFT) with either Hartmann’s solution (chloride-restrictive crystalloid solution) or 6% HES (130/0.4, Volulyte, suspended in similar solution). The results showed that there was no difference in complication rates, although the crystalloid group received more fluid than the colloid group (Yates et al. 2014). Unfortunately, there are no large, multicenter, prospective randomized controlled trials comparing crystalloid to colloid solutions intraoperatively in a GDFT protocol. Thus, when making determinations about which fluid types are most appropriate intraoperatively, clinicians are faced with either applying the results of these two small, single center trials, or extrapolating data from large crystalloid-colloid trials in unrelated populations (e.g., sepsis).
Two such trials—comparing human-derived colloids (albumin) to crystalloid in critically ill patients—found no difference in the primary outcome of 28-day mortality (Finfer et al. 2004; Caironi et al. 2014). Three trials—comparing synthetic colloids (hydroxyethyl starch solutions) to crystalloids in critically ill patients—found either an increased risk of death or an increased use of renal replacement therapy (Brunkhorst et al. 2008; Perner et al. 2012; Myburgh et al. 2012). However, synthetic colloids appeared beneficial (in terms of better survival) in an open-label trial of critically ill hypovolemic patients (Annane et al. 2013). A meta-analysis (59 randomized controlled trials with a total of 16,889 subjects) comparing crystalloids with colloids in a variety of patient populations concluded that synthetic colloids were associated with a risk of AKI and need for renal replacement therapy. Of note, subgroup analysis showed that risks were largely in patients with sepsis. General restrictions on the perioperative use of colloids are not supported by this evidence, but no sustained clinical benefits were evident with colloid use (Qureshi et al. 2016).
We therefore recommend the use of crystalloids for the treatment of hypovolemia in patients undergoing colorectal surgical procedures. We acknowledge that albumin may be safe but is more costly. We suggest that isotonic chloride-restrictive crystalloids be used based on a large body of retrospective data (Raghunathan et al. 2015; Shaw et al. 2015; Shaw et al. 2012) and some prospective trials (Shaw et al. 2015; Shaw et al. 2012). The biologic basis for such use (of chloride-restrictive buffered crystalloids over chloride-liberal solutions such as isotonic saline) is related to increased risk of hyperchloremic acidosis with the adverse pathophysiological and clinical outcomes when saline is used (Disma et al. 2014; Potura et al. 2015; Chowdhury et al. 2012; McCluskey et al. 2013; Krajewski et al. 2015; Lobo and Awad 2014). A detailed discussion of blood products is beyond the scope of this manuscript. However, we note that red blood cells have the potential for harm and blood loss should be replaced with blood products only when the risks are justified by significant anemia (Hebert et al. 1999; Hajjar et al. 2010; Carson et al. 2011).
(vi) How do variations in surgical and anesthesia technique affect intraoperative fluid management?
The administration of fluid therapy intraoperatively depends on demonstrable “fluid responsiveness” (i.e., objective evidence that fluid therapy augments circulation). Several surgical maneuvers (e.g., Trendelenberg positioning, insufflation of the peritoneum for laparoscopy) as well as by anesthetic interventions (low tidal volume ventilation, use of positive end expiratory pressure (PEEP), utilization of thoracic epidural analgesia with local anesthetics) may impact measures of “fluid responsiveness.” Understanding the physiologic implications of these maneuvers can help clinicians contextualize changes in device-based measures and avoid the use of fluid therapy based only on the presence of “fluid responsiveness” without attendant absolute hypovolemia.
Trendelenberg positioning
While Trendelenberg (“head down”) positioning has been used for over a century in an effort to improve hemodynamics by augmenting venous return, its intraoperative use is primarily for better visualization of the operative site. Immediately after placing a patient in the head down position, there is a transient increase in right ventricular preload and stroke volume from increased venous blood flow (from the lower extremities and unstressed compartments). This subsequently leads to increased left ventricular output and cardiac output measurements taken 3–5 min after initiating the head down position show an increase in cardiac index (Sibbald et al. 1979). However, these changes are transient, as there is re-equilibration over time (Magder et al. 2009) and global flow returns to baseline within 10–15 min (Ostrow et al. 1994). Thus, we recommend that clinicians avoid assuming that head down positioning has a sustained benefit (long-term increase in preload) with durable improvement in intraoperative hemodynamics.
Laparoscopy
Peritoneal insufflation is particularly relevant in patients undergoing colorectal surgery within ERPs, since minimally invasive surgical techniques are a cornerstone of enhancing recovery. As with positioning, hemodynamic changes with the initiation of laparoscopy are transient. For instance, 5 min after initiation of a 14 mmHg pneumoperitoneum, cardiac index is significantly less than immediately prior to abdominal insufflation. However, 10 min later, there is a return to baseline (Joris et al. 1993). A recent analysis of laparoscopy to an intrabdominal pressure of 14 mmHg confirmed these findings (Alfonsi et al. 2006). It is important for clinicians to note that there is a sustained increase in mean arterial pressure with insufflation. Hence, while the shifts in blood volume (between stressed and unstressed compartments) are transient, the increased afterload (hypertension) is sustained (Joris et al. 1993; Alfonsi et al. 2006; Liu et al. 2015).
Insufflation increases the absolute value of measures such as stroke volume variation and plethysmography (Liu et al. 2015), meeting the threshold defining of “fluid responsiveness.” This does not imply that fluid therapy is needed (as discussed in question iv above) (Guinot et al. 2014). Clinicians should anticipate increases in blood pressure with minimal overall sustained changes in cardiac output (with insufflation to 14 mmHg or less). We suggest that measures of fluid responsiveness (based on cardiorespiratory interactions) are less specific after abdominal insufflation. This increase in “false positives” needs to be accounted—contextualized—as suggested in the framework we have described.
Low tidal volume
Lower tidal volumes confer a mortality benefit to critically ill patients with acute respiratory distress syndrome (ARDS) (Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000). The concept of “lung protective ventilation” has expanded into the operating room environment and may improve outcomes in patients (Lellouche et al. 2012; Futier et al. 2013; Severgnini et al. 2013). As cardiorespiratory interactions depend on cyclic changes in intrathoracic pressure producing corresponding cyclic changes in venous return, thresholds for “fluid responsiveness” that utilize respiratory variation in pulse pressure or systolic pressure are conditional on tidal volumes of 8–12 mL/kg (predicted body weight (PBW)) (Tavernier et al. 1998; Kramer et al. 2004). Lower tidal volumes thus increase “false negatives” decreasing arterial respiratory variation based measures of “fluid responsiveness” (Lansdorp et al. 2012; De Backer et al. 2005; Suehiro & Okutani 2011; Reuter et al. 2003). Of note, clinical trials which use respiratory variation to guide fluid management utilize tidal volumes on average of 7.8 mL/kg (range 6–9.1 mL/kg) (Benes et al. 2010; Forget et al. 2010; Ramsingh et al. 2013; Goepfert et al. 2013). We recommend that clinicians utilizing arterial (or plethysmographic) respiratory variation as a guide to “fluid responsiveness” expect a reduction in sensitivity with low tidal volume ventilation. Approaches that do not rely on such respiratory variation, such as measured response to a fluid bolus (e.g., mini-fluid challenge (Wu et al. 2014; Muller et al. 2011)), are not affected.
High positive end expiratory pressure
Intraoperative mechanical ventilation may now incorporate PEEP (e.g., 6–8 cm H2O utilized by Futier et al.) (Futier et al. 2013). Such PEEP has a hemodynamic impact as a result of increase in intrathoracic pressure (with impedance of venous return) and a decrease in left ventricular afterload (increasing the cardiac index). The overall effect is a balance between these. In general, it appears that PEEP above 5–10 cm H2O, leads to a decrease in cardiac index (Van Trigt et al. 1982; Terai et al. 1985; Huemer et al. 1994). Both animal and human data suggest that such decreases in cardiac index accompanying higher levels of PEEP can be reversed with fluid administration (Canfran et al. 2013; van den Berg et al. 2002; Renner et al. 2008). Furthermore, it appears that higher levels of PEEP increase dynamic indicators of fluid responsiveness (such as stroke volume variation) reducing the utility of these metrics as predictors of fluid responsiveness. We suggest that clinicians anticipate that PEEP greater than 5 cm H2O may decrease cardiac index, lower systemic blood pressure, and reduce the specificity of arterial (or plethysmographic) respiratory variation as guides to “fluid responsiveness.”
Thoracic epidural placement
The use of regional or neuraxial anesthesia is a major component of many ERPs, with thoracic epidural analgesia (TEA) most commonly used for open abdominal surgical procedures. TEA with local anesthetics can leads to hypotension from reduction in venous return (sympathectomy with venodilation) and decreases in cardiac index (Gelman et al. 1980). Arterial vasodilation also occurs (which lower systemic vascular resistance) (Goertz et al. 1992; Baron et al. 1986). Lower doses of local anesthesia have been shown to preserve cardiac index in patients receiving a TEA (Tanaka et al. 1991; Hasenbos et al. 1988). These changes induced by TEA are best thought of as shifts in internal blood volume—relative hypovolemia. Thus, low dose infusions of catecholamines will counteract these effects preserving cardiac index, and fluid therapy is not necessary (Gelman et al. 1980). We suggest that clinicians electing to use TEA recognize that hypotension may be a result of relative hypovolemia and therapy, rather than fluid administration, could be low-dose catecholamine infusions or lower rates of local anesthesia infusion (to reverse or avoid sympathectomy, respectively). It is important to point out that this recommendation is based on physiological data, not on clinical outcomes data.
(vii) How should fluids be managed postoperatively?
Traditionally patients undergoing abdominal surgery were not allowed oral intake postoperatively, waiting for the gastrointestinal tract to “recover” before nutrition could be initiated safely (including both volume (fluids) and calories (through fluids or solid food)). In such fasting patients, replacement fluids must be provided intravenously. With ERPs a change in philosophy has occurred with surgeons often allowing oral intake immediately after surgery—provided there is no active nausea/vomiting. Given unrestricted access to oral fluids, patients can regulate their intake to preserve intravascular volume (as long as their thirst mechanisms are intact). Isolating the impact of this paradigm shift toward early postoperative oral intake is a challenge primarily because of the heterogeneity among various published colorectal ERPs. For instance, in a recent meta-analysis examining the characteristics of 13 colorectal ERPs, 9 of 13 centers allowed MBP, and only 8 of 13 centers protocolized perioperative fluid administration (Zhuang et al. 2013).
Since total fluid balance (or weight gain) after abdominal surgery is directly related to both length of stay and the incidence of complications (Brandstrup et al. 2003), it is important to avoid both postoperative hypovolemia and hypoperfusion (Bellamy 2006), as well as arbitrary infusion of intravenous fluids. The use of arterial (or plethysmographic) respiratory variation as guides to “fluid responsiveness” is challenging as patients are not mechanically ventilated after surgery and do not typically have invasive blood pressure monitoring in place (making maneuvers such as passive leg raising inapplicable). Several institutions, including Mayo Clinic, Duke University, and the University of Virginia have eliminated use of postoperative “maintenance” fluid therapy (continuous intravenous fluid administration) in colorectal patients who are able to tolerate the oral intake of clear liquids. All these sites have reported significant reductions in length of stay (Thiele et al. 2015a; Lovely et al. 2012; Miller et al. 2014). It hence seems reasonable to avoid intravenous fluid therapy when patients are tolerating clear oral liquids (often immediately after surgery).
What should be done when oral fluids are not being freely taken? In 2003, Brandstrup et al. (2003) showed that fluid balance and daily body weight are closely correlated for the first four postoperative days (Tolstrup & Brandstrup 2015) and that in patients undergoing major abdominal surgery, there is a clear relationship between total fluid balance and daily body weight gain and incident complications.
A meta-analysis has shown that maintaining patients near zero-fluid balance in the perioperative period leads to a decrease in postoperative complications with a reduction in length of hospital stay (Varadhan and Lobo 2010). We suggest that the fluid management framework utilized intraoperatively should be extended into the postoperative period, to the extent possible. In some instances, this may not be possible due to specific types of devices used during surgery. We suggest that patients tolerating clear liquids orally after surgery be given unrestricted access to such fluids and that intravenous fluid administration be avoided in this setting.
Future research questions
-
1)
What are the hemodynamic effects of preoperative isotonic bowel preparation (in the setting of an ERP)?
-
2)
Is there a clinical outcome difference between simple versus complex carbohydrate loading?
-
3)
Is a protocolized “restrictive” or “zero balance” technique equivalent to GDFT? This may be answered to some extent by the ongoing RELIEF trial (https://clinicaltrials.gov/ct2/show/NCT01424150), the focus of which is liberal versus restrictive fluid administration but which plans to examine the effect of GDFT using a statistical test of interaction. However, this study does not specifically focus on GDFT in the context of ERPs.
-
4)
What risk stratification tool(s) best predict outcomes in patients undergoing colorectal surgery and what are the clinical and financial implications of using risk stratification to influence monitoring decisions and hemodynamic management in patients undergoing colorectal surgery?
-
5)
Do colloids offer any benefits over crystalloid for intraoperative GDFT in non-septic patients undergoing colorectal surgery?
-
6)
Are potential benefits of chloride-restrictive electrolyte solutions (demonstrated in retrospective analyses) demonstrable in prospective studies and are there differences within available choices of such solutions (e.g., Ringer’s lactate or Hartmann’s solution versus PlasmaLyte)?
Summary
Iso-osmolar bowel preparation is unlikely to lead to preoperative hypovolemia requiring intravenous fluid therapy provided patients are given unrestricted access to clear fluids orally. In patients that present to the operating room in a hypovolemic state, rapid detection is feasible by dynamic indicators of fluid responsiveness such as arterial (or plethysmographic) respiratory variation. Inclusion of carbohydrates in preoperative oral fluids is likely to improve insulin sensitivity (particular when complex carbohydrates are used) and may reduce protein catabolism. Anuria is abnormal and requires immediate attention. In general, oliguria is common during and after anesthesia and surgery and should trigger diagnostic efforts but not fluid therapy until hypovolemia is established as the cause. Intraoperative fluid therapy should be based on a framework where all available information is integrated to determine if there is a physiologic problem requiring reversal. Low tidal volumes and PEEP alter the sensitivity and specificity of dynamic indicators of fluid responsiveness but have a minimal impact on cardiac index at levels commonly utilized in the operating room. To the extent possible, the approach to intraoperative fluid management should continue postoperatively.
Change history
10 April 2018
After publication of this article (Thiele et al., 2016 ), it was noticed that the HTML version contained errors with the collaborator group, the Perioperative Quality Initiative (POQI) I Workgroup, preventing the group members from being searchable within indexing repositories. The corrected declarations section can be found here.
Abbreviations
- ERP:
-
Enhanced recovery pathway
- ASER:
-
American Society for Enhanced Recovery
- POQI:
-
Perioperative Quality Initiative
- GDFT:
-
Goal-directed fluid therapy
- KDIGO:
-
Kidney Disease: Improving Global Outcomes
- MBP:
-
Mechanical bowel preparation
- CFM:
-
Conventional fluid management
- AKI:
-
Acute kidney injury
- NICE:
-
National Institute for Health and Care Excellence
- PEEP:
-
Positive end expiratory pressure
- ARDS:
-
Acute respiratory distress syndrome
- PBW:
-
Predicted body weight
- TEA:
-
Thoracic epidural analgesia
References
Ahn HJ, Kim JA, Lee AR, Yang M, Jung HJ, Heo B. The risk of acute kidney injury from fluid restriction and hydroxyethyl starch in thoracic surgery. Anesth Analg. 2016;122:186–93.
Alfonsi P, Vieillard-Baron A, Coggia M, Guignard B, Goeau-Brissonniere O, Jardin F, Chauvin M. Cardiac function during intraperitoneal CO2 insufflation for aortic surgery: a transesophageal echocardiographic study. Anesth Analg. 2006;102:1304–10.
Alpert RA, Roizen MF, Hamilton WK, Stoney RJ, Ehrenfeld WK, Poler SM, Wylie EJ. Intraoperative urinary output does not predict postoperative renal function in patients undergoing abdominal aortic revascularization. Surgery. 1984;95:707–11.
American Society of Anesthesiologists C. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology. 2011;114:495–511.
Annane D, Siami S, Jaber S, Martin C, Elatrous S, Declere AD, Preiser JC, Outin H, Troche G, Charpentier C, Trouillet JL, Kimmoun A, Forceville X, Darmon M, Lesur O, Reignier J, Abroug F, Berger P, Clec’h C, Cousson J, Thibault L, Chevret S, Investigators C. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA. 2013;310:1809–17.
Awad S, Varadhan KK, Ljungqvist O, Lobo DN. A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin Nutr. 2013;32:34–44.
Barker P, Trotter T, Hanning C. A study of the effect of Picolax on body weight, cardiovascular variables and haemoglobin concentration. Ann R Coll Surg Engl. 1992;74:318–9.
Baron JF, Decaux-Jacolot A, Edouard A, Berdeaux A, Samii K. Influence of venous return on baroreflex control of heart rate during lumbar epidural anesthesia in humans. Anesthesiology. 1986;64:188–93.
Bellamy MC. Wet, dry or something else? Br J Anaesth. 2006;97:755–7.
Benes J, Chytra I, Altmann P, Hluchy M, Kasal E, Svitak R, Pradl R, Stepan M. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: results of prospective randomized study. Crit Care. 2010;14:R118.
Borsheim E, Cree MG, Tipton KD, Elliott TA, Aarsland A, Wolfe RR. Effect of carbohydrate intake on net muscle protein synthesis during recovery from resistance exercise. J Appl Physiol. 2004;96:674–8.
Brandstrup B, Tonnesen H, Beier-Holgersen R, Hjortso E, Ording H, Lindorff-Larsen K, Rasmussen MS, Lanng C, Wallin L, Iversen LH, Gramkow CS, Okholm M, Blemmer T, Svendsen PE, Rottensten HH, Thage B, Riis J, Jeppesen IS, Teilum D, Christensen AM, Graungaard B, Pott F. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238:641–8.
Brandstrup B, Svendsen PE, Rasmussen M, Belhage B, Rodt SA, Hansen B, Moller DR, Lundbech LB, Andersen N, Berg V, Thomassen N, Andersen ST, Simonsen L. Which goal for fluid therapy during colorectal surgery is followed by the best outcome: near-maximal stroke volume or zero fluid balance? Br J Anaesth. 2012;109:191–9.
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39.
Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, Fanizza C, Caspani L, Faenza S, Grasselli G, Iapichino G, Antonelli M, Parrini V, Fiore G, Latini R, Gattinoni L, Investigators AS. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med. 2014;370:1412–21.
Canfran S, Gomez de Segura IA, Cediel R, Garcia-Fernandez J. Effects of fluid load on cardiovascular function during stepwise lung recruitment manoeuvre in healthy dogs. Vet J. 2013;197:800–5.
Cannesson M, Pestel G, Ricks C, Hoeft A, Perel A. Hemodynamic monitoring and management in patients undergoing high risk surgery: a survey among North American and European anesthesiologists. Crit Care. 2011;15:R197.
Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, Nemo G, Dragert K, Beaupre L, Hildebrand K, Macaulay W, Lewis C, Cook DR, Dobbin G, Zakriya KJ, Apple FS, Horney RA, Magaziner J. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453–62.
Chappell D, Jacob M, Hofmann-Kiefer K, Conzen P, Rehm M. A rational approach to perioperative fluid management. Anesthesiology. 2008;109:723–40.
Chowdhury AH, Cox EF, Francis ST, Lobo DN. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and plasma-lyte(R) 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg. 2012;256:18–24.
Chytra I, Pradl R, Bosman R, Pelnar P, Kasal E, Zidkova A. Esophageal Doppler-guided fluid management decreases blood lactate levels in multiple-trauma patients: a randomized controlled trial. Crit Care. 2007;11:R24.
Cochrane JP, Forsling ML, Gow NM, Le Quesne LP. Arginine vasopressin release following surgical operations. Br J Surg. 1981;68:209–13.
Cohen ME, Bilimoria KY, Ko CY, Richards K, Hall BL. Variability in length of stay after colorectal surgery: assessment of 182 hospitals in the national surgical quality improvement program. Ann Surg. 2009;250:901–7.
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL. Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med. 2005;31:517–23.
Disma N, Mameli L, Pistorio A, Davidson A, Barabino P, Locatelli BG, Sonzogni V, Montobbio G. A novel balanced isotonic sodium solution vs normal saline during major surgery in children up to 36 months: a multicenter RCT. Paediatr Anaesth. 2014;24:980–6.
Egal M, de Geus HR, van Bommel J, Groeneveld AB. Targeting oliguria reversal in perioperative restrictive fluid management does not influence the occurrence of renal dysfunction: a systematic review and meta-analysis. Eur J Anaesthesiol. 2016a.
Egal M, Erler NS, de Geus HR, van Bommel J, Groeneveld AB. Targeting oliguria reversal in goal-directed hemodynamic management does Not reduce renal dysfunction in perioperative and critically ill patients: a systematic review and meta-analysis. Anesth Analg. 2016b;122:173–85.
Excellence NIfHaC. CardioQ-ODM oesophageal Doppler monitor. 2011.
Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350:2247–56.
Forget P, Lois F, de Kock M. Goal-directed fluid management based on the pulse oximeter-derived pleth variability index reduces lactate levels and improves fluid management. Anesth Analg. 2010;111:910–4.
Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, Lefrant JY, Allaouchiche B, Verzilli D, Leone M, De Jong A, Bazin JE, Pereira B, Jaber S. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–37.
Gan TJ, Soppitt A, Maroof M, El-Moalem H, Robertson KM, Moretti E, Dwane P, Glass PS. Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology. 2002;97:820–6.
Gelman S, Laws HL, Potzick J, Strong S, Smith L, Erdemir H. Thoracic epidural vs balanced anesthesia in morbid obesity: an intraoperative and postoperative hemodynamic study. Anesth Analg. 1980;59:902–8.
Goepfert MS, Richter HP, Zu Eulenburg C, Gruetzmacher J, Rafflenbeul E, Roeher K, von Sandersleben A, Diedrichs S, Reichenspurner H, Goetz AE, Reuter DA. Individually optimized hemodynamic therapy reduces complications and length of stay in the intensive care unit: a prospective, randomized controlled trial. Anesthesiology. 2013;119:824–36.
Goertz A, Heinrich H, Seeling W. Baroreflex control of heart rate during high thoracic epidural anaesthesia. A randomised clinical trial on anaesthetised humans. Anaesthesia. 1992;47:984–7.
Gravante G, Caruso R, Andreani SM, Giordano P. Mechanical bowel preparation for colorectal surgery: a meta-analysis on abdominal and systemic complications on almost 5,000 patients. Int J Colorectal Dis. 2008;23:1145–50.
Guinot PG, de Broca B, Bernard E, Abou Arab O, Lorne E, Dupont H. Respiratory stroke volume variation assessed by oesophageal Doppler monitoring predicts fluid responsiveness during laparoscopy. Br J Anaesth. 2014;112:660–4.
Hajjar LA, Vincent JL, Galas FR, Nakamura RE, Silva CM, Santos MH, Fukushima J, Kalil Filho R, Sierra DB, Lopes NH, Mauad T, Roquim AC, Sundin MR, Leao WC, Almeida JP, Pomerantzeff PM, Dallan LO, Jatene FB, Stolf NA, Auler Jr JO. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA. 2010;304:1559–67.
Harbis A, Perdreau S, Vincent-Baudry S, Charbonnier M, Bernard MC, Raccah D, Senft M, Lorec AM, Defoort C, Portugal H, Vinoy S, Lang V, Lairon D. Glycemic and insulinemic meal responses modulate postprandial hepatic and intestinal lipoprotein accumulation in obese, insulin-resistant subjects. Am J Clin Nutr. 2004;80:896–902.
Hasenbos M, Liem TH, Kerkkamp H, Gielen M. The influence of high thoracic epidural analgesia on the cardiovascular system. Acta Anaesthesiol Belg. 1988;39:49–54.
Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409–17.
Holte K, Nielsen KG, Madsen JL, Kehlet H. Physiologic effects of bowel preparation. Dis Colon Rectum. 2004;47:1397–402.
Huemer G, Kolev N, Kurz A, Zimpfer M. Influence of positive end-expiratory pressure on right and left ventricular performance assessed by Doppler two-dimensional echocardiography. Chest. 1994;106:67–73.
Johnson 3rd BL, Davis BR, Rafferty JF, Paquette IM. Postoperative predictors of early discharge following laparoscopic segmental colectomy. Int J Colorectal Dis. 2015;30:703–6.
Jones C, Kelliher L, Dickinson M, Riga A, Worthington T, Scott MJ, Vandrevala T, Fry CH, Karanjia N, Quiney N. Randomized clinical trial on enhanced recovery versus standard care following open liver resection. Br J Surg. 2013;100:1015–24.
Joris JL, Noirot DP, Legrand MJ, Jacquet NJ, Lamy ML. Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg. 1993;76:1067–71.
Junghans T, Neuss H, Strohauer M, Raue W, Haase O, Schink T, Schwenk W. Hypovolemia after traditional preoperative care in patients undergoing colonic surgery is underrepresented in conventional hemodynamic monitoring. Int J Colorectal Dis. 2006;21:693–7.
Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78:606–17.
Krajewski ML, Raghunathan K, Paluszkiewicz SM, Schermer CR, Shaw AD. Meta-analysis of high- versus low-chloride content in perioperative and critical care fluid resuscitation. Br J Surg. 2015;102:24–36.
Kramer A, Zygun D, Hawes H, Easton P, Ferland A. Pulse pressure variation predicts fluid responsiveness following coronary artery bypass surgery. Chest. 2004;126:1563–8.
Kwon S, Thompson R, Dellinger P, Yanez D, Farrohki E, Flum D. Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg. 2013;257:8–14.
Lansdorp B, Lemson J, van Putten MJ, de Keijzer A, van der Hoeven JG, Pickkers P. Dynamic indices do not predict volume responsiveness in routine clinical practice. Br J Anaesth. 2012;108:395–401.
Lassnigg A, Donner E, Grubhofer G, Presterl E, Druml W, Hiesmayr M. Lack of renoprotective effects of dopamine and furosemide during cardiac surgery. J Am Soc Nephrol. 2000;11:97–104.
Lellouche F, Dionne S, Simard S, Bussieres J, Dagenais F. High tidal volumes in mechanically ventilated patients increase organ dysfunction after cardiac surgery. Anesthesiology. 2012;116:1072–82.
Liu F, Zhu S, Ji Q, Li W, Liu J. The impact of intra-abdominal pressure on the stroke volume variation and plethysmographic variability index in patients undergoing laparoscopic cholecystectomy. Biosci Trends. 2015;9:129–33.
Lobo DN, Awad S. Should chloride-rich crystalloids remain the mainstay of fluid resuscitation to prevent ‘pre-renal’ acute kidney injury?: con. Kidney Int. 2014;86:1096–105.
Lovely JK, Maxson PM, Jacob AK, Cima RR, Horlocker TT, Hebl JR, Harmsen WS, Huebner M, Larson DW. Case-matched series of enhanced versus standard recovery pathway in minimally invasive colorectal surgery. Br J Surg. 2012;99:120–6.
Luttikhold J, Oosting A, van den Braak CC, van Norren K, Rijna H, van Leeuwen PA, Bouritius H. Preservation of the gut by preoperative carbohydrate loading improves postoperative food intake. Clin Nutr. 2013;32:556–61.
Magder S, Veerassamy S, Bates JH. A further analysis of why pulmonary venous pressure rises after the onset of LV dysfunction. J Appl Physiol. 2009;106:81–90.
McCluskey SA, Karkouti K, Wijeysundera D, Minkovich L, Tait G, Beattie WS. Hyperchloremia after noncardiac surgery is independently associated with increased morbidity and mortality: a propensity-matched cohort study. Anesth Analg. 2013;117:412–21.
Miller TE, Thacker JK, White WD, Mantyh C, Migaly J, Jin J, Roche AM, Eisenstein EL, Edwards R, Anstrom KJ, Moon RE, Gan TJ, Enhanced Recovery Study G. Reduced length of hospital stay in colorectal surgery after implementation of an enhanced recovery protocol. Anesth Analg. 2014;118:1052–61.
Muller L, Toumi M, Bousquet PJ, Riu-Poulenc B, Louart G, Candela D, Zoric L, Suehs C, de La Coussaye JE, Molinari N, Lefrant JY, AzuRea G. An increase in aortic blood flow after an infusion of 100 ml colloid over 1 minute can predict fluid responsiveness: the mini-fluid challenge study. Anesthesiology. 2011;115:541–7.
Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, Glass P, Lipman J, Liu B, McArthur C, McGuinnes S, Rajbhandari D, Taylor CB, Webb SAR. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367:1901-11.
Ni CY, Yang Y, Chang YQ, Cai H, Xu B, Yang F, Lau WY, Wang ZH, Zhou WP. Fast-track surgery improves postoperative recovery in patients undergoing partial hepatectomy for primary liver cancer: a prospective randomized controlled trial. Eur J Surg Oncol. 2013;39:542–7.
Noblett SE, Snowden CP, Shenton BK, Horgan AF. Randomized clinical trial assessing the effect of Doppler-optimized fluid management on outcome after elective colorectal resection. Br J Surg. 2006;93:1069–76.
Ostrow CL, Hupp E, Topjian D. The effect of Trendelenburg and modified trendelenburg positions on cardiac output, blood pressure, and oxygenation: a preliminary study. Am J Crit Care. 1994;3:382–6.
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, Madsen KR, Moller MH, Elkjaer JM, Poulsen LM, Bendtsen A, Winding R, Steensen M, Berezowicz P, Soe-Jensen P, Bestle M, Strand K, Wiis J, White JO, Thornberg KJ, Quist L, Nielsen J, Andersen LH, Holst LB, Thormar K, Kjaeldgaard AL, Fabritius ML, Mondrup F, Pott FC, Moller TP, Winkel P, Wetterslev J, Group ST, Scandinavian Critical Care Trials G. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367:124–34.
Phan TD, D’Souza B, Rattray MJ, Johnston MJ, Cowie BS. A randomised controlled trial of fluid restriction compared to oesophageal Doppler-guided goal-directed fluid therapy in elective major colorectal surgery within an enhanced recovery after surgery program. Anaesth Intensive Care. 2014;42:752–60.
Pillai P, McEleavy I, Gaughan M, Snowden C, Nesbitt I, Durkan G, Johnson M, Cosgrove J, Thorpe A. A double-blind randomized controlled clinical trial to assess the effect of Doppler optimized intraoperative fluid management on outcome following radical cystectomy. J Urol. 2011;186:2201–6.
Potura E, Lindner G, Biesenbach P, Funk GC, Reiterer C, Kabon B, Schwarz C, Druml W, Fleischmann E. An acetate-buffered balanced crystalloid versus 0.9% saline in patients with end-stage renal disease undergoing cadaveric renal transplantation: a prospective randomized controlled trial. Anesth Analg. 2015;120:123–9.
Qureshi SH, Rizvi SI, Patel NN, Murphy GJ. Meta-analysis of colloids versus crystalloids in critically ill, trauma and surgical patients. Br J Surg. 2016;103:14–26.
Raghunathan K, Bonavia A, Nathanson BH, Beadles CA, Shaw AD, Brookhart MA, Miller TE, Lindenauer PK. Association between initial fluid choice and subsequent in-hospital mortality during the resuscitation of adults with septic shock. Anesthesiology. 2015;123:1385–93.
Ramsingh DS, Sanghvi C, Gamboa J, Cannesson M, Applegate 2nd RL. Outcome impact of goal directed fluid therapy during high risk abdominal surgery in low to moderate risk patients: a randomized controlled trial. J Clin Monit Comput. 2013;27:249–57.
Renner J, Gruenewald M, Meybohm P, Hedderich J, Steinfath M, Scholz J, Bein B. Effect of elevated PEEP on dynamic variables of fluid responsiveness in a pediatric animal model. Paediatr Anaesth. 2008;18:1170–7.
Reuter DA, Bayerlein J, Goepfert MS, Weis FC, Kilger E, Lamm P, Goetz AE. Influence of tidal volume on left ventricular stroke volume variation measured by pulse contour analysis in mechanically ventilated patients. Intensive Care Med. 2003;29:476–80.
Rollins KE, Lobo DN. Intraoperative goal-directed fluid therapy in elective major abdominal surgery: a meta-analysis of randomized controlled trials. Ann Surg. 2016;263:465–76.
Roy BD, Tarnopolsky MA, MacDougall JD, Fowles J, Yarasheski KE. Effect of glucose supplement timing on protein metabolism after resistance training. J Appl Physiol. 1997;82:1882–8.
Sanders G, Mercer SJ, Saeb-Parsey K, Akhavani MA, Hosie KB, Lambert AW. Randomized clinical trial of intravenous fluid replacement during bowel preparation for surgery. Br J Surg. 2001;88:1363–5.
Section 2: AKI definition. Kidney Int Suppl. 2012;2:19–36.
Senagore AJ, Emery T, Luchtefeld M, Kim D, Dujovny N, Hoedema R. Fluid management for laparoscopic colectomy: a prospective, randomized assessment of goal-directed administration of balanced salt solution or hetastarch coupled with an enhanced recovery program. Dis Colon Rectum. 2009;52:1935–40.
Severgnini P, Selmo G, Lanza C, Chiesa A, Frigerio A, Bacuzzi A, Dionigi G, Novario R, Gregoretti C, de Abreu MG, Schultz MJ, Jaber S, Futier E, Chiaranda M, Pelosi P. Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology. 2013;118:1307–21.
Shaw AD, Bagshaw SM, Goldstein SL, Scherer LA, Duan M, Schermer CR, Kellum JA. Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to Plasma-Lyte. Ann Surg. 2012;255:821–9.
Shaw AD, Schermer CR, Lobo DN, Munson SH, Khangulov V, Hayashida DK, Kellum JA. Impact of intravenous fluid composition on outcomes in patients with systemic inflammatory response syndrome. Crit Care. 2015;19:334.
Sibbald WJ, Paterson NA, Holliday RL, Baskerville J. The Trendelenburg position: hemodynamic effects in hypotensive and normotensive patients. Crit Care Med. 1979;7:218–24.
Sinclair S, James S, Singer M. Intraoperative intravascular volume optimisation and length of hospital stay after repair of proximal femoral fracture: randomised controlled trial. BMJ. 1997;315:909–12.
Smith MD, McCall J, Plank L, Herbison GP, Soop M, Nygren J. Preoperative carbohydrate treatment for enhancing recovery after elective surgery. The Cochrane Database of Systematic Reviews. 2014;8, CD009161.
Srinivasa S, Taylor MH, Singh PP, Yu TC, Soop M, Hill AG. Randomized clinical trial of goal-directed fluid therapy within an enhanced recovery protocol for elective colectomy. Br J Surg. 2013;100:66–74.
Suehiro K, Okutani R. Influence of tidal volume for stroke volume variation to predict fluid responsiveness in patients undergoing one-lung ventilation. J Anesth. 2011;25:777–80.
Svanfeldt M, Thorell A, Hausel J, Soop M, Rooyackers O, Nygren J, Ljungqvist O. Randomized clinical trial of the effect of preoperative oral carbohydrate treatment on postoperative whole-body protein and glucose kinetics. Br J Surg. 2007;94:1342–50.
Tanaka K, Harada T, Dan K. Low-dose thoracic epidural anesthesia induces discrete thoracic anesthesia without reduction in cardiac output. Reg Anesth. 1991;16:318–21.
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P. Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology. 1998;89:1313–21.
Terai C, Uenishi M, Sugimoto H, Shimazu T, Yoshioka T, Sugimoto T. Transesophageal echocardiographic dimensional analysis of four cardiac chambers during positive end-expiratory pressure. Anesthesiology. 1985;63:640–6.
Thiele RH, Rea KM, Turrentine FE, Friel CM, Hassinger TE, McMurry TL, Goudreau BJ, Umapathi BA, Kron IL, Sawyer RG, Hedrick TL. Standardization of care: impact of an enhanced recovery protocol on length of stay, complications, and direct costs after colorectal surgery. J Am Coll Surg. 2015a;220:430–43.
Thiele RH, Bartels K, Gan TJ. Inter-device differences in monitoring for goal-directed fluid therapy. Can J Anaesth. 2015b;62:169–81.
Tolstrup J, Brandstrup B. Clinical assessment of fluid balance is incomplete for colorectal surgical patients. Proc Nutr Soc. 2015;104:161–8.
Tsuchiya M, Yamada T, Asada A. Pleth variability index predicts hypotension during anesthesia induction. Acta Anaesthesiol Scand. 2010;54:596–602.
van den Berg PC, Jansen JR, Pinsky MR. Effect of positive pressure on venous return in volume-loaded cardiac surgical patients. J Appl Physiol. 2002;92:1223–31.
Van Trigt P, Spray TL, Pasque MK, Peyton RB, Pellom GL, Christian CM, Fagraeus L, Wechsler AS. The effect of PEEP on left ventricular diastolic dimensions and systolic performance following myocardial revascularization. Ann Thorac Surg. 1982;33:585–92.
Varadhan KK, Lobo DN. A meta-analysis of randomised controlled trials of intravenous fluid therapy in major elective open abdominal surgery: getting the balance right. Proc Nutr Soc. 2010;69:488–98.
Varadhan KK, Neal KR, Dejong CH, Fearon KC, Ljungqvist O, Lobo DN. The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr. 2010;29:434–40.
Venn R, Steele A, Richardson P, Poloniecki J, Grounds M, Newman P. Randomized controlled trial to investigate influence of the fluid challenge on duration of hospital stay and perioperative morbidity in patients with hip fractures. Br J Anaesth. 2002;88:65–71.
Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 2000;342:1301–8.
Wakeling HG, McFall MR, Jenkins CS, Woods WG, Miles WF, Barclay GR, Fleming SC. Intraoperative oesophageal Doppler guided fluid management shortens postoperative hospital stay after major bowel surgery. Br J Anaesth. 2005;95:634–42.
Wu Y, Zhou S, Zhou Z, Liu B. A 10-second fluid challenge guided by transthoracic echocardiography can predict fluid responsiveness. Crit Care. 2014;18:R108.
Yates DR, Davies SJ, Milner HE, Wilson RJ. Crystalloid or colloid for goal-directed fluid therapy in colorectal surgery. Br J Anaesth. 2014;112:281–9.
Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z. Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2013;56:667–78.
POQI I conference directors (named authors on all manuscripts)
• Timothy E Miller, Department of Anesthesiology, Duke University Medical Center, NC, USA.
• Andrew D Shaw, Department of Anesthesiology, Vanderbilt University Medical Center, Nashville, TN, USA.
• Michael G Mythen, Department of Anaesthesia, University College London, London, UK.
• Tong J Gan, Department of Anesthesiology, Stony Brook University School of Medicine, NY, USA.
Group A – analgesia
• Matthew D. McEvoy, Department of Anesthesiology, Vanderbilt University Medical Center, Nashville, TN, USA (chair).
• Michael J. Scott, Department of Anaesthesia, Royal Surrey County NHS Foundation Hospital, Surrey, UK (co-chair).
• Deborah Gordon, RN, Department of Anesthesiology and Pain Medicine, University of Washington.
• Stuart Grant, Department of Anesthesiology, Duke University Medical Center, NC, USA.
• Julie K.M. Thacker, Division of Advanced Oncologic and GI Surgery, Duke University Medical Center, NC, USA.
• Christopher L. Wu, Department of Anesthesiology, The Johns Hopkins University School of Medicine, MD, USA.
Group B – fluids
• Robert H. Thiele, Departments of Anesthesiology and Biomedical Engineering, University of Virginia School of Medicine, VA, USA (chair).
• Karthik Raghunathan, Department of Anesthesiology, Duke University Medical Center, USA (co-chair).
• CS Brudney, Department of Anesthesiology, Duke University Medical Center, USA.
• Dileep N Lobo, Division of Gastrointestinal Surgery, Nottingham University Hospitals and University of Nottingham, Nottingham, UK.
• Dr. Daniel Martin, Royal free Perioperative Research Group, Royal Free Hospital, London, UK.
• Anthony Senagore, Department of Surgery, University of Texas-Medical Branch at Galveston, Galveston, TX, USA.
• Maxime Cannesson, Department of Anesthesiology and Perioperative Medicine, University of California Los Angeles, CA, USA
Group C – infection
• Stefan D Holubar, Department of Surgery, Dartmouth-Hitchcock Medical Center, NH, USA (chair).
• Traci Hedrick, Department of Surgery, University of Virginia School of Medicine, VA, USA (co-chair).
• John Kellum, Department of Critical Care Medicine, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA.
• Ruchir Gupta, Department of Anesthesiology, Stony Brook University School of Medicine, NY, USA.
• Mark Hamilton, Department of Anaesthesia, St. George’s Hospital and Medical School, London, UK.
Group D – outcomes
• S. Ramani Moonesinghe, Department of Anaesthesia, University College London, London, UK. (chair).
• Mike PW Grocott, Department of Anesthesia and Critical Care Medicine, University of Southampton, UK (co-chair).
• Elliott Bennett-Guerrero, Department of Anesthesiology, Stony Brook University School of Medicine, NY, USA.
• Thomas J Hopkins, Department of Anesthesiology, Duke University Medical Center, NC, USA.
• Roberto Bergamaschi, Department of Surgery, Stony Brook University School of Medicine, NY, USA.
• Stuart McCluskey, Department of Anesthesia, University of Toronto, ON, Canada.
Funding
The POQI meeting received financial assistance from Baxter, Cheetah Medical, Edwards Life Sciences, Mallinckrodt, and Pacira.
Authors’ contributions
All authors contributed to the development of this manuscript, agree to its contents, and approved its final version. RHT and KR co-chaired the “fluids” subgroup.
Competing interests
RHT. has served on advisory boards of Teleflex (airway advisory board) and Masimo (real-time hemoglobin). KR received an Investigator-initiated Trial Award from Baxter and did not receive any honoraria or other funding from any other source. DNL has received unrestricted research funding, educational grants, and speaker’s honoraria from Baxter Healthcare, BBraun, and Fresenius Kabi. He has served on the advisory boards of Baxter Healthcare, Nutricia Clinical Care, and AbbVie. He has also received speaker’s honoraria from Nestle. TEM has received research funding from Edwards Lifesciences and has served as a consultant for Edwards Life Sciences, Cheetah Medical, and Grifols. TJG. has received research funding or honoraria from Baxter, Edwards Life Sciences, Mallinckrodt, and Pacira. MGM is Smiths Medical Professor of Anaesthesia and Critical Care UCL and a Consultant at UCLH. He is Director of the UCL Centre for Anaesthesia and The UCL Discovery Lab and a resident PI at the Institute of Spots Exercise and Health. He is a paid Consultant for Edwards Lifesciences (via UCL Consulting and independently) and Deltex in the USA. He was a National Clinical Advisor for the Department of Health Enhanced Recovery Partnership until May 2013; Stock holder and advisory board for Medical Defence Technologies LLC – (“Gastrostim” patented); Director Bloomsbury Innovation Group – a community interest company owned by UCLH Charity; Co-Inventor of “QUENCH” (fluid management system) IP being exploited by UCL Business. MGM’s institution has also received charitable donations and grants from Smiths Medical Endowment and Deltex Medical. MGM was also co-author of the GIFTASUP guidelines on perioperative fluid management; Editor in Chief of Perioperative Medicine; on the Editorial Board of the BJA and Critical Care; a member of the Improving Surgical Outcomes Group; Expert advisor to the NICE IV fluids guideline development group; Chairman of the Board of The National Institute of Academic Anaesthesia; Co-Director Xtreme Everest; Co-Chair Evidence Based Perioperative Medicine (EBPOM). ADS is a Consultant for Astute Medical and Edwards Lifesciences. He is on the Scientific Advisory Board for Thrasos and Battelle and DSMB chair for AM Pharma.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Thiele, R.H., Raghunathan, K., Brudney, C.S. et al. American Society for Enhanced Recovery (ASER) and Perioperative Quality Initiative (POQI) joint consensus statement on perioperative fluid management within an enhanced recovery pathway for colorectal surgery. Perioper Med 5, 24 (2016). https://doi.org/10.1186/s13741-016-0049-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13741-016-0049-9