Abstract
The emergency department (ED) has long been recognized as providing critical access to the health care system for many, yet only in the past few decades has the ED visit been recognized as an opportunity to identify and link patients to care for substance use disorders (SUDs). This review explores the evidence for ED-based screening, psychosocial and pharmacological interventions, and linkage to treatment for the spectrum of SUDs including high risk alcohol use and alcohol, opioid, tobacco and other SUDs. Despite knowledge gaps, methodological challenges and some inconsistency across interventions studied, opportunities for EDs to improve the care of patients across the spectrum of SUDs are robust.
Similar content being viewed by others
Background
The emergency department (ED) has long been recognized as a front door to the hospital and as providing critical access to the health care system for many, yet only in the past few decades has the ED visit been recognized as an opportunity to identify and link patients to care for substance use disorders [1,2,3]. Increasingly, the practice of actively screening, initiating psychosocial and pharmacological interventions, and linking patients with substance use disorders (SUD) to effective treatment has become more common, but for a variety of reasons, many EDs have not embraced the critical part they can play in this process [4].
Individuals with SUDs regularly access emergency care, with nearly half of all ED visits in the US categorized as relating to substance use disorders [5]. EDs disproportionately provide medical care for individuals with SUDs, thus offering access to the 20.1 million Americans aged 12 and older who meet criteria for a SUD [6]. The National Survey on Drug Use and Health (NSDUH) data from 2016, show that of the 19.9 million adults who needed treatment for a substance use disorder, only 2.1 million, or 10.8%, received addiction treatment within the past 12 months [7]. A Healthcare Cost and Utilization Project (HCUP) analysis on trends from 2006 to 2013 in the rate of ED visits involving substance use disorders, found a 37% increase, from 1838 to 2519, ED visits per 100,000 people ≥ 15 years of age [8].
Costs associated with SUDs, including lost productivity, healthcare costs and crime, are staggering and were reported as exceeding 400 billion dollars per year in the 2016 US Surgeon General’s Report, Facing Addiction in America [9]. This burden could potentially be reduced by closing the treatment gap, thus reducing increased costs from medical complications of SUDs, as well as higher ED admission rates, more frequent unintentional injuries, motor vehicle collisions, interpersonal violence, HIV and intentional or accidental overdose [10,11,12,13].
An ED visit for an acute change in health, whether from SUD related injury, pneumonia, soft tissue infection or overdose, provides an opportunity for physicians to actively engage patients in discussion and reflection, to help them to make the connection between substance use and their acute medical condition, which may help provide motivation for behavior change. Sometimes this connection is evident to patients, but often it is not, and concepts derived from motivational interviewing (MI) have been adapted to brief interventions used in ED settings to engage individuals in the process of making positive behavior changes through a 4 step process of engaging, focusing, evoking and planning [14, 15]. These interventions help guide the participant towards resolution of ambivalence and internal inconsistencies in an empathetic setting, and patients are assisted in making the connection between substance use and outcomes. Brief interventions are thus motivational interview-based conversations, that are empathetic, non-judgmental, patient autonomy centered, and often include MI based principals of open-ended questions, affirmations, reflective listening and summaries [16, 17]. There is a reasonably large body of literature on the effectiveness of brief intervention in the ED setting, with mixed and sometimes directly conflicting results, complicated by problematic methodology, fidelity to the intervention, concerns about assessment reactivity, variation in intervention dose, and intervention application across heterogeneous populations using a variety of different outcomes [17,18,19,20,21,22,23,24,25].
SUD screening recommendations and tools
The U.S. Preventative Services Task Force recommends screening in primary care settings for adults 18 years and older for alcohol misuse and advises brief behavioral counseling interventions for those engaged in risky or hazardous drinking to reduce alcohol misuse; no recommendations are made about ED care [26]. The American College of Emergency Physicians (ACEP) published in 2005 and then reaffirmed in 2017 a policy statement on alcohol screening in the ED: “ACEP believes emergency medical professionals are positioned and qualified to mitigate the consequences of alcohol abuse through screening programs, brief intervention, and referral to treatment” [27]. There is no policy recommendation on broad based brief intervention and referral to treatment for the treatment of other drugs of abuse in the Emergency Department.
The development of abbreviated validated tools to screen for alcohol enhances the ability for EDs to implement screening for alcohol misuse and alcohol use disorders. These tools include the 3 question AUDIT-C [28, 29], the CAGE [30, 31] (cut down, annoyed, guilty, eye-opener) questionnaire and the National Institute on Alcohol Abuse and Alcoholism (NIAAA) single question screen: ““How many times in the past year have you had 5 [for men] or 4 [for women and all adults older than 65 years] or more drinks in a day?”, [32] and have been recommended by organizations and used in multiple trials” [16, 26, 33].
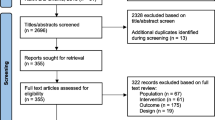
Validated screening tools for substance use disorders including the 10 item Drug Abuse Screening Test (DAST) [34, 35] exist, but the abbreviated NIDA Quick Screen Single drug use question: “How many times in the past year have you used an illegal drug or used a prescription medication for nonmedical reasons”, may be more appropriate in ED settings. This single screening question was found to be 100% sensitive and 73.5% specific for the detection of a drug use disorder in a primary care setting [36] (Fig. 1).
NIDA Quick Screen for substance use disorders. If the patient says “No” for all drugs in the Quick Screen, reinforce abstinence. Screening is complete. If patient says “Yes” to one or more days of heavy drinking, note that patient is an at-risk drinker. If patient says “Yes” to use of tobacco: Any current tobacco use places a patient at risk. If the patient says “Yes” to use of illegal drugs or prescription drugs for non-medical reasons, proceed to Question 1 of the NIDA-Modified ASSIST. Adapted from NIDA Screening for Drug Use in General Medical Settings Resource Guide [67, 68]
ED interventions for alcohol
Over the past several decades, a large body of literature has emerged relating to screening for alcohol and ED based interventions across the spectrum of patients with alcohol use and alcohol use disorders including harmful, hazardous, at-risk and dependent drinkers. Interventions focused on at-risk, harmful, hazardous drinkers have largely focused on reducing frequency or quantity of alcohol use, as well as injury prevention (i.e. alcohol-related injury, reduced drinking and driving, increasing seat belt use, etc.), while interventions focused on dependent drinkers or those meeting criteria for moderate or several alcohol use disorder focus on enhancing motivation to enter treatment [17, 18, 20, 37, 38]. Importantly, one observational study found that patients who received a direct referral, including transfer directly from the ED to a specialized treatment facility, were 30 times more likely to enroll in treatment than those with an indirect referral who are discharged home from the ED [38] (Table 1).
Although results are conflicting, in part due to heterogeneity across study populations and outcomes, the literature overall supports the use of motivational interview-based interventions for alcohol use in the emergency department. In 1997, a single site observational study of a brief intervention-based program found a significant reduction in frequency of alcohol use, drinks per day and frequency of > 5 drinks in one sitting in harmful and hazardous drinkers [41], while a 14 site study of screening and brief intervention for high risk alcohol consumers found a significant reduction in weekly drink consumption at 3 month follow-up in the group receiving a MI based intervention called the Brief Negotiated Interview (BNI) [2, 21]. A 2007 systematic review and meta-analysis examining the effect of interventions for alcohol problems in the ED identified 13 studies targeting reduction of alcohol consumption and related harm in non-alcohol dependent ED patients, and found no effect on the quantity/frequency or drinking or the frequency of heavy drinking at 12 months, inconclusive effects on the frequency of heavy drinking at 3 months, but a 41% reduction in the odds of sustaining an alcohol related injury in the 6 and 12 months following the index ED intervention [18].
A 2008 study of harmful and hazardous drinkers did not detect a difference between patients receiving a BNI and scripted discharge instructions [42], although a second study of harmful and hazardous drinkers, that included universal screening and interactive voice response methodology to reduce assessment reactivity found reduction in mean past 7-day alcohol use and past 28 day binge episodes at 6 and 12 month follow-up in the BNI group and BNI group with 30 day booster over standard care [17]. A 2017 systematic review of ED studies using brief intervention or motivational interview based intervention to reduce alcohol consumption identified 25 randomized controlled trials; 13 studies showed decreased alcohol consumption at primary outcome; 17 studies failed to demonstrate intervention effect for primary outcome of alcohol consumption, 11 of which found significant results for either a specific subgroup or a secondary outcome [37]. Overall, authors conclude that there is moderate quality evidence for the targeted use of brief interventions that showed a small reduction in alcohol use in low or moderate drinkers and a reduction in the consequences of use such as injury [37].
Despite some inconsistencies in effectiveness studies of ED brief intervention with referral to treatment with a focus on reducing alcohol use and injury, the literature demonstrates an overall trend toward cost-effectiveness [24, 43, 44]. A 2005 cost–benefit analysis of injured ED and hospitalized patients advised routine implementation of screening and brief intervention of all trauma patients after finding that 27% of all injured adult patients in the study were candidates for a brief intervention for alcohol, and factoring in health care systems level costs estimated $3.81 saved for every $1 spent on screening and intervention [44]. Additionally, an evaluation of working-age, disabled Medicaid patients in Washington State who received screening and a brief intervention that included a referral to SUD treatment if indicated found a reduction of $366 in Medicaid costs per member per month after propensity matching [43]. A more recent study calculated healthcare costs (total health care costs, 30-day ED visits, 1-year ED visits, inpatient claims, and behavioral health claims) at multiple EDs matched on location and time to a single ED that offered SBIRT to enhance SUD treatment and found a 21% reduction in health care costs in the cohort who received SBIRT, which translated to $2100 per patient receiving SBIRT per year [24].
ED interventions for non-medical opioid and illicit drug use
Early studies for MI based interventions on illicit drug use were promising, though evidence supporting the effectiveness of brief intervention in the ED setting to improve illicit drug related outcomes is limited. In general, there is a paucity of evidence supporting MI based interventions for illicit drug use in general, but compelling evidence exists specifically for ED-interventions specifically targeted for opioid use disorder (OUD) [3, 45]. A 2005 study demonstrated biochemical confirmation of increased cocaine and heroin abstinence at 6 months in the brief intervention arm of a RCT conducted in an urgent care, women’s clinic and homeless clinic setting [46]. An analysis of a large, multi-site study using brief intervention in ED and primary care settings of patients with illicit drug use at baseline reported a 67% reduction in illict drug use in those receiving brief intervention [47]. More recently, a large multisite trial prospectively evaluated the effect of randomization to brief intervention with booster versus screening, assessment and referral versus minimal screening only found no difference either in self-reported or biochemical confirmed drug use at 3, 6 or 12 months [22]. Important factors confounding the interpretation of this study include the, heterogeneity of drug type and severity use in the sample, and limited fidelity to the planned MI intervention with only 57% of participants in the MI treatment arm receiving the first booster and 39% of participants receiving the 2nd booster [22]. A large, single site study found that brief intervention for ED patients with drug or alcohol use disorders did not improve attendance at post-ED intervention over a case management intervention [48].
Two recent studies have demonstrated improved opioid-related outcomes after ED intervention for OUD. A pilot randomized clinical trial of 204 ED patients reporting non-medical prescription opioid use within the past 3 months found reductions in overdose risk behaviors and non-medical opioid use in the MI-intervention group in comparison to enhanced usual care [45]. A 2015 randomized clinical trial of ED patients with opioid dependence found a significant increase in treatment engagement at 30 days for patients randomized to the brief intervention, buprenorphine-induction and primary care follow up group (78%) in comparison to brief intervention and facilitated referral (45%) and referral to treatment (38%) [3]. Brief intervention with ED-initiated buprenorphine and primary care follow-up was also associated with decreased self-reported past 7 day opioid use at 30 day follow up [3], and cost-effectiveness using a healthcare systems perspective across all willingness-to-pay thresholds at 30 days [49].
This study has influenced a rapidly evolving clinical practice as many emergency departments are increasingly treating opioid withdrawal with buprenorphine and actively linking ED patient with opioid use disorder to care by starting buprenorphine in the ED and referring to treatment [50, 51].
Emerging evidence on the effectiveness of overdose prevention education and community naloxone distributions to individuals likely to witness or experience an overdose laid the foundation for the integration of overdose prevention and naloxone distribution into emergency departments who provide care to particularly high-risk patient populations, including those with ED visits for non-fatal overdose [52,53,54,55,56,57]. Descriptive studies about implementation of overdose prevention and naloxone distribution to ED patients at risk for opioid overdose have been reported, indicating feasibility and acceptability of overdose prevention and naloxone distribution from the ED to patients at risk of opioid overdose, though systematic prospective studies of ED overdose prevention and naloxone distribution have not been published [58, 59]. These programs are supported by an April, 2018 advisory from Jerome Adams, the 20th US Surgeon General that broadly supports clinicians to prescribe or dispense naloxone to individuals at risk of opioid overdose and their friends and family and “increase the awareness, possession and use of naloxone among at risk populations and broader communities” [60].
Some EDs are integrating the use of a peer navigator or recovery coach into post-opioid overdose ED care, though investigations on effectiveness have not been published to date [61].
ED interventions for tobacco
A meta-analysis of the literature through 2010 evaluating the effect of ED-initiated tobacco control interventions including preventative health services such as brief interventions and treatment referrals for smoking cessation identified 7 trials of weak to moderate quality and found the strongest effect of point prevalence of tobacco abstinence at 1 month (RR =1.47 (3 studies) (95% CI 1.06–2.06)), with a trend towards increased episodically measured tobacco abstinence up to 12 months (RR =1.33 (7 studies) (95% CI 0.96–1.83), P = 0.08) [62]. A randomized controlled trial published in 2011 found no difference between usual care who received screening and a brochure and enhanced care arm, who received a motivational interview, nicotine patches, and a booster call, although authors attributed the negative outcome to higher than expected quit rates in the usual care group, and hypothesized that low intensity screening and referral may have triggered some smokers to quit [63]. Interestingly, factors associated with quitting included any tobacco related ICD-9 ED diagnosis at index ED visit or subject belief that ED visit was tobacco releated [63]. A follow-up study of 778 low-income emergency department patients found that patients in the intervention group, who received a brief intervention, 6 weeks of nicotine replacement therapy, referral to a quitline had significantly higher rates of biochemically confirmed abstinence at 3 months (12.2%) compared to those who only received a brochure (4.9%). An updated meta-analysis containing 11 studies (10 published studies, 1 abstract) found a significant effect on the 1-year combined point prevalence of (RR of 1.40 (95% CI 1.06–1.86) (P = 0.02) [64]. Together, these results suggest that the ED provides a teachable moment about the relationship between a patients symptoms and his or her tobacco use, which can lead to sustained changes in tobacco-related behaviors.
Conclusion
Although opportunities exist to identify and refine effective ED care of patients with SUDs, the importance that the ED can have in improving outcomes for patients with SUDs is clear. Ample opportunities exist for emergency providers to improve care by screening, initiating treatment, either psychosocial or pharmacotherapies, and directly linking patients to ongoing treatment. Barriers to effective ED management of SUDs include competing priorities, inadequate training in addiction medicine, and stigma, some of which can be overcome by increasing the quantity and quality of addiction medicine training in the medical, nursing and allied health sciences training and post-graduate education, and by prioritization of enhanced care of the ED patient with SUDs through national and local reimbursement and quality mechanisms [65, 66].
Change history
16 July 2019
In the version of this article that was originally published [1], some information in the “Background” section was erroneously omitted.
References
Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Acad Emerg Med. 2009;16(11):1174–85.
Academic ED SBIRT Research Collaborative. The impact of screening, brief intervention, and referral for treatment on emergency department patients’ alcohol use. Ann Emerg Med. 2007;50(6):699–710.
D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. JAMA. 2015;313(16):1636–44.
Samuels EA, Dwyer K, Mello MJ, Baird J, Kellogg A, Bernstein E. Emergency department-based opioid harm reduction: moving physicians from willing to doing. Acad Emerg Med. 2016;23(4):455–65.
The DAWN Report. Highlights of the 2010 drug abuse warning network (DAWN) findings on drug-related emergency department visits [Internet]. [cited 2015 Apr 19]; http://archive.samhsa.gov/data/2k12/DAWN096/SR096EDHighlights2010.htm. Accessed 2 Feb 2018.
Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2017. https://www.samhsa.gov/data/. Accessed 20 July 2018.
Park-Lee E, Lipari RN, Hedden SL, Copello EAP, Kroutil LA. Receipt of services for substance use and mental health issues among adults: results from the 2015 National Survey on Drug Use and Health. NSDUH Data Review; 2016. http://www.samhsa.gov/data/. Accessed 20 July 2018.
Weiss AJ, Barrett ML, Heslin KC, Stocks C. Trends in emergency department visits involving mental and substance use disorders, 2006–2013 [Internet]. HCUP Stat. Br. #216. Agency Healthc. Res. Qual. Rockville, MD. 2016 [cited 2017 Nov 17]. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb216-Mental-Substance-Use-Disorder-ED-Visit-Trends.pdf. Accessed 2 Feb 2018.
Substance Abuse and Mental Health Services Administration (US), Office of the Surgeon General (US). Facing addiction in America: the Surgeon General’s report on alcohol, drugs, and health [Internet]. Washington (DC): US Department of Health and Human Services; 2016.
Rockett IRH, Putnam SL, Jia H, Chang CF, Smith GS. Unmet substance abuse treatment need, health services utilization, and cost: a population-based emergency department study. Ann Emerg Med. 2005;45(2):118–27.
Konstantopoulos WLM, Dreifuss JA, Mcdermott KA, et al. Identifying patients with problematic drug use in the emergency department: results of a multisite study. Ann Emerg Med. 2014;64(5):516–25.
Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300(22):2613–20.
Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016;54(10):901–6.
Miller RWRS. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford Press; 1991.
D’Onofrio G, Bernstein E, Rollnick S. Case studies in emergency medicine and the health of the public. Boston: Jones and Bartlett; 1996.
Bernstein E, Bernstein JA, Weiner SG, D’Onofrio G. Substance use disorders. In: Tintinalli JE, Stapczynski JS, Ma OJ, Yealy DM, Meckler GD, Cline DM, editors. Tintinalli’s emergency medicine: a comprehensive study guide. 8th ed. New York: McGraw-Hill Education; 2016.
D’Onofrio G, Fiellin DA, Pantalon MV, et al. A brief intervention reduces hazardous and harmful drinking in emergency department patients. Ann Emerg Med. 2012;60(2):181–92.
Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction. 2008;103(3):368–76.
Bernstein SL, D’Onofrio G. A promising approach for emergency departments to care for patients with substance use and behavioral disorders. Health Aff (Millwood). 2013;32(12):2122–8.
Simioni N, Rolland B, Cottencin O. Interventions for increasing alcohol treatment utilization among patients with alcohol use disorders from emergency departments: a systematic review. J Subst Abuse Treat. 2015;58:6–15.
Bernstein E, Bernstein J, Feldman J, et al. An evidence based alcohol screening, brief intervention and referral to treatment (SBIRT) curriculum for emergency department (ED) providers improves skills and utilization. Subst Abus. 2007;28(4):79–92.
Bogenschutz MP, Donovan DM, Mandler RN, et al. Brief intervention for patients with problematic drug use presenting in emergency departments: a randomized clinical trial. JAMA Intern Med. 2014;174(11):1736–45.
Donovan DM, Bogenschutz MP, Perl H, et al. Study design to examine the potential role of assessment reactivity in the screening, motivational assessment, referral, and treatment in emergency departments (SMART-ED) protocol. Addict Sci Clin Pract. 2012;7(1):16.
Pringle JL, Kelley DK, Kearney SM, et al. Screening, brief intervention, and referral to treatment in the emergency department. Med Care. 2018;56(2):146–52.
Miller WR, Rollnick S. The effectiveness and ineffectiveness of complex behavioral interventions: impact of treatment fidelity. Contemp Clin Trials. 2014;37(2):234–41.
Recommendations for Primary Care Practice - US Preventive Services Task Force [Internet]. [cited 2017 Mar 20]. https://www.uspreventiveservicestaskforce.org/Page/Name/recommendations. Accessed 2 Feb 2018.
American College of Emergency Physicians. ACEP—alcohol screening in the emergency department [Internet]. [cited 2018 Jul 22]. https://www.acep.org/patient-care/policy-statements/alcohol-screening-in-the-emergency-department/#sm.00000bvan9jy5bdjfuqbu1on3m52b. Accessed 22 July 2018.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory care quality improvement project (ACQUIP). Alcohol use disorders identification test. Arch Intern Med. 1998;158(16):1789–95.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG, World Health Organization, Dept. of Mental Health and Substance Dependence. AUDIT: the Alcohol Use Disorders Identification Test: guidelines for use in primary health care. 2nd ed. Geneva: World Health Organization; 2001. http://www.who.int/iris/handle/10665/67205. Accessed 2 Feb 2018.
Ewing JA. Detecting alcoholism. JAMA. 1984;252(14):1905.
O’Brien CP. The CAGE questionnaire for detection of alcoholism. JAMA. 2008;300(17):2054.
NIAAA. Helping patients who drink too much: a clinician’s guide. 2005. https://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. Accessed 2 Feb 2018.
Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. Primary care validation of a single-question alcohol screening test. J Gen Intern Med. 2009;24(7):783–8.
Skinner HA. The drug abuse screening test. Addict Behav. 1982;7(4):363–71.
Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the drug abuse screening test. J Subst Abuse Treat. 2007;32(2):189–98.
Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. A single-question screening test for drug use in primary care. Arch Intern Med. 2010;170(13):1155–60.
Barata IA, Shandro JR, Montgomery M, et al. Effectiveness of SBIRT for alcohol use disorders in the emergency department: a systematic review. West J Emerg Med. 2017;18(6):1143–52.
D’Onofrio G, Degutis LC. Integrating project ASSERT: a screening, intervention, and referral to treatment program for unhealthy alcohol and drug use into an urban emergency department. Acad Emerg Med. 2010;17(8):903–11.
Alcohol-use disorders: prevention | Guidance and guidelines | National Institute for Health and Care Excellence (NICE) [Internet]. [cited 2018 Jun 6]. https://www.nice.org.uk/guidance/ph24/chapter/8-glossary#harmful-drinking. Accessed 5 June 2018.
Ries R, Miller SC, Saitz R, Fiellin DA. The ASAM principles of addiction medicine. Philadelphia: Lippincott Williams & Wilkins; 2014.
Bernstein E, Bernstein J, Levenson S. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann Emerg Med. 1997;30(2):181–9.
D’Onofrio G, Pantalon MV, Degutis LC, et al. Brief intervention for hazardous and harmful drinkers in the emergency department. Ann Emerg Med. 2008;51(6):742–50.
Estee S, Wickizer T, He L, Shah MF, Mancuso D. Evaluation of the Washington state screening, brief intervention, and referral to treatment project. Med Care. 2010;48(1):18–24.
Gentilello LM, Ebel BE, Wickizer TM, Salkever DS, Rivara FP. Alcohol interventions for trauma patients treated in emergency departments and hospitals: a cost benefit analysis. Ann Surg. 2005;241(4):541–50.
Bohnert ASB, Bonar EE, Cunningham R, et al. A pilot randomized clinical trial of an intervention to reduce overdose risk behaviors among emergency department patients at risk for prescription opioid overdose. Drug Alcohol Depend. 2016;163:40–7.
Bernstein J, Bernstein E, Tassiopoulos K, Heeren T, Levenson S, Hingson R. Brief motivational intervention at a clinic visit reduces cocaine and heroin use. Drug Alcohol Depend. 2005;77(1):49–59.
Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99(1):280–95.
Blow FC, Walton MA, Murray R, et al. Intervention attendance among emergency department patients with alcohol-and drug-use disorders. J Stud Alcohol Drugs. 2010;71(5):713–9.
Busch SH, Fiellin DA, Chawarski MC, et al. Cost-effectiveness of emergency department-initiated treatment for opioid dependence. Addiction. 2017;112(11):2002–10.
Rubin R. As overdoses climb, emergency departments begin treating opioid use disorder. JAMA. 2018;319:2158–60.
Love JS, Perrone J, Nelson LS. Should buprenorphine be administered to patients with opioid withdrawal in the emergency department? Ann Emerg Med. 2018;72(1):26–8.
Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174.
McDonald R, Strang J. Are take-home naloxone programmes effective? Systematic review utilizing application of the Bradford Hill criteria. Addiction. 2016;111(7):1177–87.
Lagu T, Anderson BJ, Stein M. Overdoses among friends: drug users are willing to administer naloxone to others. J Subst Abuse Treat. 2006;30(2):129–33.
Hawk KF, Vaca FE, D’Onofrio G. Reducing fatal opioid overdose: prevention, treatment and harm reduction strategies. Yale J Biol Med. 2015;88(3):235.
Wheeler E, Jones TS, Gilbert MK, Davidson PJ. Centers for disease control and prevention (CDC). Opioid overdose prevention programs providing naloxone to laypersons—United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(23):631–5.
Seal KH, Thawley R, Gee L, et al. Naloxone distribution and cardiopulmonary resuscitation training for injection drug users to prevent heroin overdose death: a pilot intervention study. J Urban Health. 2005;82(2):303–11.
Dwyer KH, Walley AY, Sorensen-Alawad A, et al. Opioid education and nasal naloxone rescue kit distribution in the emergency department. Ann Emerg Med. 2013;62(4):S123.
Kestler A, Buxton J, Meckling G, et al. Factors associated with participation in an emergency department-based take-home naloxone program for at-risk opioid users. Ann Emerg Med. 2017;69(3):340–6.
Adams JM. Increasing naloxone awareness and use. JAMA. 2018;319(20):2073.
Samuels E. Emergency department naloxone distribution: a Rhode Island department of health, recovery community, and emergency department partnership to reduce opioid overdose deaths. R I Med J. 2014;97(10):38–9.
Rabe GL, Wellmann J, Bagos P, et al. Efficacy of emergency department-initiated tobacco control-systematic review and meta-analysis of randomized controlled trials. Nicot Tob Res. 2013;15(3):643–55.
Bernstein SL, Bijur P, Cooperman N, et al. A randomized trial of a multicomponent cessation strategy for emergency department smokers. Acad Emerg Med. 2011;18(6):575–83.
Lemhoefer C, Rabe GL, Wellmann J, et al. Emergency department-initiated tobacco control: update of a systematic review and meta-analysis of randomized controlled trials. Prev Chronic Dis. 2017;14:160434.
Wood E, Samet JH, Volkow ND. Physician education in addiction medicine. JAMA. 2013;310(16):1673–4.
O’Connor PG, Sokol RJ, D’Onofrio G. Addiction medicine: the birth of a new discipline. JAMA Intern Med. 2014;174(11):1717–8.
NIDA. Screening for drug use in general medical settings - resource guide [Internet]. [cited 2018 Feb 6]. https://d14rmgtrwzf5a.cloudfront.net/sites/default/files/resource_guide.pdf. Accessed 2 Feb 2018.
NIDA. Quick screen V1.0 1 STEP 1-Ask the NIDA quick screen question [Internet]. [cited 2018 Jul 20]. http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Accessed 20 July 2018.
Authors’ contributions
KH and GD performed a literature review, and participated fully in the writing and editing of this manuscript. Both authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval
Not applicable.
Funding
NIDA, 5K12DA033312.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hawk, K., D’Onofrio, G. Emergency department screening and interventions for substance use disorders. Addict Sci Clin Pract 13, 18 (2018). https://doi.org/10.1186/s13722-018-0117-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13722-018-0117-1