Abstract
Background
Low birth weight (LBW) predisposes physical and mental growth failure and premature death among infants. Studies report that LBW predominately explains infant mortality. However, existing studies rarely demonstrate the phenomenon of both observed and unobserved factors, which may influence the likelihood of birth and mortality outcomes simultaneously. In this study, we identified the spatial clustering of the prevalence of LBW along with its determinants. Further, the relationship between of LBW and infant mortality, considering the unobserved factors, has been explored in the study.
Methods
Data for this study have been extracted from the National Family Health Survey (NFHS) round 5, 2019-21. We used the directed acyclic graph model to identify the potential predictors of LBW and infant mortality. Moran’s I statistics have been used to identify the high-risk areas of LBW. We applied conditional mixed process modelling in Stata software to account for the simultaneous nature of occurrences of the outcomes. The final model has been performed after imputing the missing data of LBW.
Results
Overall, in India, 53% of the mothers reported their babies’ birth weight by seeing health card, 36% reported by recall, and about 10% of the LBW information was observed as missing. The state/union territory of Punjab and Delhi were observed to have the highest levels of LBW (about 22%) which is much higher than the national level (18%). The effect of LBW was more than four times larger compared to the effect in the analysis which does not account for the simultaneous occurrence of LBW and infant mortality (marginal effect; from 12 to 53%). Also, in a separate analysis, the imputation technique has been used to address the missing data. Covariates’ effects showed that female children, higher order births, births that occur in Muslim and non-poor families and literate mothers were negatively associated with infant mortality. However, a significant difference was observed in the impact of LBW before and after imputing the missing values.
Conclusions
The current findings showed the significant association of LBW with infant deaths, highlighting the importance of prioritising policies that help improve the birth weight of new-born children that may significantly reduce the infant mortality in India.
Similar content being viewed by others
Introduction
India plays a crucial role in ending premature deaths as the nation carries the highest number of child mortality globally [1]. Infant mortality rate (IMR) declined from 81 to 35 per 1000 live births between 1990 and 2016, with a 1.3% reduction rate [2]. The sustainable development goals (SDG) envisage to end preventable deaths of new-borns and children under 5 years of age, with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1000 live births and under-5 mortality to as low as 25 per 1000 live births by 2030 [2]. Unfortunately, the IMR in India is much higher than in the neighbouring countries, i.e. Nepal, Bangladesh, and Sri Lanka [1]. A study stated that due to the regional variations, half of the districts in India are unlikely to achieve the SDG target of child mortality by 2030 [3].
In India, approximately 83% of neonatal deaths occur due to complications from low birth weight (LBW) [4]. Pprevious studies have reported that infants born with a weight less than 2.5 kg face a higher risk of malnutrition and childhood morbidities such as diarrhoea and pneumonia [5, 6], which are the leading causes of neonatal and child mortality [7] and remain as an alarming concern among policymakers [8]. Furthermore, those who survive with LBW are more likely to experience problems related to cognitive capacity, attainment of schooling, degenerative disorder and growth faltering, which affect their income and productivity [5, 9, 10]. Child malnutrition, which is one of the results of LBW, alone accounts for half of the global child deaths [11]. Therefore, understanding the determinants of LBW is necessary to reduce mortality and improve the development indicators for future generations, especially in the limited resource countries such as India.
The etiology of LBW is not clearly understood. A study in South Africa demonstrated that the lack of antenatal care, hypertensive disorder during pregnancy, and previous cesarean delivery are associated with LBW [12]. Also, mother’s weight and height are significantly associated with LBW [13]. Additionally, mother’s education, wealth status, and birth order of the infant are the critical contributors to LBW [14]. Further, maternal nutritional status plays a significant role in the growth of the fetus, which is one of the important determinants of LBW [15]. Previous studies stated that household sanitation facilities, drinking water, and cooking fuel are the significant contributors to infant deaths [16, 17]. Therefore, the rationale for the present study is to understand the factors explaining LBW and its effects on their survival during their infancy. Also, interest lies in identifying the spatial clustering of LBW. We hypothesized that there are some common maternal and child health care factors, which can be useful to reduce the burden of both LBW and infant mortality. Thus, it would be helpful for the policymakers to relook into the strategies to achieve the third goal of SDGs, that is, ensuring good health and wellbeing for all at all ages in limited resource countries.
Conceptual framework
The study investigates the association between LBW and infant mortality. In the conceptual model, Fig. 1 displays the mechanism that is investigated in the present study. In social science research it is sometimes unable to observe the relevance of an occurrence. For example, in this study, the unobserved characteristics refer to maternal biological factors including factors that are not directly observed in the data. Therefore, it is difficult to explain the correlated error term as they can be correlated in many ways. However, without controlling for this, it may bias the covariates’ effect in the model and conclusions on risk factors. Therefore, a child born with LBW may depend on unobserved maternal characteristics (among explanatory variables). Similarly, infant mortality may depend on (among explanatory variables) unobserved maternal characteristics. For example, some mothers are more prone to give birth with LBW, leading to infant death. This is a common phenomenon for observations for the same unit that are influenced by the same (shared) unit-specific time unobserved invariant heterogeneity. Ignoring such indignity (confounding) may lead to biased inference of the impact of LBW on infant death. Our model accounted for cross equation correlation where the idiosyncratic error term (ε1, ε2) of each equation allowed to be correlated. Failing to include potential observed covariates in the model might lead to an unobserved heterogeneity (unobserved variability) in the response variable. For instance, potential covariates of LBW such as ‘maternal smoking during pregnancy, hypertensive disorder during pregnancy, which we cannot enter in our LBW model because of unavailability; thus, it remains unobserved and included in the idiosyncratic error term. Similarly, these factors may influence the mother’s behavior, a shared factor that influences the death of her child in an unobserved way.
Methodology
Data
The National Family Health Survey (NFHS), round 5 is a nationally representative survey that collected information on a wide range of socio-demographic and health indicators, conducted from June 2019 to April 2021 across 36 states and union territories. Census enumeration areas have been considered the primary sampling unit at the first stage of the sampling frame. In the second stage, households have been randomly selected from the sampling frame’s primary sampling unit, ‘cluster’. The details of the sampling technique are published elsewhere [18]. In the nationally representative study, data have been collected by using computer-assisted personal interviewing (CAPI). The response rate was 97%. The NFHS-5 survey collected information of 232,920 children during the survey period. The survey asked about the birth weight using the following questions: ‘Was weighed at birth?’ if yes, ‘How much did weight’ [18]. Mothers reported in two ways; the first is by remembering the baby’s weight, and the second is by using any card. The data revealed that 7924 children died before completing their first year of birth.
The NHFS has been conducted under the authority of the International Institute for Population Sciences (IIPS), under the Ministry of Health and Family Welfare. Ethical approval for the survey has been taken from the research ethics committee of the Ministry of Health and Family Welfare. Further, informed consent has been taken from each respondent before enrolling in the survey.
Dependent variables
Based on the question on the information of birth weight collected by the NFHS survey, LBW was defined as per the definition of the World Health Organization (WHO); with weight at birth less than 2500 grams. We created a dichotomous variable of birth weight based on the definition: ‘1’ for LBW and ‘0’ for no LBW.
Infant mortality is defined as a child’s death before completing the first year of life [19]. The survey collected information on the child’s survival status; whether the child was ‘died’ or ‘alive’. If the child is not surviving, they asked about the child’s age at death. The dependent variable is categorized into a dichotomous variable; ‘0’ for alive children and ‘1’ for infant deaths.
Directed Acyclic Graph (DAG) model to select the covariates
The DAG model was used to establish a causal inference in epidemiology to illustrate how associations translate into causal relationships. Epidemiologists mostly use DAG model to identify the mediators and moderators of the casual relationship between predictor and outcome variables that is also useful to identify the actual covariates. In the DAG model (Fig. 2), the blue circle with a bar indicates the outcome variable of the study. The yellow circle with a triangle represents the main exposure variable. A blue and yellow circle indicates the ancestors of outcome and exposure variables, respectively. The red circles represent the ancestor of exposure and outcome variable. The green and red lines indicate the causal and open pathways (where confounding might occur), respectively. The confounding pathways can be avoided by adjusting the observed and unobserved variables on the pathway.
Insti_deli = Institutional delivery, Fath_edu = Father’s education, Mom_edu = Mother’s Education, wealth = Wealth status of the household, smok_alco = Consumption of alcohol or smoking, F_secur = Food security, Sani = Sanitation facility of the household, Drin_water = Sources of drinking water, LBW = Low birth weight, preg_comp = Pregnancy complication, PTB = Preterm birth, ANC = Antenatal care, weight_gain = Weight gain during pregnancy, Age_mother = Maternal age at birth, nutria_edu = Nutritional education during pregnancy. Using the DAG model, we selected the explanatory variables to adjust the confounding pathways for the present study.
Thus, the potential risk factors of LBW and Infant mortality were selected from the DAG model. Preterm birth was defined as ‘live births before completing the gestational period of 37 weeks’, following the method given by Jana et al. [20]. The preterm birth was recoded as ‘yes’ and ‘no’. The place of delivery of the child was recoded as ‘home’, ‘private hospital’ and ‘public hospital’. The birth order of the child was recoded as ‘1’, ‘2’, and ‘3 & above’. Religion was classified as ‘Hindu’, ‘Muslim’ and ‘others’; ‘Others’ included Christian, Sikh, Buddhist/Neo-Buddhist, Jain, Jewish, Parsi/Zoroastrian, no religion and others. The place of residence was recoded as ‘rural’ and ‘urban’. National Family Health Survey-4 collected anthropometric measurements using biomarkers. Using this information, the mother who had Body Mass Index (BMI) less than 18.5 was defined as a thin mother, according to the definition of NFHS-5 [18]. The variable that a mother is thin was recoded as ‘yes’ and ‘no’. Mother’s age at birth has been categorized into ‘below 20’, ‘20-24’, ‘25-29’ and ‘30 & above’. Mother’s education was recoded as ‘illiterate or primary’, ‘secondary’ and ‘higher’. Furthermore, using the principal component analysis, the scores were generated based on the household assets such as television, bicycle, car, etc. Then the scores have been divided into two wealth quintiles. The wealth quintiles of the household were classified as ‘poor’ and ‘non-poor. The sanitation facility and sources of drinking water of the household were categorized as ‘improved’ and ‘unimproved’. Mother’s mass media exposure was recoded as ‘yes’ and ‘no’. The region of India was categorized into six; ‘North’, ‘North-East’, ‘South’, ‘Central’, ‘West’ and ‘East’.
Statistical analysis
The study used Global Positioning System (GPS) point data to create the hotspot map of low birth weight. Local Moran’s I statistics has been used to identify the high-risk areas of low birth weight. Moran’s I provides five clustering categories, including high-high, low-low, low-high, high-low, and not significant. High-high cluster (HH) illustrates the high prevalence areas and high-risk clusters or hotspots. In contrast, low-low (LL) cluster indicates the areas of low prevalence and the low-risk clusters of incidence or cold spots [21]. Further, we estimated a two-equation model considering LBW and infant mortality separately and allowed for correlated error terms associated with each equation (cross equation correlation). For example, we observed the propensity that a mother gave birth with LBW as y1 = 1 if y *1 > 0, and y1 = 0, otherwise. We also observed the propensity that the mother found her birth (child) to death during infancy, born to her with LBW as y2 = 1 if y *2 > 0, and y2 = 0, otherwise. Below we defined the equations.
where, θ1 = β1χ
Where, θ2 = δ y1 + β2χ. Both equations are (standard) probit equations. \(\varepsilon ={\left({\varepsilon}_1,{\varepsilon}_2\right)}^{\prime}\sim N\left(0,\Sigma \right),\sum =\left|\begin{array}{cc}1& {\sigma}_{12}\\ {}{\sigma}_{12}& 1\end{array}\right|,{\sigma}_{12}=\rho 12\), where ρ12 measured the endogeneity of y1 in the y2 equation. We estimated the model by exploiting cmp (conditional mixed process) command in stata [22]. Further, a multiple imputation technique has been used to impute the missing values of low birth weight in the study. Finally, model has been performed with the imputed data. We have used ArcMap version 10.3 and Stata version 14 for the analysis.
Results
Low birth weight, reporting system and missing data
Table 1 explains the state-wise distribution of sample children born with LBW and reporting system whether LBW outcome was reported by recalling or seeing the health card. Overall, in India, 53% of the mothers reported their babies’ birth weight by seeing health card, 36% reported by recall, and about 10% of the LBW information was observed as missing in the sample of this study. However, among the states, the missing information of LBW, means birth weight was not taken or mother did not report, was higher in Nagaland (50%) followed by Manipur (25%), Bihar (23%), Arunachal Pradesh (18%) and Meghalaya (17%), and lower percentage of missing information was observed in the South Indian states. Again, state-wise distribution of the reporting system revealed that a large proportion of mothers reported by seeing the health card which was higher in West Bengal (79%) follow by, Lakshadweep (78%), and Assam (76%). The state/union territory of Punjab and Delhi were observed to have the highest levels of LBW (about 22%), which was much higher than the national level (18.2%). However, Dadra and Nagar Haveli were observed to have 20.8% of children that are born with LBW followed by Haryana (20.5%), Madhya Pradesh (20.5%), Uttar Pradesh (20.2%) and Maharashtra (20.1%). Most of the North-Eastern states, such as Mizoram (4%), Nagaland (4.7%) and Manipur (7.2%) had the least prevalence of LBW.
Table 2 explains the distribution of LBW, missing cases of LBW and infant mortality by background characteristics of the child, parents and households. More female children were born with LBW (16.7%) as compared to male children (14.7%). The percentage of children with LBW was found to be more among preterm babies (23.6% vs 14.5% non-preterm babies). The delivery occurring at public (16.5%) or private hospitals (17%) were found to have more LBW than the deliveries occurring at home. A high proportion of children with LBW was observed among thin (BMI < 18 kg/m2), below 20 years old and illiterate mothers. LBW information was observed missing to some children and the missing cases varied by different background characteristics. Out of all sample children, 17% were observed as missing the information on their birth weight status. This leads to missing the cases for the outcome variable of LBW. By background characteristics, it is revealed that 50% of the children born at home were observed to have missing information on LBW. About 20% of all illiterate mothers did not report the birth weight information. The missing cases for LBW were observed more frequent in the female births, births that were in the higher birth order, births that occurred in rural areas and births by mothers who had no exposure to mass media.
In the dataset, 3.4% infants died before completing their first year of age. However, this rate varied by different background characteristics. About 5.5% of infants died among children with LBW compared to 2% in children with no LBW (> 2500 g). The infant death was higher among children born at home (home delivery) (3.2%), with three or higher orders (3.3%), those born to adolescent mothers (3.4%) and those born as preterm (5.8%). Also, infant death was higher among children born to mothers belonging to the poorest households and mothers who were illiterate, who had no mass media exposure were observed.
Further, we performed spatial analysis considering 30,198 clusters across all states and union territories to find out the spatial heterogeneity of LBW. Figure 3 shows the spatial distribution of the hot spots of LBW in India. The map shows that a high concentration of statistically significant hot spots were found in the Northern region, states/ union territories like Delhi, Punjab, Haryana and Uttar Pradesh. On the other hand, statistically significant cold spots were observed in the North-Eastern part of India.
Determinants of low birth weight and infant mortality
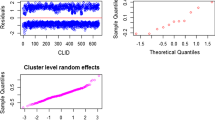
The study exploits the conditional mixed model, which is a general framework to estimate models with various link functions. The empirical model using cmp command was estimated in other research as well [23]. We report the coefficient estimates of infant mortality (Eq. 2) (Panel A) and LBW (Eq. 1) (Panel B) in Table 3. Three models were estimated: an uncorrelated (model 1), a correlated (model 2; based on case-wise deletion; benchmark model) and a correlated model (model 3; based on imputations). The imputation is considered for the missing values against the LBW variable.
Our primary focus was to estimate the effects of LBW on the probability of child deaths during infancy (0-11 months old), taking into account the frailty that the child born with LBW and death was influenced by the shared time-invariant mother specific unobserved heterogeneity, shown in panel A. Being born with LBW significantly increased the probability of death during infancy. The findings show that children born with LBW had 200% higher risk of death in the first year of life compared to children born with normal birth weight (β = 2.02, 95% CI: 1.93, 2.12). Accounting for the endogeneity of LBW (i.e., correlated errors) increased the estimated effects (marginal effects 53% in model 2 instead of 12% in uncorrelated model 1). Further, instead of case-wise deletion (model 2), the effect in a model (model 3; imputations) was estimated as less (marginal effects 48%). We consider model 3 as our benchmark (main results) model, where LBW was positively associated with the likelihood of infant mortality, and also the associated standard errors were relatively smaller compared to model 2 (correlated model with case-deletion, considering the confidence intervals). Covariates’ effects showed that female children, higher order births, births that occur in Muslim and non-poor families and to literate mothers were negatively associated with infant death. However, another set of covariates that increase the likelihood of infant deaths was: children being born to older mothers (aged 30 years and above), in rural area, and states from the Central and Eastern areas.
Results of panel B showed that preterm birth was significantly associated with the reduction in birth weight across all models. However, we explain the covariates’ effects of our benchmark model 3. The likelihood that a child will be born with LBW was 37% more in the preterm group compared to the group with ordinary births. Children being born to undernourished or thin mother, born at higher birth order, born to mothers who were uneducated or belonged to poor economic status were found to be significantly associated with LBW, while institutional birth and being born to mothers who were exposed to mass media were negatively associated with LBW.
Discussion
Infant mortality in India has reduced from 37 per 1000 live births in 2015 to 30 per 1000 live births in 2019 at national level [24]. However, it poses a challenge to meet the SDG of reducing the infant mortality to 25 per 1000 live births by 2030. Evidence suggests that LBW is a major contributor to morbidity and infant mortality [25,26,27,28]. Children born with LBW are more common in the developing countries. A proportion ranging from 15 to 20% of all births worldwide are observed to be born with a LBW, with the highest rate in South Asian countries, i.e., 28% [29]. India alone contributes to more than 40% of the LBW newborns in developing countries and 50% in Asia [30]. Thus, this study explored the effects of LBW and the likelihood of infant mortality among children with LBW, using the latest data of national survey of NFHS 2019-21.
Earlier studies on the effects of LBW and infant mortality rarely exploits the model where it accounts for the shared mother specific frailty that influences the occurrences of LBW and influences infant death simultaneously. The current study found that half of the mothers who gave birth at their home had missing data on LBW and the multivariable estimates attenuated in the model with imputations which corroborates the previous finding that the prevalence of LBW from only the sample of measured birth weight by ignoring missing data may result in underestimation [31], and highlights the need for imputation of missing information on LBW in future studies. We estimated two equations taking into account both observed and unobserved factors. To manifest the unobserved factors that may arise failing to address all important variables in the estimation models, we allowed two correlation terms of each equation to be associated. The results of the effects of covariates were more robust in this case and provided strong evidence on the maternal, child and socioeconomic determinants of LBW and its association with infant mortality in India.
Bringing down the prevalence of LBW remains an arduous task in India. As India will not only accomplish the SDG target of reducing child mortality by preventing LBW, it may also be a push factor for human capital development [32, 33]. Although, since the 1950s, the Indian Ministry of Health has started maternal and child health care services, approximately 53% of mothers reported birth weight by health card, with significant regional disparities. This suggests the unsuccessful universal coverage of maternal and child health care services, especially institutional delivery. However, the current analysis revealed that about 18% of children were born with LBW in India. The study found an increased prevalence of LBW in Northern states such as Delhi, Punjab, Haryana and the northern part of Uttar Pradesh. Previous studies revealed that the population of Delhi and the Northern part of Uttar Pradesh are more exposed to ambient air pollution [34]. In addition, a large volume of air pollution comes from the crop residue burning that most of the farmers practice in Punjab and Haryana [35, 36]. Past evidence suggests that mothers being exposed to air pollution during pregnancy have restricted feotal growth that indicates a strong relationship between LBW and air pollution [37, 38]. This may explain having the high concentration of LBW in those regions. Furthermore, the state of Nagaland is found to have worse performance in the maternal and child health care indicators, ranking lowest among the Northeastern states [39]. Still, one out of three mothers received full antenatal care in Punjab and Haryana [18]. Although, antenatal and postnatal coverages is substantially improving in the central region of India, still a large proportion of women do not go for institutional delivery, antenatal and postnatal checkup [40, 41]. However, maternal and child health care indicators indicates the coverage of the public health programs, which are critical for LBW that is also found in our study. On the other hand, infant mortality in this study has been observed higher in the central and eastern regions which have the higher proportion of tribal population in the country, and as reported, most of the indicators related to maternal and child health are poor in these regions [42].
However, in line with our hypothesis, we noted a significant association between LBW and infant mortality. The chances of a baby dying were 53% (marginal effects in model 3) higher when the baby was born with LBW. This effect is observed about five times larger in the correlated benchmark model (model 3) compared to the effects (12%) in the uncorrelated model (model 1). A reduction of the effect is observed in the model with case-deletion (model 2) and it was 53%. The smaller marginal effect (by 5%) was observed in model 3, which may be the case that imputation for missing cases of LBW addresses the selection bias. This is shown in the covariates’ effects as well and confidence intervals (by comparing model 2 & model 3). These results evidence the importance of two steps modelling and imputation of missing observations for better conclusions.
Regarding the mechanism, LBW may cause newborn complications such as asphyxia, improper physical growth, and respiratory and metabolic dysfunction, which can increase the probability of contracting infectious diseases and malnutrition during childhood [43], which is a significant factor in reducing the survival probability of an infant [44, 45]. The factors associated with LBW in this study were premature birth, place of delivery, birth order, mother’s thinness, age at birth and exposure to mass media. Importantly, the study found that babies born before completing the 37 weeks of gestation period were more likely to have LBW—the finding supported by previous studies [46, 47]. A preterm baby gets less time in the mother’s uterus to grow and gain weight, and most of the weight of the fetus is taken during the latter part of the pregnancy [48]. In line with this, preterm birth is found to be an independent factor of LBW in our study.
Albeit the Indian government has launched Pradhan Mantri Matru Vandana Yojana (PMMVY), a conditional cash transfer scheme to improve antenatal care and institutional delivery [49], our study found that the place of delivery is a significant contributor to LBW and infant mortality. In this regard, pregnant women are eligible for the scheme if they register their pregnancy at the Anganwadi Center (AWC) within 4 months of conception; attends at least one prenatal care session; and receive iron-folic acid tablets and TT injections. Nevertheless, our study also found a lower proportion of mothers who reported birth weight by health card. It can be assumed that women who had institutional delivery have more chances of receiving health checkups and other health care services during pregnancy, which positively affects fetal growth. The WHO suggests antenatal care for pregnant women to achieve SDGs through five interventions: nutritional interventions, physical health checkups, maternal and fetal assessment, preventive measures, and health system interventions [50]. A mother needs healthy weight gain during pregnancy, which is possible through ANC visits, especially for women belonging to low-income families [51, 52]. Moreover, iron supplementation during pregnancy helps improve the mother’s nutritional status and her fetus [53]. Thus, utilizing maternal health care services increases the probability of having a healthy child. Also, it has been observed that institutional delivery raises the survival probability of newborn children with LBW as they avail the medical facilities [54, 55].
The educated and wealthy women are usually more aware of access to healthcare facilities and the risks of inadequate healthcare use than the uneducated [56]. Previous study also reported that increased awareness through media can reduce the risk of LBM and related mortality [57]. Thus, the media can potentially spread information about maternal health care that could improve health of mothers and children, especially of those with limited education [58]. Our findings also found an association between media exposure and LBW. However, parents who belong to poor economic households may not be able to afford the economic burden of hospitalization [59]. Moreover, economically wealthy families have more chances of utilizing improved healthcare facilities. Consistently, our study found a lower probability of having children with LBW and the infant deaths with the increasing mother’s education and wealth status.
Notably, the study also found that adolescent maternal age (< 20 years) is linked with an increased risk of children being born with LBW. Adolescent mothers do not have proper biological development and might not be physically or emotionally prepared to carry the fetus during pregnancy [60, 61]. A previous study based on the NFHS-4 data revealed that child marriage is associated with poor child health, i.e. LBW, due to a lack of knowledge of health and undernutrition [62]. This poor knowledge regarding maternal and child health conditions and medical care decreases the survival probability of infants [57]. In addition, a thin mother represents malnutrition, which is independently associated with LBW due to the fetus’s inadequate nutrition supply [61]. The present study also showed that babies belonging to the 1st birth order were more likely to experience LBW, which is consistent with other studies [14, 63].
This study has several strengths. Firstly, it is based on the national-level data that used validated questionnaires and methodology. Secondly, this is one among the first studies in India that address the potential risk factors of LBW and simultaneously analyze its impact on infant mortality along with other risk factors using national representative data. Lastly, this study used the imputation technique to account for the missing information.
This study had some limitations too. Firstly, the accuracy of self-reported data for the diagnosis of LBW is subject to recall and reporting bias. Secondly, as previous studies explored a strong correlation between multiple gestation and preterm birth, which has been also observed in the dataset used for the study, we could not include multiple births in the model to avoid the multicollinearity. Although maternal anemia is a good predictor of LBW, the study was not able to consider it due to the unavailability of the information.
Conclusion
The findings of this study suggested a higher prevalence of LBW across India, which is higher in Northern India. Since LBW is shown to be associated with infant deaths in this study, it is important to prioritize the policies targeting risk factors of LBW to reduce significantly the infant mortality in India. Preterm birth is the most important predictor of LBW along with maternal factors such as delivery at home, nutritional status, age at birth and education. Measures should also be taken to improve the schemes such as iron supplementation, antenatal visit, and institutional delivery in India. The media can be used as a helpful tool for making people aware of the complications of LBW. Public-private partnerships that are recommended by the WHO in the health sector can strengthen survival outcomes of new-born babies with LBW. Through minimizing the burden of LBW, India might achieve the SDG target of reducing child mortality and malnutrition by 2030.
Availability of data and materials
The study uses secondary data that are available on reasonable request through https://dhsprogram.com/data/dataset_admin/.
References
WHO. Newborns: improving survival and well-being. Geneva: World Health Organization; 2020. https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality. Accessed 20 June 2022.
UN SDGs. Transforming our world: The 2030 Agenda for Sustainable Development. The United Nations Department of Economic and Social Affairs (UNDESA). New York. 2015.
Bora JK, Saikia N. Neonatal and under-five mortality rate in Indian districts with reference to sustainable development goal 3: an analysis of the National Family Health Survey of India (NFHS), 2015–2016. PLoS One. 2018;13:e0201125.
Dandona R, Kumar GA, Henry NJ, Joshua V, Ramji S, Gupta SS, et al. Subnational mapping of under-5 and neonatal mortality trends in India: the global burden of disease study 2000–17. Lancet. 2020;395:1640–58.
Fall CHD. Fetal malnutrition and long-term outcomes. Nestle Nutr Inst Workshop Ser. 2013;74:11–25.
McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312:82–90.
Million Death Study Collaborators, Bassani DG, Kumar R, Awasthi S, Morris SK, Paul VK, et al. Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet. 2010;376:1853–60.
Shashikantha SK, Sheethal MP. In: Shashikantha SK, Sheethal MP, editors. Prevalence of low birth weight and its associated factors: a community based cross sectional study in a rural area of Rohtak, Haryana: IJCMPH; 2017.
Christian P, Lee SE, Donahue Angel M, Adair LS, Arifeen SE, Ashorn P, et al. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low- and middle-income countries. Int J Epidemiol. 2013;42:1340–55.
Gluckman PD, Hanson MA, Beedle AS. Early life events and their consequences for later disease: a life history and evolutionary perspective. Am J Hum Biol. 2007;19:1–19.
WHO. Children: reducing mortality. 2016.
Olusanya BO, Ofovwe GE. Predictors of preterm births and low birthweight in an inner-city hospital in sub-Saharan Africa. Matern Child Health J. 2010;14:978–86.
de Britto RPA, Florêncio TMT, Silva AAB, Sesso R, Cavalcante JC, Sawaya AL. Influence of maternal height and weight on low birth weight: A cross-sectional study in poor communities of northeastern Brazil. PLoS One. 2013;8:e80159.
Gathimba NW, Wanjoya A, Kiplagat GK, Mbugua L, Kibiwott K. Modeling maternal risk factors affecting low birth weight among infants in Kenya. Am J Theor Appl Stat. 2017;6:22.
Dharmalingam A, Navaneetham K, Krishnakumar CS. Nutritional status of mothers and low birth weight in India. Matern Child Health J. 2010;14:290–8.
Patel R, Gupta A, Chauhan S, Bansod DW. Effects of sanitation practices on adverse pregnancy outcomes in India: a conducive finding from recent Indian demographic health survey. BMC Pregnancy Childbirth. 2019;19:378.
Patel N, Olickal JJ. Maternal and child factors of under-five mortality in India. Findings from NFHS-4. Clin Epidemiol Global Health. 2021;12:100866.
IIPS, ICF. National family Healh survey. Mumbai: international Institute for Population Sciences; 2022.
OECD, Organization WH. Infant mortality. Paris: OECD; 2020.
Jana A, Banerjee K, Khan PK. Early arrivals: association of maternal obstetric factors with preterm births and their survival in India. Public Health. 2022;211:37–46.
Gatrell AC. Book reviews: Griffith, D.A. 1987: spatial autocorrelation: a primer. Pennsylvania: Association of American Geographers. Iv + 82 pp. US $6.00. Prog Hum Geogr. 1989;13:144–5.
Roodman D. Fitting fully observed recursive mixed-process models with cmp. Stata J. 2011;11:159–206.
Saha UR, Bijwaard GE, Muhajarine N, Vrijkotte TG. Disadvantaged neighborhoods, birth weight, and problem behavior in five- and six-year-old pre-school children: evidence from a cohort born in Amsterdam. Soc Sci Med. 2020;265:113400.
Office of the Registrar General & Census Commissioner, India (ORGI). India - SAMPLE REGISTRATION SYSTEM (SRS)-BULLETIN 2020 VOLUME 55-I. 2020. https://censusindia.gov.in/nada/index.php/catalog/42687. Accessed 25 Jun 2022.
Lau C, Ambalavanan N, Chakraborty H, Wingate MS, Carlo WA. Extremely low birth weight and infant mortality rates in the United States. Pediatrics. 2013;131:855–60.
Rai SK, Kant S, Srivastava R, Gupta P, Misra P, Pandav CS, et al. Causes of and contributors to infant mortality in a rural community of North India: evidence from verbal and social autopsy. BMJ Open. 2017;7:e012856.
Sangamam R. Perinatal mortality and morbidity among low birth weight babies. Int J Community Med Public Health. 2017;2:51–8.
Shrimpton R. Preventing low birthweight and reduction of child mortality. Trans R Soc Trop Med Hyg. 2003;97:39–42.
WHO. Global nutrition targets 2025: low birth weight policy brief. Geneva: World Health Organization; 2014.
Reddy RS, Sarma YV. Comparative study of Socio-economic status of mothers who delivered term low birth weight babies with mothers who delivered normal birth weight babies in a tertiary care rural hospital. Int Arch Integr Med. 2015;2:6.
Singh U, Ueranantasun A, Kuning M. Factors associated with low birth weight in Nepal using multiple imputation. BMC Pregnancy Childbirth. 2017;17:1–10.
Petrou S. Economic consequences of preterm birth and low birthweight. BJOG. 2003;110(Suppl 20):17–23.
Johnson RC, Schoeni RF. The influence of early-life events on human capital, health status, and labor market outcomes over the life course. B E J Econom Anal Policy. 2011;11:2521.
Gautam AS, Dilwaliya NK, Srivastava A, Kumar S, Bauddh K, Siingh D, et al. Temporary reduction in air pollution due to anthropogenic activity switch-off during COVID-19 lockdown in northern parts of India. Environ Dev Sustain. 2021;23:8774–97.
Saxena P, Sonwani S, Srivastava A, Jain M, Srivastava A, Bharti A, et al. Impact of crop residue burning in Haryana on the air quality of Delhi, India. Heliyon. 2021;7:e06973.
Singh T, Biswal A, Mor S, Ravindra K, Singh V, Mor S. A high-resolution emission inventory of air pollutants from primary crop residue burning over northern India based on VIIRS thermal anomalies. Environ Pollut. 2020;266:115132.
Goyal N, Canning D. The association of in-utero exposure to ambient fine particulate air pollution with low birth weight in India. Environ Res Lett. 2021;16:054034.
Lavigne E, Yasseen AS, Stieb DM, Hystad P, van Donkelaar A, Martin RV, et al. Ambient air pollution and adverse birth outcomes: differences by maternal comorbidities. Environ Res. 2016;148:457–66.
Kim YE. Determinants of childhood vaccination in Nagaland, India: a cross-sectional study with multilevel modelling. BMJ Open. 2021;11:e045070.
Singh P, Singh KK, Singh P. Maternal health care service utilization among young married women in India, 1992–2016: trends and determinants. BMC Pregnancy Childbirth. 2021;21:122.
Bhatia M, Dwivedi LK, Banerjee K, Bansal A, Ranjan M, Dixit P. Pro-poor policies and improvements in maternal health outcomes in India. BMC Pregnancy Childbirth. 2021;21:389.
Ranjan M, Dwivedi LK, Mishra R, Sharma B. Infant mortality differentials among the tribal and non-tribal populations of central and Eastern India. Int J Popul Stud. 2016;2:26–43.
Karande S. Consequences of low birth weight, maternal illiteracy and poor access to medical care in rural India: infantile iatrogenic Cushing syndrome. BMJ Case Rep. 2015;2015:bcr2015211387.
Xiao X, Zhang Z-X, Li W-H, Feng K, Sun Q, Cohen HJ, et al. Low birth weight is associated with components of the metabolic syndrome. Metabolism. 2010;59:1282–6.
Aryastami NK, Shankar A, Kusumawardani N, Besral B, Jahari AB, Achadi E. Low birth weight was the most dominant predictor associated with stunting among children aged 12–23 months in Indonesia. BMC Nutrition. 2017;3:16.
Sutan R, Mohtar M, Mahat AN, Tamil AM. Determinant of low birth weight infants: A matched case control study. Open J Prev Med. 2014;4:91–9.
Alijahan R, Hazrati S, Mirzarahimi M, Pourfarzi F, Ahmadi HP. Prevalence and risk factors associated with preterm birth in Ardabil, Iran. Iran J Reprod Med. 2014;12:47–56.
Paneth NS. The problem of low birth weight. Futur Child. 1995;5:19–34.
Gautam A. A critical evaluation of Pradhan Mantri Matru Vandana Yojana. Jindal J Public Policy. 2018;4:(1):46–62.
Villar J, Ba’aqeel H, Piaggio G, Lumbiganon P, Miguel Belizán J, Farnot U, et al. WHO antenatal care randomised trial for the evaluation of a new model of routine antenatal care. Lancet. 2001;357:1551–64.
White DE, Fraser-Lee NJ, Tough S, Newburn-Cook CV. The content of prenatal care and its relationship to preterm birth in Alberta, Canada. Health Care Women Int. 2006;27:777–92.
Panaretto KS, Lee HM, Mitchell MR, Larkins SL, Manessis V, Buettner PG, et al. Impact of a collaborative shared antenatal care program for urban indigenous women: a prospective cohort study. Med J Aust. 2005;182:514–9.
Khanal V, Zhao Y, Sauer K. Role of antenatal care and iron supplementation during pregnancy in preventing low birth weight in Nepal: comparison of national surveys 2006 and 2011. Arch Public Health. 2014;72:4.
Tekelab T, Chojenta C, Smith R, Loxton D. The impact of antenatal care on neonatal mortality in sub-Saharan Africa: a systematic review and meta-analysis. PLoS One. 2019;14:e0222566.
Doku DT, Neupane S. Survival analysis of the association between antenatal care attendance and neonatal mortality in 57 low- and middle-income countries. Int J Epidemiol. 2017;46:1668–77.
Vilanova CS, Hirakata VN, de Souza Buriol VC, Nunes M, Goldani MZ, da Silva CH. The relationship between the different low birth weight strata of newborns with infant mortality and the influence of the main health determinants in the extreme south of Brazil. Popul Health Metrics. 2019;17:15.
Nabiwemba EL, Atuyambe L, Criel B, Kolsteren P, Orach CG. Recognition and home care of low birth weight neonates: a qualitative study of knowledge, beliefs and practices of mothers in Iganga-Mayuge health and demographic surveillance site, Uganda. BMC Public Health. 2014;14:546.
Singh PK, Singh L. Examining inter-generational differentials in maternal health care service utilization: insights from the Indian demographic and health survey. J Biosoc Sci. 2014;46:366–85.
Russell RB, Green NS, Steiner CA, Meikle S, Howse JL, Poschman K, et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics. 2007;120:e1–9.
Shrivastava. A longitudinal study of maternal and socioeconomic factors influencing neonatal birth weight in pregnant women attending an urban health center; 2013.
Han Z, Lutsiv O, Mulla S, McDonald SD, Knowledge Synthesis Group. Maternal height and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. J Obstet Gynaecol Can. 2012;34:721–46.
Raj A, Saggurti N, Winter M, Labonte A, Decker MR, Balaiah D, et al. The effect of maternal child marriage on morbidity and mortality of children under 5 in India: cross sectional study of a nationally representative sample. BMJ. 2010;340:b4258.
Tshotetsi L, Dzikiti L, Hajison P, Feresu S. Maternal factors contributing to low birth weight deliveries in Tshwane District, South Africa. PLoS One. 2019;14:e0213058.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Arup Jana: Conceptualization, methodology, data curation, formal analysis, writing (original draft preparation). Unnati Rani Saha: Conceptualization, methodology, supervision, validation, writing and editing the draft. Reshmi R.S: Conceptualization, supervision, writing and editing the draft. T. Muhammad: Conceptualization, writing and editing the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The organization committee of the survey received ethical approval from the Ministry of Health and Family Welfare (MoHFW) of India for collecting the human data. The Indian Demographic and Health Survey (DHS) is known as National Family Health Survey (NFHS) in India. We used published large scale national data where every respondent was anonymized in the data set itself. As it is not based on a primary survey- cases, we need not to do any anonymization in the study as the data is already made in that fashion following all ethical protocols. Thereby, it is certified that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of the survey. Also, verbal as well as written informed consent was obtained from all the participants. The informed consent was taken from their parent or legal guardian who were not mature or below 18 aged.
Consent for publication
The dataset is publicly available, thus consent for publication is not applicable for the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jana, A., Saha, U.R., Reshmi, R.S. et al. Relationship between low birth weight and infant mortality: evidence from National Family Health Survey 2019-21, India. Arch Public Health 81, 28 (2023). https://doi.org/10.1186/s13690-023-01037-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-023-01037-y