Abstract
Background
Homelessness is often described as both a driver and a consequence of poor health, social exclusion and economic marginalisation. The present protocol provides a detailed description of the study Examining the health situation of homeless people in Berlin: a retrospective analysis of data from the health centre for the homeless of the Jenny De la Torre Foundation from 2006 to 2020 (GIG study). The primary objective of the GIG study is to describe and analyse the social and health situation of homeless people in Berlin.
Methods
A retrospective secondary data analysis of an anonymous full census of medical records for the years 2006 until 2020 from a health centre for homeless people will be carried out. The main outcome is the description and analysis of the social and health situation of homeless people in Berlin. Total and cross-sectional sample characteristics will be presented in a descriptive analysis using Chi-Square Test, Mann-Whitney-U-Test or independent t-Test as appropriate to test (sub) group differences. Further, outcomes will be analysed using finite mixture modelling in order to distinguish different types of social and health conditions. Latent variable regressions will be applied in order to identify sociodemographic and disease-related factors associated with decreasing health conditions.
Discussion
Given the high number of homeless individuals in Germany, it is of great importance to examine their social and health situation in order to gain a better understanding of challenges and needs of homeless people and work on new approaches and solutions to effectively address these.
Trail registration
The study was prospectively registered with the German Clinical Trials Register (trial registration number: DRKS00021172). Registered 26 June 2020.
Similar content being viewed by others
Background
Homelessness is an extreme reflection of poverty and social exclusion [1] and represents a complex social and public health challenge [2]. Previous research has acknowledged the difficulty in the assessment of the scale of homelessness across Europe, due to inconsistencies in the definitions of homelessness as well as the variety of methodologies applied in data collection [3, 4]. In 2018 about 678,000 homeless people were living in Germany out of which approximately 41,000 spent at least some of their nights without shelter on the streets [5]. In Berlin, 60,000 people are currently estimated to be homeless [6] of which 2000–6000 sleeping rough [7, 8].
Homelessness is often described as both a driver and a consequence of poor health, social exclusion and economic marginalisation [9,10,11]. Life on the street or in collective accommodation, shelters or hostels represents a major health burden and is often associated with a variety of health problems [12]. For example, research depicts the consistently high rates of acute infectious and parasitic diseases, diseases of the circulatory, respiratory and musculoskeletal system [13] as well as high rates of blood borne infections such as hepatitis C, HIV, tuberculosis, as well as myocardial infarction and pneumonia [14,15,16]. In addition to acute conditions, a high percentage of the homeless suffer from multimorbidity and chronic diseases [14, 17] such as chronic pain [18] or chronic obstructive pulmonary disease [19]. A study by Queen, Lowrie, Richardson & Williamson [20] found in a homeless cohort with an average age of 42.8 years comparable levels of multimorbidity with those aged > 85 years in the general population. High prevalence of somatic diseases and harsh living conditions might also explain why homeless people generally suffer from higher mortality rates and earlier deaths [11, 21,22,23]. Homelessness is also associated with a higher risk of psychiatric disorders such as psychosis, major depression, personality disorders, alcohol dependency and drug dependency [24,25,26]. The high prevalence of somatic and psychiatric diseases can partially be explained by the various stressors associated with the loss of accommodation such as inadequate health maintenance, risk-prone health behaviours [27] and childhood traumata [28]. There have been a number of studies reporting high rates of smoking [29], as well as high rates of alcohol and/or substance misuse [30, 31]. Additionally, homeless people suffer from food insecurity resulting in a generally poorer diet characterised by higher intakes of salt and lower intakes of fruit, vitamin C and fibre [32]. Another major risk factor is the high exposure to violence and higher chance of injury experienced by homeless individuals [33,34,35]. Furthermore, medical care is usually provided outside the structures of the regular health care system and not always accessible [13, 36]. Rough sleepers are less likely to be registered with a general practitioner [37] and often do not have access to preventive care such as routine check-ups [38, 39]. The consequence of this lack of access to primary care results in a higher number of emergency department visits, hospital (re) admissions and longer inpatient stays [36, 40, 41]. This aspect is also reflected by the high use of emergency departments for dental problems by homeless people [42, 43].
To sum up, past research acknowledges a variety of health needs among homeless individuals. Despite growing recent evidence on the health status of homeless people, data and results do not allow for comparison across countries. Research on homelessness across the EU suffers from a variety of difficulties due to differences in definitions of homelessness and inconsistencies in applied research methodologies [3, 44,45,46,47]. Additionally, for Germany, there is a clear lack of empirical investigations on the social and health situation of homeless people. Further, homeless people are difficult to sample which limits most research and results in small and highly selected samples. A recent review found that previous research is highly selective were participants are often older, male and from a subgroup setting as for example from supervised drug consumption facilities [48]. Thus, there is a clear lack of investigation among women and younger individuals. In response to sampling difficulties, other countries such as Denmark, implemented a Homeless Register, where every contact in homeless shelters is documented [21]. There is a need of unbiased research of the homeless population in Germany. In addition, there is little evidence about the course of the social and health situation of homeless people. It is of great importance to gain better understanding of the social and health situation and needs of homeless people. The project Examining the health situation of homeless people in Berlin: a retrospective analysis of data from the health centre for the homeless of the Jenny De la Torre Foundation from 2006 to 2020 (GIG study) aims to explore cross-sectional and longitudinal data from medical records of homeless individuals in Berlin and provide further insights on that subject’s matter. The objective of the present study is to present a study protocol and to describe potential limitations.
Aim of the present study
The main aim of the present study protocol is the description of the objectives, design, methodology and potential limitations of the GIG study. The objectives of the retrospective analysis can be summarised as the following: 1) comprehensive socio-demographic characterisation of patients and 2) detailed description and analysis of health status and medical history (including utilisation of social and medical services). Both are analysed cross-sectional and longitudinal. Evaluation of longitudinal data will include analysis of individual courses (intra-individually for patients with multiple measure points), as well as analysis of trends where cross sections are considered over time (inter-individual analysis). In line with the study design (retrospective analysis of medical records), research questions will be examined in an explorative manner, based on type and quality of data available from medical records (document analysis). Among others, we aim to address the following research questions:
Objective 1
O1a: Characterise the sample by age, education, gender, migration background, insurance status, detention experience, type of accommodation.
O1b: How often is there a change in the homeless status over time? How does the socio-demographic structure change over time?
Objective 2
O2a: Which are the most frequent health problems homeless people face?
O2b: How is the health and social services utilisation among homeless people?
O2c: How often/long are patients receiving care in the health centre?
O2d: Is there a change in health or social challenges during the last years?
O2e: Is there a change in frequency of specific diseases over time?
O2f: Are there associations between extreme social conditions and the health status of individuals?
Methods
Study design
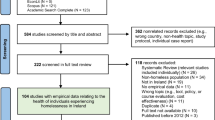
To explore the social and health situation of homeless people in Berlin a retrospective analysis of medical records from the health centre for homeless people of the Jenny De la Torre Foundation will be carried out. An overview of the study design can be obtained from Fig. 1.
Study setting
Data will be obtained from medical records collected and provided by the health centre for homeless people. The health centre provides donation-based and low-threshold medical care for homeless people. The centre includes a medical practice with medical specialists from various areas, a dental practice and an ophthalmic practice. Further, the centre offers psychological and social counselling as well as legal advice within various fields. In addition, two meals per day, clothing and a hairdresser are at the disposal of patients. The centre also offers the service of taking passport photographs. Every individual visiting the health centre has to first check in with the doctor’s office. At the first visit a medical record is generated for each person. Every time individuals visit the health centre, the reason of the visit and utilisation of any service is documented in the medical record. If required, patients may be treated anonymously.
Database and data extraction
Based on the general structure and type of data available from medical records, the main purpose of this step was to build a database structure that allows extracting and entering as much relevant data as possible. Therefore, as part of a preliminary screening, N = 50 randomly selected medical records were screened for content and data availability. Groups and variables are designed under consideration of previous research [49, 50]. As a result, we identified eight different data sources that can be extracted from medical records (see Table 1): 1) floating medical record (a file that contains all information available), 2) social and medical anamnesis (social and medical history of the patient; a standardised form that is filled out by the medical personnel at the first visit), 3) patient information sheet (a standardised form that contains information on any change of the homelessness, health insurance status, as well as the receipt of financial support), 4) doctors letters (including reports and hospital discharge letters), 5) psychological report (patients who make use of the psychological counselling in the centre are documented and a report of the counselling is written by the psychologist), 6) psychiatric record (a medical record about the psychological well-being of a patient), 7) documents provided by the health centre (doctors certificates or sick certificates), and 8) others (any other data available from the medical record). Based on the structure of medical records, a database was created using the software Research Electronic Data Capture (REDCap). REDCap is a browser-based, metadata-driven EDC software for designing research databases. It is secured under data protection law by the Charité – Universitätsmedizin Berlin. The database is accessible online which simplifies the entry of data on site while ensuring data safety and protection. No personal identifying data is collected. During data collection, the survey is pseudonymised. For analysis and presentation of results, anonymised data is used. Data extraction started in July 2020 and will end in July 2022.
Inclusion and exclusion criteria
Every medical record created in the health centre for homeless people from the year 2006 until 2020 will be entered in the database and included in the analysis (N ≈ 3000). There are no other inclusion or exclusion criteria.
Measures
Data will be extracted from medical records and was collected within routine medical care by medical doctors and health care personnel. Data was primarily collected for the purpose of medical care documentation in the health centre. However, a variety of health and social information can be obtained from the medical records. Generally, data can be divided in eight data sources. An overview of all data sources can be obtained from Table 1.
Pretest and quality assurance
After creating a first database, a pretest was conducted to ensure a complete and fully operational data entry. The pretest included N = 55 medical records. Data was entered by two experienced research associates. Data entry was documented and conspicuous differences and needs for adjustment collected. Based on the pretest the database was revised and edited. The new database was again tested with N = 10 medical records. Further, minor changes where implemented, and the data base was finalised. Data will be entered by two trained medical students. For quality insurance, prior to the beginning of data entry, a training on the data base and data collection was conducted with the medical students. Further, a code book for data entry was developed. Regular supervisions and random controls of data entry will be taking place during the entire period of data entry.
Statistical analysis
Total and cross-sectional sample characteristics will be presented in a descriptive analysis using Chi-Square Test, Mann-Whitney-U-Test or independent t-Test as appropriate to test (sub) group differences. The absolute standardised mean difference (ASMD) will be calculated to check the balancing of the characteristics. We consider ASMD< 0.1 as adequate balance between groups. The level of significance will be considered at 0.05. Further, statistical analyses might use finite mixture modelling – particularly latent class analysis – in order to distinguish different types of social and health conditions. We will conduct latent variable regression in order to identify sociodemographic and disease-related factors associated with decreasing health conditions.
By performing latent class analysis collinearity between indicator variables is not a problem, since these procedures are aimed precisely at such configurations and patterns. Latent class analysis explicitly assumes that manifest variables occur in common expressions. In contrast, the usual limitations of conventional regression models apply for exogenous covariates. To increase estimation accuracy, we aim at testing for collinearity between covariates using the following two different approaches. First, a correlation matrix of predictor variables will be calculated. Bivariate correlations larger 0.8 indicate collinearity. Second, we will compute coefficients of determination of each independent variable regressed on the remaining predictor variables to reveal collinear relationships involving more than two variables. Single coefficients of determination being larger than the overall model’s coefficient of determination indicate collinearity [51].
All statistical analyses will be performed using IBM SPSS statistics software (IBM SPSS Statistics for Windows, Version 25.0).
Program governances and ethical approval
The research project will be conducted according to the principles of Good Clinical Practice and the Declaration of Helsinki and was prospectively registered with the German Clinical Trials Register (trial registration number: DRKS00021172). The study received Human Research Ethics Committee approval from Charité – Universitätsmedizin Berlin (EA1/058/20). Further, the GIG study established an independently chaired steering committee prior to the start of data entry. It is comprised of representatives, program funders, board members, service providers engaged in the program, state government and the lead Chief Investigator of the research team. The committee members receive on a regular base short briefings from the research team on the current state of the project and in return, give advice on the research project. Additionally, the committee meets once a year in order to present and discuss the current state of the project. The first meeting already took place via a conference call in June 2020. The next chaired steering meeting will take place in June 2021.
Discussion
Given the number of homeless individuals in Germany, it is of great importance to explore the social and health situation of homeless people in order to better understand challenges and needs as well as work on new health care solution approaches. The present study addresses an important gap in literature as data on this matter is lacking, especially in Germany. The present study has substantial strengths including a secondary database which contains information on the health and social situation of homeless people collected in a health centre for homeless people under naturalistic conditions. Medical record data represent a unique possibility for a better understanding of the health situation and needs of homeless patients. The analysis will be exclusively based on medical record data. However, some medical records are incomplete whereas others are very exhaustive and contain lots of information including material that is not directly related to our research question (for example private pictures or letters of the patients). Another strength includes the study design, as longitudinal data is available for a long period of time (14 years) and for a large, representative population (about 3000 medical records). As no inclusion criteria are applied, a broad range of social and health situations will be analysed, including marginalised groups in research such as women and young patients [48]. Further, a big strength of the present study is the consideration of the course of time for both cross sectional analysis (analysis of trends) and longitudinal analysis (inter and intra individually) of data. This also enables a morbidity analysis. At the very minimum, the compilation and structuring of medical and social information by building categories in order to create an exploratory data base may contribute to the development of standardised instruments in the field of homelessness research [52].
To sum up, homelessness has serious implications for the health of individuals and populations. Based on the findings of the present study we expect to gain a better understanding on the health situation of homeless people in Germany and draw implications for its improvement by adapting services to changes in population demographics and morbidities. In order to improve health care services for homeless people, the further development of multifarious and diverse approaches seem necessary [53]. Thus, we expect the results to reveal a wide range of implications. For example, in a study conducted by Kaduszkiewicz et al. [13] a variety of concrete suggestions such as improving state funding and the range of health services and providing intermediate care centres were discussed. In order to achieve a long-term improvement, we believe it is inevitable to include and examine social policy and structural factors that contribute to or result in homelessness [54].
Limitations
A number of limitations have to be acknowledged. First, the present study is based on a mono-centred survey in the centre of Berlin and therefore under risk of selection bias. The infrastructure of a capital is most of the times better than in regional and smaller cities. Due to the low mobility of homeless people and a frequent word-of-mouth recommendation which reaches only certain communities the health centre likely shows a limited target audience. Further, low-threshold care services for homeless people differ in terms of specific target groups or the scope of (medical) services offered. Reasons are a wild growth of providers, sources of funding or location. Extending the current design to additional health care facilities would contribute to insure findings and reduce the risk of selection bias. Nonetheless, as described earlier the included health care centre is kind of a local ‘maximum provider’ for homeless and uninsured patients. Among the homelessness community the health centre is well known and many shelters and accommodations across Berlin often refer homeless people to the centre. Thus, findings of the present study will contribute to a general better understanding of the health situation and health needs of homeless people and provide impetus beyond local health policy makers. Further, the study’s design and methods including the strength of analysing secondary data collected under naturalistic conditions may serve future health research in hard to reach populations.
Second, due to the unique health and social system in Germany the generalizability of findings will be constrained. This limitation has to be taken into account when interpreting results and comparing them to other health systems and countries. The German health system is not a universal healthcare system. Condition for access to medical services is the existence of a regular health insurance. However, despite standard statutory medical care, there are non-statutory welfare organisations that provide low-threshold universal care, especially for the homeless population. The Jenny De la Torre health centre represent such a low-threshold and free of charge care provider. It plays a key role in the medical care of their homeless patients, as it provides complementary universal care by primary physicians as well as medical specialists from different medical fields and in emergency cases, works together with hospitals in the surrounding area. Therefore, homeless individuals visit the centre for medical advice and care, for both, a short (acute symptoms) or a long (chronical conditions) period of time.
Conclusion
In conclusion, the GIG study will provide a unique and essential insight into social and health care needs of homeless individuals. The results will provide impetus on how to improve the social and health situation of homeless people for both policy makers and health care providers. We regard this research project as an important study for providing knowledge on standardised assessment of homeless peoples social and health conditions. This might be useful for adapting current public health reporting for this vulnerable group. Further, based on the results, we aim to draw conclusions and discuss implications.
Availability of data and materials
Data is stored in a non-publically available repository. Data are however available from the corresponding author on request.
References
Commission to the European Parliament, The Council, The European Economic and Social Committee, The Committee of the Regions. Confronting Homelessness in the European Union. Brussels: European Commission; 2013.
Stafford A, Wood L. Tackling Health Disparities for People Who Are Homeless? Start with Social Determinants. Int J Environ Res Public Health. 2017;14:12.
Busch-Geertsema V. Housing first Europe–results of a European social experimentation project. Eur J Home. 2014;8:1.
Baptista I, Benjaminsen L, Pleace N, Busch-Geertsema V. Counting homeless people in the 2011 housing and population census: EOH comparative studies on homelessness 2. 2012.
Wohnungslosenhilfe B. Pressemitteilung der Bundesarbeitsgemeinschaft Wohnungslosenhilfe e. V. vom 11. November 2019: Kein Ende in Sicht - BAG Wohnungslosenhilfe stellt aktuelle Schätzung für das Jahr 2018 vor 2019.
Hannes H, Bacher F. Obdachlose bekommen mehr Hilfe vom Senat. Tagesspiegel. 2018.
Senatsverwaltung für Integration Arbeit und Soziales. Anzahl der obdachlosen Menschen in Berlin im Jahr 2020. Berlin: Statista; 2020.
Caritasverband für das Erzbistum Berlin e. V., GEBEWO – Soziale Dienste – Berlin gGmbH. Gesundheitsbericht zur Lage der medizinischen und zahnmedizinischen Versorgung obdachloser Menschen 2016. Berlin: 2018.
McLoughlin P, Carey G. Re-framing the links between homelessness and health: insights from the social determinants of health perspective. Parity. 2013;26(10):20–1.
Fitzpatrick S, Bramley G, Johnsen S. Pathways into multiple exclusion homelessness in seven UK cities. Urban Stud. 2012;50(1):148–68.
Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–40.
Gerull S. 1. systematische Lebenslagenuntersuchung wohnungsloser Menschen. 2018.
Kaduszkiewicz H, Bochon B, van den Bussche H, Hansmann-Wiest J, van der Leeden C. The medical treatment of homeless people. Deutsches Arzteblatt Int. 2017;114(40):673–9.
Alagna E, Santangelo OE, Raia DD, Gianfredi V, Provenzano S, Firenze A. Health status, diseases and vaccinations of the homeless in the city of Palermo, Italy. Ann Ig. 2019;31(1):21–34.
Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(11):859–70.
Levorato S, Bocci G, Troiano G, Messina G, Nante N. Health status of homeless persons: a pilot study in the Padua municipal dorm. Ann Ig. 2017;29(1):54–62.
Henwood BF, Lahey J, Rhoades H, Winetrobe H, Wenzel SL. Examining the health status of homeless adults entering permanent supportive housing. J Public Health (Oxf). 2018;40(2):415–8.
Vogel M, Frank A, Choi F, Strehlau V, Nikoo N, Nikoo M, et al. Chronic pain among homeless persons with mental illness. Pain Med. 2017;18(12):2280–8.
Beijer U, Bruce D, Burstrom B. Changes over time in the risk of hospitalization for physical diseases among homeless men and women in Stockholm: a comparison of two cohorts. Scand J Public Health. 2016;44(8):784–90.
Queen AB, Lowrie R, Richardson J, Williamson AE. Multimorbidity, disadvantage, and patient engagement within a specialist homeless health service in the UK: an in-depth study of general practice data. BJGP Open. 2017;1(3):bjgpopen17X100941.
Nielsen SF, Hjorthøj CR, Erlangsen A, Nordentoft M. Psychiatric disorders and mortality among people in homeless shelters in Denmark: a nationwide register-based cohort study. Lancet. 2011;377(9784):2205–14.
Feodor Nilsson S, Laursen TM, Hjorthoj C, Nordentoft M. Homelessness as a predictor of mortality: an 11-year register-based cohort study. Soc Psychiatry Psychiatr Epidemiol. 2018;53(1):63–75.
Vuillermoz C, Aouba A, Grout L, Vandentorren S, Tassin F, Moreno-Betancur M, et al. Mortality among homeless people in France, 2008-10. Eur J Pub Health. 2016;26(6):1028–33.
Schreiter S, Bermpohl F, Krausz M, Leucht S, Rössler W, Schouler-Ocak M, et al. Prävalenzen psychischer Erkrankungen bei wohnungslosen Menschen in Deutschland. Dtsch Arztebl Int. 2017;114(40):665–72.
Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225.
Briner D, Jager M, Kawohl W, Baumgartner-Nietlisbach G. Mental disorder and self-rated health among homeless people in Zurich - first epidemiological data from Switzerland. Psychiatr Prax. 2017;44(6):339–47.
da Silva FP, de Assis Siqueira Paiva F, Guedes CP, da Silva Frazao I, Vasconcelos SC, da Costa Lima MD. Nursing diagnoses of the homeless population in light of self-care theory. Arch Psychiatr Nurs. 2018;32(3):425–31.
Sundin EC, Baguley T. Prevalence of childhood abuse among people who are homeless in Western countries: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2015;50(2):183–94.
Chen JS, Nguyen AH, Malesker MA, Morrow LE. High-risk smoking behaviors and barriers to smoking cessation among homeless individuals. Respir Care. 2016;61(5):640–5.
Hynes F, Kilbride K, Fenton J. A survey of mental disorder in the long-term, rough sleeping, homeless population of inner Dublin. Ir J Psychol Med. 2019;36(1):19–22.
Pribish A, Khalil N, Mhaskar R, Woodard L, Mirza AS. Chronic disease burden of the homeless: a descriptive study of student-run free clinics in Tampa, Florida. J Commun Health. 2019;44(2):249–55.
Fallaize R, Seale JV, Mortin C, Armstrong L, Lovegrove JA. Dietary intake, nutritional status and mental wellbeing of homeless adults in Reading, UK. Br J Nutr. 2017;118(9):707–14.
Lombardi K, Pines JM, Mazer-Amirshahi M, Pourmand A. Findings of a national dataset analysis on the visits of homeless patients to US emergency departments during 2005-2015. Public Health. 2020;178:82–9.
Topolovec-Vranic J, Schuler A, Gozdzik A, Somers J, Bourque PE, Frankish CJ, et al. The high burden of traumatic brain injury and comorbidities amongst homeless adults with mental illness. J Psychiatr Res. 2017;87:53–60.
Nilsson SF, Nordentoft M, Fazel S, Laursen TM. Homelessness and police-recorded crime victimisation: a nationwide, register-based cohort study. Lancet Public Health. 2020;5(6):e333–e41.
Hwang SW, Chambers C, Chiu S, Katic M, Kiss A, Redelmeier DA, et al. A comprehensive assessment of health care utilization among homeless adults under a system of universal health insurance. Am J Public Health. 2013;103(Suppl 2):S294–301.
Elwell-Sutton T, Fok J, Albanese F, Mathie H, Holland R. Factors associated with access to care and healthcare utilization in the homeless population of England. J Public Health (Oxf). 2017;39(1):26–33.
Martin P, Liaw W, Bazemore A, Jetty A, Petterson S, Kushel M. Adults with housing insecurity have worse access to primary and preventive care. J Am Board Fam Med. 2019;32(4):521–30.
D'Ath PJ, Keywood LJ, Styles EC, Wilson CM. East London's homeless: a retrospective review of an eye clinic for homeless people. BMC Health Serv Res. 2016;16:54.
Amato S, Nobay F, Amato DP, Abar B, Adler D. Sick and unsheltered: homelessness as a major risk factor for emergency care utilization. Am J Emerg Med. 2019;37(3):415–20.
Bowen M, Marwick S, Marshall T, Saunders K, Burwood S, Yahyouche A, et al. Multimorbidity and emergency department visits by a homeless population: a database study in specialist general practice. Br J Gen Pract. 2019;69(685):e515–e25.
Figueiredo R, Dempster L, Quiñonez C, Hwang SW. Emergency department use for dental problems among homeless individuals: a population-based cohort study. J Health Care Poor Underserved. 2016;27(2):860–8.
Beaton L, Coles E, Freeman R. Homeless in Scotland: an oral health and psychosocial needs assessment. Dentist J. 2018;6(4):67.
Baptista I, Marlier E. Fighting homelessness and housing exclusion in Europe. A Study of National Policies. Eur Soc Policy Netw (ESPN). 2019:93.
Amore K, Baker M, Howden-Chapman P. The ETHOS definition and classification of homelessness: an analysis. Eur J Home. 2011;5:2.
Edgar B. The ETHOS definition and classification of homelessness and housing exclusion. Euro J Home. 2012;6(2):219–25.
Busch-Geertsema V, Culhane D, Fitzpatrick S. Developing a global framework for conceptualising and measuring homelessness. Habit Int. 2016;55:124–32.
Schindel D, Kleyer C, Schenk L. Somatische Erkrankungen Wohnungsloser in Deutschland. Ein narratives Literaturreview der Jahre 2009–2019. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz 2020.
Brem D. Alt und wohnungslos in München: Eine Untersuchung über Lebenslagen älterer wohnungsloser Männer in einer Notunterkunft. Sozialer Fortschritt. 2012:312–25.
Brem D, Seeberger B. Alt und wohnungslos in Bayern—eine Untersuchung über Lebenslagen von älteren wohnungslosen Männern in betreuten Wohnformen. Sozialer Fortschritt. 2010:209–19.
Mason CH, Perreault WD. Collinearity, power, and interpretation of multiple regression analysis. J Mark Res. 1991;28(3):268–80.
Gordon SJ, Grimmer K, Bradley A, Direen T, Baker N, Marin T, et al. Health assessments and screening tools for adults experiencing homelessness: a systematic review. BMC Public Health. 2019;19(1):994.
Luchenski S, Maguire N, Aldridge RW, Hayward A, Story A, Perri P, et al. What works in inclusion health: overview of effective interventions for marginalised and excluded populations. Lancet. 2018;391(10117):266–80.
Hwang SW, Burns T. Health interventions for people who are homeless. Lancet. 2014;384(9953):1541–7.
Acknowledgements
We would like to thank Elke Matheis for her contribution to the project by creating and reliably editing the database. Further, the authors thank Christine Kleyer for her contribution to the literature background.
Authors’ information (optional)
Not applicable.
Funding
The research is funded by Paritätischer Wohlfahrtsverband Landesverband Berlin e.V. We acknowledge support from the German Research Foundation (DFG) and the Open Access Publication Funds of Charité – Universitätsmedizin Berlin. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
SL was primary contributor to manuscript drafting. LS, JDLT and DS assisted with the writing. LS and DS designed and lead the GIG study. All authors contributed to the present paper and critically revised and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained by the ethics committee of the Charité – Universitätsmedizin Berlin (EA1/058/20).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lech, S., Schenk, L., De la Torre Castro, J. et al. A retrospective analysis of the health and social situation of homeless people in Berlin: study protocol. Arch Public Health 79, 28 (2021). https://doi.org/10.1186/s13690-021-00546-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-021-00546-y