Abstract
Background
Patients presenting with acute hypercapnic respiratory failure due to exacerbations of chronic obstructive pulmonary disease (AECOPD) are typically managed with non-invasive ventilation (NIV). The impact of low-flow extracorporeal carbon dioxide removal (ECCO2R) on outcome in these patients has not been explored in randomised trials.
Methods
Open-label randomised trial comparing NIV (NIV arm) with ECCO2R (ECCO2R arm) in patients with AECOPD at high risk of NIV failure (pH < 7.30 after ≥ 1 h of NIV). The primary endpoint was time to cessation of NIV. Secondary outcomes included device tolerance and complications, changes in arterial blood gases, hospital survival.
Results
Eighteen patients (median age 67.5, IQR (61.5–71) years; median GOLD stage 3 were enrolled (nine in each arm). Time to NIV discontinuation was shorter with ECCO2R (7:00 (6:18–8:30) vs 24:30 (18:15–49:45) h, p = 0.004). Arterial pH was higher with ECCO2R at 4 h post-randomisation (7.35 (7.31–7.37) vs 7.25 (7.21–7.26), p < 0.001). Partial pressure of arterial CO2 (PaCO2) was significantly lower with ECCO2R at 4 h (6.8 (6.2–7.15) vs 8.3 (7.74–9.3) kPa; p = 0.024). Dyspnoea and comfort both rapidly improved with commencement of ECCO2R. There were no severe or life-threatening complications in the study population. There were no episodes of major bleeding or red blood cell transfusion in either group. ICU and hospital length of stay were longer with ECCO2R, and there was no difference in 90-day mortality or functional outcomes at follow-up.
Interpretation
There is evidence of benefit associated with ECCO2R with time to improvement in respiratory acidosis, in respiratory physiology and an immediate improvement in patient comfort and dyspnoea with commencement of ECCO2R. In addition, there was minimal clinically significant adverse events associated with ECCO2R use in patients with AECOPD at risk of failing or not tolerating NIV. However, the ICU and hospital lengths of stay were longer in the ECCO2R for similar outcomes.
Trial registration The trial is prospectively registered on ClinicalTrials.gov: NCT02086084. Registered on 13th March 2014, https://clinicaltrials.gov/ct2/show/NCT02086084?cond=ecco2r&draw=2&rank=8
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease (COPD) is characterized by progressive and not fully reversible expiratory airflow limitation with intermittent acute exacerbations (AECOPD) complicated by hypercapnic respiratory failure (arterial partial pressure of carbon dioxide (PaCO2) > 6.5 kPa (49 mmHg) and pH < 7.35) [1]. In these patients, non-invasive ventilation (NIV) decreases the rate of tracheal intubation [2] and provides a significant survival benefit [2]. However, 15–30% of patients on NIV experience treatment failure and receive invasive mechanical ventilation (IMV) [3]. Reasons for NIV treatment failure include device or mask intolerance, discomfort, or unresolving respiratory acidosis, tachypnoea and respiratory distress [4,5,6]. These patients are at significantly higher risk of death [7].
Extracorporeal carbon dioxide removal (ECCO2R) pumps venous blood through an extracorporeal circuit with a gas exchanging membrane to clear CO2 [8, 9]. ECCO2R has been shown to have physiological benefits in pre-clinical trials [10] and uncontrolled case series in AECOPD [11,12,13]. To date, there have been no randomised controlled trials on the role of ECCO2R in AECOPD. There are 6 further trials currently registered with clinicaltrials.gov [14].
The hypothesis for this trial is that ECCO2R results in faster correction of hypercapnia and earlier cessation of NIV, by at least 12 h. Time to cessation of NIV is an important outcome as longer duration of NIV is associated with greater complications and discomfort—both independent predictors of NIV failure [5, 6].
Methods
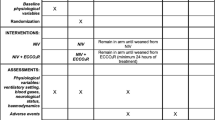
This study was a randomised, open-label, parallel-arm trial comparing standard therapy using NIV (NIV arm) with ECCO2R added to NIV (ECCO2R arm) in adults with AECOPD. Patients were included if they were over 18 years of age, had a history of COPD presenting with AECOPD and with a persisting pH < 7.30 due to hypercapnia after initial medical therapy and at least 1 h of NIV. Patients were randomised following written informed consent by the patient or nominated legal representative. Randomisation was computer-generated and allocation was concealed in opaque, sealed envelopes. Patients were excluded if they had acute multiple organ failure, intolerance, allergy or contraindication to heparin or a contraindication to NIV.
Patients were randomised to continuation of NIV alone or to the addition of ECCO2R to NIV. The full trial methodology has been published [15] (Additional file 1: Appendix S1 and Additional file 2: Figure S1). NIV was delivered using an ICU ventilator in NIV mode (Draeger V500, Germany) with a mask specifically designed for dual limb ventilators (Freemotion, Fisher and Paykel, New Zealand). ECCO2R was delivered using the Hemolung Respiratory Assist System (ALung Technologies, USA). The device has a cross-sectional membrane area of 0.59m2 and has an extracorporeal blood flow between 300 and 500 mL/min. Cannulation was with a dual lumen cannula inserted in either femoral or jugular veins using previously published methods [11]. Membrane VCO2 reported by the device was recorded. This has been previously shown to be consistent with that calculated using trans-membrane blood gases [16]. ECCO2R and heparin were managed in accordance with agreed institutional protocols (Additional file 1: Appendix S1). ECCO2R was weaned as the respiratory failure improved, with a goal of maintaining a respiratory rate of 25 or less and a pH 7.35–7.45. Once the sweep gas flow was reduced to 1L/minute for at least 4 h, the sweep gas was discontinued for 4–12 h. If there were no signs of respiratory failure at this point then the ECCO2R device was stopped and the cannula removed.
The primary outcome was time to discontinuation of NIV. Time to cessation of NIV was based on a combination of patient preference and physiological indicators—improvement in respiratory rate to less than 25 and pH more than 7.35. Short breaks for meals or patient comfort were allowed and did not count as discontinuing NIV. It was estimated that the addition of ECCO2R would reduce NIV duration by at least 12 h. When patients in the NIV arm had ceased NIV they were transferred to the ward the same day. The estimated sample size—1:1 enrolment ratio—was 12 patients in each arm. This would achieve 80% power to reject the null hypothesis of equal means when the population mean difference is 12 h with a standard deviation of 10 h with alpha level of 5% and a loss to follow-up of 10%. The trial was ceased early due to the onset of the SARS-2 Coronavirus pandemic resulting in all non-COVID-19-related research being ceased in the UK.
Secondary outcomes included physiological measurements, ICU and hospital length of stay (LOS) and outcomes (90-day mortality). Adverse outcomes included incidence of major haemorrhage (according to the ISTH bleeding score [17]), thrombosis, haemolysis, mechanical complications and need for IMV. Subjective discomfort and dyspnoea were measured using a visual analogue scale (VAS) (0–100 mm). A higher score indicates greater subjective discomfort or dyspnoea. Quality-of-life measurements, including the COPD assessment test (CAT) [18], the St George’s respiratory questionnaire (SGRQ) [19] and the EuroQuol-5D–5L [20] were administered at the 90-day follow-up visit. Recruitment was ceased by the investigators due to slow recruitment and with the onset of the SARS-CoV-2 pandemic leading to the cessation of all non-COVID research in critical care in the NHS.
Ethical approval
The trial protocol was approved by the Cambridge NHS Human Research Authority Research Ethics Committee (14/EE/0109).
Statistics
Statistical analysis was performed using Prism 9.1.1 for Mac (GraphPad, San Diego, USA). All data is presented as median (inter-quartile range). Data was tested for normal distribution using a Kolmogorov–Smirnov test and presented as median (inter-quartile range). Inter-group differences with continuous unpaired, non-parametric data were compared using a Mann–Whitney U test. Inter-group differences with discrete paired, non-parametric data were compared using a Wilcoxon matched pairs signed rank test. Intra-group differences over time with continuous, parametric data were compared using a one-way ANOVA with Dunnett’s correction for post-hoc comparisons. Intra-group differences over time with continuous non-parametric data were compared using Friedman’s test with Dunnett’s correction for post-hoc comparisons. Categorical data were compared using a Chi-squared analysis. Survival was analysed using a log-rank test. Statistical significance was defined as p < 0.05.
Results
Baseline characteristics
Between December 2017 and March 2020, 261 potentially eligible patients were screened, 32 patients met inclusion criteria, 18 consented and were randomised (Fig. 1). Nine were randomised to each group (Table 1). All patients had severe COPD (median GOLD stage 3 in both groups), but no patients were receiving chronic domiciliary ventilation. Two were lost to follow-up, one from each group, and were considered alive for the analysis (data from the UK NHS database). Patients in both groups were comparable although baseline respiratory rate was higher with ECCO2R (24 [20–28] vs 29 [26–32] breaths/min, p < 0.05), haemoglobin was higher with ECCO2R (130 (120–136) vs 151(143–157) g/L p < 0.05), as was c-reactive protein (13 (3.5–16) vs 32 (30–51) mg/L, p < 0.05).
ECCO2R
All patients were cannulated via the femoral vein by patient choice as they preferred to not lie flat for jugular insertion. Blood and sweep flow rates were all within the operating range of the device (Additional file 3: Table S6). ECCO2R was ceased after a median (IQR) of 96 (60–138) h following successful weaning for all patients. CO2 clearance through the membrane lung (VCO2ML) was a median of 88 (83–104) mL/min in the first hour and was maintained during the first 48 h (Additional file 3: Table S6).
Physiological changes post-randomisation
Levels of respiratory support did not differ between groups (Additional file 3: Table S1). The respiratory rate was higher with ECCO2R compared with NIV at baseline and 12 h post randomisation (22(20–24) vs 17 (15–19) breaths/min, p = 0.038) (Fig. 2a, Additional file 3: Table S1). There was no significant difference in respiratory rate over the first 48 h with NIV (Fig. 2a, Additional file 3: Table S1). There was, however, a significant reduction in respiratory rate with ECCO2R compared to baseline at four (22 (20–25) vs 29 (26–32) breaths/min, p = 0.039), eight (20 (20–22) vs 29 (26–32) breaths/min, p = 0.015), twelve (22 (20–24) vs 29 (26–32) breaths/min, p = 0.015), 24 (21 (20–23) vs 29 (26–32) breaths/min, p = 0.039) and 48 h (17 (16–23) vs 29 (26–32) breaths/min, p = 0.015).
Respiratory rate, arterial pH and PaCO2 over the first 48 h. a: Respiratory rate over the first 48 h (* statistically significant difference between the NIV and ECCO2R groups (p < 0.05); ^ statistically significant difference over time in the ECCO2R group compared with baseline (time 0) (p < 0.05)); b: Arterial pH over the first 48 h (* statistically significant difference between the NIV and ECCO2R groups (p < 0.05); ^ statistically significant difference over time in the ECCO2R group compared with baseline (time 0) (p < 0.05); # statistically significant difference over time in the NIV group compared with baseline (time 0) (p < 0.05)); c: PaCO2 over the first 48 h (* statistically significant difference between the NIV and ECCO2R groups (p < 0.05); ^ statistically significant difference over time in the ECCO2R group compared with baseline (time 0) (p < 0.05); # statistically significant difference over time in the NIV group compared with baseline (time 0) (p < 0.05))
Arterial pH was not significantly different between the two groups (Fig. 2b, Additional file 3: Table S1). With ECCO2R, the arterial pH in was significantly higher than baseline at each timepoint for the first 48 h (Fig. 2b, Additional file 3: Table S1). With NIV, the arterial pH was significantly higher than baseline at 8 h (7.32 (7.28–7.33) vs 7.27 (7.21–7.27), p = 0.022) and remained significantly higher at 12 and 24 h (Fig. 2b).
Partial pressure of arterial CO2 (PaCO2) was significantly lower with ECCO2R compared with NIV at 4 h (6.8 (6.2–7.15) vs 8.3 (7.74–9.3) kPa; p = 0.024) following randomisation (Fig. 2c). With ECCO2R, the arterial CO2 was significantly lower than baseline at each timepoint for the first 48 h. With NIV, the arterial CO2 was not statistically different to baseline at any timepoint in the first 48 h.
Time on NIV
Four patients in the NIV arm ceased NIV against the treating clinician’s advice. Median time from randomisation to cannulation and commencing ECCO2R was 2:27 (1:22–2:50) h (Table 2). Time from randomisation to pH > 7.35 was significantly lower with ECCO2R (5:32 (3:39–11:48) vs 23:58 (22:48–26:55) h, p = 0.024). Time to NIV discontinuation was significantly shorter with ECCO2R (7:00 (6:18–8:30) vs 24:30 (18:15–49:45) h, p = 0.004) (Table 2, Fig. 3a).
Subjective discomfort and dyspnoea
ECCO2R resulted in a rapid and significant reduction in VAS for discomfort (84 (78–87) vs 13 (4–65), p = 0.0156) and dyspnoea (85 (80–87) vs 20 (7–52), p < 0.01). There were no significant differences between ECCO2R and NIV in either dyspnoea or discomfort at any timepoint. The discomfort and dyspnoea scores did not change between days 1 and 2 for NIV or ECCO2R (Fig. 4, Additional file 3: Table S2).
Biochemistry and haematology data
Haematological, biochemical and coagulation parameters over the first 2 days are described (Additional file 3: Table S3). Serum bilirubin levels were significantly higher with ECCO2R compared with NIV at day 2 (14 (10–22) vs 5 (4.5–7.5) umol/L; p = 0.013). The platelet count was lower with ECCO2R compared with NIV at day 2 (96 (73–124) vs 225 (169–244) × 109/L; p = 0.044) and baseline (96 (73–124) vs 204 (163–308) × 109/L, p = 0.0001). Fibrinogen remained significantly higher with ECCO2R compared with NIV at baseline (4.3 (4.1–5) vs 2.2 (1.5–2.3) g/L, p < 0.001), days 1 and 2. APTTr was significantly higher with ECCO2R, who were on a heparin infusion at day 2 (1 (1–1.1) vs 1.6 (1.4–2.7), p = 0.0013).
Complications
There were no severe or life-threatening complications in either group. The number of complications related to NIV was higher than ECCO2R (Additional file 3: Table S4). The majority of NIV-related complications were due to discomfort. Four patients stopped NIV due to discomfort, no patients stopped ECCO2R. There were no patient complications related to cannulation for ECCO2R. There was one ECCO2R cannula which thrombosed prior to commencement of ECCO2R and was changed without adverse incident. There was no major bleeding in either group. No patient required red blood cell transfusion. One patient with ECCO2R received a pool of platelets. No patient in either group underwent IMV, while they were on therapy. One patient who had received ECCO2R required IMV later in the hospital stay due to development of a hospital acquired pneumonia.
Length of stay
The ICU and hospital LOS were significantly longer with ECCO2R than NIV (161:45 (132:27–174:50) vs 45:49 (40:22–53:00) h, p = 0.001 and 240:00 (219:52–337:31) vs 124:00 (103:38–213:15) h, p = 0.014).
90-day survival and symptoms at follow-up
Survival with ECCO2R was 6/9 (ICU), 6/9 (hospital) and 5/9 at 90-day follow-up. Survival with NIV was 9/9 (ICU), 8/9 (hospital) and 7/9 at 90-day follow-up. There was no difference in survival between NIV and ECCO2R at any timepoint out to 90 days (Fig. 3b, Additional file 3: Table S5).
The CAT (NIV: 22.5 (19.3–27.3), ECCO2R 26 (20–28)) and SGRQ (NIV: 71 (49.7–77.5), ECCO2R: 55.3 (54.3–64.9)) were similar at follow-up. EuroQoL 5D–5L VAS was no different (NIV: 37.5 (21.25–50), ECCO2R: 45 (36.25–55)).
Discussion
The data shows that in patients with hypercapnic respiratory failure due to AECOPD, addition of ECCO2R to NIV leads to faster resolution of hypercapnia and tachypnoea, a significant improvement in dyspnoea and discomfort and earlier NIV discontinuation. The study demonstrates that ECCO2R is safe, feasible and could be commenced within 2 h of randomisation. ICU and hospital LOS were both significantly longer with ECCO2R.
This study has demonstrated an earlier normalisation of arterial pH with ECCO2R compared with NIV by more than 18 h. Given that four patients in the NIV arm withdrew from NIV against treating clinician’s advice, it is possible that this is an underestimate. The improvement in respiratory acidosis is consistent with results from observational studies exploring ECCO2R [11,12,13, 21]. In this study we report that ECCO2R led to a significant reduction in respiratory rate with at 8 h, while there was no reduction in respiratory rate with NIV over the first 48 h. Other studies have demonstrated a reduction in respiratory rate associated with ECCO2R between 1 and 24 h after commencement [11, 21]. Despite randomisation there was a difference in baseline respiratory rate between the two groups and it is possible that this contributed to the apparent improvement in respiratory rate in the first few hours after commencing ECCO2R.
The optimal blood flow rate for provision of ECCO2R is currently a subject of significant debate, with physiological evidence clearly demonstrating that higher blood flow rates are associated with greater CO2 clearance with a maximum sweep flow to blood flow ratio (i.e., membrane ventilation:perfusion) of 10:1 [16, 22,23,24,25,26]. In the present study, the blood flow was a median of 400 mL/min and the improvement in respiratory rate and acidosis suggests that in AECOPD in spontaneously breathing patients, removing CO2 at an average rate of ~ 90 mL/minute (roughly equivalent 30–40% of the theoretical total CO2 production of ~ 3 mL/kg/minute) was clinically meaningful.
Adverse consequences of NIV included significant discomfort (13/18 (72.2%) patients), consistent with other reports [4, 27]. This contributed to the withdrawal of NIV in 4/9 (44.4%) of the NIV group despite having persisting respiratory acidosis. By comparison, no patients with ECCO2R requested withdrawal of treatment and only one patient reported discomfort associated with the cannula insertion site.
ECCO2R was associated with significant and sustained improvements in dyspnoea and discomfort (Fig. 4) as measured by the VAS [28]. Dyspnoea is a complex symptom which is incompletely understood but likely relates to the neurological impact of hypoxia and hypercapnia within the brainstem as well as respiratory muscle activity [29]. Given the relationship between hypercapnia and dyspnoea, it is plausible that this resulted from the impact of ECCO2R on arterial CO2 and pH.
In keeping with other studies, adverse consequences of ECCO2R included development of hyperbilirubinaemia and thrombocytopaenia at day 2 [11,12,13, 30]. Thrombocytopaenia is commonly associated with pumped extracorporeal circuits [31]. The underlying mechanisms are incompletely understood, but may relate to platelet damage as blood transits the pump [31]. Hyperbilirubinaemia is thought to be due to red cell injury and the increase in free haemoglobin supports this [31]. Blood trauma has been linked to blood flow rates of 1L/minute or less blood flow rates, pump revolutions per minute over 3000 and negative pressures, all of which are limitations of the technique [32, 33]. Fibrinogen levels were significantly elevated with ECCO2R. Both hypo- and hyperfibrinogenaemia have been reported in patients requiring extracorporeal support and mechanisms are incompletely understood [30, 34]. Despite changes in platelets and fibrinogen and evidence of haemolysis there were no episodes of significant bleeding or thrombosis with ECCO2R and no need for blood transfusion. Other studies have shown a significant risk of bleeding with ECCO2R [21], possibly due to endothelial dysfunction contributed to by both the underlying disease and the circuit [35]. Other complications relating to ECCO2R included minor site bleeding, circuit/cannula thrombosis and one device failure and these plus the need for anticoagulation remain a limitation of the technique [30].
There is benefit for early rehabilitation in critical illness [1, 36]. It is, therefore, a little concerning that although the time to rehabilitation was did not reach statistical significance, it was numerically longer. This may be due to the route of cannulation and familiarity with mobilization with femoral cannulation. The importance of rehabilitation should be considered in future trials.
ICU and hospital lengths of stay were both 4–5 days longer with ECCO2R than with NIV. This was due to a longer ICU LOS—time from ICU discharge to home discharge was equal in both groups. This compares with other retrospective work which has found that the ICU LOS was shorter with ECCO2R compared with invasive mechanical ventilation [37]. The longer ICU stay is contributed by the differences in the protocolised care between the techniques. With NIV, nurse-led weaning occurred 24/7, based around arterial blood gases, respiratory rate and patient preference. Patients were discharged to the ward during daytime if they had been off NIV overnight. In addition, patients who consistently declined NIV (4/9) were discharged to a ward bed regardless of pH and this will have contributed to the lower ICU length of stay in the NIV arm. The protocol for patients receiving ECCO2R did not allow weaning overnight. There was a median of 8 h [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24] from cessation of ECCO2R to decannulation and unit protocols required a further overnight stay for observation. ICU, hospital and 90-day mortality were not significantly different between groups; however, the study was not powered to detect a mortality difference. All in-hospital deaths were due to the underlying disease. Results of the CAT, SGRQ and EuroQoL 5D–5L index were not significantly different between groups and indicate that patients in both groups had significantly impaired health-related quality of life at follow-up [38].
This study is limited by the small sample size of only nine in each group, 3 patients short of the planned enrolment in each group. Despite this the primary end point of a reduction in time to cessation of NIV of at least 12 h was met. Despite randomisation there were baseline differences between groups, notably a higher respiratory rate, haemoglobin and C-reactive protein with ECCO2R. The withdrawal from NIV by four patients in the NIV arm led to an earlier reduction in NIV than would have been advised by the treating clinical team and resulted in earlier than expected discharge of patients from ICU at this point. These differences could have contributed to the study results and there could have been further, unmeasured differences between groups. It is possible that the higher respiratory rate at baseline led to the apparent improvement in the ECCO2R group. The small size limits the interpretation of the adverse consequences of ECCO2R as less common adverse consequences would not have been detected. Only one device was used with a 400 mL blood flow and consequently we cannot comment whether this is the optimal blood flow for management of patients with AECOPD.
The study’s strengths are that it is the first randomised, controlled trial of ECCO2R in a population of patients with severe COPD and severe exacerbations and powered to physiological endpoints.
Conclusions
There is evidence of benefit associated with ECCO2R with time to improvement in respiratory acidosis, improvement in respiratory physiology from baseline and an immediate improvement in patient comfort and dyspnoea with commencement of ECCO2R and minimal clinically significant adverse events associated with its use in a population of patients with AECOPD at risk of failing or not tolerating NIV. However, the ICU and hospital lengths of stay were longer in the ECCO2R for similar outcomes.
Availability of data and materials
The data sets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AECOPD:
-
Acute exacerbations of chronic obstructive pulmonary disease
- ECCO2R:
-
Extracorporeal CO2 removal
- IMV:
-
Invasive mechanical ventilation
- NIV:
-
Non-invasive ventilation
- PaCO2 :
-
Partial arterial pressure of carbon dioxide
References
Davidson AC, Banham S, Elliott M, Kennedy D, Gelder C, Glossop A, et al. BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults. Thorax. 2016;71(Suppl 2):1–35.
Osadnik CR, Tee VS, Carson-Chahhoud KV, Picot J, Wedzicha JA, Smith BJ. Non-invasive ventilation for the management of acute hypercapnic respiratory failure due to exacerbation of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017;7:004104.
Ozsancak Ugurlu A, Habesoglu MA. Epidemiology of NIV for Acute Respiratory Failure in COPD Patients: Results from the International Surveys vs. the “Real World.” COPD. 2017;14(4):429–38.
Plant PK, Owen JL, Elliott MW. Non-invasive ventilation in acute exacerbations of chronic obstructive pulmonary disease: long term survival and predictors of in-hospital outcome. Thorax. 2001;56(9):708–12.
Ozyilmaz E, Ugurlu AO, Nava S. Timing of noninvasive ventilation failure: causes, risk factors, and potential remedies. BMC Pulm Med. 2014;14:19.
Steriade AT, Johari S, Sargarovschi N, Necula D, Tudose CE, Ionita D, et al. Predictors of outcome of noninvasive ventilation in severe COPD exacerbation. BMC Pulm Med. 2019;19(1):131.
Martin-Gonzalez F, Gonzalez-Robledo J, Sanchez-Hernandez F, Moreno-Garcia MN, Barreda-Mellado I. Effectiveness and predictors of failure of noninvasive mechanical ventilation in acute respiratory failure. Med Intensiva. 2016;40(1):9–17.
Barrett NA, Camporota L. The evolving role and practical application of extracorporeal carbon dioxide removal in critical care. Crit Care Resusc. 2017;19(Suppl 1):62–7.
Camporota L, Barrett N. Current applications for the use of extracorporeal carbon dioxide removal in critically ill patients. Biomed Res Int. 2016;2016:9781695.
Batchinsky AI, Jordan BS, Regn D, Necsoiu C, Federspiel WJ, Morris MJ, et al. Respiratory dialysis: reduction in dependence on mechanical ventilation by venovenous extracorporeal CO2 removal. Crit Care Med. 2011;39(6):1382–7.
Moss CE, Galtrey EJ, Camporota L, Meadows C, Gillon S, Ioannou N, et al. A Retrospective Observational Case Series of Low-Flow Venovenous Extracorporeal Carbon Dioxide Removal Use in Patients with Respiratory Failure. ASAIO J. 2016;62(4):458–62.
Kluge S, Braune SA, Engel M, Nierhaus A, Frings D, Ebelt H, et al. Avoiding invasive mechanical ventilation by extracorporeal carbon dioxide removal in patients failing noninvasive ventilation. Intensive Care Med. 2012;38(10):1632–9.
Burki NK, Mani RK, Herth FJ, Schmidt W, Teschler H, Bonin F, et al. A novel extracorporeal CO(2) removal system: results of a pilot study of hypercapnic respiratory failure in patients with COPD. Chest. 2013;143(3):678–86.
Tonetti T, Pisani L, Cavalli I, Vega ML, Maietti E, Filippini C, et al. Extracorporeal carbon dioxide removal for treatment of exacerbated chronic obstructive pulmonary disease (ORION): study protocol for a randomised controlled trial. Trials. 2021;22(1):718.
Barrett NA, Kostakou E, Hart N, Douiri A, Camporota L. Extracorporeal carbon dioxide removal for acute hypercapnic exacerbations of chronic obstructive pulmonary disease: study protocol for a randomised controlled trial. Trials. 2019;20(1):465.
Barrett NA, Hart N, Camporota L. In-vitro performance of a low flow extracorporeal carbon dioxide removal circuit. Perfusion. 2020;35(3):227–35.
Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–4.
Jones PW, Harding G, Berry P, Wiklund I, Chen W-H, Kline LN. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–54.
Jones PW, Quirk FH, Baveystock CM. The St George's Respiratory Questionnaire. Resp Med. 1991;85(Suppl B):25–31; discussion 3–7.
Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ. 2018;27(1):7–22.
Braune S, Sieweke A, Brettner F, Staudinger T, Joannidis M, Verbrugge S, et al. The feasibility and safety of extracorporeal carbon dioxide removal to avoid intubation in patients with COPD unresponsive to noninvasive ventilation for acute hypercapnic respiratory failure (ECLAIR study): multicentre case-control study. Intensive Care Med. 2016;42(9):1437–44.
Karagiannidis C, Strassmann S, Brodie D, Ritter P, Larsson A, Borchardt R, et al. Impact of membrane lung surface area and blood flow on extracorporeal CO2 removal during severe respiratory acidosis. Intensive Care Med Exp. 2017;5(1):34.
Strassmann S, Merten M, Schafer S, de Moll J, Brodie D, Larsson A, et al. Impact of sweep gas flow on extracorporeal CO2 removal (ECCO2R). Intensive Care Med Exp. 2019;7(1):17.
Karagiannidis C, Kampe KA, Sipmann FS, Larsson A, Hedenstierna G, Windisch W, et al. Veno-venous extracorporeal CO2 removal for the treatment of severe respiratory acidosis: pathophysiological and technical considerations. Crit Care (London, England). 2014;18(3):R124.
Gross-Hardt S, Hesselmann F, Arens J, Steinseifer U, Vercaemst L, Windisch W, et al. Low-flow assessment of current ECMO/ECCO(2)R rotary blood pumps and the potential effect on hemocompatibility. Crit Care (London, England). 2019;23(1):348.
Barrett NA, Hart N, Camporota L. In vivo carbon dioxide clearance of a low-flow extracorporeal carbon dioxide removal circuit in patients with acute exacerbations of chronic obstructive pulmonary disease. Perfusion. 2020;35(5):436–41.
Carron M, Freo U, BaHammam AS, Dellweg D, Guarracino F, Cosentini R, et al. Complications of non-invasive ventilation techniques: a comprehensive qualitative review of randomized trials. Br J Anaesth. 2013;110(6):896–914.
Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society. Am J Resp Crit Care Med. 1999;159(1):321–40.
O’Donnell DE, Ora J, Webb KA, Laveneziana P, Jensen D. Mechanisms of activity-related dyspnea in pulmonary diseases. Respir Physiol Neurobiol. 2009;167(1):116–32.
Combes A, Fanelli V, Pham T, Ranieri VM. Feasibility and safety of extracorporeal CO2 removal to enhance protective ventilation in acute respiratory distress syndrome: the SUPERNOVA study. Intensive Care Med. 2019.
Chandler WL. Platelet, Red Cell, and Endothelial Activation and Injury During Extracorporeal Membrane Oxygenation. ASAIO J. 2021.
Schöps M, Groß-Hardt SH, Schmitz-Rode T, Steinseifer U, Brodie D, Clauser JC, et al. Hemolysis at low blood flow rates: in-vitro and in-silico evaluation of a centrifugal blood pump. J Transl Med. 2021;19(1):2.
Toomasian JM, Bartlett RH. Hemolysis and ECMO pumps in the 21st Century. Perfusion. 2011;26(1):5–6.
Doyle AJ, Hunt BJ, Sanderson B, Zhang J, Mak SM, Benedetti G, et al. A comparison of thrombosis and hemorrhage rates in patients with severe respiratory failure due to coronavirus disease 2019 and influenza requiring extracorporeal membrane oxygenation. Crit Care Med. 2021.
Diehl JL, Augy JL, Rivet N, Guerin C, Chocron R, Smadja DM. Severity of endothelial dysfunction is associated with the occurrence of hemorrhagic complications in COPD patients treated by extracorporeal CO(2) removal. Intensive Care Med. 2020;46(10):1950–2.
Hashem MD, Parker AM, Needham DM. Early Mobilization and rehabilitation of patients who are critically ill. Chest. 2016;150(3):722–31.
Braune S, Burchardi H, Engel M, Nierhaus A, Ebelt H, Metschke M, et al. The use of extracorporeal carbon dioxide removal to avoid intubation in patients failing non-invasive ventilation–a cost analysis. BMC Anesthesiol. 2015;15:160.
Morishita-Katsu M, Nishimura K, Taniguchi H, Kimura T, Kondoh Y, Kataoka K, et al. The COPD assessment test and St George’s Respiratory Questionnaire: are they equivalent in subjects with COPD? Int J Chron Obstruct Pulmon Dis. 2016;11:1543–51.
Acknowledgements
The authors would like to acknowledge the work of the research and clinical nurses who cared for the patients at each institution.
Funding
The study was funded by ALung Inc, Pittsburgh, USA. The funder had no role in the design of the study, data collection, analysis and interpretation of data or in writing the manuscript. The study was investigator-led, academically sponsored (Guy’s and St Thomas’ NHS Foundation Trust) and industry funded (ALung Technologies Inc, Pittsburgh, USA). The funder was not involved in the design, conduct, analysis or reporting of the study.
Author information
Authors and Affiliations
Contributions
All authors contributed to drafting the work or revising it critically for important intellectual content; and gave final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. NB contributed to conception and design of the work; and the acquisition, analysis, and interpretation of data for the work; NH contributed to conception and design of the work; and the analysis, and interpretation of data for the work; KJR contributed to acquisition of data for the work; MM contributed to acquisition of data for the work; EK contributed to acquisition of data for the work; CC contributed to the acquisition, analysis, and interpretation of data for the work; SL contributed to the acquisition, analysis, and interpretation of data for the work; SS contributed to the acquisition, analysis, and interpretation of data for the work; AB contributed to the acquisition, analysis, and interpretation of data for the work; AD contributed to design of the work; and the acquisition, analysis, and interpretation of data for the work; LC contributed to conception and design of the work; and the acquisition, analysis, and interpretation of data for the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The trial protocol was approved by the Cambridge NHS Human Research Authority Research Ethics Committee (14/EE/0109). Patients or their designated next of kin provided written informed consent prior to randomisation.
Consent for publication
Not applicable.
Competing interests
NB’s institution has received research funding from ALung Inc. The authors declare that they have no other competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1 Appendix S1.
Clinical guideline.

Additional file 2: Figure S1.
Study workflow showing the elements which impacted patient care in both arms.
Additional file 3.
Additional tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barrett, N.A., Hart, N., Daly, K.J.R. et al. A randomised controlled trial of non-invasive ventilation compared with extracorporeal carbon dioxide removal for acute hypercapnic exacerbations of chronic obstructive pulmonary disease. Ann. Intensive Care 12, 36 (2022). https://doi.org/10.1186/s13613-022-01006-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-022-01006-8