Abstract
Background
Intravenous crystalloid solutions are administered commonly for critically ill patients. We performed this meta-analysis of randomized trials with trial sequential analysis (TSA) to evaluate effects of chloride content of intravenous crystalloid solutions on clinical outcomes among critically ill adult patients.
Methods
Electronic databases were searched up to June 1, 2018, for randomized trials of use of balanced crystalloids versus 0.9% saline solutions in critically ill adult patients. The outcome variables included mortality, renal outcomes, serum content alterations and organ function. Subgroup analysis was conducted according to patient settings, types or volume of crystalloid fluid, or among sepsis versus non-sepsis, TBI versus non-TBI or subpopulations by the categories of baseline kidney function. Random errors were evaluated by trial sequential analysis.
Results
Eight studies with 19,301 patients were analyzed. A trend of in-hospital survival benefit with no statistical difference could be observed with balanced crystalloids compared with 0.9% saline (RR 0.92, 95% CI 0.85–1.0, p = 0.06). The use of balanced crystalloid solutions was associated with longer RRT-free days (SMD 0.09, 95% CI 0.06–0.12, p < 0.001), less risk of increase in serum concentrations of chloride (SMD − 1.23, 95% CI − 1.59 to − 0.87, p < 0.001) and sodium (SMD − 1.28, 95% CI − 1.65 to − 0.92, p < 0.001), less risk of decline in serum base deficit (SMD − 0.58, 95% CI − 0.98 to − 0.18, p = 0.004), longer ventilator-free days (SMD 0.08, 95% CI 0.05–0.11, p < 0.001) and vasopressor-free days (SMD 0.04, 95% CI 0.00–0.07, p = 0.02). Subgroup analysis showed that balanced crystalloid solutions were associated with a reduced in-hospital mortality rate among septic patients (RR 0.86, 95% CI 0.75–0.98; p = 0.02) and non-traumatic brain injury patients (RR 0.90, 95% CI 0.82–0.99, p = 0.02), while the TSA results indicated a larger sample size is still in need.
Conclusions
Limited evidence supported statistical survival benefit with balanced crystalloid solutions, while it benefited in reducing organ support duration and fluctuations in serum electrolyte and base excess and was associated with decreased in-hospital mortality in subpopulation with sepsis and non-TBI. Large-scale rigorous randomized trials with better designs are needed to provide robust evidence for clinical management.
Trial registration The protocol for this meta-analysis was registered on PROSPERO: International prospective register of systematic reviews (CRD42018102661), https://www.crd.york.ac.uk/prospero/#recordDetails
Similar content being viewed by others
Background
Intravenous crystalloid solutions are administered commonly in critical care unit, especially for patients with need of resuscitation. Crystalloid solutions as the fluid of choice for initial resuscitation and subsequent intravascular volume replacement in patients with sepsis and septic shock were recommended in guidelines for management of sepsis and septic shock published in 2016 [1]. Resuscitation with large volumes of crystalloid solutions with non-physiological content may lead to electrolyte disturbance and hyperchloremic metabolic acidosis which could result in severe renal, cardiac or hepatic disease. Different component electrolytes of the crystalloid solutions interact with the body’s internal equilibrium [2].
0.9% saline solutions have been the most commonly administered intravenous fluid. Since first developed by adding the buffer lactate to Ringer’s solution in the 19th century, balanced crystalloid solutions such as (Plasma-Lyte 148, lactated or acetate Ringer) have been preferable alternative for relatively physiological concentrations of ions [3,4,5]. Data suggest that 0.9% saline can increase the risk of hyperchloremic metabolic acidosis and related complications, such as acute kidney injury: One before and after prospective trial has shown the beneficial effects of chloride-restrictive intravenous fluid in the improvement of preventing acute kidney injury (AKI) and decreasing use of renal replacement therapy (RRT) in critically ill patients [6]. In addition, saline administration has been proved to result in reductions in renal blood flow velocity and renal cortical tissue perfusion following sustained hyperchloremia compared with Plasma-Lyte 148 in healthy adults [7]. For critically ill patients, it should be more cautious when choosing crystalloid fluid type for initial resuscitation and subsequent intravascular volume maintenance. However, 2016 Surviving Sepsis Campaign (SSC) guidelines could not provide recommendations for the use between normal saline of supraphysiological chloride content and balanced salt solution of low chloride content with indirect low-quality evidence from observational or retrospective studies [1, 8, 9].
A recent large pragmatic trial suggested balanced crystalloid fluid administration in critically ill adults compared with use of 0.9% saline could decrease incidence of a major adverse kidney event within 30 days [10] rather than mortality or other renal-related outcomes. Effects of chloride content of intravenous crystalloid solutions in critically ill patients were still controversial. Therefore, the objective of this meta-analysis with trial sequential analysis (TSA) was to evaluate effects of balanced crystalloids compared to controls with 0.9% saline on mortality and renal outcomes for critically ill adult patients, with which minor differences might be detected in patient outcomes with statistical power, providing the hint for clinical practice.
Methods
Approval
There is no requirement for ethical approval, and patient consent for this meta-analysis is based on previous published studies. The protocol for this meta-analysis was registered on PROSPERO: International prospective register of systematic reviews (CRD42018102661).
Search strategy and study selection
We conducted a search for randomized trials in the following databases until June 2018: Medline, EMBASE, Cochrane (Central) database, Elsevier, Web of Science and ClinicalTrials.gov. The details of search strategy were as the meta-analysis by Kawano-Dourado used [11], shown in Additional file 1. There was no language restriction.
The titles and abstracts were screened to determine whether a study should be included by two reviewers (MX and FL) independently. Then, the full texts were reviewed according to the inclusion and exclusion criteria. Any discrepancies were resolved by a consensus on the inclusion or exclusion of a study after a discussion with a third reviewer.
Inclusion and exclusion criteria
We included trials with the following features:
-
1.
Type of study: randomized controlled trials and cluster randomized trials.
-
2.
Population: Acutely ill adult patients in the ICU or surgical adult patients transferred to ICU in the perioperative period.
-
3.
Intervention: balanced crystalloid fluid characterized by a near-physiological chloride concentration (ion concentration 111 mmol/l or less, including Plasma-Lyte 148, lactated or acetate Ringers), given intravenously for resuscitation or maintenance.
-
4.
Control: 0.9% saline solution works as control group with relatively high chloride content for fluid resuscitation or maintenance.
-
5.
Outcomes: The primary outcome was in-hospital mortality. The secondary outcomes were renal outcomes including new RRT use, stage 2 or higher AKI development according to kidney disease: improving global outcomes (KDIGO) criterion [12] after enrollment, RRT-free days and the incidence of MAKE30 [10]; the change of serum content concentrations including chloride, sodium, pH value, bicarbonate and base acid; mechanical ventilation (MV) use, MV-free days and vasopressor-free days.
We excluded trials with the following features:
-
1.
If they made the comparisons between crystalloids versus colloids, hypertonic saline versus balanced solutions, or among solutions with different colloid components, to minimize the confounding factors and make sure the difference between the experimental and control groups involved a buffer in the solution (usually lactate and/or acetate).
-
2.
If they were involved with the patients receiving renal transplantation.
Data extraction and synthesis
All available data including characteristics of the selected studies, details of the population enrolled, details of the intervention including type of crystalloid fluid, volume and duration and details of the predefined primary outcome were independently extracted by two investigators (MX and FL). Disagreements between the two investigators were resolved by a consensus after discussing with a third reviewer (XZ).
Quality assessment
We summarized the evidence by evaluating design, quality, consistency, precision, directness and possible publication bias of the included studies in accordance with the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (high, moderate, low and very low) [13].
Statistical analysis
Data were conducted by RevMan 5.3 software according to the Cochrane Handbook. Mantel–Haenszel (M–H) Chi-square test and the I2 test were used to assess the statistical heterogeneity and inconsistency in RevMan 5.3 [14]. A p value < 0.10 was predefined as the statistically significant heterogeneity in the M–H Chi-square test, while I2 index was used to assess heterogeneity in the meta-analysis. Higgins and colleagues proposed 25%, 50% and 75% of I2 values would mean low, medium and high heterogeneity, respectively [14]. Both the fixed and random models were used to report the data. A risk ratio (RR) with 95% confidence interval (CI) for the dichotomous data and standardized mean differences (SMD) with 95% CI for the continuous data were reported. The visual inspection of the funnel plot was established to evaluate the publication bias by RevMan 5.3 software (The Nordic Cochrane Centre, Rigshospitalet, Copenhagen, Denmark) according to the Cochrane Handbook [15].
Predefined subgroup analysis was conducted comparing patients setting (ICU versus transferred to ICU in perioperative period), crystalloid fluid type (lactated Ringers, Plasma-Lyte or mixed of both) and fluid volume (mean or median volume above versus < 5 L). To investigate the potential sources of heterogeneity, we performed post hoc analyses according to specific patients. Patients were classified into sepsis and non-sepsis, TBI and non-TBI or subpopulations according to the categories of baseline kidney function by Semler study in 2018 [10]: normal kidney function, AKI, chronic kidney disease (CKD) and RRT prior to enrollment. To better explore the effects of SMART and SPLIT trials with large sample size on our study, we perform sensitivity analysis by removing each single study and additional subgroup analysis by sample size and risk levels of bias.
Additional analysis
Sensitivity analyses were used to estimate the effect of chloride content of intravenous fluid on clinical outcomes of in-hospital, 30-day and 60-day mortality, development of stage 2 or higher AKI, new RRT use, RRT-free days. It was conducted by sequentially omitting a single study each time, to identify the potential influence of an individual study by STATA (Stata Corporation, College Station, TX, USA).
To prevent the risk of random error from being increased by repeated updates, a two-sided trial sequential analysis (TSA; TSA software version 0.9 Beta; Copenhagen Trial Unit, Copenhagen, Denmark) was performed with α = 0.05 and β = 0.10 (power 90%) and a required diversity-adjusted information size based on the intervention effect suggested by the included trials using a random-effects model, which aimed to assess the effects of chloride content of intravenous crystalloid fluid on in-hospital mortality of critically ill patients [16,17,18,19].
Results
Summary of the randomized trial characteristics
The flow diagram shows the study selection process in Fig. 1. Overall, we identified 2666 articles and excluded 2555 after screening the titles and abstracts for the terms “saline,” “balanced solution,” “randomized control trial” and “critically ill.” Eight trials with 19,326 patients were finally included in this meta-analysis after retrieving 103 full-length manuscripts. The subjects who were included were critically ill adult patients and were randomized to buffered crystalloids of low chloride content versus saline administration. A total of 9744 subjects received balanced solutions, while the remainder were in the control group. Among all the included studies, six studies followed the patients until hospital discharge [9, 20,21,22,23,24], and the others followed the patients for 60 days [10, 25]. Ninety-six (0.5%) patients of two studies included were transferred to ICU postoperation [20, 21], while most of studies were performed in the ICU setting [9, 10, 22,23,24,25]. The main characteristics of the included studies are shown in Table 1.
Fluid interventions
A total of 19,301 patients reporting outcomes and analyzed were exposed to crystalloid solutions of different chloride contents as outlined in Table 1. Lactated Ringers alone as balanced crystalloid solution exposures was received in experimental group arms by 48 patients [20,21,22] and Plasma-Lyte 148 alone by 1207 patients [9, 23, 24]. The majority of the studies, including the two largest studies included [10, 25] used a mixed low-chloride crystalloid solution of lactated Ringers and Plasma-Lyte 148. Only 142 subjects (8.3%) in our meta-analysis received volume with a median or mean around 5L or above [20, 21, 23]. Most of the patients (19,105/19,301) experienced a relatively low, 2–3 L study fluid exposure during the follow-up period [9, 10, 24, 25]. One study did not report the crystalloid fluid volume [22].
Risk of bias and GRADE levels
We assessed each included trial by the mode of randomization, allocation concealment, level of blinding and loss to follow up (Additional file 1: Figure S1). Four studies [9, 20, 22, 24] were judged to be at low risk of bias, with adequate randomized sequences, concealed allocation and analyzed outcomes of patients by assigned group. Three trials were judged to be at high risk of bias due to performance bias [10, 25] or attrition bias [23]. Risk of bias was unclear for the remaining one study [21]. The GRADE profile shows that evidence of this meta-analysis is of low quality for in-hospital mortality and of low or very low quality for renal outcomes, as seen in Additional file 1: Figure S2, suggesting further studies might be needed to reach a solid conclusion.
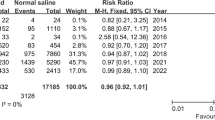
Impact on mortality
Among the included studies, 19,301 patients reported the in-hospital mortality and were included in the primary analysis, among which the pooled in-hospital mortality rate was 10.1% (986/9744) and 10.9% (1045/9557) in groups of balanced crystalloids and 0.9% saline, respectively. Pooled estimates of included studies indicated a trend toward survival benefit with no significant difference in patients receiving balanced crystalloid solutions versus 0.9% saline with an RR of 0.92 (95% CI, 0.85–1.00; p = 0.06, Fig. 2). There was no significant heterogeneity (p = 0.88, I2 = 0%) among all in-hospital mortality analyses (Table 2). Meanwhile, there were no significant differences in the 30-day and 60-day mortality between groups with balanced crystalloids and 0.9% saline (Table 2).
In the TSA shown in Fig. 3, a required diversity-adjusted information size of 80,946 patients was calculated with the relative risk reduction of 6.42% according to the in-hospital mortality of 10.2% and 10.9% in balanced crystalloids group and 0.9% saline group, respectively [9, 10, 20,21,22,23,24,25]. The cumulated Z-curve (blue) failed to reach the traditional boundary (p = 0.05), the trial sequential monitoring boundary as well as the estimated information size boundary (Fig. 3), indicating insufficient evidence to draw the conclusion.
Trial sequential analysis for in-hospital mortality. TSA was performed based on a relative risk reduction of in-hospital mortality of 6.42% according to 10.2% in balanced crystalloids group and 10.9% in 0.9% saline group in eight trials with 19,301 patients reporting in-hospital mortality. A required diversity-adjusted information size of 80,946 patients was calculated. The cumulated Z-curve (blue) failed to reach the traditional boundary (p = 0.05), the trial sequential monitoring boundary as well as the estimated information size boundary. TSA is for trial sequential analysis
Subgroup analysis revealed that the effect of balanced crystalloid fluid on in-hospital mortality was not associated with the balanced crystalloid fluid type, volume or patients’ settings (Table 3). No significant differences were detected in subpopulations with non-sepsis (5 trials, RR = 0.96; 95% CI, 0.86–1.07; p = 0.48, I2 = 0%, Table 3) or TBI (2 trials, RR = 1.11; 95% CI, 0.86–1.43; p = 0.02, I2 = 0%, Table 3) with balanced crystalloids administration compared with 0.9% saline. Of note, significant differences were observed in septic and non-traumatic patients.
Notably, a reduced in-hospital mortality rate was detected in subgroup analysis to be associated with balanced crystalloids compared with 0.9% saline among septic patients (n = 2420; RR = 0.86; 95% CI, 0.75–0.98; p = 0.02, I2 = 0%, Table 3) rather than non-septic patients (RR = 0.96; 95% CI, 0.86–1.07; p = 0.48, Table 3) despite no substantial evidence of such differences when trials were stratified by sepsis or not (p = 0.18 for interaction, Fig. 4). Besides, TSA was performed with expectation of relative risk reduction of 14.48% according to the in-hospital mortality in balanced crystalloids group (24.8%) and the control group (29%) [9, 10, 20,21,22]. The Z-curve crossed the conventional boundary, but did not exceed either the trial sequential monitoring boundary for benefit or the required information size of 4686, suggesting that this meta-analysis could not draw firm positive results for the insufficient sample currently (Fig. 5).
Trial sequential analysis for in-hospital mortality in subgroup of septic patients. A relative risk reduction relative risk reduction of 14.48% according to the in-hospital mortality in balanced crystalloids group (24.8%) and the control group (29%) was pursued. The cumulated Z-curve (blue) crossed the conventional boundary, but did not exceed either the trial sequential monitoring boundary for benefit or the required information size of 4686
Subgroup analysis revealed that balanced crystalloid fluid administration was associated with a lower in-hospital mortality rate when compared with 0.9% saline group for patients without traumatic brain injury (n = 16,794; RR = 0.90; 95% CI, 0.82–0.99; p = 0.02, Table 3), but not the patients with traumatic brain injury (n = 1420; RR = 1.11; 95% CI, 0.86–1.43; p = 0.43, Table 3). This is despite the fact that we found no substantial evidence of such differences when trials were stratified by TBI or not (p = 0.13 for interaction, Fig. 6). In the TSA, a required information size of 31,123 patients was calculated with the relative risk reduction of 10.48% according to the in-hospital mortality of 9.4% and 10.5% of patients without TBI in balanced crystalloids group and 0.9% saline group, respectively [9, 10, 20,21,22]. The Z-curve crossed the conventional line, but reached neither the trial sequential monitoring boundary for benefit nor the estimated information size boundary (Fig. 7), indicating lack of samples to reach the reliable and conclusive cumulative evidence.
Trial sequential analysis for in-hospital mortality in subgroup of non-traumatic brain injury patients. Trial sequential analysis for a relative risk reduction of 10.48% according to the in-hospital mortality of 9.4% and 10.5% of patients without TBI in balanced crystalloids group and 0.9% saline group, respectively [9, 10, 20,21,22], was performed. A required diversity-adjusted information size of 31,123 patients was calculated. The cumulated Z-curve (blue) crossed the conventional line, but reached neither the trial sequential monitoring boundary for benefit nor the estimated information size boundary. TBI is for traumatic brain injury
Impact on renal outcomes
Meta-analysis results for renal end points (receipt of new RRT, stage 2 or higher AKI development and RRT-free days) are summarized in Table 2. No statistically significant impact on development of stage 2 or higher AKI was detected in the three studies included (I2 = 0, p = 0.11) [9, 10, 25]. A total of 531 patients received new RRT after enrollment in the five trials included, and there was no apparent effect in patients treated with balanced crystalloid compared to 0.9% saline (I2 = 0%, p = 0.24). Among them, three studies (9, 10, 25) with 423 patients provided detailed indications for new RRT use, which included oliguria, acidemia, blood urea nitrogen over 70 mg/dL, serum creatinine over 3.39 mg/dL and organ edema. The data showed no difference between groups of patients treated with balanced crystalloid and 0.9% saline solutions (Additional file 1: Figure S3). However, regardless of no difference of new RRT use, there was a significant advantage with respect to longer RRT-free day in patients treated with balanced crystalloid solutions compared to the controls (SMD 0.09, 95% CI [0.06, 0.12], I2 = 0, p < 0.001, Table 2).
Two studies of Selmer in 2016 and 2018 introduced the composite outcome of MAKE30, which is defined as the occurrence of any of the following: in-hospital mortality, new RRT use or a 200% increase in serum creatinine from admission to discharge at 30 days after ICU admission [10, 25]. The effect of balanced crystalloid fluid administration seemed to be protective in reducing MAKE30 incidence for subgroups of patients with sepsis (RR = 0.81, 95% CI, 0.66–1.01, p = 0.06, Additional file 1: Fig S4a). Balanced crystalloid fluid administration was found to be associated with a reduction in incidence of MAKE30 in patients receiving RRT prior to enrollment when compared with the controls (RR = 0.73, 95% CI, 0.55–0.97, p = 0.03, Additional file 1: Fig S4b), while there was no difference among subgroups stratified according to baseline renal function (p = 0.31 for interaction).
Impact on serum content
Three studies [20, 21, 23] provided data of biochemical values before and after crystalloid fluids administration (Additional file 1: Figure S5). Analysis of effects on serum content revealed that balanced crystalloid fluid was associated with significantly lower risk of increase in serum chloride (SMD − 1.23, 95% CI [− 1.59, − 0.87], p < 0.001; I2 = 0%) and sodium (SMD − 1.28, 95% CI [− 1.65, − 0.92], p < 0.001; I2 = 0%) compared to 0.9% saline. There was a significant decline in serum base deficit (SMD − 0.58, 95% CI [− 0.98, − 0.18], p = 0.004; I2 = 26%) with 0.9% saline compared to balanced crystalloid fluid infusion. There was no significant difference in alterations of serum pH value and bicarbonate concentration between balanced crystalloids and 0.9% saline groups.
Impact on organ function
There was no significant difference between balanced crystalloids versus 0.9% saline with respect to use of MV, but balanced crystalloid fluid was associated with significantly longer ventilator-free days (SMD 0.08, 95% CI [0.05, 0.11], p < 0.001; I2 = 0%) and vasopressor-free days (SMD 0.04, 95% CI [0.00, 0.07], p = 0.02; I2 = 0%, Additional file 1: Figure S6) compared to the control.
Discussion
Consist with the previous meta-analysis [11, 26], the available RCTs fail to prove significant difference in in-hospital mortality and show a slight trend of in-hospital survival benefit without statistic difference toward balanced crystalloid solutions administration compared with 0.9% saline in critically ill adult patients. However, we found that assignment to balanced crystalloid solutions instead of 0.9% saline was associated with reduced mortality risk among the subgroup of patients with sepsis or non-TBI despite insufficient samples within present trials to draw the robust conclusion. In addition, the use of balanced crystalloid solutions was associated with longer RRT-free days, MV-free days and vasopressor-free days as well as less risk of increase in serum concentrations of chloride and sodium and less risk of decline in serum base deficit.
The use of 0.9% saline was proved with risk of hyperchloremic metabolic acidosis and related complications [7], suggesting an increase in death risk. Our meta-analysis revealed no statistically beneficial effect of balanced crystalloid fluid on in-hospital survival in critically ill adult patients compared with 0.9% saline. The neutral result might be explained by the following reasons. Firstly, an optimal sample size was not achieved according to the TSA results for reaching the reliable and conclusive cumulative evidence. Besides, the clinical heterogeneity should be taken into considerations. As the Semler study in 2016 suggested, there was a “dose-dependent” relationship between the development of major adverse kidney event and volume of crystalloid fluid received [25]. The relatively low volume of fluid exposure in selected study (median volume of 4 trials is no more than 5 L) during follow-up period [9, 10, 24, 25] may underestimate the effects of crystalloid fluid on prognosis. Thirdly, most patients included in our meta-analysis held a relatively low death risk of 10.1% (986/9744) and 10.9% (1045/9557) in groups of balanced crystalloids and 0.9% saline, respectively. The potential harm might surface among patients with high risk of death and renal injury. In this line, the effects of crystalloids administration might be underestimated by such a small proportion of included patients at high risk of acute kidney injury or who required large volumes of intravenous fluids, such as septic or septic shock patients. Hence, we conducted subgroup analyses by volume and type of crystalloid fluid, patient settings as well as specific patients with sepsis or not, TBI or not and different baseline of renal function. Of note, the difference in reducing in-hospital mortality between balanced crystalloids and saline appeared to be greater for patients with sepsis and non-traumatic brain injury.
For sepsis and septic shock, fluid therapy remains the cornerstone of hemodynamic resuscitation [27, 28]. Septic patients were likely to need larger volume of crystalloid fluid than those of non-sepsis and held higher severity of disease with elevated risk of renal injury and death. In our study, the calculated death risk in groups of balanced crystalloids and 0.9% saline was 24.8% (300/1208) and 29.0% (351/1212), respectively, in septic subpopulations, higher than 10.1% (986/9744) and 10.9% (1045/9557) for overall population. The subgroup analysis showed balanced crystalloid fluid administration could benefit septic patients with significantly reduced death risk, in accordance with the 2018 Selmer study and parts of review by Rochwerg in 2014 [8, 10]. However, there was no significant difference in the subgroup analysis stratified by the volumes of crystalloids fluid administration, which might be explained by the bias following the quite small population of 142 in group receiving larger volume of 5 L leading to a large variation. More samples were still in need to draw the firm positive results for septic patients according to the TSA. These findings suggest that it is necessary to be aware of the risks to septic patients in clinical management of fluid resuscitation.
Subgroup analysis and TSA revealed trends toward accumulative evidence that patients without TBI would benefit from the use of balanced crystalloid fluid. Previous studies have recognized that 0.9% saline solutions could benefit the TBI patients from reduced complications of cerebral edema and intracranial hypertension with a relatively higher osmolality [29,30,31]. The use of balanced crystalloid fluid may worsen the condition of TBI patients for relatively low osmolality with risk of cerebral edema and intracranial hypertension [32], which is clinically important.
It is worth noticing that two large studies of SPLIT [9] and SMART [10] trials consist of more than 98% of patients. Our meta-analysis showed similar results with SPLIT (9) and SMART (10) studies regarding to comparisons between balanced crystalloid fluid versus 0.9% saline on in-hospital mortality of critically ill adult patients. There was no effect on statistical results either following variety of sample size in subgroup analysis or when removing each single study in sensitivity analysis. The evidence levels remain debatable though results of large-scale RCTs seemed persuasive. The results did not differ among studies of high, low or unclear risk levels as subgroup analysis shown in subgroup analysis, while the Semler study in 2018 was judged to be at low risk of bias due to performance bias, degrading the level of evidence despite contributing the largest sample size.
Inconsistent with the before and after treatment study in which balanced crystalloid solutions administration was associated with decreasing the incidence of AKI and RRT use [7], our meta-analysis showed no difference between balanced crystalloid and 0.9% saline fluid groups regarding development of stage 2 or higher AKI and new RRT use. Our study found statistically longer RRT-free days with use of balanced crystalloid fluid in the two selected trials [10, 25], despite no statistical difference regarding incidence of RRT use compared to 0.9% saline. Besides, after stratifying the patients by categories of baseline kidney function, we found that balanced crystalloid fluid was associated with decreased risk of the incidence of MAKE30 in prior RRT subgroup [10, 25]. Therefore, further studies remain in need to make meaningful comparisons in terms of renal end points for heterogeneous ICU populations with categories of baseline kidney function.
Our findings showed that balanced crystalloid fluid administration was associated with less increase in serum concentrations of chloride and sodium and less decline in serum base deficit, which is in agreement with previous literature data [33]. Of note, the data in our study showed the alterations of serum content without considerations of preconditions such as hypernatremia/hyponatremia or hyperchloremia/hypochloremia, in which effects of balance crystalloid fluid might differ between trials.
Our study merges several strengths. Two of the largest RCT trials, SMART [10] and SPLIT trials [9], were included with which the total sample exceeded 19,000. We believe that our study is one of the first meta-analyses with TSA to assess the effects of chloride content of intravenous crystalloid fluid on critically ill patients. We did an estimation of optimal sample size to provide the definite conclusion, which was not performed in Zayed’s review published recently [26]. What is more, our predefined subgroups took clinical heterogeneity into consideration and results of subgroup analyses provide a trend toward accumulative evidence of benefit in use of balanced crystalloid fluid in septic and non-TBI populations in ICU. These findings provide important and reasonable suggestions between the fluid types for clinical management for patients with sepsis or non-traumatic brain injury.
There are several limitations in our study. First, the evidence was limited for the following reasons. There were variable risks of performance and attrition bias of the included trials as described above, downgrading the quality of the evidence. Despite the statistically low heterogeneity and inconsistency by M–H Chi-square test and the I2 test, the potential heterogeneity originating from varied duration of follow-up and fluid exposure could not be ignored. TSA confirmed no firm conclusion of the results. Accordingly, a larger population with better designed would add more power to the results. Above all, we concluded that limited evidence supported statistical survival benefit with balanced crystalloid solutions according to the GRADE system, which was consistent with the previous literature. Second, rather than relatively small sample size studies, the potential bias following the two large studies of SMART and SPLIT trials with more than 98% of patients could not be ignored despite no statistical difference according to sensitivity analysis and subgroup analysis. Third, although subgroup analyses were performed, heterogeneity existed among trials included. Subgroups in terms of volume exposure were predefined according to median and mean value without considering the range and variance, which might influence results when pooling data. In addition, for the studies presented here, the volume of crystalloid fluid varied from less than 2 L to above 10 L with variable follow-up and incomparable data of daily fluid intake, which limited further analysis of its confounded impact on patients’ outcomes. We estimated the change of serum content before and after the use of crystalloid fluid according to recordable mean and standard deviation as the transferring formulas published. The further discussion regarding effects of balanced crystalloid fluid could not be performed in lack of baseline as mentioned above. The pragmatic ongoing trials [34, 35] may provide high-quality evidence on whether a low-chloride balanced crystalloid, compared with 0.9% saline, improves important clinical outcomes in critically ill patients.
Conclusions
Longer free days of organ support and less fluctuations of serum electrolyte levels as well as base deficit were found with use of balanced crystalloid solutions. Current evidence is insufficient to draw a firm conclusion on mortality with a slight trend of survival benefit toward balanced crystalloid solutions. Nevertheless, our subgroup analysis suggested that its administration was associated with a decrease in in-hospital mortality in septic and non-TBI patients. Large-scale rigorous randomized trials with relatively large fluid exposure among patients of high risk are needed to provide robust evidence for guiding crystalloid fluid choice in critically ill patients.
Abbreviations
- AKI:
-
acute kidney injury
- AKIN:
-
acute kidney injury network
- CI:
-
confidence interval
- CKD:
-
chronic kidney disease
- GRADE:
-
grading of recommendations assessment, development and evaluation
- KDIGO:
-
kidney disease: improving global outcomes
- MAKE30:
-
major adverse kidney event within 30 days
- MV:
-
mechanical ventilation
- M–H:
-
Mantel–Haenszel
- NS:
-
normal saline
- RCT:
-
randomized controlled trial
- RIFLE:
-
risk, injury, failure, loss, and end-stage
- RR:
-
risk ratio
- RRT:
-
renal replacement therapy
- SMD:
-
standard mean difference
- SSC:
-
surviving sepsis campaign
- TBI:
-
traumatic brain injury
- TSA:
-
trial sequential analysis
References
Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–77.
Boer C, Bossers SM, Koning NJ. Choice of fluid type: physiological concepts and perioperative indications. Br J Anaesth. 2018;120(2):384–96.
Hartmann AF, Senn MJ. Studies in the metabolism of sodium r-lactate, I: response of normal human subjects to the intravenous injection of sodium r-lactate. J Clin Invest. 1932;11:327–35.
Ringer S. Regarding the action of hydrate of soda, hydrate of ammonia, and hydrate of potash on the ventricle of the frog’s heart. J Physiol. 1882;3:195–202.
Awad S, Allison SP, Lobo DN. The history of 0.9% saline. Clin Nutr. 2008;27:179–88.
Chowdhury AH, Cox EF, Francis ST, et al. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and Plasma-Lyte® 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg. 2012;256(1):18–24.
Yunos NM, Bellomo R, Hegarty C, et al. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012;308(15):1566–72.
Rochwerg B, Alhazzani W, Sindi A, et al. Fluid resuscitation in sepsis: a systematic review and network meta-analysis. Ann Intern Med. 2014;161(5):347–55.
Young P, Bailey M, Beasley R, et al. Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: the SPLIT randomized clinical trial. JAMA. 2015;314(16):1701–10.
Semler MW, Self WH, Wanderer JP, et al. Balanced crystalloids versus saline in critically ill adults. N Engl J Med. 2018;378(9):829–39.
Kawano-Dourado L, Zampieri FG, Azevedo LCP, et al. Low- versus high-chloride content intravenous solutions for critically ill and perioperative adult patients: a systematic review and meta-analysis. Anesth Analg. 2018;126(2):513–21.
Ad hoc Working Group of ERBP, Fliser D, Laville M, et al. A European renal best practice (ERBP) position statement on the kidney disease improving global outcomes (KDIGO) clinical practice guidelines on acute kidney injury: part 1: definitions, conservative management and contrast-induced nephropathy. Nephrol Dial Transplant. 2012;27:4263–72.
Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Wetterslev J, Thorlund K, Brok J, et al. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol. 2008;61:64–75.
Brok J, Thorlund K, Wetterslev J, et al. Apparently conclusive metaanalyses may be inconclusive-trial sequential analysis adjustment of random error risk due to repetitive testing of accumulating data in apparently conclusive neonatal meta-analyses. Int J Epidemiol. 2009;38:287–98.
Thorlund K, Devereaux PJ, Wetterslev J, et al. Can trial sequential monitoring boundaries reduce spurious inferences from meta-analyses? Int J Epidemiol. 2009;38:276–86.
Torlund K, Engstrøm J, Wetterslev J, et al. User manual for trial sequential analysis (TSA). Copenhagen Trial Unit, Centre for Clinical Intervention Research, Copenhagen, Denmark (2011), pp 1–115 [Available from www.ctu.dk/tsa].
Waters JH, Gottlieb A, Schoenwald P, et al. Normal saline versus lactated Ringer’s solution for intraoperative fluid management in patients undergoing abdominal aortic aneurysm repair: an outcome study. Anesth Analg. 2001;93:817–22.
Takil A, Eti Z, Irmak P, et al. Early postoperative respiratory acidosis after large intravascular volume infusion of lactated Ringer’s solution during major spine surgery. Anesth Analg. 2002;95:294–8.
Young JB, Utter GH, Schermer CR, et al. Saline versus PlasmaLyte A in initial resuscitation of trauma patients: a randomized trial. Ann Surg. 2014;259:255–62.
Van Zyl DG, Rheeder P, Delport E. Fluid management in diabetic-acidosis–Ringer’s lactate versus normal saline: a randomized controlled trial. QJM. 2012;105:337–43.
Verma B, Luethi N, Cioccari L, et al. A multicentre randomised controlled pilot study of fluid resuscitation with saline or Plasma-Lyte 148 in critically ill patients. Crit Care Resusc. 2016;18(3):205–12.
Semler MW, Wanderer JP, Ehrenfeld JM, et al. Balanced crystalloids versus saline in the intensive care unit: the SALT randomized trial. Am J Crit Care Med. 2016;195:1362–72.
Zayed YZM, Aburahma AMY, Barbarawi MO, et al. Balanced crystalloids versus isotonic saline in critically ill patients: systematic review and meta-analysis. J Intensive Care. 2018;6:51.
Winters ME, Sherwin R, Vilke GM, et al. What is the preferred resuscitation fluid for patients with severe sepsis and septic shock? J Emerg Med. 2017;53(6):928–39.
Mendes PV, Zampieri FG, Park M. Is there a role for balanced solutions in septic patients? Shock. 2017;47(1S):30–4.
Finfer S, Bellomo R, Boyce N, et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350:2247–56.
Myburgh J, Cooper DJ, Finfer S, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874–84.
Ertmer C, Van Aken H. Fluid therapy in patients with brain injury: What does physiology tell us? Crit Care. 2014;18(2):119.
Lobo DN, Awad S. Should chloride-rich crystalloids remain the mainstay of fluid resuscitation to prevent ‘pre-renal’ acute kidney injury? Con. Kidney Int. 2014;86(6):1096–105.
Huang L, Zhou X, Yu H. Balanced crystalloids vs 09% saline for adult patients undergoing non-renal surgery: a meta-analysis. Int J Surg. 2018;51:1–9.
Zampieri FG, Azevedo LCP, Corrêa TD, Falavigna M, Machado FR, Assunção MSC, et al. Study protocol for the Balanced Solution versus Saline in Intensive Care Study (BaSICS): a factorial randomised trial. Crit Care Resusc. 2017;19(2):175–82.
Hammond NE, Bellomo R, Gallagher M, Gattas D, Glass P, Mackle D, et al. The Plasma-Lyte 148 v Saline (PLUS) study protocol: a multicentre, randomised controlled trial of the effect of intensive care fluid therapy on mortality. Crit Care Resusc. 2017;19(3):239–46.
Authors’ contributions
MX and HQ contributed to the conception of the systematic review. MX and FL performed the search and extracted the data with discrepancies resolved by XZ. MX, XZ and WC contributed to statistical analysis. MX, JX, JX, YY and HQ contributed to results interpretation. MX and HQ drafted the manuscript. All authors revised the manuscript. All authors read and approved the final manuscript.
Acknowledgements
None.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable for no datasets generated or analyzed during the current study.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
Dr. Haibo Qiu received grant support from Jiangsu Provincial Key Medical Discipline (Grant No. ZDXKA2016025) and the National Natural Science Foundations of China (Grants 81571874). Dr. Yi Yang received grant support from Jiangsu Provincial Key Research and Development program (Grant No. SBE2018750279). Dr. Jianfeng Xie received grant support from the National Natural Science Foundations of China (Grant No. 81601723). The funding sources had no role in study design and conduct, the data collection, analysis and management or manuscript review and approval.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Sensitivity analysis of the effects of chloride content in crystalloid fluid on critically ill patients’ outcomes. Figure S1. a Risk of bias graph. Review authors’ judgements about each risk of bias item resented as percentages across all included studies. b Risk of bias summary for each included study Red (-) indicates high risk of bias; yellow (?) indicates unclear risk; and green (+) indicates low risk of bias. Figure S2. GRADE profile for assessing quality of evidence. Figure S3. Forest plots for indications of new RRT use after enrollment. Figure S4. Forest plots for MAKE30 in predefined subgroups. a Sepsis and non-sepsis subgroups. b Subgroups according to categories of baseline renal function. MAKE30 is for major adverse kidney events within 30 days. Figure S5. Forest plots for alterations’ of serum content among critically ill patients. Figure S6. Forest plots for organ support. a MV use of critically ill patients. b Ventilator-free day of critically ill patients. c Vasopressor-free days of critically ill patients. MV is for mechanic ventilation. Figure S7. Funnel plots. a Funnel plots for in-hospital mortality. b Funnel plots for 30-day mortality. c Funnel plots for 60-day mortality. d Funnel plots for development of stage 2 of higher AKI of critically ill patients. e Funnel plots for new RRT use of critically ill patients. f Funnel plots of for RRT-free days of critically ill patients. AKI is for acute kidney injury according to KDIGO criterion; RRT is for renal replacement therapy.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Xue, M., Zhang, X., Liu, F. et al. Effects of chloride content of intravenous crystalloid solutions in critically ill adult patients: a meta-analysis with trial sequential analysis of randomized trials. Ann. Intensive Care 9, 30 (2019). https://doi.org/10.1186/s13613-019-0506-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-019-0506-y