Abstract
Background
Pneumonia is one of the major complications of drowning, but the optimal empirical antibiotic treatment is not clearly defined. Multidrug-resistant (MDR) bacteria and fungi have been identified in a recent series of freshwater drowning-associated pneumonia. However, microbial data in seawater drowning are scarce. The objective of the study is to describe the microorganisms isolated in early respiratory specimens obtained from seawater drowning-associated pneumonia and to provide their antibiotic susceptibility pattern.
Methods
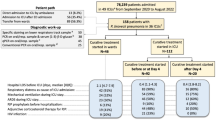
All patients admitted for seawater drowning between 2003 and 2013 to two intensive care units, from the region in France with the highest drowning rate, were retrospectively included. Demographics, antimicrobial therapy and microbiological data from respiratory samples collected within the first 48 h after admittance were analyzed.
Results
Seventy-four drowned patients were included, of which 36 (49%) were diagnosed by the clinician as having early pneumonia. Concerning the overall population, the median simplified acute physiology score (version 2) was 45 (30–65), and the mortality was 26%. Twenty-four respiratory samples from different patients were obtained within the first 48 h. Sixteen were positive. The main microorganisms found were Enterobacteriaceae (Enterobacter spp., Klebsiella spp. and Escherichia coli) and Gram-positive aerobic cocci (Streptococcus pneumonia and Staphylococcus aureus) with a low rate of antimicrobial resistance. No MDR bacteria or fungi were identified. However, among the positive respiratory samples collected, 5/16 (31%) grew bacteria with natural resistance to amoxicillin–clavulanate, the first-line antibiotic commonly used in our cohort. Resistance was only found among Gram-negative bacteria and from respiratory samples of patients with a higher drowning grade at admission (p = 0.01).
Conclusions
This 10-year descriptive study, the largest cohort to date, provides early respiratory samples from seawater drowning patients. The microorganisms retrieved were either mostly part of the human oro-pharyngeal flora or Enterobacteriaceae and displayed low rates of antimicrobial resistance. Respiratory samples should nonetheless be collected at admittance to the ICU to avoid inappropriate treatment. Empiric use of cephalosporin could be restricted to severe patients or if Gram-negative bacilli are found after direct examination.
Similar content being viewed by others
Background
Despite recent progress in the management of respiratory complications due to drowning [1, 2], criteria to initiate antibiotic or to collect respiratory samples are lacking [2,3,4]. In addition, available data on the microorganisms involved in drowning-associated pneumonia are too scarce to recommend a straightforward antibiotic strategy [3]. Two recent series on freshwater drowning in urban areas, from Paris and Amsterdam region with, respectively, 37 and 49 patients [5, 6], described a significant proportion of MDR bacteria or presence of fungi in early respiratory samples suggesting the use of broad-spectrum antibiotics or even empirical antifungal therapy. Water composition (i.e., freshwater or seawater) and locality may influence such susceptibility patterns [2]. However, to the best of our knowledge, microbial data in seawater drowning-associated pneumonia are very scarce and generally gathered from cases reports [7,8,9,10] or reviews of cases from warm seas [3] but none from temperate Mediterranean zones.
The aim of this study is to describe the bacterial species and their antibiotic susceptibility patterns recovered from early respiratory samples of drowning-associated pneumonia from seawater drowning patients in the Mediterranean Sea.
Methods
Study population and demographics
This retrospective observational bi-center study traced and identified through ICD coding of all adult patients admitted for seawater drowning between 2003 and 2013 in two intensive care units in the city of Nice (Mediterranean Sea) which lies in the region with the highest drowning rate in France [11]. Patients admitted for swimming pool or freshwater drowning were excluded. There were no specific guidelines for the management of drowning pneumonia in either center.
Drowning was defined as respiratory impairment following immersion in water, whatever the survival [12]. The drowning grade was determined according to the recent classification described by Szpilman et al. [2, 13] (Table 1). Collected data were: age, sex, presence of initial cardiac arrest, drowning grade [2], respiratory samples collected within 48 h, microorganisms and antibiotic susceptibility patterns, diagnosis of pneumonia or ARDS, causes of drowning, season and place of drowning, duration of mechanical ventilation, length of stay and mortality in the ICU, therapeutic administration and the SAPS2 score [14].
Because of the observational nature of the study, patient’s consent was waived. Follow-up for the study was performed until ICU discharge. According to the Commission Nationale de l’Informatique et des libertés, there were no needs of specifics authorization because of the anonymous character of the data collected.
Bacteriology and microbiological data
Respiratory samples collected within the first 48 h of admission were analyzed. Cultures were incubated in aerobic (with or without 5% CO2) and in anaerobic conditions during 48 h at 35 °C on both selective and non-selective media. Colonies of interest were identified, quantified and tested for antibiotic susceptibility. The 48-h limit was retained so as to exclude ICU-acquired infection (i.e., ventilator-associated pneumonia) [15].
In accordance with current guidelines, the quantitative bacterial thresholds used to define bacterial pneumonia were 103 colony-forming units per milliliter (cfu/mL) for distal protected samples and 105 cfu/mL for tracheal aspirates [16]. When tracheal aspirates were performed, only high-quality specimens (i.e., with more than 25 neutrophils and less than 25 epithelial cells per microscopic field) graded groups 4 or 5 according to the Murray–Bartlett–Washington definition were taken into consideration [17].
Diagnosis of pneumonia
Diagnosis of pneumonia was based on miscellaneous criteria, including fever defined by body temperature of more than 38.5 °C, presence of purulent endotracheal secretions, leukocyte blood count greater than 10,000/mm3 or less than 4000/mm3, and radiological features of pneumonia according to the perception of the clinician [18,19,20]. Bacteriological criteria could not always be used because respiratory samples were not systematically collected. Diagnosis of ARDS was made according to the 2012 Berlin definition [22] and based on the American and European Consensus Conference on ARDS prior to 2012 [23].
Statistical analysis
Statistical analyses were performed using the Statistical Package for Social Science software, version 19 (SPSS, Chicago, Illinois, USA). Continuous variables are presented as median and 25th–75th percentile. Categorical variables are presented as either rates or percentages. The Fisher’s exact test was used for comparison of categorical variables. U Mann and Whitney tests were used for comparison of continuous variables. Differences were considered statistically significant when the p value was <0.05.
Results
Demographics
From January 2003 to April 2013, 74 patients were admitted for seawater drowning to the two ICU. None of them was excluded.
The male-to-female sex ratio was 1.85, and the median age was 68 (51–77) years. Thirty patients (41%) presented out-of-hospital cardiac arrest. Nineteen patients died during their ICU stay, defining a 26% ICU mortality rate. The median SAPS2 score was 45 (30–65). The main objectified causes for drowning were medical with 22/74 (30%) cases of divers medicals pathologies (such as seizures or cardiovascular dysfunction). Other causes were 16 (22%) sports-related injuries or unspecified trauma (including those occurring under the influence of alcohol), 7 (9%) physical exhaustion and 6 (8%) suicides. Unknown causes accounted for 23 (31%) cases in which resuscitation was carried out without prior knowledge of the time of drowning. Patient characteristics are summarized in Table 2.
All patients were found at sea in a similar coastal environment within 300 meters of the coast. In 61 (84%) cases, drowning occurred during the summer and spring.
Pneumonia, respiratory samples and bacteriological data
Of the 74 patients, four died within the first 24 h of admission and before any bacteriological sample could be obtained. Thirty-six patients (49%) were diagnosed and curatively treated for pneumonia. Twenty-five (34%) had ARDS. Four patients (5%) received curative antibiotics (more than 24 h) without proven pneumonia diagnosis and without respiratory sample during the first 48 h. Four additional patients (5%) received antibiotics for less than 24 h after admission, until the medical team challenged the diagnosis of pneumonia. Finally, 44 patients (59%) received antibiotics; among them, 40 (54%) received antibiotics for more than 24 h during the first week of hospitalization.
Respiratory specimens were obtained from 24 (32%) patients within the first 48 h of admission to the ICU with 19 (79%) protected distal samples and 5 (21%) tracheal aspirates. Bacteria were isolated at a significant count from 16 respiratory samples (22% of all patients and 67% of the early respiratory samples), and 24 different bacterial species were identified. Enterobacter spp. were the most frequent microorganisms followed by Streptococcus pneumonia and Staphylococcus aureus. Pseudomonas aeruginosa was found in only one case. No fungi were isolated (Table 3).
Antibiotic susceptibility testing showed chromosomal penicillinase in four cases (for two Klebsiella spp. and two Citrobacter koserii) with a preserved susceptibility to amoxicillin–clavulanate (AMC). An inducible chromosome-encoded AmpC cephalosporinase was present in six strains: five Enterobacter spp. and one Pseudomonas aeruginosa. P. aeruginosa isolate is also resistant to ticarcillin, ticarcillin–clavulanate and aztreonam due to overexpression of MexAB-OprM efflux pump (Table 4) but did not qualify as a multidrug-resistant (MDR) bacteria according to international criteria [21]. Five respiratory samples had at least one strain with bacterial resistance to AMC. Overall, resistance to AMC was observed in 5/16 (31%) of early respiratory samples and in 6/24 (25%) bacterial species (Table 3). All cases of AMC resistance were observed for the Gram-negative bacilli species with 6/14 (43%) resistant.
Characteristics and outcomes of patients according to the resistance of the microorganisms
Compared to patients with sensitive microorganisms, patients with naturally resistant microorganism to AMC, found during the first 48 h, had a higher rate of cardiac arrest (p = 0.026), higher drowning grade (p = 0.013), longer duration of initial resuscitation (p = 0.004), longer duration of mechanical ventilation (p = 0.025) and a higher mortality rate in ICU (p = 0.013). The SAPS2 score was not significantly different between the two groups nor the age, sex, initial Glasgow score, number of comorbidities (such as COPD, diabetes, coronary disease and chronic kidney disease), rate of invasive ventilation and length of stay (Table 5).
Type of antibiotic therapy and adaptation to the microbiological results
AMC was the most common empiric antimicrobial treatment within the first 48 h (in 34/36 cases, 94%). However, two patients received, on admission, piperacillin–tazobactam as empiric treatment that was downgraded to AMC after obtaining the results of antibiotic susceptibility testing. Thirty-three patients received AMC as definitive treatment, and another three received cephalosporin for infection due to Enterobacter spp. The median duration of the antibiotic treatment was 7 (5–7) days.
All patients with positive respiratory specimens were initially treated empirically, 8/16 (50%) had appropriate empirical treatment, 4/16 (25%) had their treatment modified after receiving the bacteriological results (adapted to culture and susceptibility testing), 3/16 (19%) did not benefit from adaptation of their treatment to the microbiological results without a clear explanation mentioned in the medical record, but survived in the ICU. One patient died in the ICU without adaptation of the antibiotic treatment because the decision to limit life-sustaining therapies was taken before obtaining the final bacteriological results.
Discussion
This 10-year retrospective study is to date the largest cohort of early respiratory sample collection from seawater drowning patients. We found that wild-type Enterobacter spp. is the most represented bacterial species and is likely due to aspiration of contaminated water or endogen flora. Among the respiratory samples collected, 5/16 (31%) grew bacteria with natural resistance to amoxicillin–clavulanate, the first-line antibiotic commonly used in our cohort. Unlike freshwater drowning-associated pneumonia, no specific MDR bacteria nor fungi were found [5, 6].
Pneumonia appears to be a common complication in large series of drowning survivors admitted to ICU [4] and was diagnosed in nearly half of all patients in our series. Antimicrobial susceptibility patterns are currently debated as illustrated in recent series of freshwater drowning in urban areas. Low rates of antibiotic resistance were found in respiratory samples from our patients. Only one strain of Pseudomonas aeruginosa was found, and despite showing resistance to ticarcillin, it did not qualify as a MDR species [21].
However, resistance to AMC was seen in a third of cases mainly due to Enterobacter spp. This chromosomal resistance pattern could not be associated with a specific population in our study, but these findings should encourage clinicians to perform respiratory sample collection as early as possible to avoid inappropriate antibiotic therapy.
We cannot identify the pathophysiological or environmental processes that would explain the microbial findings. The bacterial species that were isolated are likely to come from the oro-pharyngeal and/or gastric flora and would suggest aspiration pneumonia as described in previous series [22]. Conversely, the large proportion of Enterobacter spp. that was identified in our series is not typical of aspiration pneumonia and suggests seawater inhalation.
Accidental bacterial flora constituted by fecal contamination has been frequently described in seawater [23], and this contamination could explain the bacterial findings. French local authorities are therefore frequently compelled to specifically quantify this flora as a marker of marine pollution, but their analysis mainly focuses on microorganisms of interest to reflect human fecal pollution (Escherichia coli and Enterococcus spp.). Pollution by antibiotic substances in freshwater has been described near urban areas [24] but poorly studied in seawater. Further bacteriological studies into the marine environment are needed to understand the involvement of fecal flora contaminating seawater in the pathophysiology of pneumonia associated with drowning.
To reduce the risk of emergence of AmpC-hyperproducing Enterobacteriaceae, European guidelines discourage the use of third-generation cephalosporins as single-drug therapy against Enterobacter spp. [25]. When antibiotic treatment cannot be delayed, fourth-generation cephalosporin such as cefepime could be suggested as a first-line treatment and later downgraded according to bacteriological results. When direct examination can be rapidly obtained, cefepime may be kept specifically for Gram-negative bacilli, whereas Gram-positive cocci could be treated with amino-penicillin combined with a beta-lactamase inhibitor. The authors highlight that antibiotic treatments should always be tailored to local epidemiological microbial data.
Patients presenting with an AMC-resistant bacteria respiratory infection seemed to have a more severe initial clinical presentation (more cardiac arrest, longer resuscitation duration and higher drowning grade) and worse outcome (duration of mechanical ventilation, mortality in ICU), which was not associated with specific demographic characteristics (age, sex or comorbidity). Indeed half of them were less than 65 years and had never been hospitalized.
This point should be specifically addressed in a larger prospective study and a larger antibiotic spectrum discussed for patient with an initial severe clinical presentation notably after cardiac arrest and a high drowning grade.
Our results show a clear difference between seawater and freshwater drowning-associated pneumonia, with recent data promoting the use of a broad-spectrum antibiotic and even suggesting empirical antifungal therapy [5, 6]. Should this be confirmed in a future prospective study combined with environmental analysis, the water composition should define the antimicrobial strategy for empirical treatment.
Limitations
This study represents a local population admitted to the two intensive care units with the biggest local recruitment of severe drowning. However, patients were all found in a similar coastal environment and mostly during the summer and spring. The marine bacterial ecology may change according to the season, location and human pollution, but the impact of such modifications is still unknown and can be minimal if the main mechanism involved is aspiration of the endogen flora of the patients. Indeed, seawater samples have not been described in our study because they were not considered to represent the water composition during the ten years of the study. Such samples could be analyzed in a future prospective study and be compared with respiratory sputum collected from patients during the same period.
Only 24/36 patients presenting with early pneumonia had a respiratory sample. This may affect the prevalence of the susceptible microorganisms observed in this study.
The absence of anaerobic bacteria found in the respiratory samples does not formally exclude their potential impact in the pathogenic process of pneumonia associated with seawater drowning. Indeed, these bacteria are fragile and require specific conditions and media for culture [26, 27]. Even if we cannot formally exclude anaerobic germs in this inhalation context, according to our results treatment with specific empirical antibiotic against these bacteria seems unnecessary.
Finally, the diagnosis of pneumonia is difficult for this population. An X-ray and biomarkers cannot be considered as a relevant tool to confirm or rule out diagnosis. Bacteriological samples may be of clinical, economical and of ecological interest.
Conclusions
This cohort is the largest providing early respiratory samples from seawater drowning patients. Unlike recent data from freshwater drowning series, microorganisms found are mostly bacteria with a low rate of antibiotic resistance suggesting that drowning environment influenced previous observations. When empirical antibiotic therapy is required after seawater drowning, systematic broad-spectrum antibiotics appear unnecessary. Early respiratory sample collection should nonetheless be mandatory to avoid inappropriate therapy. Empirical cephalosporin could be proposed for the most severe patients or, if a direct examination can be rapidly performed, for Gram-negative bacilli, whereas patients with Gram-positive cocci could be treated with amino-penicillin combined with a beta-lactamase inhibitor.
Abbreviations
- ARDS:
-
acute respiratory distress syndrome
- MDR:
-
multidrug resistant
- ICD:
-
International Classification of Diseases
- ICU:
-
intensive care unit
- SAPS2:
-
simplified acute physiology score 2
- COPD:
-
chronic obstructive pulmonary disease
- AMC:
-
amoxicillin–clavulanate
References
Michelet P, Bouzana F, Charmensat O, Tiger F, Durand-Gasselin J, Hraiech S, et al. Acute respiratory failure after drowning: a retrospective multicenter survey. Eur J Emerg Med. 2015. doi:10.1097/MEJ.0000000000000362
Szpilman D, Bierens JJLM, Handley AJ, Orlowski JP. Drowning. N Engl J Med. 2012;366(22):2102–10.
Ender PT, Dolan MJ. Pneumonia associated with near-drowning. Clin Infect Dis. 1997;25(4):896–907.
Modell JH. Drowning. N Engl J Med. 1993;328(4):253–6.
Tadié JM, Heming N, Serve E, Weiss N, Day N, Imbert A, et al. Drowning associated pneumonia: a descriptive cohort. Resuscitation. 2012;83(3):399–401.
Assink-de Jong E, Douma M, Beishuizen A, Hoogewerf M, Debets-Ossenkopp YJ, de Waard MC, et al. Microbiological findings and adequacy of antibiotic treatment in the critically ill patient with drowning-associated pneumonia. Intensive Care Med. 2014;40(2):290–1.
Patel R, Abraham A, Thomas J, Zhi W, Ahmed S, Verley J. A rare case of pneumonia caused by Shewanella putrefaciens. Case Rep Med. 2012;2012:597301.
Wenger JD, Hollis DG, Weaver RE, Baker CN, Brown GR, Brenner DJ, et al. Infection caused by Francisella philomiragia (formerly Yersinia philomiragia). A newly recognized human pathogen. Ann Intern Med. 1989;110(11):888–92.
Kelly MT, Avery DM. Lactose-positive Vibrio in seawater: a cause of pneumonia and septicemia in a drowning victim. J Clin Microbiol. 1980;11(3):278–80.
Chierakul W, Winothai W, Wattanawaitunechai C, Wuthiekanun V, Rugtaengan T, Rattanalertnavee J, et al. Melioidosis in 6 tsunami survivors in southern Thailand. Clin Infect Dis. 2005;41(7):982–90.
Lasbeur L, Szego Zguem E, Thelot B, DMNTT. Surveillance épidémiologique des noyades. Enquête NOYADES 2015. 1er juin–30 septembre 2015. InVS 2016.
Layon AJ, Modell JH. Drowning: update 2009. Anesthesiology. 2009;110(6):1390–401.
Szpilman D. Near-drowning and drowning classification: a proposal to stratify mortality based on the analysis of 1831 cases. Chest. 1997;112(3):660–5.
Le Gall J, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–63.
Chastre J, Fagon J-Y. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867–903.
American Thoracic Society. Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
Murray PR, Washington JA. Microscopic and baceriologic analysis of expectorated sputum. Mayo Clin Proc. 1975;50(6):339–44.
Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL. Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med. 2000;162(2 Pt 1):505–11.
Pugin J. Clinical signs and scores for the diagnosis of ventilator-associated pneumonia. Minerva Anestesiol. 2002;68(4):261–5.
Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic “blind” bronchoalveolar lavage fluid. Am Rev Respir Dis. 1991;143(5 Pt 1):1121–9.
Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–81.
Bartlett JG, Gorbach SL, Finegold SM. The bacteriology of aspiration pneumonia. Am J Med. 1974;56(2):202–7.
Oyafuso ZS, Baxter AE, Hall JE, Naman SM, Greene CM, Rhodes LD. Widespread detection of human- and ruminant-origin Bacteroidales markers in subtidal waters of the Salish Sea in Washington State. J Water Health. 2015;13(3):827–37.
Fatta-Kassinos D, Meric S, Nikolaou A. Pharmaceutical residues in environmental waters and wastewater: current state of knowledge and future research. Anal Bioanal Chem. 2011;399(1):251–75.
Leclercq R, Cantón R, Brown DFJ, Giske CG, Heisig P, MacGowan AP, et al. EUCAST expert rules in antimicrobial susceptibility testing. Clin Microbiol Infect. 2013;19(2):141–60.
Bartlett JG. Anaerobic bacterial infections of the lung and pleural space. Clin Infect Dis. 1993;16(Suppl 4):S248–55.
Strobel HJ. Basic laboratory culture methods for anaerobic bacteria. Methods Mol Biol. 2009;581:247–61.
Authors’ contributions
AR, PED, DD and JD had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. AR, HQ, CI, GB and CP contributed to the study conception; AR, DD, ND and JD contributed to the data acquisition, analysis and interpretation; AR, PED, DD, NM, ND, CP, RR and JD contributed to drafting the manuscript; and AR, PED, DD, HQ, NM, ND, CP, RR and JD contributed to revising the manuscript for important intellectual content and approving the final copy. All authors read and approved the final manuscript.
Acknowledgements
We would like to address specifics acknowledgements to Professor Darmon (Saint-Etienne University, France) for his participation .
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data are presented in the main paper or in table’s files.
Funding
The authors declare that they have no funding for this research.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Robert, A., Danin, PÉ., Quintard, H. et al. Seawater drowning-associated pneumonia: a 10-year descriptive cohort in intensive care unit. Ann. Intensive Care 7, 45 (2017). https://doi.org/10.1186/s13613-017-0267-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-017-0267-4